Bridging the Translational Gap: Establishing Causality Between Animal Models and Human Studies in Microbiome Research
This article provides a comprehensive analysis for researchers and drug development professionals on the critical relationship between animal model findings and human studies in microbiome research.
Bridging the Translational Gap: Establishing Causality Between Animal Models and Human Studies in Microbiome Research
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on the critical relationship between animal model findings and human studies in microbiome research. It explores the foundational principles of host-microbiome interactions, details the application and limitations of current experimental methodologies like germ-free and humanized microbiota mouse models, and addresses pervasive challenges such as establishing causality and overcoming translational bottlenecks. Furthermore, it synthesizes advanced strategies for validating and comparing findings across studies, including the use of machine learning and multi-omics integration. The content is framed by the latest consensus statements and pipeline analyses, offering a practical guide to navigating the complexities of translating preclinical microbiome insights into successful clinical therapies.
The Bedrock of Microbiome Research: From Dysbiosis to Therapeutic Hypotheses
The fundamental challenge in defining dysbiosis stems from the inherent complexity and individuality of the microbiome. Unlike traditional pathogens, dysbiosis represents an ecological imbalance within the microbial community, rather than the presence of a single causative agent [1] [2]. This imbalance can manifest as a reduction in microbial diversity, a loss of beneficial microorganisms, an overgrowth of potentially harmful ones, or a disruption in the community's functional capacity [1] [2]. The core scientific hurdle is the lack of a single, idealized "healthy" microbiome composition against which to compare potentially dysbiotic states [3]. Research indicates that microbiome communities are highly individualized, show a high degree of interindividual variation to perturbation, and tend to be stable over years in healthy adults [3]. Consequently, dysbiosis is often context-specific, with patterns of alteration varying significantly across different diseases and even among individuals with the same condition [3] [2].
Establishing a universal baseline is further complicated by the dynamic nature of the microbiome throughout life. The microbiome undergoes significant development during early life, influenced by factors such as mode of delivery, infant feeding practices, and early antibiotic exposure [3]. This assembly process is shaped by both deterministic host and environmental factors and unpredictable stochastic ecological processes [3]. In adulthood, while the gut microbiome becomes relatively stable, it remains shaped more by environment than host genetics, with factors like diet, medication, and lifestyle accounting for approximately 20% of its variation [3]. The remaining high degree of interindividual variation suggests that a single "healthy" microbiome profile may not exist, but rather a range of functional healthy states [3].
Comparative Analysis: Human Studies vs. Animal Models of Dysbiosis
To understand dysbiosis, researchers employ both human association studies and causal animal models, each with distinct strengths and limitations. The table below summarizes the core methodological approaches and their translational challenges.
Table 1: Comparison of Dysbiosis Research Approaches
| Research Approach | Key Features | Primary Findings on Dysbiosis | Major Limitations |
|---|---|---|---|
| Human Observational Studies | - Correlates microbiome composition with health status.- Uses sequencing & metabolomic profiling.- Large, diverse cohorts. | - High inter-individual variation [3].- Altered composition in diseases (e.g., IBD, obesity) [1] [2].- Mechanistic links are correlations, not causations [3]. | - Cannot establish causality [3].- Confounded by environment, diet, medications [3]. |
| Human Microbiota-Associated (HMA) Mouse Models | - Transplant human microbiota into germ-free or antibiotic-treated mice [4].- Allows controlled intervention studies. | - Can transfer donor microbial signatures and some disease phenotypes [4].- Demonstrates causal role of microbiota in some conditions (e.g., metabolic syndrome) [4]. | - Host genetics, GI anatomy differ from humans [4].- Risk of overestimating causal associations [4]. |
A recurring theme across both human and animal studies is the association between higher microbial diversity and health, while a dynamic loss of diversity may be prognostic of increased disease risk [3]. However, the specific changes associated with disease are often inconsistent across studies. For instance, in aging research, mouse models have helped isolate age-related changes from environmental confounders, revealing consistent declines in taxa like Lactobacillus and increased abundance of genera like Coprococcus and Turicibacter in aged mice [5]. These models demonstrate that the microbiome contributes significantly to the age-related metabolome, particularly in lipid-associated pathways such as linoleic acid metabolism [5].
Experimental Workflows and Key Signaling Pathways
Establishing HMA Animal Models
A critical methodology for establishing causality in dysbiosis research is the creation of HMA animals. The workflow involves stringent donor screening, standardized sample processing, and careful recipient preparation.
Table 2: Key Protocols for Human Microbiota-Associated (HMA) Model Generation
| Experimental Stage | Standardized Protocol | Rationale & Purpose |
|---|---|---|
| Donor Screening | - No antibiotics for 2-12 months [4].- No laxatives for ≥3 months [4].- Exclude GI, neuropsychiatric, and chronic diseases [4]. | Ensures a "healthy" or defined-disease microbiota without recent pharmacological perturbations. |
| Fecal Sample Processing | - Process quickly in anaerobic conditions [4].- Use cryoprotectants for low-temperature storage [4]. | Maintains viability of oxygen-sensitive commensal bacteria during transplantation. |
| Recipient Preparation | - Use germ-free (GF) or antibiotic-induced "pseudo-germ-free" mice [4]. | Creates a vacant niche to maximize engraftment of the human donor microbiota. |
| Fecal Microbiota Transplantation (FMT) | - Multiple gavages over single dose [4]. | Significantly improves the efficiency and stability of donor microbiota colonization. |
| Engraftment Validation | - 16S rRNA gene sequencing of recipient fecal samples [4]. | Confirms successful colonization by donor microbiota before beginning experiments. |
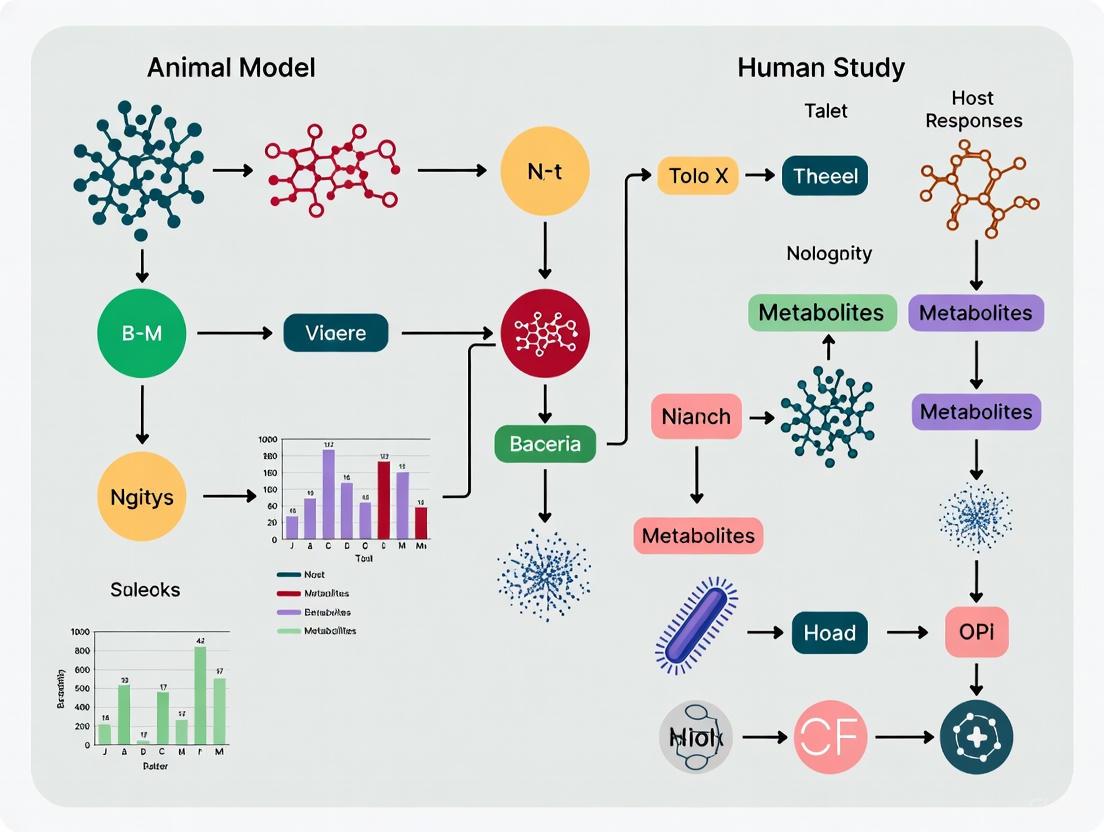
Figure 1: Workflow for Creating HMA Mouse Models. This diagram outlines the standardized protocol for generating HMA animals, from donor screening to final validation.
Pathophysiological Pathways of Dysbiosis
Dysbiosis influences host health through multiple interconnected mechanistic pathways. The primary mechanisms include impaired intestinal barrier function, immune dysregulation, and systemic metabolic effects.
Figure 2: Key Pathophysiological Pathways of Dysbiosis. This diagram illustrates how gut dysbiosis triggers core pathological mechanisms that lead to systemic diseases.
The impaired intestinal barrier allows bacterial products like lipopolysaccharide (LPS) to translocate into circulation, a state known as endotoxemia, which can trigger systemic inflammation [2] [6]. Immune dysregulation occurs as the balance between pro-inflammatory and anti-inflammatory responses shifts, often involving Th cell activation and the release of cytokines like IL-1β and TNF-α [6]. Metabolically, dysbiosis alters the production of microbial metabolites, including short-chain fatty acids (SCFAs), bile acids, and amino acids, which play critical roles in host metabolism, immune function, and even brain health [7] [5]. These mechanisms form the basis of the gut-brain and gut-liver axes, linking dysbiosis to a wide range of conditions far beyond the gastrointestinal tract [1] [6].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Cut-edge dysbiosis research relies on a suite of specialized reagents and technological solutions. The following table details key materials and their applications in microbiome research.
Table 3: Essential Research Reagents and Solutions for Microbiome Research
| Research Reagent / Solution | Function & Application | Experimental Consideration |
|---|---|---|
| DNA/RNA Shield Kits | Preserves nucleic acid integrity in fecal samples during collection and storage. | Critical for accurate sequencing data; prevents microbial community shifts post-collection. |
| 16S rRNA Gene Sequencing Primers | Amplifies specific hypervariable regions for taxonomic profiling of bacterial communities. | Choice of primer set (e.g., V4 vs. V3-V4) influences taxonomic resolution and coverage. |
| Shotgun Metagenomics Kits | Enables comprehensive analysis of all genetic material, providing functional and taxonomic insights. | More expensive than 16S sequencing but allows strain-level and functional potential analysis. |
| Anaerobic Chamber Systems | Creates an oxygen-free environment for processing fecal samples and cultivating fastidious gut anaerobes. | Essential for maintaining the viability of oxygen-sensitive commensals for FMT and culture. |
| Targeted Metabolomics Panels | Quantifies specific classes of microbial metabolites (e.g., SCFAs, bile acids, tryptophan metabolites). | Provides functional readout of microbiome activity; links microbial taxa to host-physiological effects. |
| Germ-Free (Axenic) Mice | Serves as recipients for HMA studies, providing a vacant niche for human microbiota engraftment. | Gold-standard but costly; requires specialized isolator facilities for housing and breeding. |
| Antibiotic Cocktails | Used to deplete the indigenous microbiota, creating "pseudo-germ-free" mouse models. | A more accessible alternative to germ-free mice; regimen must be validated for efficacy. |
| Machine Learning Algorithms (e.g., LOCATE) | Integrates multi-omics data to predict host condition from microbiome-metabolome interactions. | Moves beyond correlation to identify latent representations predictive of health and disease [7]. |
The challenge of defining dysbiosis underscores a fundamental truth in microbiome science: health is not defined by a single microbial profile but by a community's functional capacity and resilience. While high microbial diversity is generally associated with health, the specific characteristics of a "healthy" microbiome remain elusive, as they are shaped by a complex interplay of host genetics, life stage, diet, and environmental exposures [3] [8]. The field is moving beyond simple taxonomic associations toward a functional understanding, leveraging multi-omics technologies and machine learning to decipher the complex interactions between microbes, their metabolites, and the host [7] [6]. Tools like LOCATE demonstrate that a latent representation of the microbiome-metabolome interaction can predict host condition more accurately than either dataset alone, offering a promising path forward [7].
Future research must focus on standardizing methodologies, as called for by the STORMS initiative, to improve reproducibility and cross-study comparisons [9]. Furthermore, establishing a universal healthy baseline may be less critical than understanding the ecological rules that govern microbiome stability and function. The integration of artificial intelligence with large-scale, longitudinal studies that capture the dynamic nature of the microbiome across diverse populations will be key to unraveling the context-dependent nature of dysbiosis and developing targeted, personalized microbial therapeutics.
In the realm of scientific research, particularly in the complex field of human microbiome studies, distinguishing between correlation and causation represents a critical intellectual challenge with profound implications for research validity and therapeutic development. Correlation describes a statistical association between variables—when one variable changes, so does the other. Causation, in contrast, means that changes in one variable directly bring about changes in another through a demonstrable cause-and-effect relationship [10]. While causation typically produces correlation, the reverse is not true; correlation does not imply causation [11] [12].
This distinction is especially crucial in microbiome research, where observational studies frequently identify microbial patterns associated with health and disease states. However, determining whether these microbial changes cause disease, result from disease, or merely coincide with disease processes remains methodologically challenging [13] [14]. The consequences of conflating these concepts can be significant, potentially leading to misdirected research resources, flawed therapeutic targets, and ineffective clinical interventions [11] [15]. This review examines the conceptual framework separating correlation from causation, explores experimental approaches for establishing causal relationships in microbiome research, and provides methodological guidance for researchers navigating this critical scientific distinction.
Table: Core Conceptual Differences Between Correlation and Causation
| Aspect | Correlation | Causation |
|---|---|---|
| Definition | Statistical association between variables | One variable directly causes changes in another |
| Temporal requirement | None | Cause must precede effect |
| Evidence required | Statistical covariance | Controlled experiments + covariance + elimination of alternatives |
| Implied mechanism | None | Direct mechanistic link |
| Common in | Observational studies | Randomized controlled trials |
The Critical Distinction: Why Correlation Does Not Imply Causation
The maxim "correlation does not imply causation" represents a fundamental principle in scientific reasoning, yet its violation remains commonplace in research interpretation. Two primary problems explain why correlated variables may not be causally related: the third variable problem and the directionality problem [10].
The third variable problem (also known as confounding) occurs when an unaccounted external factor affects both variables being studied, creating a spurious association. A classic example involves ice cream sales and crime rates, which correlate positively but are not causally connected; instead, hot weather influences both variables independently [11] [12]. In microbiome research, numerous confounding variables can create illusory associations, including diet, medications, age, and genetic factors that independently affect both microbial composition and health outcomes [16] [15].
The directionality problem arises when two variables correlate and may indeed have a causal relationship, but determining which variable influences the other proves impossible from the correlation alone. For example, studies have identified correlations between vitamin D levels and depression, but determining whether low vitamin D causes depression or whether depression leads to reduced vitamin D intake remains challenging without experimental manipulation [10]. In microbiome-disease associations, this ambiguity is particularly salient—does microbial dysbiosis cause disease pathology, or does established disease create an environment that favors dysbiosis? [13] [17]
Table: Common Challenges in Establishing Causality in Microbiome Research
| Challenge | Description | Impact on Causal Inference |
|---|---|---|
| Confounding variables | Unmeasured factors (diet, medications, genetics) affecting both microbiome and health | Creates spurious associations between specific microbes and diseases |
| Technical variability | Differences in DNA extraction, sequencing technologies, and bioinformatics across labs [15] | Reduces reproducibility and consistency of microbial signatures |
| Population homogeneity | Over-reliance on white, affluent populations in microbiome studies [15] | Limits generalizability of findings to diverse populations |
| Microbial community complexity | Thousands of interacting microbial species and strains | Difficult to isolate effects of individual microbial taxa |
Establishing Causality: Experimental Approaches in Microbiome Research
Moving from correlational observations to causal conclusions requires specific experimental approaches that can test and verify hypothesized cause-effect relationships. In microbiome research, this typically involves a multi-stage "funnel" approach that progresses from broad associations to increasingly precise mechanistic investigations [13].
The Causal Funnel: From Associations to Molecular Mechanisms
Research to establish microbiome-disease causality often follows a sequential pathway of evidence generation [13]:
- Level 1: Associations - Observational studies identify microorganisms statistically associated with diseased versus healthy individuals using sequencing technologies.
- Level 2: Altered phenotypes in microbiome-depleted models - Studies in germ-free animals or antibiotic-treated organisms demonstrate that microbes play causal roles in disease pathophysiology.
- Level 3: Phenotype transfer via fecal microbiota transplants (FMT) - Transfer of microbial communities from diseased donors to recipient animals establishes whether disease phenotypes can be transmitted through microbiota.
- Level 4: Microbial strain effects - Identification of specific microbial strains that produce disease-associated phenotypes.
- Level 5: Molecular mechanisms - Identification and functional testing of microbially produced molecules that elicit host phenotypes.
This progressive approach enables researchers to narrow candidate causal factors from entire microbial communities to specific strains and eventually to precise molecular mechanisms [13].
Key Experimental Models for Establishing Causality
Different experimental models offer distinct advantages and limitations for establishing causal relationships in microbiome research:
Germ-free animals represent a gold standard model, maintained in completely sterile conditions without any microorganisms. These models allow precise introduction of specific microbial communities or individual strains to test their causal effects on host physiology [13] [17]. However, germ-free animals exhibit physiological abnormalities, including underdeveloped immune systems, which may limit translational relevance [17].
Antibiotic-induced microbiota depletion provides a more accessible alternative to germ-free models, using broad-spectrum antibiotics to substantially reduce endogenous microbial taxa. While more practical and cost-effective, this approach cannot eliminate all intestinal microbes and may have off-target drug effects that complicate interpretation [17].
Human microbiota-associated (HMA) animal models involve transferring fecal microbiota from human donors to germ-free animals, creating "humanized" models that reflect human microbial ecosystems. These models have successfully transferred various human disease phenotypes, including obesity, inflammatory bowel disease, and malnourishment [14] [17].
Microbiome Causality Research Funnel
Methodological Framework: Protocols for Causal Inference
Experimental Workflows for Establishing Causality
Several well-established experimental protocols enable researchers to move from correlation to causation in microbiome studies. These methodologies provide structured approaches to test causal hypotheses and eliminate alternative explanations for observed associations.
Fecal Microbiota Transplantation (FMT) protocols involve transferring minimally manipulated microbial communities from donor fecal or cecal matter to recipient animals [17]. Donor inoculum can be prepared fresh or frozen with cryoprotectants, with administration varying from single to multiple gavage cycles. Recipients typically include germ-free mice or conventionally raised mice with antibiotic-induced microbiota depletion. Successful FMT experiments have transferred numerous human disease phenotypes to animal models, providing strong evidence for microbial causality in conditions ranging from metabolic disorders to neurological conditions [13] [17].
Gnotobiotic models involve colonizing germ-free animals with defined microbial communities, ranging from single bacterial strains (monocolonization) to simplified synthetic communities. This approach allows researchers to test the specific effects of individual microbial taxa on host phenotypes while controlling for broader community context [13] [14].
Longitudinal studies track variables over extended time periods, establishing temporal precedence required for causal inference—the cause must precede the effect [12]. In microbiome research, longitudinal sampling can determine whether microbial changes precede disease onset or follow it, helping resolve directionality questions in observed correlations [15].
Causal Inference Experimental Workflow
Causal Inference Methods Beyond Traditional Experimentation
When controlled experiments are not feasible due to ethical, financial, or practical constraints, researchers increasingly turn to advanced causal inference methods from econometrics and machine learning [16]:
Double Machine Learning (Double ML) uses flexible ML models to control for high-dimensional confounders in microbiome-disease associations, providing robust effect estimates even with many potential confounding variables [16].
Instrumental Variables (IV) approaches, including Mendelian randomization, use genetic variants as natural experiments to test causal relationships while minimizing confounding [16] [18].
Difference-in-Differences (DiD) designs compare outcomes over time between groups exposed and unexposed to a putative causal factor, helping isolate causal effects from secular trends [16].
These methodological advances enable more rigorous causal claims from observational data, though they typically require stronger assumptions than randomized experiments.
Table: Comparison of Causal Inference Methodologies
| Method | Key Principle | Strengths | Limitations |
|---|---|---|---|
| Randomized Controlled Trials | Random assignment to treatment/control groups | Gold standard for causal inference; minimizes confounding | Often infeasible for microbiome interventions; ethical constraints |
| Germ-free animal models | Complete absence of microbiota; controlled microbial introduction | Maximum control over microbial variables; establishes causality | Physiological abnormalities; limited translational relevance |
| Double Machine Learning | Uses ML to control for high-dimensional confounders | Handles complex, high-dimensional data; robust to confounding | Requires large sample sizes; complex implementation |
| Mendelian Randomization | Uses genetic variants as instrumental variables | Minimizes confounding; exploits natural variation | Requires specific genetic assumptions; limited to modifiable exposures |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successfully navigating from correlation to causation in microbiome research requires specific experimental tools and reagents. The following table outlines essential materials for conducting causal investigations in microbiome science.
Table: Essential Research Reagents for Microbiome Causal Studies
| Reagent/Material | Function | Application Context |
|---|---|---|
| Germ-free animals | Provide microbiologically sterile hosts for controlled colonization | Causal testing of specific microbial strains/communities without background microbiota interference |
| Antibiotic cocktails (e.g., ampicillin, vancomycin, neomycin, metronidazole) | Deplete endogenous microbiota in conventional animals | Create microbiota-reduced models for FMT studies; test microbiota-dependent phenotypes |
| Cryoprotectants (e.g., glycerol) | Preserve microbial viability during frozen storage | Maintain complex microbial community structure in frozen FMT inocula |
| Gnotobiotic isolators | Maintain sterile housing conditions for germ-free animals | Prevent microbial contamination during long-term germ-free animal studies |
| Defined microbial communities | Simplified, reproducible microbial consortia | Test specific microbial combinations in gnotobiotic models; reduce complexity of natural communities |
| Organoid/ gut-on-a-chip systems | Replicate human intestinal microenvironment ex vivo | Study host-microbe interactions in human-derived systems with environmental control |
| Multi-omics platforms (genomics, transcriptomics, metabolomics) | Comprehensive molecular profiling | Identify mechanistic pathways linking microbes to host phenotypes |
Establishing causal relationships between the microbiome and human health represents a fundamental challenge with significant implications for therapeutic development and clinical practice. While correlational studies using high-throughput sequencing technologies have identified numerous associations between microbial patterns and disease states, translating these observations into validated causal mechanisms requires rigorous experimental approaches including germ-free models, fecal microbiota transplantation, gnotobiotic systems, and molecular mechanistic studies. The emerging integration of causal inference methods from econometrics and machine learning offers promising approaches for strengthening causal claims, particularly when traditional randomized experiments are not feasible. By systematically applying these methodological frameworks and maintaining distinction between correlational and causal evidence, researchers can advance the field from associative observations to validated mechanistic insights that support targeted therapeutic interventions.
Fecal Microbiota Transplantation (FMT) represents a paradigm shift in the treatment of recurrent Clostridioides difficile infection (rCDI) and establishes a foundational model for establishing causality in microbiome research. Unlike correlative studies, FMT provides direct experimental evidence that restoring a healthy gut microbiota can resolve a specific disease state. This review synthesizes clinical efficacy data, elucidates the mechanistic pathways validated through FMT interventions, and details the standardized protocols that have established FMT as both a therapeutic breakthrough and a powerful scientific tool for deconvoluting host-microbiome interactions. The lessons learned from FMT in rCDI provide a rigorous framework for evaluating microbiome-based therapies in other disease contexts.
The human gut microbiome has been correlated with numerous health and disease states, but proving causal relationships remains a central challenge. FMT's success in rCDI provides one of the clearest examples of a causal link between microbial ecology and human disease. Where observational studies can only identify associations, FMT interventions function as definitive experiments that test the hypothesis that microbial dysbiosis is a principal factor in disease pathogenesis. The restoration of a healthy microbial community leads to resolution of rCDI, demonstrating that microbial ecology is not merely a consequence but a driver of disease. This established causal relationship offers a template for investigating other conditions where dysbiosis is implicated, from inflammatory bowel disease to metabolic and neurological disorders.
Clinical Efficacy: Quantitative Data Establishing the Standard
Robust clinical trials and meta-analyses have consistently demonstrated the superior efficacy of FMT over standard antibiotic therapy for rCDI, transforming clinical practice and validating the causal role of dysbiosis.
Comparative Efficacy of FMT vs. Standard Therapies
Table 1: Clinical Efficacy of FMT for Recurrent CDI from Systematic Reviews
| Comparison | Clinical Cure / Resolution Rate | Source Study Details |
|---|---|---|
| FMT (pooled across routes) | 70% to 91% [19] | Systematic review of 7 studies (N=1,030 patients) [19] |
| Vancomycin (standard therapy) | 19% [19] | Direct comparative data from RCTs [19] |
| Fidaxomicin (standard therapy) | 33% [19] | Direct comparative data from RCTs [19] |
| Donor FMT vs. Autologous FMT | 90.9% vs. 62.5% (p=0.042) [19] | Highlights superiority of healthy donor microbiota [19] |
| Single FMT in Immunocompromised | 75.3% (95% CI, 71.7%-78.6%) [20] | Meta-analysis of 44 studies in high-risk patients [20] |
| Consecutive FMT in Immunocompromised | 87.4% (95% CI, 84.8%-89.6%) [20] | Demonstrates efficacy can be enhanced with repeated treatment [20] |
Standardized, FDA-Approved Microbiota-Based Therapeutics
The clinical success of conventional FMT has spurred the development of standardized, quality-controlled products.
- Rebyota (fecal microbiota, live-jslm): A single-dose, rectally administered suspension derived from donor stool. Clinical trials demonstrated a success rate of approximately 70% at 8 weeks, with a sustained clinical response of ~90% at 6 months in initial responders. Each enema contains a diverse community of microorganisms, with a high percentage of Bacteroides (> 1x10^5 CFU/cc) [21].
- Vowst (fecal microbiota spores, live-brpk): An orally administered, FDA-approved product consisting of spore-based microbiota [22].
These products offer a more standardized and scalable approach compared to conventional FMT, though with comparable high efficacy, further validating the principle of microbiota restoration [21] [22].
Elucidating Causal Mechanisms: From Correlation to Pathophysiology
The therapeutic effect of FMT in rCDI is not merely a black box; research has illuminated specific mechanistic pathways that explain its success, providing a model for how to connect microbial shifts to host physiology.
Restoration of Colonization Resistance
A healthy, diverse gut microbiota provides colonization resistance, which prevents C. difficile spores from germinating and proliferating. Antibiotics disrupt this protective ecosystem, creating an opportunity for C. difficile to establish an infection. FMT directly reverses this by re-introducing a complex microbial community that outcompetes the pathogen for nutrients and ecological niches [22].
Modulation of Bile Acid Metabolism
This is one of the most precisely elucidated causal pathways.
- Primary bile acids (e.g., cholic acid, chenodeoxycholic acid) promote the germination of C. difficile spores into vegetative, toxin-producing cells [22].
- Secondary bile acids (e.g., deoxycholate, lithocholate) inhibit C. difficile germination and growth [22].
- A healthy gut microbiota, particularly specific members of the phylum Firmicutes, performs 7-alpha-dehydroxylation, converting primary bile acids to secondary bile acids. rCDI is characterized by a depletion of these key bacteria. FMT restores the microbial consortia necessary for this critical biotransformation, re-establishing an inhibitory environment for C. difficile [22].
Production of Protective Metabolites
- Short-Chain Fatty Acids (SCFAs): Beneficial bacteria in a restored microbiome produce SCFAs like butyrate. Butyrate has multiple protective roles: it inhibits C. difficile growth, promotes the conversion of primary to secondary bile acids, and supports immune modulation and intestinal barrier integrity [22].
The following diagram synthesizes these core mechanisms into a unified pathway of how FMT treats rCDI.
The Scientist's Toolkit: Protocols and Reagents for FMT Research
The translational success of FMT relies on rigorous, reproducible protocols for donor screening, material preparation, and administration.
Key Research Reagent Solutions
Table 2: Essential Materials and Reagents for FMT Studies
| Item / Reagent | Function / Application | Key Considerations & Examples |
|---|---|---|
| Donor Screening Panels | Ensures safety of fecal material by excluding pathogens. | Comprehensive serologic and stool testing for viruses (HIV, Hepatitis), bacteria (C. difficile, Salmonella), parasites [23] [24] [22]. |
| Anaerobic Stool Processing Equipment | Maintains viability of oxygen-sensitive commensal bacteria during preparation. | Automated mixing/filtering systems; work performed in anaerobic chambers or biological safety cabinets [23]. |
| Cryopreservation Solutions | Enables long-term storage of prepared FMT material. | Final concentration of 10% glycerol; storage at -80°C [23]. |
| Placebo Materials | Serves as a control in blinded clinical trials. | Isotonic saline is commonly used as an inert placebo for enemas [24]. |
| DNA Extraction Kits | For microbial genomic DNA extraction from stool pre- and post-FMT. | e.g., PowerMax Extraction Kit; enables 16S rRNA gene sequencing and shotgun metagenomics to assess engraftment [23] [25]. |
Detailed Experimental Methodology
The following diagram outlines a standardized workflow for an FMT clinical trial, from donor to data analysis.
FMT's success in rCDI provides an unparalleled evidence-based framework for establishing causality in microbiome research. It demonstrates that a defined intervention (transplantation of healthy microbiota) leads to a specific phenotypic reversal (resolution of infection) through elucidated mechanisms (bile acid metabolism, SCFA production, colonization resistance). This end-to-end validation, from correlation to mechanistic understanding, sets the "gold standard" that research into other microbiome-associated conditions should strive to emulate. Future work will focus on refining standardized products, identifying key therapeutic consortia within the microbiota, and applying this causal framework to more complex, non-infectious diseases linked to the gut-brain axis, metabolism, and immunity.
The human gut microbiome, a complex ecosystem of trillions of microorganisms, plays an indispensable role in maintaining host health by regulating immune homeostasis, supporting metabolic functions, and protecting against pathogens. Dysbiosis—an imbalance in this microbial community—has been increasingly implicated in the pathogenesis of diverse diseases, including metabolic disorders, inflammatory bowel disease (IBD), and gastrointestinal cancers [26] [27]. The relationship between microbial shifts and disease is not merely correlative; emerging evidence from animal and human studies demonstrates that specific microbial alterations can directly influence disease pathways through metabolic outputs, immune modulation, and host-microbe co-metabolism [28] [29]. This review synthesizes evidence from recent research to objectively compare the microbial and metabolic signatures associated with these conditions, supported by experimental data and the methodologies used to generate them.
Comparative Analysis of Microbial and Metabolic Signatures Across Diseases
The following sections and tables summarize the key microbial shifts and functional consequences observed in metabolic disorders, IBD, and cancer, providing a side-by-side comparison for researchers.
Table 1: Key Microbial Taxa and Functional Shifts in Metabolic Disorders, IBD, and Cancer
| Disease Category | Key Microbial Shifts (Abundance) | Associated Functional & Metabolic Consequences | Supporting Experimental Models |
|---|---|---|---|
| Metabolic Disorders (Obesity, T2D, NAFLD) | ↑ Firmicutes/Bacteroidetes (F/B) ratio [30]↓ Akkermansia muciniphila [30]↓ Bifidobacterium spp. [30]↓ Butyrate producers (Faecalibacterium prausnitzii, Roseburia) [30] | Reduced SCFA production [30]Increased intestinal permeability & metabolic endotoxemia [30]Disrupted bile acid metabolism [30]Altered linoleic acid metabolism (aged models) [5] | Human cohort studies [30]Conventional vs. Germ-Free (GF) mice [5]Fecal Microbiota Transplantation (FMT) in mice [4] |
| Inflammatory Bowel Disease (IBD) | ↑ Escherichia coli, Klebsiella [27]↑ Ruminococcus gnavus [27]↓ Faecalibacterium prausnitzii [26] [27]↓ Roseburia hominis [27]↓ SCFA producers (Lachnospiraceae, Ruminococcaceae) [27] | Reduced SCFAs (butyrate) [31] [28]Altered tryptophan metabolism & NAD+ biosynthesis [26] [28]Dysregulated sulfur metabolism & bile acid conversion [28]Increased oxidative stress pathways [27] | Human longitudinal IBD cohorts [28]Human Microbiota-Associated (HMA) mouse models [4] [29]Genome-scale metabolic modeling (coralME) [31] |
| Gastrointestinal Cancers (e.g., Colorectal Cancer - CRC) | ↑ Fusobacterium [32] [27]↑ Bacteroides & Prevotella [32]↓ Lactobacillus [32]↓ Faecalibacterium [32] | Production of oncogenic metabolites (e.g., H2S, secondary bile acids) [32]Disrupted lipid & amino acid metabolism [32]Increased inflammation & immune suppression [32] | Human case-control studies [32] [27]Machine learning models on human microbiomes [32] |
Table 2: Key Pathogenic Mechanisms and Microbial Metabolites in GI Diseases
| Mechanism/Metabolite | Role in Disease Pathogenesis | Associated Diseases |
|---|---|---|
| Reduced Short-Chain Fatty Acids (SCFAs) | Loss of anti-inflammatory properties, impaired gut barrier integrity, and dysregulated immune cell differentiation [26] [28]. | IBD [31] [28], Metabolic Disorders [30] |
| Altered Tryptophan Metabolism | Depletion of host tryptophan, disruption of NAD+ biosynthesis, and heightened intestinal inflammation [26] [28]. | IBD [26] [28] |
| Bile Acid Dysregulation | Altered primary-to-secondary bile acid ratios promote inflammation and disrupt immune signaling [28] [27]. | IBD [28], Metabolic Disorders [30] |
| Virulence Factors & Pathobionts | Toxins (e.g., ETEC's LT/ST, CPE) compromise intestinal tight junctions, increasing permeability and inflammation [27]. | IBD [27] |
| Shift to Aerotolerance | Inflammation-driven oxidative stress favors pro-inflammatory aerotolerant bacteria over obligate anaerobes [27]. | IBD [27] |
Experimental Protocols and Methodologies for Microbiome-Disease Research
A critical component of linking microbes to disease is the use of robust and reproducible experimental models. Below are detailed methodologies for key approaches cited in this field.
Establishment of Human Microbiota-Associated (HMA) Mouse Models
HMA models are indispensable for investigating causal relationships between the human microbiome and host physiology [4].
1. Donor Screening and Fecal Sample Collection:
- Donor Criteria: Healthy donors are typically screened for the absence of gastrointestinal disorders, no recent (1-12 months) antibiotic or laxative use, and a balanced omnivorous diet. Donors with neuropsychiatric disorders, excessive alcohol use, or smoking are often excluded [4].
- Sample Processing: Fecal samples are collected anaerobically and processed immediately, or preserved with cryoprotectants at low temperatures to maintain microbial viability. Samples are diluted, homogenized, and filtered under anaerobic conditions to create a standardized fecal suspension [4].
2. Recipient Preparation and Fecal Microbiota Transplantation (FMT):
- Recipient Animals: Germ-free (GF) mice are the gold standard. Alternatively, pseudo-germ-free mice are created by depleting indigenous microbiota with antibiotic cocktails [4].
- Transplantation Protocol: A single gavage of the fecal suspension is often sufficient for colonization, but multiple gavages over a longer duration significantly improve the engraftment efficiency of the donor microbiota [4].
3. Engraftment Validation:
- Microbial community profiling via 16S rRNA gene sequencing is the primary method to confirm that the recipient's microbiome successfully mirrors the donor's profile [4].
Genome-Scale Metabolic Modeling (e.g., coralME tool)
Computational models like coralME translate genetic data into predictive models of microbial community behavior [31].
- Model Reconstruction: The tool rapidly generates ME-models (models of metabolism, gene, and protein expression) from large omics datasets, linking a microbe's genome to its phenotypic attributes [31].
- Simulation and Prediction: These models can simulate how microbes respond to different nutrients, predict the formation of undesired metabolites (e.g., toxins), and uncover how microbes interact with each other and the host [31].
- Application: For instance, researchers used coralME to generate 495 models of common gut species and simulated the effects of low-iron or low-zinc diets, revealing survival advantages for certain harmful bacteria that traditional models missed [31]. Inputting data from IBD patients allowed the models to reveal real-time microbial activities, such as decreased production of protective short-chain fatty acids and shifts in gut pH [31].
Machine Learning for Cross-Disease Biomarker Prediction
Advanced computational methods are used to identify and validate microbial and metabolic biomarkers across different gastrointestinal diseases (GIDs) [32].
- Data Preprocessing: Sparse features are removed from microbiome and metabolome datasets. The remaining data is normalized (e.g., min-max scaling) to ensure all features contribute equally to the model [32].
- Model Training and Feature Selection: Multiple algorithms, including Random Forest, XGBoost, and LASSO regression, are trained on datasets from specific diseases (e.g., Gastric Cancer (GC), IBD, CRC). These models identify the most significant microbial and metabolite features that distinguish diseased from healthy states [32].
- Cross-Disease Prediction: Models trained on one disease's biomarkers are used to predict another. For example, a model trained on GC data has successfully predicted IBD biomarkers, and a CRC model has predicted GC biomarkers, highlighting shared pathogenic mechanisms across GIDs [32].
Visualization of Key Pathways and Workflows
Tryptophan-NAD+ Pathway Disruption in IBD
The following diagram illustrates the host-microbiome metabolic disruption in tryptophan and NAD+ metabolism, a key pathway identified in IBD studies [28].
Host-Microbiome Metabolic Disruption in IBD. This diagram illustrates how inflammation in IBD drives host tryptophan depletion via the kynurenine pathway, impairing NAD+ biosynthesis. Concurrently, the microbiome shows reduced production of nicotinic acid, a key NAD+ precursor, exacerbating the metabolic deficit [28].
Workflow for Human Microbiota-Associated (HMA) Model Generation
This flowchart outlines the general procedure for creating HMA mouse models, a cornerstone of causal microbiome research [4].
HMA Mouse Model Generation Workflow. The process involves stringent donor screening, anaerobic processing of fecal samples, preparation of germ-free or antibiotic-treated recipient mice, FMT via gavage, and final validation of microbiota engraftment using sequencing [4].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for Microbiome-Disease Investigations
| Reagent / Solution | Function in Research | Specific Application Example |
|---|---|---|
| Gnotobiotic Animal Models | Provides a controlled environment free of unknown microbes to study causality of transplanted human microbiota [4]. | Establishing HMA mice to test the inflammatory potential of donor microbiomes from IBD patients [4] [29]. |
| Antibiotic Cocktails | Depletes the native gut microbiota of conventional animals, creating "pseudo-germ-free" recipients for FMT studies [4]. | Preparing recipient mice for FMT to improve engraftment of donor microbiota [4]. |
| Cryoprotectants (e.g., Glycerol) | Preserves microbial viability during long-term storage of fecal samples at low temperatures [4]. | Maintaining integrity of donor fecal samples for later processing and FMT. |
| Anaerobic Chamber/Workstation | Creates an oxygen-free environment for processing fecal samples and preparing fecal suspensions to protect obligate anaerobic bacteria [4]. | Essential for the preparation of high-viability fecal suspensions for FMT. |
| 16S rRNA Sequencing Kits | Enables taxonomic profiling of microbial communities to assess composition and diversity [4] [27]. | Validating engraftment in HMA models and characterizing dysbiotic signatures in patient cohorts [4] [32]. |
| Shotgun Metagenomics Kits | Allows for strain-level identification and functional gene profiling of the entire microbiome [27]. | Analyzing shifts in metabolic pathways (e.g., SCFA synthesis) in disease states [28] [27]. |
| Metabolomics Kits & Standards | Facilitates the identification and quantification of metabolites (e.g., SCFAs, bile acids, tryptophan metabolites) in host samples [28] [5]. | Correlating microbial shifts with functional metabolic outputs in disease [28] [5]. |
The convergence of evidence from human studies, animal models, and advanced computational tools solidifies the role of specific microbial shifts in the pathogenesis of metabolic disorders, IBD, and cancer. While each disease exhibits a distinct microbial signature, common themes emerge, such as the loss of key commensal taxa, a decline in protective SCFA production, and dysregulation of host-microbiome co-metabolism in pathways involving amino acids and lipids. The translation of these findings from correlation to causation relies heavily on robust experimental models like HMA mice and genome-scale metabolic modeling. As these tools and datasets continue to mature, the path forward lies in leveraging this knowledge for precise diagnostics and targeted, microbiome-based therapeutics, ultimately paving the way for personalized medicine approaches in these complex diseases.
The field of microbiome therapeutics has evolved from a scientific curiosity to a rapidly expanding frontier in drug development. With over 180 drugs currently in development across more than 140 companies, this sector represents one of the most innovative areas in biopharmaceutical research. The market is projected to grow from approximately $791 million in 2025 to $6.09 billion by 2035, reflecting a compound annual growth rate of 20.4% [33]. This growth is fueled by a deeper understanding of the human microbiome's profound influence on various biological processes and the recognition that unlike many host determinants, it represents a readily accessible target for manipulation to promote health benefits [34]. This review provides a comprehensive overview of the current microbiome therapeutic pipeline, examines the critical role of animal models in translating these discoveries to human applications, and details the experimental methodologies advancing this promising field.
The Microbiome Therapeutic Pipeline: A Quantitative Landscape
The microbiome therapeutic landscape has expanded dramatically, characterized by diverse modalities targeting a broad spectrum of diseases.
Table 1: Microbiome Therapeutics Pipeline Overview (2025)
| Development Stage | Number of Candidates | Representative Examples | Key Indications |
|---|---|---|---|
| Preclinical & Discovery | ~60% (≈108 drugs) | SNIPR001 (SNIPR Biome), Kanvas Biosciences programs | IBD, Immuno-oncology, various [35] [36] |
| Phase I Trials | ~20% (≈36 drugs) | EO2463 (Enterome), SER-155 (Seres Therapeutics) | Non-Hodgkin Lymphoma, Sepsis [37] [36] |
| Phase II Trials | ~15% (≈27 drugs) | VE202 (Vedanta Biosciences), ST-598 (Siolta Therapeutics) | Ulcerative Colitis, Allergy Prevention [35] |
| Phase III Trials | <5% (≈9 drugs) | VE303 (Vedanta Biosciences), MaaT013 (MaaT Pharma) | rCDI, Graft-vs-Host Disease [34] [35] [36] |
| Approved Drugs | 2 (FDA) | Rebyota (Ferring/Rebiotix), Vowst (Seres Therapeutics) | Recurrent C. difficile Infection [35] |
Table 2: Segmentation by Therapeutic Modality
| Modality | Mechanism of Action | Advantages | Limitations | Example Candidates |
|---|---|---|---|---|
| Fecal Microbiota Transplantation (FMT) & Derivatives | Transfer of complete or processed microbial communities from healthy donors | High efficacy in rCDI (>80%), holistic ecological approach [34] | Donor variability, pathogen transmission risk, manufacturing complexity [35] | Rebyota (approved), MaaT013 (Phase III) [35] |
| Defined Microbial Consortia | Rationally selected bacterial communities ("bottom-up") | Controlled composition, reproducible manufacturing, improved safety [34] [35] | May lack ecological complexity of full microbiota, challenging engraftment [34] | VE303 (Phase III), VE202 (Phase II) [34] [35] |
| Single-Strain Live Biotherapeutic Products (LBPs) | Single bacterial strain with defined pharmacological activity | Simple manufacturing, clear mechanism of action [34] | May not address complex dysbiosis, limited functional breadth | IBP-9414 (IBT), EXL01 (Exeliom) [37] |
| Engineered Microbes & Phages | Genetically modified bacteria or bacteriophages for precise targeting | High specificity, ability to deliver therapeutic payloads [37] [38] | Regulatory hurdles for GMOs, potential immune responses | SYNB1934 (Synlogic), Eligobiotics (Eligo Bioscience) [37] [35] |
The pipeline demonstrates significant clinical diversification. While recurrent Clostridioides difficile infection (rCDI) was the initial focus, developers are now actively targeting inflammatory bowel disease (IBD), metabolic disorders, autoimmune diseases, cancer, and neurological conditions [35]. Over 70 companies worldwide are engaged in developing therapies that manipulate the human microbiome [33].
The Scientist's Toolkit: Essential Reagents and Research Solutions
Advancing microbiome therapeutics requires specialized tools and reagents. The following table details key resources essential for research and development in this field.
Table 3: Essential Research Reagent Solutions for Microbiome Therapeutics Development
| Research Reagent / Solution | Primary Function | Application in Microbiome Research |
|---|---|---|
| 16S rRNA Gene Sequencing Reagents | Amplification and sequencing of the bacterial 16S rRNA gene for taxonomic identification [39] | Profiling microbial community composition and diversity in fecal samples, tissue biopsies, and in vitro cultures [39] |
| Anaerobic Chamber Systems | Creation of oxygen-free environment for processing and culturing obligate anaerobic gut bacteria [4] | Preservation of microbial viability during fecal sample processing and cultivation of fastidious anaerobic species for LBPs [4] |
| Cryopreservation Protectants (e.g., Glycerol) | Protect bacterial cells from damage during freezing and thawing [4] | Long-term storage of donor fecal samples, defined microbial consortia, and single-strain LBPs while maintaining viability [4] |
| Germ-Free (Gnotobiotic) Animal Models | Animals devoid of any microorganisms, serving as a "blank slate" for microbial colonization studies [39] [40] | Investigating causal microbe-host interactions by colonizing with human-derived microbiota or specific bacterial strains [4] [40] |
| Multi-Omics Kits (Metagenomics, Metatranscriptomics, Metaproteomics, Metabolomics) | Comprehensive profiling of microbial genes, gene expression, proteins, and metabolites [41] | Understanding functional dynamics of the microbiome and mechanistic effects of therapeutic interventions [41] |
| Gnotobiotic Isolators | Sterile housing systems that maintain germ-free status or defined microbial status of animals [40] | Maintaining the integrity of Human Microbiota-Associated (HMA) animal models during long-term studies [4] [40] |
Experimental Models: Bridging the Gap from Animal Models to Human Trials
A critical challenge in microbiome research is the translatability of findings from animal models to human clinical trials. Human Microbiota-Associated (HMA) mouse models, established by transplanting human fecal microbiota into germ-free mice, have become an indispensable tool for investigating microbe-host interactions and disease pathogenesis [4].
Diagram 1: HMA Model Workflow for Therapeutic Development. This workflow outlines the critical steps in creating humanized gnotobiotic mouse models for microbiome therapeutic research, from donor screening to therapeutic translation.
Detailed Protocol: Establishing a Human Microbiota-Associated (HMA) Mouse Model
The establishment of a reproducible HMA model requires meticulous attention to donor selection, sample processing, and transplantation protocols [4] [40].
Donor Screening and Selection Criteria
- Inclusion Criteria: Healthy donors typically require a minimum of 2-12 months without antibiotic exposure, elimination of laxative agents for ≥3 months, an omnivorous diet, and absence of gastrointestinal disorders or recent pathogen infections [4].
- Exclusion Criteria: Common exclusions include recent exposure to antimicrobials, prebiotics, or probiotics (within 1-2 months), active neuropsychiatric disorders, excessive alcoholism or smoking habits, and pregnancy or lactation [4].
- Special Considerations: Donor diet, exercise, geographical origin, and ethnicity significantly influence gut microbiota composition and must be documented, as they affect the translatability of findings [40].
Fecal Sample Processing and Preservation
- Collection: Fecal samples should be collected anaerobically and processed immediately after passage to preserve viability of oxygen-sensitive commensals [4].
- Homogenization: Suspend fecal material in anaerobic, reduced PBS or similar buffer (typically 1:5-1:10 weight/volume) under anaerobic conditions [4].
- Filtration: Remove large particulate matter by filtration through sterile mesh (e.g., 100-500 μm) [4].
- Preservation: If not used immediately, add cryoprotectants (e.g., 10-15% glycerol) and store at -80°C or in liquid nitrogen. Multiple freeze-thaw cycles should be avoided [4].
Recipient Preparation and Fecal Microbiota Transplantation (FMT)
- Recipient Models: Two primary options exist:
- Transplantation Protocol:
- Administration Route: Oral gavage is most common, but rectal installation is also used.
- Dosing Regimen: While a single gavage can establish colonization, multiple administrations (e.g., 3 times per week for 2-3 weeks) significantly improve donor microbiota engraftment efficiency [4].
- Post-FMT Monitoring: Allow 1-2 weeks for stable microbial ecosystem establishment before initiating experimental interventions.
Engraftment Validation
- 16S rRNA Gene Sequencing: The primary method for analyzing microbiome composition and verifying donor microbiota engraftment [4].
- Functional Metagenomics: Assess the functional potential of the transplanted microbiota [41].
- Metabolomic Profiling: Validate functional engraftment through analysis of microbially-derived metabolites (e.g., short-chain fatty acids) in recipient feces and serum [41].
Correlation Between Animal Model and Human Study Findings
The predictive value of animal models for human outcomes remains a central consideration in microbiome therapeutic development. Key findings and challenges include:
Successful Correlations: The high success rate of FMT for rCDI in humans (>80%) was reflected in animal studies, validating the model's predictive capability for this indication [34]. Similarly, studies using HMA models have successfully recapitulated human metabolic phenotypes, such as the transfer of lean and obese phenotypes through microbiota transplantation [40].
Limitations and Disconnects: Significant differences exist between mouse and human microbiota. Despite an 89% similarity in overall bacterial genera between clean laboratory mice and humans, a number of human-specific genera are completely absent in mice, including ones linked to gut health in humans [39]. Furthermore, germ-free mice have substantial physiological differences in their gastrointestinal tracts, including fewer Peyer's patches, smaller mesenteric lymph nodes, and reduced production of secretory IgA, which must be considered when interpreting results [39].
Standardization Challenges: Inadequate standardization in creating HMA models across research groups poses significant constraints on the effective translatability of the system [40]. Variations in donor selection, fecal processing methods, recipient mouse strain, and housing conditions can all influence experimental outcomes and reproducibility [39] [4].
Diagram 2: Iterative Research Framework for Microbiome Therapeutics. This framework illustrates the multi-stage approach recommended for translating correlational findings into successful clinical applications, emphasizing the iterative refinement process based on clinical feedback.
The pipeline of over 180 microbiome drugs in development reflects a field rich with innovation and potential. The progression from broad-spectrum FMT to precisely defined microbial consortia and engineered live biotherapeutics represents a maturation of the entire sector. The continued refinement of HMA animal models and standardized experimental protocols will be crucial for enhancing the translatability of preclinical findings to human applications. As these therapeutic candidates advance through clinical trials, they hold the promise of addressing not only gastrointestinal disorders but also a wide range of systemic conditions, fundamentally expanding our approach to disease treatment and prevention.
A Researcher's Toolkit: Experimental Models for Host-Microbiome Interaction Studies
In the investigation of host-microbe interactions, a fundamental challenge persists: distinguishing mere correlation from true causation. While large-scale sequencing and multi-omics approaches can identify microbial associations with health and disease, they fall short of proving mechanistic causality [41]. Germ-free (GF) animal models have therefore become indispensable tools, providing a controlled "blank slate" for rigorously testing hypotheses about microbiome function. These animals, completely devoid of all living microorganisms, allow researchers to dissect the specific contributions of microbiota to physiology and disease pathogenesis with a precision unmatched by other models [42] [43].
The value of GF models lies in their unique experimental flexibility. By maintaining animals in sterile isolators and then introducing defined microbial communities, scientists can move beyond observation to direct experimentation [44]. This approach has revealed the profound influence of gut microbiota on diverse bodily systems, including immune development, metabolic function, and even brain behavior through the gut-brain axis [43]. As microbiome research transitions from correlational findings to therapeutic applications, GF animals provide the critical experimental platform needed to validate causal links and advance our understanding of microbiome-based interventions.
Germ-Free vs. Antibiotic-Treated Models: A Comparative Analysis
Two primary approaches are used to study microbiota depletion in animal models: isolated germ-free systems and antibiotic-treated models. Each method offers distinct advantages and limitations, making them suitable for different research applications.
Table 1: Comparison of Germ-Free and Antibiotic-Treated Animal Models
| Characteristic | Germ-Free Models | Antibiotic-Treated Models |
|---|---|---|
| Microbial Status | Complete absence of all living microorganisms [42] | Drastically reduced microbial diversity and density [42] |
| Immune System | Underdeveloped; reduced immune cells & lymphoid tissues [44] | Altered but not completely ablated [42] |
| Cecal Morphology | Significantly enlarged cecum [44] | Mild to moderate cecal enlargement [42] |
| Experimental Control | Maximum control; known microbial composition [42] | Less control; residual microbes present [42] |
| Technical Demand | High (requires sterile isolators) [44] | Moderate (standard housing) [42] |
| Cost & Maintenance | High cost, labor-intensive [42] | Lower cost, easier maintenance [42] |
| Human Translation | Excellent for reductionist causality studies [4] | May better mimic antibiotic-exposed humans [42] |
Strengths and Limitations in Practice
Germ-free models provide the highest level of experimental control, creating a true "blank slate" with no historical microbial exposure [42]. This complete absence of microbes allows for precise colonization studies with defined microbial communities, enabling researchers to establish direct causal relationships between specific microbes and host phenotypes [43]. However, this approach requires specialized sterile isolator equipment and intensive maintenance, creating significant technical and financial barriers [44]. Additionally, the physiological adaptations to a microbe-free life—particularly the underdeveloped immune system and enlarged cecum—represent abnormal conditions that must be considered when interpreting results [44].
Antibiotic-treated models offer greater practicality and accessibility for many research settings [42]. The depletion (rather than elimination) of microbiota may better mimic common human conditions such as antibiotic exposure. However, these models face significant limitations including incomplete microbial eradication, potential off-target drug effects, and the inability to control for the composition of residual microbial communities [42]. The presence of remaining microbes or their components can confound experimental results and complicate causal interpretations.
Experimental Workflows and Key Methodologies
The power of GF models is fully realized through carefully designed colonization experiments. Two primary methodologies dominate the field: human microbiota-associated (HMA) models and defined microbial community applications.
Establishing Human Microbiota-Associated (HMA) Models
HMA models involve transplanting entire human microbial communities into GF recipients, creating "humanized" animals that carry a donor's gut microbiome [4]. This approach allows researchers to study the functional effects of human microbiomes in a controlled animal model.
Table 2: Key Stages in Establishing HMA Models
| Research Stage | Key Actions | Considerations |
|---|---|---|
| Donor Screening | Apply strict inclusion/exclusion criteria [4] | Exclude recent antibiotic/probiotic use (≥1-2 months); assess diet, health status, medications [4] |
| Sample Processing | Collect and process fecal samples anaerobically [4] | Minimize oxygen exposure; use cryoprotectants for storage; process quickly [4] |
| Recipient Preparation | Use GF or antibiotic-pretreated animals [4] | GF animals show superior engraftment; antibiotic pretreatment creates "pseudo-GF" state [4] |
| Transplantation | Administer fecal suspension via gavage [4] | Single gavage may suffice; multiple doses improve colonization efficiency [4] |
| Engraftment Validation | Analyze microbiome composition (16S rRNA sequencing) [4] | Verify donor microbiome profile establishment in recipients [4] |
The following diagram illustrates the generalized workflow for creating HMA mouse models:
Reductionist Approaches with Defined Microbial Communities
For mechanistic studies, GF animals can be colonized with defined, simplified microbial communities rather than complete human microbiota. This reductionist approach enables precise attribution of specific functions to individual microbial species or defined consortia, allowing researchers to dissect complex host-microbe interactions at a molecular level [42]. The resulting "gnotobiotic" animals (with known microbiota) provide a powerful platform for investigating microbial metabolism, immune modulation, and pathway-specific activities in ways not possible with complex, undefined communities.
The Scientist's Toolkit: Essential Research Reagents and Materials
Success in germ-free research depends on specialized materials and reagents that maintain sterility and enable precise experimentation.
Table 3: Essential Research Reagents for Germ-Free Studies
| Reagent/Material | Function & Application | Key Considerations |
|---|---|---|
| Sterile Isolators | Maintain germ-free environment with physical barrier [44] | Require specialized equipment and training; regular sterility monitoring essential [44] |
| Gamma-Irradiated Feed | Provides sterile nutrition without live microorganisms [44] | Must be fortified to compensate for nutrient loss during sterilization [44] |
| Fecal Suspension Buffer | Preserves microbial viability during transplantation [4] | Anaerobic conditions and cryoprotectants enhance microbial survival [4] |
| Antibiotic Cocktails | Depletes microbiota in pseudo-germ-free models [42] | Must control for off-target drug effects; incomplete eradication [42] |
| 16S rRNA Sequencing | Verifies germ-free status and engraftment efficiency [4] | Primary method for analyzing microbiome composition [4] |
Research Applications and Key Findings
GF models have generated foundational insights across numerous biomedical fields by enabling causal inferences between microbiota and host physiology.
Establishing Causality in Disease Pathogenesis
GF animals have been instrumental in demonstrating that gut microbiota can directly influence disease development and progression. For example, studies have shown that transferring gut microbiota from humans with specific diseases (such as metabolic syndrome, inflammatory bowel disease, or even neuropsychiatric conditions) to GF animals can transfer certain disease characteristics [4] [43]. This experimental paradigm provides compelling evidence for microbiota's causal role in disease pathogenesis, moving beyond correlational observations to mechanistic understanding.
Elucidating Host-Microbe Signaling Pathways
The diagram below illustrates how germ-free models help researchers dissect specific signaling pathways through which gut microbiota influence host physiology:
Research using this approach has revealed that microbiota suppress tonic Hedgehog signaling in the small intestine through Toll-like receptor (TLR2/TLR6) signaling, regulating intestinal barrier function [42]. Similarly, intestinal epithelial neuropilin-1 has been identified as a microbiota-dependent Hedgehog regulator that contributes to epithelial stabilization [42]. These findings exemplify the molecular precision possible with GF model systems.
Germ-free animal models remain irreplaceable tools for establishing causal links in microbiome research, providing the critical experimental platform needed to advance from correlation to mechanism. While each model system has distinct strengths and limitations, GF animals offer unparalleled control for reductionist studies of microbial function [42] [44]. As the field progresses toward clinical applications, these "blank slate" models will continue to enable rigorous testing of microbiome-based therapeutics and mechanistic investigations of host-microbe interactions across physiological systems.
The integration of GF models with multi-omics technologies and human microbiota-associated approaches creates a powerful framework for translational microbiome research [41] [4]. By combining the control of GF systems with the physiological relevance of human microbial communities, researchers can accelerate the development of novel microbiome-based diagnostics and interventions, ultimately bridging the gap between experimental models and human health.
The quest to establish causal links between the human gut microbiome and disease pathophysiology has positioned Human Microbiota-Associated (HMA) rodent models as indispensable tools in contemporary biomedical research. These models are created by transplanting human fecal microbiota into germ-free (GF) or antibiotic-pretreated rodents, enabling researchers to study human-specific microbial communities within a controlled laboratory setting [4] [45]. The fundamental premise underlying HMA models is their ability to transfer phenotypic traits from human donors to rodent recipients, thereby providing a causal experimental platform that transcends the correlative nature of human observational studies [45]. As the field of microbiome research rapidly expands, with implications for understanding conditions ranging from inflammatory bowel disease and obesity to neurological disorders and cancer immunotherapy responses, the proper utilization and critical assessment of HMA models becomes increasingly vital [4] [46] [45].
This comparison guide objectively examines the translational value of HMA rodent models by synthesizing current experimental data and methodological approaches. We present a balanced analysis of their significant contributions to mechanistic discovery alongside their inherent physiological constraints, with the aim of empowering researchers to design more interpretable and reproducible studies within the broader context of microbiome animal model human study findings correlation research.
Strengths of HMA Rodent Models
HMA rodent models offer several distinct advantages that have solidified their role in microbiome research.
Establishing Causality in Microbiome-Disease Relationships
The primary strength of HMA models lies in their ability to demonstrate causal relationships between specific human microbial communities and disease phenotypes. Unlike correlative human studies, HMA experiments can directly test whether microbiota from diseased individuals can induce or exacerbate pathophenotypes in recipient animals [45]. A recent scoping review of 489 studies revealed remarkably high success rates (>80%) in transferring disease-specific alterations for parameters including intestinal barrier function, gastrointestinal inflammation, circulating immune markers, and fecal metabolites [45]. This demonstrates the powerful phenotype transfer capability of these models across diverse disease contexts.
Environmental and Experimental Control
HMA models provide unprecedented control over variables that confound human studies, including genetic background, dietary composition, housing conditions, and medication exposure [47]. This controlled environment allows researchers to isolate the effects of the transplanted microbiota from other influencing factors, enabling rigorous hypothesis testing that would be impossible in human subjects [45]. Furthermore, the ability to manipulate these models through antibiotic treatments, dietary interventions, or pharmaceutical administration facilitates mechanistic studies exploring microbiome-host interactions [4].
Methodological Versatility and Phenotyping Depth
The flexibility of HMA protocols supports diverse research applications, from studying microbial community ecology to evaluating targeted therapeutic strategies [4]. Researchers can perform longitudinal sampling and access tissues for comprehensive multi-omics analyses, including metagenomics, transcriptomics, and metabolomics [48] [49]. This enables deep mechanistic insights into how transplanted human microbiota influence host physiology at multiple biological levels.
Table 1: Experimentally Demonstrated Phenotype Transfer Success Rates in HMA Models
| Outcome Category | Success Rate | Example Findings |
|---|---|---|
| Intestinal Barrier Function | >80% | Altered permeability, tight junction protein expression [45] |
| Gastrointestinal Inflammation | >80% | Increased pro-inflammatory cytokines, immune cell infiltration [45] |
| Circulating Immune Parameters | >80% | Changed T-cell populations, systemic cytokine levels [45] |
| Fecal Metabolites | >80% | Altered SCFA, bile acid, and tryptophan metabolite profiles [45] [48] |
| Behavioral Alterations | Reported | Depression/anxiety-like behaviors in neuropsychiatric disorder models [45] |
Limitations and Ecological Constraints
Despite their utility, HMA rodent models possess significant inherent limitations that affect their translational fidelity.
Incomplete Microbial Engraftment and Ecological Drift
A fundamental constraint of HMA models is the incomplete engraftment of human-derived microbial communities in rodent recipients. Multiple studies have demonstrated that only a taxonomically restricted set of human microbes successfully colonizes the murine gut, with consistent enrichment of specific taxa like Akkermansia muciniphila and Bacteroides species regardless of donor characteristics [46]. This engraftment limitation results in HMA mouse communities that resemble other mice more than their human donors, with one study reporting that "HMA mice were more similar to each other than the human donors or inoculum they are derived from" [46]. This ecological restructuring poses significant challenges for interpreting which specific microbial components drive observed phenotypes.
Physiological Disparities Between Species
The evolutionary divergence between humans and rodents creates fundamental differences in gastrointestinal anatomy, immune system function, and metabolic processes that limit translational potential [47]. Mice possess different bile acid compositions, faster intestinal transit times, and distinct immune cell distributions compared to humans [46]. These physiological differences create selective pressures that shape the transplanted microbiota differently than in the human donor, potentially altering microbial metabolism and host-microbe interactions [46]. Additionally, germ-free recipients used for HMA modeling have compromised immune development due to the absence of microbial exposure during early life, further diverging from human physiology [48] [47].
Methodological Heterogeneity and Standardization Challenges
Current HMA research suffers from significant methodological variability between research groups, hindering result comparability and reproducibility [4] [45]. Critical parameters including donor screening criteria, fecal processing methods, transplantation protocols, and engraftment validation approaches differ across studies [4]. A scoping review identified inconsistent reporting of key methodological aspects, making it difficult to assess technical quality or compare results across studies [45]. This lack of standardization represents a major challenge for the field.
Table 2: Comparative Engraftment Efficiency Across Different Recipient Models
| Recipient Model | Engraftment Efficiency | Notable Taxa | Developmental Considerations |
|---|---|---|---|
| Conventional HMA Mice | Limited, taxonomically restricted | Enrichment of Akkermansia, Bacteroides spp. [46] | Compromised immune development in GF recipients [48] |
| Two-Generation HMA Mice | Improved stability | Better retention of infant microbiota features [48] | Offspring show more developed immune systems [48] |
| HMA Piglets | Superior for child/adult/elderly microbiota | More donor species retained compared to mice [50] | Physiologically closer to humans; practical limitations |
Methodological Protocols for HMA Model Establishment
Standardized protocols are essential for generating reproducible HMA models. Below, we detail the critical methodological components based on current literature.
Donor Screening and Selection
Rigorous donor screening is paramount for HMA model validity. Comprehensive criteria should include:
- Medical History Assessment: Exclusion for recent antibiotic use (typically ≥1-2 months), gastrointestinal disorders, recent pathogen infections, and chronic illnesses that alter gut microbiota [4].
- Lifestyle Factors: Evaluation of dietary patterns, alcohol consumption, smoking status, and medication use (including probiotics and laxatives) [4].
- Laboratory Testing: Pathogen screening and basic health metrics to confirm donor status [4].
- Specialized Donor Groups: For disease-focused studies, donors must meet established diagnostic criteria for the condition under investigation, with careful consideration of comorbidities and concomitant medications that could confound results [4] [45].
Fecal Sample Processing and Preparation
Proper handling of fecal samples preserves microbial viability and integrity:
- Collection and Transport: Immediate freezing at -80°C or processing in anaerobic chambers to maintain anaerobic conditions [4] [46].
- Slurry Preparation: Homogenization in degassed phosphate-buffered saline (PBS) with cryoprotectants (e.g., 20% glycerol), typically at 0.1-0.3 g/mL concentration [46] [48].
- Filtration: Removal of large particulate matter using 300µm filters to prevent gavage needle clogging [46].
- Quality Control: Assessment of microbial viability and composition stability before transplantation [4].
Recipient Preparation and Transplantation
- Recipient Status: Use of germ-free mice or antibiotic-pretreated conventional mice to create a microbial niche [4] [45]. Antibiotic cocktails typically include broad-spectrum drugs like ampicillin, vancomycin, neomycin, and metronidazole administered via drinking water for 1-2 weeks [45].
- Transplantation Route: Most studies utilize oral gavage with 200-250µL of fecal slurry [46] [45]. Multiple administrations (e.g., daily for 3 days) improve colonization efficiency [4].
- Environmental Transfer: Additional exposure via fur smearing and cage bedding transfer to enhance microbial exchange [46].
- Stabilization Period: Allow 2-4 weeks for microbial community stabilization before experimental procedures [46].
Diagram 1: HMA Model Establishment Workflow. The process involves sequential phases from donor screening through experimental phenotyping, with critical quality control checkpoints at each stage.
The Researcher's Toolkit: Essential Reagents and Materials
Successful HMA experiments require specific reagents and materials carefully selected to maintain microbial viability and ensure reproducible results.
Table 3: Essential Research Reagents for HMA Studies
| Reagent/Material | Function/Purpose | Specification Considerations |
|---|---|---|
| Cryoprotectants | Preserve microbial viability during frozen storage | Glycerol (10-20%) in degassed PBS; anaerobic preparation [46] |
| Anaerobic Chambers | Maintain oxygen-free environment for sample processing | Essential for strict anaerobe viability; typically <1 ppm O₂ [46] |
| DNA Extraction Kits | Microbial DNA isolation for community analysis | Must effectively lyse Gram-positive bacteria; e.g., DNeasy PowerSoil Pro [46] |
| Sequencing Reagents | Taxonomic and functional profiling | 16S rRNA gene (V3-V4) or shotgun metagenomic sequencing kits [46] [48] |
| Antibiotic Cocktails | Deplete indigenous microbiota in conventional mice | Broad-spectrum combination (e.g., ampicillin, vancomycin, neomycin, metronidazole) [45] |
| Germ-Free Mice | Provide microbial-naive recipients | Require specialized isolator facilities and sterility monitoring [48] |
Critical Analysis of Model Fidelity and Alternative Approaches
Ecological Fidelity Assessment
Recent investigations have raised important concerns about the ecological fidelity of HMA models. A 2025 study systematically evaluating HMA mice found they "resembled other mice more than their respective human donors in gut microbial composition and function," indicating that host species effects overshadow donor-specific ecological features [46]. This fundamental limitation suggests that HMA mice may be poor avatars for assessing ecological responses to human microbiome-targeting interventions, though they remain valuable for studying specific mechanistic pathways [46].
Methodological Refinements and Alternatives
Several methodological innovations have emerged to address HMA model limitations:
- Two-Generation Models: Colonizing germ-free dams and studying offspring shows improved immune development and more stable human microbiota representation [48].
- Humanized Mice: Engrafting human hematopoietic stem cells or peripheral blood mononuclear cells creates chimeric models with human immune components, better recapitulating human immune-microbe interactions [51].
- Alternative Species: Porcine models demonstrate superior engraftment of human microbiota from child, adult, and elderly donors compared to mice, leveraging physiological similarities to humans [50].
Diagram 2: HMA Model Fidelity Framework. The translation from human donor to experimental readouts is influenced by several fidelity limitations, with corresponding model improvements being developed to address these constraints.
HMA rodent models represent a powerful but imperfect tool for investigating causal relationships between human gut microbiota and host physiology. While they provide unmatched experimental control and have successfully demonstrated phenotype transfer across numerous disease contexts, researchers must critically acknowledge their inherent limitations, particularly regarding incomplete microbial engraftment and physiological disparities between species.
Future methodological developments should focus on standardizing protocols across research groups, improving recipient models through humanization approaches, and potentially incorporating alternative species like pigs for specific research questions. Additionally, rigorous validation of microbial engraftment and ecological representation should become a standard component of HMA studies. By acknowledging both the strengths and limitations of these models and continuously refining their implementation, researchers can maximize the translational value of HMA studies in elucidating the causal role of human microbiota in health and disease.
The critical role of gut microbiota in host physiology and disease has catalyzed the need for robust animal models to investigate host-microbe interactions. Gnotobiotic models—hosts with entirely defined microbial compositions—provide a powerful tool for establishing causal relationships and elucidating mechanistic insights. While rodent models are widely used, several alternative organisms offer unique advantages for specific research questions. This guide objectively compares the application, experimental performance, and translational value of three key gnotobiotic models: zebrafish, Drosophila melanogaster (fruit fly), and pigs. Framed within the broader context of microbiome animal model human study findings correlation research, we detail the distinct capabilities of each model, supported by experimental data and standardized protocols to inform researchers and drug development professionals.
The table below provides a high-level comparison of the three gnotobiotic models, highlighting their core characteristics and primary research applications.
Table 1: Core Characteristics and Research Applications of Gnotobiotic Models
| Feature | Zebrafish (Danio rerio) | Drosophila (Fruit Fly) | Pigs |
|---|---|---|---|
| Microbiome Complexity | Low to moderate diversity [52] | Very low diversity (5-20 species) [53] | High diversity; resembles human [54] |
| Primary Research Applications | Host development, infectious disease, immunology, toxicology [52] | Bacterial genetics, host-pathogen interactions, nutrition [55] [53] | Human enteric infections, nutrition, vaccine development [56] [54] |
| Key Advantage | Optical transparency for in vivo imaging [52] | Powerful genetics; rapid, low-cost screening [55] [53] | High translational similarity to human GI system [54] |
| Human Microbiota Engraftment | Moderate | Low (non-human adapted microbiota) [55] | High (remarkable similarity to donor) [54] |
| Genetic Tractability | High | Very High | Low |
Model-Specific Insights and Experimental Data
The Zebrafish Model
Zebrafish serve as an efficient vertebrate model for gut microbiota studies, bridging the gap between invertebrate and mammalian systems.
Table 2: Quantitative Insights from Gnotobiotic Zebrafish Studies
| Experimental Finding | Quantitative Data | Research Implication |
|---|---|---|
| Timing of Gut Development | Digestive system functional at 76-126 hours post-fertilization (hpf); adult structure at ~33 days post-fertilization (dpf) [52]. | Enables developmental studies on microbiota influence during specific ontogenetic windows. |
| Conservation of Physiology | Gene expression and regulatory regions of intestinal epithelial cells (IECs) are conserved with mammals [52]. | Supports translational research on conserved gut functions like bile salt signaling [52]. |
| Method of GF Model Generation | Surface sterilization of the chorion [52]. | Allows for high-throughput generation of germ-free embryos for experimentation. |
Intestinal Structure and Human Correlation: The zebrafish intestine, while lacking a stomach, shares functional homology with mammals. Its epithelium is organized into folds analogous to mammalian villi, and it possesses specialized cells like lysosome-rich enterocytes (LREs) for protein absorption, a mechanism conserved in suckling mammals [52]. This structural and functional conservation makes zebrafish a compelling model for investigating fundamental host-microbe interactions.
The Drosophila melanogaster Model
The fruit fly is a powerhouse for genetic studies of host-microbe interactions, characterized by its simplicity and experimental tractability.
Table 3: Quantitative Insights from Gnotobiotic Drosophila Studies
| Experimental Finding | Quantitative Data | Research Implication |
|---|---|---|
| Stable Colonization Saturation | Foregut niche for Lactobacillus plantarum saturates at a carrying capacity of ~10^4 CFUs/fly [57]. | Demonstrates a finite, host-constructed niche governing bacterial population stability. |
| Colonization Stability | Stable colonizers (e.g., L. plantarum, Acetobacter indonesiensis) have a gut half-life of ~2.5 days [57]. | Quantifies the persistence of symbiotic associations against constant flushing. |
| Priority Effects | Pre-colonization with a strain reduces subsequent colonization by the same strain, but can facilitate unrelated species [57]. | Illustates ordered assembly rules for multi-species communities in a defined niche. |
Mechanism of Microbial Stability: Recent research has identified a host-constructed physical niche in the Drosophila foregut (proventriculus and crop duct) that selectively binds specific bacterial strains with remarkable stability [57]. This niche is saturable and exhibits strong priority effects, where initial colonizers can remodel the environment, for instance, through glycan-rich secretions, to favor secondary colonization by other commensals [57]. This provides a mechanistic framework for understanding the establishment and stability of a multi-species microbiome.
The Gnotobiotic Pig Model
Gnotobiotic pigs represent a highly translational model, closely mimicking the human intestinal microenvironment.
Table 4: Quantitative Insights from Gnotobiotic Pig Studies
| Experimental Finding | Quantitative Data | Research Implication |
|---|---|---|
| Human Norovirus (HuNoV) Inactivation | HPP at 350 MPa, 0°C for 2 min achieved a 3.7-log10 reduction in viral RNA; no infection in pigs. HPP at 350 MPa, 35°C achieved only a 1-log10 reduction; caused infection [56]. | Provided critical data for food safety, validating HPP parameters to inactivate the prevalent HuNoV GII.4 strain. |
| Model Translationality | Susceptible to human enteric pathogens (e.g., human rotavirus); can be fed authentic human diets [54]. | Directly models human infectious diseases and nutritional studies with high clinical relevance. |
| Human Microbiota Engraftment | Transplantation results in microbial profiles "remarkably similar" to the original human donor [54]. | Creates a highly accurate in vivo system of the human gut flora for mechanistic studies. |
Application in Infectious Disease and Nutrition: The gnotobiotic pig model has been pivotal in areas where other models fall short. Its susceptibility to human enteric viruses like norovirus and rotavirus, combined with its ability to support human microbiota and diets, makes it an unparalleled system for studying the pathophysiology of infectious diseases, evaluating vaccine efficacy, and understanding the interplay between malnutrition, gut dysbiosis, and immune function [56] [54].
Experimental Protocols for Gnotobiotic Model Generation
Standardized methodologies are crucial for reproducibility. Below are detailed protocols for creating gnotobiotic models in each organism.
Protocol 1: Generating a Gnotobiotic Zebrafish Model
This protocol is used to create germ-free zebrafish larvae for subsequent association with defined microbes [52].
- Surface Sterilization of Embryos: Collect zebrafish embryos and immerse them in a disinfectant solution, such as bleach diluted in sterile embryo medium, for a defined period.
- Washing and Verification: Thoroughly rinse the embryos multiple times with sterile embryo medium to remove all traces of the disinfectant.
- Aseptic Rearing: Transfer the sterilized embryos to sterile tissue culture flasks containing sterile embryo medium.
- Axenity Validation: Confirm the germ-free status throughout the experiment by culturing water samples on nutrient-rich media and using molecular methods (e.g., 16S rRNA PCR) on both water and homogenized larvae samples.
Protocol 2: Generating a Gnotobiotic Drosophila Model
This protocol describes the standard method for deriving germ-free flies and associating them with specific bacteria [55] [53].
- Egg Dechorionation: Collect fly eggs and briefly treat them with a chemical agent like bleach or a solution of hydrochloric acid and ethanol to remove the outer chorion.
- Aseptic Washing: Rinse the dechorionated eggs extensively with sterile water.
- Germ-Free Rearing: Transfer the sterilized eggs to a sterile vial or isolator containing autoclaved fly food.
- Microbial Association (Optional): To create a gnotobiotic fly, introduce a defined bacterial inoculum (e.g., by mixing with food or directly pipetting onto the surface of the sterile food) once the flies have developed to the desired life stage.
Protocol 3: Generating a Human Microbiota-Associated (HMA) Pig Model
This protocol involves transplanting human fecal microbiota into germ-free piglets to create a humanized model [58] [54].
- Donor Screening: Screen human donors based on strict inclusion/exclusion criteria, typically excluding recent antibiotic use (≥1-2 months), laxative/probiotic use, and individuals with gastrointestinal, neuropsychiatric, or chronic illnesses [58].
- Fecal Inoculum Preparation: Collect fresh fecal sample and process it anaerobically as soon as possible. Homogenize the sample in a reduced sterile buffer (e.g., with glycerol) and filter to remove large particulates.
- Recipient Preparation: Use cesarean-derived piglets reared in germ-free isolators to ensure no prior microbial exposure.
- Fecal Microbiota Transplantation (FMT): Orally administer the prepared fecal suspension to the germ-free piglets. Multiple gavages over several days may improve colonization efficiency [58].
- Engraftment Validation: Monitor engraftment by profiling the microbiome composition in piglet feces over time using 16S rRNA gene sequencing and compare it to the donor profile [58].
Diagram Title: Workflow for Creating a Human Microbiota-Associated (HMA) Pig Model
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and their functions essential for conducting gnotobiotic research across these models.
Table 5: Essential Reagents for Gnotobiotic Research
| Reagent / Material | Function | Application Across Models |
|---|---|---|
| Germ-Free Isolators | Provides a sterile physical barrier to maintain an axenic environment. | Zebrafish, Drosophila, Pigs [52] [59] |
| Sterilized Diet | Autoclaved or irradiated food to prevent microbial contamination. | Zebrafish, Drosophila, Pigs [55] [59] |
| Chemical Sterilants (e.g., Bleach) | Surface decontamination of embryos or eggs. | Zebrafish, Drosophila [52] [53] |
| Gnotobiotic Husbandry Equipment | Sterile cages, water systems, and handling tools. | Zebrafish, Drosophila, Pigs |
| Defined Bacterial Stocks | Known microbial strains for creating gnotobiotic associations. | Zebrafish, Drosophila, Pigs [53] [52] |
| Anaerobic Chamber | For processing oxygen-sensitive human fecal samples. | HMA Pig Model [58] |
| Cryopreservants (e.g., Glycerol) | For long-term storage of bacterial stocks and fecal inocula. | All models, HMA Pigs [58] |
| 16S rRNA Sequencing Reagents | To validate germ-free status and confirm microbial engraftment. | All models [58] |
The selection of a gnotobiotic model is dictated by the specific research question. Zebrafish offer unparalleled visual access to host-microbe dynamics in vivo. Drosophila provides unmatched genetic tools for high-throughput screening of interactions. The gnotobiotic pig stands as the most physiologically and translationally relevant model for human gastrointestinal and nutritional studies. By understanding the distinct capabilities, experimental outputs, and methodological requirements of each system, researchers can strategically deploy these powerful models to advance microbiome science and therapeutic development.
In the pursuit of advanced drug development and microbiome research, the scientific community faces a significant challenge: the limited translatability of findings from animal models to human clinical outcomes. Microphysiological systems (MPS), particularly organoids and organ-on-a-chip (OoC) technologies, have emerged as transformative tools that bridge this gap by offering human-relevant models with enhanced physiological accuracy. These systems replicate critical aspects of human tissue architecture, cellular diversity, and functional characteristics that are essential for studying host-microbiome interactions and drug responses [60]. The integration of these technologies into high-throughput screening (HTS) platforms represents a paradigm shift in preclinical research, enabling more efficient and predictive assessment of therapeutic compounds while addressing the ethical and translational limitations of traditional animal models [61]. This guide provides a comprehensive comparison of these systems, their experimental applications, and their growing role in correlating animal model findings with human biology.
Organoids and gut-on-a-chip systems represent distinct but complementary approaches to modeling human intestinal physiology. Intestinal organoids are three-dimensional (3D) miniature organ-like structures derived from adult stem cells (ASCs) or pluripotent stem cells (PSCs) that self-organize to mimic key aspects of intestinal architecture and cellular diversity [62] [63]. These models capture patient-specific characteristics and are highly scalable for screening applications. In contrast, gut-on-a-chip systems are microfluidic devices that incorporate human intestinal cells within a dynamic environment that mimics physiological conditions, including fluid flow, mechanical strain (peristalsis), and often multi-cellular interactions with endothelial, immune, or microbial components [64] [65].
Table 1: Fundamental Characteristics of Organoid and Gut-on-a-Chip Systems
| Feature | Organoid Systems | Gut-on-a-Chip Systems |
|---|---|---|
| Structural Basis | 3D cell aggregates with self-organizing properties [63] | Microfluidic channels with controlled microenvironments [66] |
| Key Cell Sources | Adult intestinal stem cells (ASCs), induced pluripotent stem cells (iPSCs) [62] | Intestinal organoids, cell lines (e.g., Caco-2, HT-29), primary cells [64] |
| Physiological Cues | Limited innate mechanotransduction; static culture conditions [63] | Incorporates fluid shear stress, peristaltic motions, and mechanical strain [64] |
| Microbiome Integration | Technically challenging due to enclosed apical surface [64] | Direct access to apical epithelium facilitates controlled microbiome co-culture [64] [65] |
| Throughput Potential | High; amenable to 96-well and 384-well formats [61] [63] | Moderate to high with recent advancements (e.g., 96-chip arrays) [67] [61] |
| Key Advantages | Patient specificity, rich cellular heterogeneity, scalability [63] | Dynamic microenvironments, direct microbiome access, real-time monitoring [65] |
Performance Comparison in Key Applications
When evaluated across critical research and development parameters, organoids and gut-on-a-chip systems demonstrate distinct performance characteristics that make them suitable for different applications within the drug development pipeline.
Table 2: Performance Comparison for Research and Development Applications
| Application | Organoid Performance | Gut-on-a-Chip Performance | Supporting Evidence |
|---|---|---|---|
| Drug Screening & Toxicity | High throughput; excellent for compound prioritization; maintains patient-specific responses [63] | Enhanced physiological relevance for absorption, distribution, metabolism, excretion (ADME) studies; better predicts human toxicity [67] [61] | Liver-Chip validated for DILI prediction; Kidney-Chip for oligonucleotide de-risking [67] |
| Host-Microbiome Research | Limited by inaccessible apical surface and lack of dynamic flow [64] | Superior for controlled microbiome studies; enables real-time observation of host-microbe-immune interactions [64] [65] | Gut-on-a-chip with fecal microbiome predicted melanoma immunotherapy responses [64] |
| Barrier Function Studies | Forms functional barriers but lacks physiological shear stress [62] | Recapitulates mature intestinal barrier with low permeability; responsive to inflammatory stimuli [64] | Permeability to dextran decreased significantly with endothelial co-culture (Papp 2.29 × 10⁻⁷ cm/s) [64] |
| Personalized Medicine | Excellent; biobanks of patient-derived organoids enable tailored therapeutic testing [63] | Emerging; requires complex integration of patient-derived cells but offers dynamic monitoring [65] | Pediatric IBD models using matched biopsies, stool, and blood samples [65] |
| Multi-Organ Interaction | Limited to single organ type without specialized systems | Advanced systems enable linked organ models for systemic pharmacology and toxicology [61] | Multi-chamber systems by TissUse, CN Bio, Kirkstall Ltd. [61] |
High-Throughput Screening Platforms and Experimental Outcomes
The evolution of high-throughput organ-on-chip (HT-OoC) platforms has significantly expanded the screening capabilities of microphysiological systems, addressing the pharmaceutical industry's need for efficiency and predictive power in early drug discovery.
Table 3: Commercial High-Throughput OoC Platforms and Capabilities
| Platform/Company | Technology Basis | Throughput Format | Key Applications | Reported Outcomes |
|---|---|---|---|---|
| AVA Emulation System (Emulate) | Microfluidic control with automated imaging [67] | 96 Organ-Chip "Emulations" [67] | Toxicology, ADME, immune cell recruitment [67] | 4-fold drop in consumable spend; 50% fewer cells and media per sample [67] |
| OrganoPlate (MIMETAS) | Microfluidic 3D culture without artificial membranes [61] | 40-, 64-, or 96-independent chips per plate [61] | Barrier integrity, transport, migration assays [61] | Direct apical and basolateral access for compounds and stimuli [61] |
| Chip-R1 (Emulate) | Rigid chip with minimal drug absorption [67] | Compatible with Zoë-CM2 Culture Module [67] | ADME and toxicology applications [67] | Low drug absorption; physiologically relevant shear stress [67] |
Recent studies demonstrate how these platforms are being applied to address specific research questions. A landmark 2025 study published in Nature Biomedical Engineering developed a gut-on-a-chip incorporating fecal samples from melanoma patients receiving immune checkpoint inhibitors [64]. This system identified epithelium-specific biomarkers and microbial factors that correlated with clinical outcomes, demonstrating that "the microbiome of non-responders has a reduced ability to buffer cellular stress and self-renew" [64]. The model successfully recapitulated microbiome-host interactions predictive of patient responses, showcasing the potential of OoC technology to uncover mechanistic insights not accessible through animal models or conventional in vitro systems.
Detailed Experimental Protocols
Protocol 1: Establishing a Gut-on-a-Chip with Microbiome Integration
This protocol adapts methodologies from the melanoma immunotherapy response study [64] for creating a human-relevant gut-on-a-chip model capable of incorporating patient-derived microbiome samples.
Key Reagents and Materials:
- Microfluidic device with two parallel channels separated by a collagen matrix
- Human intestinal organoids derived from induced pluripotent stem cells (hiPSCs) OR co-culture of Caco-2 and HT-29 MTX cell lines
- Human microvascular endothelial cells (HMEC-1)
- Type I collagen matrix
- Intestinal cell culture medium (appropriate for cell type selected)
- Endothelial cell culture medium
- Fecal sample from human donor (processed into sterile microbial inoculum)
Procedure:
- Device Preparation: Coat the vascular channel with collagen matrix (3-4.5 mg/mL concentration optimal for intestinal differentiation) [62] and allow to polymerize.
- Cell Seeding:
- Seed intestinal epithelial cells (dispersed organoids or cell lines) in the intestinal channel at density of 10-20×10⁶ cells/mL.
- Seed HMEC-1 cells in the vascular channel at density of 5-10×10⁶ cells/mL.
- Dynamic Culture:
- Connect channels to perfusion system providing continuous medium flow (shear stress of 0.02 dyne/cm²).
- Apply peristaltic-like mechanical deformation (10-15% strain, 0.2 Hz frequency).
- Culture for 7-14 days to allow epithelial polarization and maturation.
- Microbiome Introduction:
- After epithelial barrier formation (confirmed by TEER measurement or dextran permeability), introduce processed fecal microbiome sample to the apical surface of the intestinal channel.
- Continue co-culture with perfusion and mechanical actuation for desired experimental duration.
- Endpoint Analysis:
- Collect effluents from vascular and intestinal channels for multi-omic analysis (transcriptomics, metabolomics).
- Fix device for immunostaining of epithelial, endothelial, and immune markers.
- Assess barrier integrity via fluorescent dextran permeability assay.
Protocol 2: High-Throughput Drug Screening Using Intestinal Organoids
This protocol outlines the process for utilizing intestinal organoids in high-throughput drug screening campaigns, incorporating best practices for matrix selection and assay compatibility [63].
Key Reagents and Materials:
- Matrigel or defined hydrogel alternative (e.g., fibrin-based with laminin-111) [62]
- Intestinal organoids (patient-derived or iPSC-derived)
- Organoid culture medium with growth factors (Wnt, R-spondin, Noggin)
- 96-well or 384-well plates compatible with high-content imaging
- Compound library for screening
- Cell viability assay reagents (e.g., ATP-based, calcein-AM/propidium iodide)
Procedure:
- Organoid Generation:
- Culture intestinal organoids from stem cell sources in Matrigel domes with appropriate growth factor supplementation.
- Passage every 7-14 days using mechanical/enzymatic dissociation to maintain exponential growth phase.
- Assay Plate Preparation:
- Harvest and dissociate organoids into single cells or small clusters (3-10 cells).
- Mix cell suspension with BME or defined hydrogel at ratio 1:1-1:3.
- Plate 10-20 µL matrix-cell mixture per well in 96-well plates (1,000-5,000 cells/well).
- Allow matrix to polymerize (20-30 minutes at 37°C) before adding culture medium.
- Compound Treatment:
- After 3-5 days of culture (when organoids have reformed), add test compounds using robotic liquid handling.
- Include appropriate controls (vehicle, reference compounds).
- Incubate for desired treatment duration (typically 24-144 hours).
- Endpoint Assessment:
- Assess viability using ATP-based assays or live/dead staining.
- Evaluate morphology and size via brightfield or fluorescent imaging.
- For advanced endpoints, process for RNA/protein extraction or fix for immunostaining.
- Data Analysis:
- Normalize data to vehicle controls.
- Calculate IC₅₀ values using non-linear regression.
- Apply machine learning approaches for response classification and biomarker identification.
Visualization of Workflows and Signaling Pathways
Experimental Workflow for Gut-on-a-Chip Assembly
Gut-on-a-Chip Experimental Workflow
Host-Microbiome Signaling Interactions in Gut Models
Host-Microbiome Signaling Pathways
Essential Research Reagent Solutions
Successful implementation of organoid and gut-on-a-chip models requires specific reagent systems optimized for these advanced culture platforms.
Table 4: Essential Research Reagents for Intestinal MPS Models
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Extracellular Matrices | Matrigel, Cultrex, Geltrex [63] | Provides 3D scaffold for organoid growth | Batch variability; tumor-derived composition [62] |
| Defined Hydrogels | Alginate, hyaluronic acid, chitosan, fibrin [62] | Chemically-defined alternatives to Matrigel | Tunable stiffness; reproducible composition [62] [63] |
| Specialized Media | Intestinal stem cell media (Wnt, R-spondin, Noggin) [63] | Supports stem cell maintenance and differentiation | Growth factor quality and concentration critical [63] |
| Cell Sources | Intestinal organoids, Caco-2/HT-29 co-cultures, iPSCs [64] | Epithelial barrier formation | Primary vs. immortalized; donor variability [64] |
| Microfluidic Chips | Chip-S1, Chip-R1, OrganoPlate [67] [61] | Provides platform for gut-on-a-chip models | PDMS vs. plastic; drug absorption properties [67] |
| Characterization Tools | TEER electrodes, fluorescent dextrans, antibodies [64] | Assess barrier function and differentiation | Compatibility with 3D structures and microfluidics [64] |
Organoids and gut-on-a-chip systems offer complementary strengths for high-throughput screening in microbiome and drug development research. Organoids excel in scalability and patient-specific modeling, making them ideal for high-content drug screening and personalized medicine applications. Gut-on-a-chip platforms provide superior physiological relevance through dynamic microenvironments that better mimic human intestinal physiology, particularly for host-microbiome interaction studies. The strategic integration of both technologies throughout the drug development pipeline—from initial compound screening (organoids) to mechanistic investigation and preclinical validation (gut-on-a-chip)—represents the most powerful approach for enhancing the predictive accuracy of in vitro models and strengthening the correlation between animal model findings and human clinical outcomes. As these technologies continue to evolve through interdisciplinary collaboration and standardization, they promise to significantly advance microbiome research and therapeutic development.
The field of microbiome-based therapeutics is rapidly advancing, with multiple candidates now demonstrating significant clinical potential. This guide provides a detailed, objective comparison of three leading pipeline drugs: MaaT 013 (MaaT Pharma), SER-155 (Seres Therapeutics), and BMC128 (Biomica Ltd.). Each represents a distinct technological approach—from full-ecosystem restoration to rationally designed consortia—targeting different clinical indications within oncology and immunology. The following analysis synthesizes the latest clinical data, experimental methodologies, and mechanistic insights to inform researchers and drug development professionals about the current landscape and future directions of microbiome-based therapies.
Comprehensive Therapeutic Profiles
The microbiome therapeutic pipeline features diverse approaches, from full-ecosystem restoration to targeted bacterial consortia, each with distinct mechanisms and clinical targets.
Table 1: Pipeline Drug Overview and Status
| Drug Candidate | Company | Therapeutic Approach | Current Phase | Primary Indication(s) | Key Differentiator |
|---|---|---|---|---|---|
| MaaT 013 | MaaT Pharma | Pooled-donor, full-ecosystem enema [68] | Phase 3 [69] | GI-acute Graft-versus-Host Disease (GI-aGvHD) [68] | First microbiome therapy with positive Phase 3 results in third-line GI-aGvHD [70] |
| SER-155 | Seres Therapeutics | Oral, 16-strain cultivated consortium [71] | Phase 1b [69] [71] | Prevention of infections & GvHD in allo-HSCT patients [71] | Designed to decolonize antibiotic-resistant ESKAPE pathogens [71] |
| BMC128 | Biomica Ltd. | Rationally-designed 4-strain bacterial consortium [72] | Phase 1 [69] [72] | Solid tumors (NSCLC, Melanoma, RCC) in combo with anti-PD-1 [69] | Developed using AI-powered microbiome analysis platform (PRISM) [72] |
Table 2: Detailed Clinical Trial Data and Findings
| Parameter | MaaT 013 | SER-155 | BMC128 |
|---|---|---|---|
| Trial Identifier | ARES (NCT04769895) [70] | Not specified in sources | Ongoing Phase 1 (early results May 2024) [69] |
| Patient Population | Steroid & ruxolitinib refractory GI-aGvHD (n=66) [68] | Allo-HSCT patients (Cohort 1, n=13 dosed) [71] | NSCLC, melanoma, or RCC patients on nivolumab [69] |
| Primary Endpoint Result | 62% GI-Overall Response Rate at Day 28 (38% CR, 20% VGPR) [68] | Successful drug bacteria engraftment; reduced pathogen domination [71] | Promising early results on safety and tolerability [69] |
| Key Secondary Outcomes | 64% all-organ ORR; 12-month OS: 54% (67% in responders vs 28% non-responders) [68] [70] | No treatment-attributed serious adverse events [71] | Data pending from ongoing trial [69] |
| Safety Profile | Well-tolerated, no increased infection risk or treatment-related fatalities in initial cohort [70] | Favorable tolerability supporting continued development [71] | Early data shows acceptable safety profile [69] |
Mechanism of Action and Experimental Protocols
MaaT 013: Full-Ecosystem Restoration for GI-aGvHD
Therapeutic Mechanism: MaaT013 is a pooled-donor, high-richness microbiota ecosystem therapy delivered via enema. It is characterized by its Butycore component—a group of bacterial species known to produce anti-inflammatory metabolites including butyrate, which helps modulate immune function and enhance tolerance [68]. The therapy aims to restore the symbiotic relationship between the gut microbiome and immune system, correcting immune responsiveness in steroid-resistant, gastrointestinal-predominant aGvHD [68].
Key Experimental Protocol (Phase 3 ARES Trial):
- Study Design: Single-arm, open-label, multicenter Phase 3 trial across 50 European sites [68]
- Dosing Regimen: Pretreatment with oral vancomycin (250mg QID) on Days 0-1, followed by MaaT013 enema on Day 2, additional doses Days 3-5, and weekly doses during weeks 2 and 3 [70]
- Endpoint Measurement: GI-specific and overall organ response assessed at Day 28 using revised Glucksberg criteria, with durability assessed through 12-month survival [68] [70]
- Manufacturing Process: Faecal material from 3-8 strictly vetted healthy donors pooled and manufactured under cGMP conditions to ensure consistent high diversity and richness [73]
SER-155: Targeted Pathogen Decolonization
Therapeutic Mechanism: SER-155 is an oral, 16-strain cultivated microbiome therapeutic designed to reduce colonization and abundance of ESKAPE pathogens (e.g., Enterococcaceae, Enterobacteriaceae) in the GI tract [71]. It functions through multiple mechanisms: enhancing epithelial barrier integrity to prevent pathogen translocation, and modulating host immune responses to decrease GvHD incidence in immunocompromised allo-HSCT patients [71].
Key Experimental Protocol (Phase 1b Trial):
- Study Design: Two-cohort trial; Cohort 1 (n=13) assessed safety and pharmacology, Cohort 2 randomized, double-blinded, placebo-controlled (n=60 planned) [71]
- Endpoint Assessment: Primary safety monitoring; microbiome analysis for drug strain engraftment and reduction in GI domination by ESKAPE pathogens [71]
- Analytical Methods: Shotgun metagenomic sequencing to evaluate engraftment of drug strains and reduction of pathogenic organisms [71]
BMC128: AI-Designed Immuno-Oncology Consortium
Therapeutic Mechanism: BMC128 is a rationally-designed live bacterial product consisting of four unique bacterial strains selected using Biomica's PRISM platform powered by Evogene's MicroBoost AI technology [72]. The consortium enhances immune responses and supports anti-tumor activity through multiple biological mechanisms, potentially restoring anti-tumor immunity in patients receiving immune checkpoint inhibitors [72].
Key Experimental Protocol (Phase 1 Trial):
- Study Design: Phase 1 trial evaluating safety and tolerability in combination with nivolumab (anti-PD-1) [69]
- Patient Population: Patients with non-small cell lung cancer, melanoma, or renal cell carcinoma [69]
- Primary Focus: Initial safety and tolerability assessment with preliminary efficacy signals [69]
Diagram 1: Comparative mechanisms of action for profiled microbiome therapies
The Scientist's Toolkit: Essential Research Reagents & Platforms
Table 3: Key Research Tools and Platforms in Microbiome Drug Development
| Tool/Platform | Function | Representative User |
|---|---|---|
| PRISM with MicroBoost AI | High-resolution microbiome analysis platform for rational consortium design [72] | Biomica Ltd. [72] |
| Shotgun Metagenomic Sequencing | Comprehensive analysis of microbial community structure and function [71] | Seres Therapeutics [71] |
| cGMP FMT Manufacturing | Standardized production of pooled-donor microbiota therapeutics [73] | MaaT Pharma [73] |
| Butycore Analysis | Assessment of bacterial consortia producing immuno-regulatory metabolites [68] | MaaT Pharma [68] |
| Pathogen Domination Assays | Quantification of ESKAPE pathogen abundance in patient microbiome [71] | Seres Therapeutics [71] |
| Reverse Translation Platform | Discovery platform using human data, cell-based assays, and animal models [71] | Seres Therapeutics [71] |
Translational Research: Animal Models and Human Correlation
Animal models remain crucial for validating microbiome therapies before human trials. The National Academies of Sciences, Engineering, and Medicine has highlighted the importance of selecting appropriate animal models that best recapitulate specific aspects of human microbiome physiology and disease [74]. While mice have been the primary model organism, researchers are increasingly employing diverse animal models to better understand how microbial communities respond to various environmental and host stimuli [74].
The transition from animal models to human studies requires careful consideration of predictability and translatability. Key challenges include standardization of gnotobiotic animal research and accounting for biological variability [74]. Successful translation is evidenced by MaaT013, where Phase 2a findings of increased microbiota richness and butyrate-producers in human responders [73] aligned with its proposed mechanism, validating the preclinical research approach.
Diagram 2: Translational research workflow for microbiome therapeutics
The microbiome therapeutic pipeline demonstrates remarkable diversity in technological approaches, from full-ecosystem restoration to rationally designed consortia. MaaT013's positive Phase 3 results represent a watershed moment for the field, providing the first pivotal validation of microbiome-based therapy in a life-threatening condition [68] [70]. SER-155's targeted approach to pathogen decolonization addresses the critical unmet need of antibiotic resistance in immunocompromised patients [71], while BMC128's AI-driven design represents the next frontier in precision microbiome engineering for oncology [72].
The correlation between animal model research and human study findings continues to strengthen, with consistent signals across platforms that microbial richness, specific metabolite production, and pathogen reduction correlate with improved clinical outcomes [73] [71]. As these therapies advance through clinical development, they collectively underscore the transformative potential of microbiome-based interventions in reshaping treatment paradigms across immunology, oncology, and infectious disease.
Navigating Experimental Pitfalls: Critically Examining Bias and Rigor in Microbiome Models
Human microbiota-associated (HMA) animal models are indispensable tools for investigating causal links between the gut microbiome and human health. However, a critical scrutiny of recent evidence reveals significant limitations in their ecological fidelity. Studies consistently demonstrate that these models exhibit a restricted and biased engraftment of human microbes, favoring a taxonomically restricted set of bacterial taxa. This systematic bias challenges the interpretation of high efficacy rates, such as implausible 95% positive outcomes, and underscores the necessity for rigorous validation and standardized protocols in microbiome research.
The pursuit of causal mechanisms in human microbiome research relies heavily on human microbiota-associated (HMA) animal models. By transplanting human fecal microbiota into germ-free (GF) or antibiotic-treated animals, researchers aim to recreate human donor ecology to assess associated disease pathologies and therapeutic interventions [4]. These models have become a cornerstone for investigating microbe-host interactions across a spectrum of conditions, including inflammatory bowel disease, obesity, cancer immunotherapy response, and neurological disorders [39] [46]. The fundamental assumption underpinning these models is that they can faithfully recapitulate key aspects of human microbial ecology and function within a controlled laboratory setting, thereby enabling mechanistic studies that are impractical or impossible in human subjects.
However, a growing body of evidence challenges this assumption, pointing to systematic biases that may lead to overoptimistic interpretations of model efficacy. This review scrutinizes the premise of implausibly high success rates—exemplified by a hypothetical 95% positive rate—by examining the technical and biological constraints of HMA models. We synthesize findings from recent studies that directly assess the ecological fidelity of these models, analyze the factors contributing to biased engraftment, and provide evidence-based recommendations to enhance methodological rigor and translational relevance in this critical field of research.
Quantitative Evidence: Documenting Ecological Disparity
A critical evaluation of HMA model performance requires examining quantitative data on microbial engraftment. The following tables summarize key comparative findings from recent studies that directly quantify the divergence between human donor microbiomes and the resulting HMA mouse models.
Table 1: Key Findings from HMA Mouse Model Fidelity Assessment
| Metric of Comparison | Finding in HMA Mice | Implication for Model Fidelity |
|---|---|---|
| Overall Microbial Composition | More similar to other mice than to their respective human donors [46] | Host species effects overshadow donor ecology |
| Responses to Microbial Consortia | Ecological effects more strongly associated with host species than donor stool ecology or human treatment response [46] | Limited utility for predicting ecological impact of interventions in humans |
| Specific Taxa Enrichment | Consistent enrichment of Akkermansia muciniphila and Bacteroides spp., regardless of donor profile [46] | Systematic selection for a taxonomically restricted, mouse-adapted set of microbes |
| Engraftment Reproducibility | A limited repertoire of microbes successfully engrafts across different HMA mouse studies [46] | Fundamental restriction in the transferable diversity of human gut communities |
Table 2: Factors Influencing Microbiota Engraftment and Model Reproducibility
| Factor | Effect on Engraftment & Reproducibility | Supporting Evidence |
|---|---|---|
| Host Species Physiology | Gastrointestinal tract anatomy, immunity, and metabolism significantly constrain which human microbes can colonize [46] [4] | Mice lack certain human-specific genera; rats and pigs show somewhat closer phyla-level similarity to humans [39] |
| Donor Screening & Preparation | Antibiotic history, diet, and health status profoundly alter the starting inoculum [4] | Antibiotics can reduce diversity for >1.5 months; diet provides substrate for specific microbes [4] |
| Fecal Sample Processing | Exposure to oxygen, processing delays, and preservation methods affect microbial viability [4] | Standardized, anaerobic processing with cryoprotectants is recommended for stability [4] |
| Recipient Preparation | Germ-free vs. antibiotic-treated pseudo-germ-free states offer different starting environments for engraftment [4] | Germ-free animals have underdeveloped immune systems, which may affect later responses [39] |
The data reveal a consistent pattern: the gut microbiome in HMA mice is shaped more by the recipient's murine biology than by the human donor's microbial blueprint. This fundamental disparity is driven by a "taxonomically restricted gut microbiome" in HMA mice, where a predictable, limited set of bacteria—such as Akkermansia muciniphila and Bacteroides species—dominates, irrespective of the donor's original microbial composition [46]. This selective engraftment creates a systematic bias, potentially amplifying the role of these easily transplantable taxa while rendering invisible the functions of microbes that fail to colonize.
Experimental Protocols: Methodological Roots of Bias
The ecological disparities observed in HMA models stem from specific methodological choices across the experimental pipeline. Understanding and standardizing these protocols is essential for interpreting results and mitigating bias.
Donor Screening and Fecal Sample Processing
Establishing a successful HMA model begins with rigorous donor screening. Current protocols for studies involving human donors often include exclusion criteria such as:
- Antibiotic exposure: A minimum of 2 to 12 months without antibiotic use prior to donation [4].
- Medication and health status: Exclusion for recent use of laxatives, probiotics, or prebiotics; presence of gastrointestinal disorders, acute or chronic illnesses that alter gut microbes, and active neuropsychiatric disorders [4].
- Lifestyle factors: Exclusion for excessive alcoholism or smoking habits [4].
Following donor selection, fecal sample processing must preserve microbial viability. Best practices include:
- Immediate processing: Fecal samples should be processed as soon as possible after collection [4].
- Anaerobic environment: Processing should occur in an anaerobic chamber to protect oxygen-sensitive microbes [46].
- Cryopreservation: The use of suitable cryoprotectants, such as phosphate-buffered saline (PBS) with 20% glycerol, is crucial for preserving microbial communities during low-temperature storage [46].
Recipient Preparation and Fecal Microbiota Transplantation (FMT)
The choice and preparation of recipient animals are critical. The most common recipients are:
- Germ-free (GF) mice: Raised in complete isolation from microorganisms [4].
- Pseudo-germ-free mice: Generated through antibiotic-mediated depletion of the native microbiota [4].
The FMT procedure itself involves:
- Inoculation: Typically, a single gavage of a standardized fecal suspension (e.g., 250 µL) into recipient mice is sufficient for model establishment [46].
- Stabilization: Post-FMT, a stabilization period of several weeks is allowed for the donor microbiota to establish a stable community within the recipient gut [46].
- Engraftment Validation: Microbial community profiling via 16S rRNA gene sequencing is the primary method for verifying the successful colonization of donor microbiota [4].
Route of Intervention Exposure
A particularly insightful protocol examines how interventions are tested. A 2025 study compared two routes:
- Human-treated route: HMA mice are generated using stool from humans collected before and after they have received an intervention (e.g., a microbial consortium).
- Mouse-treated route: HMA mice are generated using pre-intervention human stool, and the mice themselves are subsequently treated with the intervention directly. The study found that regardless of the exposure route, the resulting microbial communities in the mice clustered by host species rather than by donor ecology or intervention response, highlighting the overwhelming effect of the murine host environment [46].
Visualizing Workflows and Limitations
The following diagrams, defined using the DOT language and adhering to the specified color palette, illustrate the standard experimental workflow and its core limitation.
Graph 1: General Workflow for Establishing HMA Mouse Models. The process involves sequential steps of donor preparation (yellow), recipient preparation (green), a critical transplantation step (red), and subsequent validation and experimentation (blue).
Graph 2: The Core Limitation of HMA Models. The transformation from a complex human donor microbiome to a taxonomically restricted mouse microbiome demonstrates that the recipient's host species effect is a more powerful determinant of the final community structure than the donor's original microbial composition.
The Scientist's Toolkit: Essential Research Reagents
To conduct rigorous HMA studies, researchers rely on a suite of specialized reagents and tools. The following table details key solutions and their critical functions in establishing and validating these models.
Table 3: Essential Reagent Solutions for HMA Model Research
| Research Reagent / Solution | Critical Function in HMA Experiments |
|---|---|
| Degassed PBS + Glycerol | Serves as an anaerobic, cryoprotective suspension medium for preparing fecal slurries from human donor samples, preserving microbial viability during processing and storage [46]. |
| Antibiotic Cocktails | Used for depleting the native gut microbiota of conventional mice to generate "pseudo-germ-free" recipients, creating a niche for donor microbiota engraftment [4]. |
| DNA Extraction Kits (e.g., DNeasy PowerSoil Pro) | Essential for high-yield microbial DNA extraction from complex fecal and gut tissue samples, enabling subsequent molecular analysis of the microbiome [46]. |
| 16S rRNA Gene Sequencing Reagents | Allow for taxonomic profiling of the microbial community to analyze composition, verify donor engraftment efficiency, and track changes over time [4] [75]. |
| Metagenomic Sequencing Kits (e.g., Illumina) | Enable whole-genome shotgun sequencing of the microbial community, providing insights not only into taxonomy but also into functional metabolic potential [46]. |
| Microbial Consortium Formulations | Defined communities of bacterial isolates (e.g., MET4) used as interventions to test specific hypotheses about microbial functions in disease contexts within HMA models [46]. |
The pursuit of scientific truth in microbiome research demands a clear-eyed view of our tools. The evidence is clear: HMA animal models, while invaluable, do not function as perfect avatars of human gut ecology. The documented systematic biases, particularly the selective engraftment of a limited repertoire of microbes and the dominance of host-species effects, fundamentally challenge the plausibility of universally high success rates. Assertions of 95% positive outcomes likely reflect these inherent model constraints rather than true biological efficacy. Therefore, a more nuanced and critical approach is imperative. Future research must prioritize methodological transparency, adopt rigorous standardization of donor screening and processing protocols, and employ multi-omics validation to better quantify model limitations. By acknowledging and actively working to mitigate these biases, the scientific community can more reliably harness the power of HMA models to uncover meaningful, translatable insights into human health and disease.
In the pursuit of translating microbiome research from animal models to human therapies, pseudoreplication and donor variability represent formidable yet frequently underestimated challenges. This review objectively compares experimental approaches in microbiome science, demonstrating how inadequate sample sizes and unaccounted donor effects can jeopardize data integrity and translational potential. We synthesize empirical evidence from fecal microbiota transplantation (FMT) studies, human microbiota-associated mouse models, and clinical trials, providing structured quantitative comparisons of methodological efficacy. The analysis reveals that studies implementing rigorous donor stratification and sufficient biological replication achieve significantly higher experimental consistency and clinical success rates. Supporting experimental data underscore the critical importance of standardized protocols, appropriate statistical frameworks, and comprehensive reporting practices for advancing reproducible microbiome research with genuine translational impact.
Pseudoreplication occurs when researchers incorrectly treat non-independent data points as independent observations, violating core statistical assumptions and generating misleading conclusions. In microbiome research, this manifests when technical replicates from the same biological source are treated as true biological replicates, or when donor-specific effects are ignored in studies involving fecal transplants or microbial consortia. The repercussions extend beyond statistical inaccuracies to fundamentally flawed biological interpretations that impede translational progress.
The complexity of microbiome data exacerbates this challenge. Characterized by high dimensionality (more features than samples), compositionality, and significant inter-individual variation, microbiome datasets require specialized statistical approaches that account for these inherent properties [76] [77]. When combined with pseudoreplication, these features create a perfect storm of statistical artifacts that can persist undetected through publication, particularly in animal model systems where cost and logistics incentivize inadequate sample sizes.
Within the broader thesis of microbiome animal model-human study correlation research, addressing pseudoreplication is not merely a statistical formality but a fundamental prerequisite for valid scientific inference. The following sections analyze how donor variability and sample size considerations specifically impact key experimental paradigms in microbiome research, providing comparative data and methodological frameworks for enhancing research rigor.
Donor Variability as a Source of Experimental Noise
Quantitative Evidence of Donor-Dependent FMT Outcomes
Fecal microbiota transplantation represents a powerful case study for examining donor effects, with substantial evidence demonstrating that donor selection critically influences therapeutic outcomes. Systematic analysis reveals that donor microbial composition directly determines FMT efficacy, with profound implications for experimental consistency and clinical translation.
Table 1: Impact of Donor Microbial Composition on FMT Efficacy in Murine Colitis Models
| Donor Type | Clinical Improvement | Microbial Diversity Restoration | Key Microbial Shifts Post-FMT |
|---|---|---|---|
| High-abundance beneficial genera | Significant amelioration of colitis symptoms | Restored to healthy control levels | Increased Firmicutes/Bacteroidota; decreased Verrucomicrobiota; enrichment of Lactobacillus and Dubosiella |
| Low-abundance beneficial genera | Limited therapeutic effect | Partial restoration | Incomplete microbial community reorganization |
| 5-ASA (drug control) | Moderate improvement | Minimal improvement | Limited impact on microbial architecture |
Research stratifying donors based on the abundance of health-associated microbial genera demonstrates that FMT from high-abundance donors substantially outperforms both low-abundance donors and conventional 5-ASA treatment in murine colitis models [78]. Specifically, mice receiving FMT from high-abundance donors showed increased Firmicutes and Bacteroidota phyla with decreased Verrucomicrobiota, along with specific enrichment of beneficial genera including Lactobacillus and Dubosiella [78].
Beyond composition, strain-level engraftment efficiency varies dramatically between donors. Integrated meta-analysis of 226 FMT triads across eight diseases revealed that recipients with higher donor strain engraftment were significantly more likely to experience clinical success (P = 0.017) [79]. Engraftment efficiency exhibits notable phylogenetic patterns, with Bacteroidetes and Actinobacteria species (including Bifidobacteria) displaying consistently higher engraftment rates than most Firmicutes species [79].
Donor-Driven Variability in Human Microbiota-Associated Mouse Models
The limitations of donor variability extend to human microbiota-associated (HMA) mouse models, where ecological recapitulation of human microbiomes faces fundamental constraints. Assessment of HMA mouse fidelity reveals that recipient mice consistently resemble other mice more than their human donors, with a taxonomically restricted set of microbes reliably engrafting regardless of the donor stool ecology [46].
Table 2: Limitations of Human Microbiota-Associated Mouse Models
| Aspect | Finding | Implication |
|---|---|---|
| Community similarity | HMA mice more similar to other mice than human donors | Host species effects overshadow donor ecology |
| Engraftment capacity | Limited repertoire of microbes engraft regardless of donor | Taxonomically restricted representation of human microbiome |
| Ecological response | Ecological effects more strongly associated with host species than donor | Limited utility for assessing ecological impact of human interventions |
| Cross-study validation | Pattern consistent across four distinct health conditions | Fundamental limitation rather than protocol-specific issue |
This phenomenon persists across multiple studies and health conditions, suggesting that comparatively large host-species effects overshadow ecological effects of treatments that HMA models aim to recapitulate [46]. Specifically, taxa including Akkermansia muciniphila and Bacteroides spp. become enriched in mouse recipients regardless of donor profile, indicating strong host-specific selection pressures that constrain translational predictability.
Sample Size and Statistical Power in Microbiome Studies
The Multiplicity Challenge in High-Dimensional Data
Microbiome data presents unique statistical challenges due to its high-dimensional nature, with typically hundreds to thousands of operational taxonomic units (OTUs) or amplicon sequence variants (ASVs) measured across far fewer samples [76] [77]. This high feature-to-sample ratio creates a multiple comparisons problem, where the probability of false discoveries increases exponentially with the number of hypotheses tested.
Without appropriate statistical correction, studies with inadequate sample sizes generate seemingly significant findings that cannot be distinguished from random noise. The problem is compounded by data compositionality, where changes in the abundance of some taxa necessarily alter the apparent abundances of others, creating spurious correlations that reflect data structure rather than biological reality [77].
Statistical methods for addressing these challenges include:
- False Discovery Rate (FDR) control: Procedures like the Benjamini-Hochberg method that control the expected proportion of false discoveries among significant results
- Compositional data analysis: Approaches that account for the constant-sum constraint of relative abundance data
- Permutation-based testing: Non-parametric methods that generate empirical null distributions without relying on potentially inappropriate distributional assumptions
Power Analysis Considerations for Microbiome Studies
Conventional power analysis approaches often prove inadequate for microbiome studies due to effect size uncertainty and complex correlation structures among microbial taxa. While general guidelines suggest minimum sample sizes, appropriate powering requires consideration of specific research questions and anticipated effect sizes.
Key considerations for power analysis in microbiome research include:
- Diversity metrics: Richness estimates (Chao1) typically require smaller samples than evenness-based metrics (Shannon)
- Effect size expectations: Based on prior literature, microbiome interventions often produce small to moderate effect sizes on individual taxa, necessitating larger samples
- Grouping factors: Studies with multiple categorical predictors or continuous covariates require additional samples to account for increased model complexity
- Dropout rates: The high frequency of zero counts (sparsity) in microbiome data reduces effective sample size for specific taxa
Statistical software packages such as G*Power, GEEpower (for correlated data), and microbiome-specific tools like metagenomeSeq offer specialized approaches for power calculation in microbiome studies, though pre-study pilot data remains invaluable for realistic parameter estimation.
Experimental Protocols and Methodological Standards
Donor Selection and Stratification Protocols
Robust experimental design begins with systematic donor selection and stratification. The following protocol, adapted from FMT studies with demonstrated efficacy, provides a framework for minimizing donor-driven variability:
Step 1: Donor Recruitment and Initial Screening
- Recruit healthy donors without recent antibiotic exposure (typically >30 days)
- Exclude donors with familial history of gastrointestinal disorders, autoimmune diseases, or severe allergies
- Obtain written informed consent and ethical approval in accordance with Declaration of Helsinki standards [78]
Step 2: Microbiome Profiling
- Collect fecal specimens preprandially using sterile, gas-impermeable anaerobic collection tubes
- Process samples in anaerobic chamber to minimize oxygen exposure
- Extract fecal genomic DNA using standardized kits (e.g., HiPure Stool DNA Mini Kit)
- Amplify V3-V4 hypervariable regions of bacterial 16S rRNA genes with specific primers (341F/805R)
- Sequence on Illumina MiSeq platform (2×300 bp paired-end) with minimum read depth of 50,000 reads per sample and Q30 >80% [78]
Step 3: Bioinformatics and Donor Stratification
- Process raw sequencing reads through DADA2 pipeline or similar quality-controlled workflow
- Cluster high-fidelity sequences into OTUs (97% similarity) or ASVs using UPARSE algorithm
- Conduct taxonomic classification against reference databases (e.g., SILVA 138.1)
- Perform differential abundance analysis via LEfSe with significance thresholds (LDA score >3.0, p < 0.05)
- Rank donors according to median relative abundance of health-associated microbial genera identified through differential analysis [78]
Step 4: Validation in Animal Models
- Utilize dextran sulfate sodium (DSS)-induced colitis mice or other disease-relevant models
- Administer donor microbiota transplants from stratified donors
- Evaluate disease activity indices and microbiota dynamics through longitudinal sequencing
- Compare against appropriate controls (e.g., low-abundance donors, conventional therapeutics)
Figure 1: Experimental Workflow for Donor Selection and Validation. This protocol emphasizes systematic donor characterization and stratification to minimize variability in microbiota transplantation studies.
Sample Size Determination and Avoidance of Pseudoreplication
Statistical Planning Phase
- Conduct power analysis based on primary outcome metric (e.g., beta-diversity effect size)
- For pilot studies, focus on feasibility and variance estimation for future powered studies
- Account for anticipated dropout and technical failure rates in sample planning
Experimental Design Phase
- Ensure true biological replication: each experimental unit represents an independent source of biological material
- Avoid treating technical replicates (multiple sequencing runs from same sample) as biological replicates
- For longitudinal designs, use appropriate mixed-effects models that account for within-subject correlation
- Block designs by known confounding factors (e.g., sequencing batch, processing date)
Analysis Phase
- Apply multiple testing corrections for high-dimensional taxonomic analyses
- Use compositionally appropriate methods for relative abundance data
- For clustered data (multiple observations per subject), employ generalized estimating equations or mixed models
- Document and report all samples, including exclusions, with explicit justification
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents and Solutions for Robust Microbiome Studies
| Category | Specific Product/Kit | Function | Considerations |
|---|---|---|---|
| DNA Extraction | HiPure Stool DNA Mini Kit | Fecal genomic DNA extraction | Maintains DNA integrity for amplification |
| 16S rRNA Amplification | 341F/805R primers | V3-V4 hypervariable region amplification | Standardized for microbiome profiling |
| Sequencing Platform | Illumina MiSeq | High-throughput sequencing | 2×300 bp paired-end provides sufficient read length |
| Bioinformatics Tools | QIIME 2, DADA2 pipeline | Processing raw sequencing data | Quality control, chimera removal, ASV inference |
| Reference Database | SILVA 138.1 | Taxonomic classification | Curated database for accurate taxonomic assignment |
| Statistical Analysis | LEfSe, MaAsLin2 | Differential abundance analysis | Accounts for compositionality and multiple comparisons |
| Data Visualization | R ggplot2, PCoA plots | Data exploration and presentation | Effective communication of complex data |
Comparative Analysis of Alternative Approaches
Emerging Solutions to Donor Variability
Conventional FMT faces significant challenges regarding donor variability and safety concerns. Emerging approaches aim to address these limitations while maintaining therapeutic efficacy:
Fecal Virome Transplantation (FVT)
- Utilizes sterile-filtered donor feces containing mainly viruses (bacteriophages) and minimal bacteria
- Demonstrates comparable efficacy to FMT for recurrent C. difficile infection in some studies [80]
- Reduces risk of bacterial pathogen transmission but retains eukaryotic virus transfer concerns
Enhanced Safety FVT Protocols
- Solvent/Detergent Treatment (FVT-SDT): Inactivates enveloped viruses while preserving bacteriophage activity
- Chemostat Propagation (FVT-ChP): Removes eukaryotic viruses through dilution and allows production scale-up
- Pyronin-Y Treatment (FVT-PyT): Inhibits RNA virus replication, targeting major eukaryotic virus groups
Table 4: Comparative Efficacy of Modified FVT Approaches in C. difficile Infection Model
| Treatment Approach | Incidence Reaching Humane Endpoint | C. difficile Load Reduction | Key Advantages |
|---|---|---|---|
| FVT-SDT | 0/8 | Significant (7/8 negative by qPCR) | Eliminates enveloped eukaryotic viruses |
| FVT-UnT | 2/7 | Significant | Maintains native virome composition |
| FVT-ChP | 3/8 | Significant | Scalable production, improves reproducibility |
| FVT-PyT | 7/8 | Limited | Targets RNA viruses specifically |
| FMT | 5/8 | Moderate | Established protocol, broad microbial transfer |
| Saline Control | 5/7 | Minimal | Baseline disease progression |
Defined Microbial Consortia
- Utilize precisely characterized bacterial isolates with known functional properties
- Offer improved reproducibility and safety profile
- MET4 consortium comprises 30 individually cultured bacterial isolates chosen based on association with immune checkpoint inhibitor response [46]
- Limited engraftment in HMA mice highlights persistence-host specificity challenges [46]
Pathway to Improved Translation
Figure 2: Challenges and Solutions in Microbiome Translation Research. This conceptual diagram illustrates major barriers to translational validity in microbiome research and evidence-based approaches to address them.
The perils of pseudoreplication and donor variability in microbiome research represent more than statistical nuances—they constitute fundamental barriers to scientific progress and therapeutic development. The comparative evidence presented demonstrates that studies implementing systematic donor selection, appropriate sample sizes, and statistical methods accounting for microbiome data characteristics achieve substantially improved consistency and translational potential.
As the field advances, methodological rigor must evolve accordingly. Researchers should prioritize standardized protocols for donor characterization, transparent reporting of sample processing and statistical approaches, and validation of findings across multiple model systems when feasible. By confronting these challenges directly, the microbiome research community can enhance the reliability of mechanistic insights and accelerate the development of effective microbiome-based therapeutics.
In microbiome research, the absence of standardized protocols across different research groups presents a significant crisis, profoundly affecting the interpretation, reproducibility, and translational potential of scientific findings. This standardization challenge is particularly acute in studies utilizing animal models to investigate human microbiome-associated diseases. The field lacks a consistent set of methods, with variations arising from differences in budget, technical preferences, and the heterogeneous adoption of new technologies [81]. These methodological discrepancies create substantial interpretation challenges, as even minor variations in experimental design can significantly impact study outcomes and conclusions. For researchers and drug development professionals, this crisis necessitates a thorough understanding of how specific methodological choices can influence their results and the subsequent correlation between animal model findings and human applications. This guide objectively compares how different experimental decisions affect data interpretation in microbiome research, providing a structured framework for evaluating methodological approaches within the broader context of translating animal model findings to human relevance.
Quantitative Impact of Methodological Variations
The tables below synthesize empirical data demonstrating how specific methodological choices quantitatively impact microbiome study outcomes, highlighting the critical need for standardization in the field.
Table 1: Impact of DNA Extraction Methods on Microbiome Data Interpretation
| Extraction Kit | Cost Relative to Gold Standard | Bead Beating Step | Effect on Microbial Biomarker Identification | Impact on Diversity Measures |
|---|---|---|---|---|
| Qiagen PowerSoil | Baseline (Gold Standard) | Yes | Reference standard | Reference standard |
| Qiagen Blood & Tissue | 50% lower | No | Significant effect | Moderate effect |
| Macherey-Nagel NucleoSpin | Significantly lower | Yes | Significant effect | Moderate effect |
Table 2: Effects of Experimental Decisions on Microbiome Study Outcomes
| Experimental Decision | Alternatives | Impact on Data Interpretation | Statistical Significance |
|---|---|---|---|
| Dissection Method | Gut dissection vs. whole fish | Significant effect on microbial biomarker identification | Context-dependent significance |
| PCR Replication | Single vs. pooled triplicate reactions | Smallest effect on final interpretations | Generally non-significant |
| Animal Model Origin | Different facility sources | Very different microbiotas, affecting immune cell interactions | Major impact on reproducibility |
| Sample Handling | Immediate processing vs. freeze-drying | Subtle changes in apparent composition | Requires standardization |
Detailed Experimental Protocols
Protocol 1: Zebrafish Microbiome Exposure Study
This protocol evaluates how experimental decisions impact the assessment of chemical effects on the zebrafish gut microbiome, based on established methodologies [81].
Materials and Methods:
- Animal Model: Tropical 5D strain zebrafish reared at 28°C on a 14h light/10h dark photoperiod
- Exposure Paradigm: 384 zebrafish embryos exposed to either 10µM benzo[a]pyrene (BaP) or embryo medium control in 96-well plates for 9 days
- Sample Collection: At 9 days post-fertilization, euthanize via ice slurry immersion; two dissection approaches:
- Intestinal tissue dissection only
- Whole carcass processing
- DNA Extraction: Parallel extractions using three different kits:
- Qiagen DNA Powersoil Pro Kit (with bead beating)
- Qiagen DNA Blood & Tissue Kit (without bead beating)
- Macherey-Nagel NucleoSpin DNA Stool Kit (with bead beating)
- Sequencing Preparation: PCR amplification of V4 region of 16S rRNA gene using Earth Microbiome Project primers 515F/806R; compare single versus pooled triplicate reactions
- Analysis: Assess impacts on alpha diversity, beta diversity, and microbial biomarker identification
Protocol 2: Human Microbiota-Associated (HMA) Animal Model Generation
This protocol outlines the critical stages for creating standardized HMA models for microbiome research [82].
Materials and Methods:
- Donor Screening: Implement strict inclusion/exclusion criteria; exclude donors with short-term antibiotic, probiotic, or laxative use
- Fecal Sample Processing: Collect samples anaerobically; process immediately with suitable protectants; avoid prolonged low-temperature storage
- Recipient Preparation: Utilize germ-free or pseudo-germ-free animals generated via antibiotic-mediated microbiota depletion
- Fecal Microbiota Transplantation (FMT):
- Minimum: Single gavage of fecal suspension
- Optimal: Multiple frequencies and longer FMT durations for improved donor microbiota colonization
- Engraftment Validation: Microbial community profiling via 16S rRNA gene sequencing to verify donor microbiota establishment
Visualizing Experimental Workflows
The following diagrams illustrate key experimental workflows and their impact on data interpretation in microbiome research.
Advanced Analytical Approaches
The standardization crisis extends to statistical analysis methods, where different approaches can yield varying interpretations of the same underlying data.
microSLAM: Population Structure-Aware Analysis
The microSLAM framework addresses limitations of standard relative abundance tests by incorporating within-species genetic variation into association analyses [83].
Methodological Overview:
- Step 1: Estimate population structure across hosts for each microbial species
- Step 2: Calculate association between population structure and host traits to identify species where specific strain subsets confer risk
- Step 3: Model traits as a function of gene occurrence while accounting for strain relatedness using random effects
Performance Data:
- Application to 710 inflammatory bowel disease metagenomes identified 56 species with IBD-associated population structure
- 20 species had genes significantly associated with IBD after controlling for population structure
- Standard relative abundance tests missed the majority of these associations
- Enabled identification of a seven-gene operon in Faecalibacterium prausnitzii involved in fructoselysine utilization
Research Reagent Solutions
The table below details essential materials and their functions for conducting standardized microbiome research.
Table 3: Essential Research Reagents for Microbiome Studies
| Reagent Category | Specific Product/Kit | Function | Considerations for Standardization |
|---|---|---|---|
| DNA Extraction Kits | Qiagen PowerSoil Pro Kit | Gold standard for soil/microbiome DNA extraction | Includes bead beating for mechanical lysis |
| Qiagen Blood & Tissue Kit | Lower-cost alternative for DNA extraction | Lacks bead beating step; affects cell lysis efficiency | |
| Macherey-Nagel NucleoSpin | Cost-effective stool DNA extraction | Includes bead beating; alternative to gold standard | |
| PCR Reagents | Earth Microbiome Project Primers 515F/806R | Amplification of 16S rRNA V4 region | Enables cross-study comparisons |
| Sequencing Standards | 16S rRNA gene sequencing | Microbial community profiling | Primary method for engraftment validation |
| Animal Models | Germ-free zebrafish | Host for controlled microbiome studies | Eliminates confounding native microbiota |
| Pseudo-germ-free animals | Antibiotic-treated recipients for FMT | Requires validation of microbiota depletion |
The standardization crisis in microbiome research represents a critical challenge for translating animal model findings to human applications. Methodological variations in DNA extraction, sample processing, animal model generation, and statistical analysis significantly impact data interpretation and study conclusions. The empirical data presented in this guide demonstrates that specific choices—particularly regarding dissection methods and DNA extraction kits—can substantially alter the identification of microbial biomarkers and diversity measures. To enhance reproducibility and translational potential, researchers should prioritize transparent reporting of methodological details, adoption of established protocols where available, and implementation of sensitivity analyses to evaluate how methodological choices might influence their specific research outcomes. Furthermore, advanced analytical approaches like microSLAM that account for population structure and within-species variation offer promising avenues for uncovering biologically meaningful associations that might be obscured by standard methods. As the field evolves, continued attention to standardization practices will be essential for advancing our understanding of microbiome-host interactions and developing effective microbiome-based therapeutics.
The pursuit of effective therapeutics for human diseases increasingly relies on understanding the complex ecosystem of the human microbiome. However, a significant translational gap persists between findings from animal models and outcomes in human clinical trials. This discrepancy arises from fundamental model-specific limitations, wherein not all human-relevant microbial taxa can colonize animal hosts, and profound physiological differences alter host-microbe interactions. This guide objectively compares the performance of traditional animal models against emerging human-focused methodologies within microbiome and drug development research, providing a framework for selecting physiologically relevant models.
The Core Problem: Divergence Between Animal and Human Physiology
Animal models, while instrumental in foundational biological research, often fail to accurately predict human responses due to inherent physiological and genetic differences. These limitations have direct consequences for the development of drugs and therapies.
Quantitative Evidence of Translational Failure
Analysis of clinical trial data reveals the scope of this problem. The high failure rate of drug candidates underscores a systemic issue in preclinical modeling [84].
Table 1: Analysis of Clinical Trial Failures Attributed to Preclinical Models
| Cause of Failure | Percentage of Failures | Primary Reason for Discrepancy |
|---|---|---|
| Lack of Efficacy in Humans | ~50% | Inability of animal models to fully recapitulate human disease pathophysiology and heterogeneity [84]. |
| Unmanageable Toxicity | ~30% | Species-specific differences in drug metabolism, immune response, and organ physiology [84]. |
| Poor Pharmacokinetics/Commercial | ~20% | Differences in drug absorption, distribution, metabolism, and excretion (ADME) [84]. |
Specific case studies highlight these failures. For example, the drug vupanorsen appeared safe in rodents and monkeys but caused significant liver enzyme elevations and hepatic fat accumulation in humans, halting its development [84]. Similarly, ziritaxestat showed no toxicity in rats and dogs but was terminated after excess deaths occurred in Phase 3 human trials [84].
Limitations in Microbiome Research
The challenges are particularly acute in microbiome science. The assembly of an individual's microbiome begins at birth and is shaped by mode of delivery, diet, and environmental exposures [85]. The "what" that is transmitted—whether live microbial cells, their structural components, or metabolites—fundamentally influences host physiology [86]. Animal models often fail to replicate these nuanced human-specific acquisition pathways and the resulting community structures.
- Early-Life Programming: The neonatal gut microbiome, foundational to immune and metabolic development, is seeded by maternal transmission during vaginal delivery (e.g., Lactobacillus, Prevotella) or from the skin microbiome during C-section (e.g., Staphylococcus) [85]. This early divergence, difficult to model in standard laboratory animals, has long-term health implications [85].
- Microbial Transmission Frameworks: A reconceptualized "4 W" framework (What, Where, Who, When) is necessary to fully describe human microbiome acquisition, moving beyond the imprecise terms of "vertical" and "horizontal" transmission inherited from infectious disease epidemiology [86]. This complexity is rarely captured in animal studies.
Comparative Experimental Models and Methodologies
Researchers have several models at their disposal, each with distinct advantages and limitations for studying host-microbiome interactions.
Model Systems: Protocols and Performance Data
Table 2: Comparison of Experimental Models in Microbiome and Drug Development Research
| Model System | Key Experimental Protocols | Performance & Limitations in Microbiome Studies |
|---|---|---|
| Animal Models(e.g., Rodents) | - Use of germ-free animals gavaged with human donor microbiota.- Genetically modified strains to study disease pathophysiology.- Long-term dosing studies to assess toxicity and efficacy. | Limitations: • Differential Metabolism: Variations in liver enzyme function and immune response lead to poor prediction of human toxicity and efficacy [84] [87].• Inability to Harbor Human Taxa: Many human-specific microbial strains fail to colonize or persist in the murine gut [85].• Lack of Heterogeneity: Genetically identical lines do not reflect human genetic and phenotypic diversity [84]. |
| Organ-on-a-Chip(e.g., Emulate Liver Chip) | - Microfluidic devices lined with living human cells.- Hollow channels simulate vascular and organ lumens.- Can be linked to create multi-organ "human-on-a-chip" systems. | Performance: • Advantage: Better predicted drug-induced liver injury than animal models and hepatic spheroids [87].• Limitation: Difficulties replicating some whole-organ functions and complex, multi-systemic diseases [87]. |
| Ex Vivo Perfused Human Organs(Revalia Bio Platform) | - Donated human organs not suitable for transplant are maintained on perfusion machines.- Drug candidates are introduced, and real-time responses are monitored via imaging, fluid biomarkers, and tissue biopsies [84]. | Performance: • Advantage: Provides a "Human Organ Data Layer" with physiological responses far closer to those in patients, including metabolic and toxicological pathways animal models miss [84] [87].• Advantage: Captures human population heterogeneity as organs come from diverse donors [84]. |
| In Silico & AI Models(Digital Twins, CIVMs) | - Use of AI and quantitative systems pharmacology to generate virtual patient populations.- Models are trained on high-fidelity human data from clinical records and organ perfusion platforms [87]. | Performance: • Advantage: Can simulate clinical trials and forecast unknown disease mechanisms using generative AI [87].• Limitation: Challenging for diseases with poorly understood pathology or behavioral symptoms [87]. |
Visualization of Research Pathways and Concepts
A Framework for Human Microbiome Acquisition
The following diagram illustrates the "4 W" framework for understanding the multifaceted nature of early-life microbiome acquisition, which is often oversimplified in animal models.
Integrated Workflow for Human-Relevant Research
This workflow diagram outlines a modern, integrated approach to microbiome and drug development research that prioritizes human-relevant data.
The Scientist's Toolkit: Essential Research Reagent Solutions
This table details key reagents, technologies, and platforms essential for conducting research in this field, from traditional models to cutting-edge alternatives.
Table 3: Research Reagent Solutions for Microbiome and Translational Research
| Item / Solution | Function & Application | Specific Example / Vendor |
|---|---|---|
| Germ-Free Rodents | Provides a blank slate for studying the effects of introduced human microbiota; foundational for establishing causal relationships in microbiome research. | Various commercial animal suppliers (e.g., Jackson Laboratory, Taconic Biosciences). |
| Multi-Omic Reagents & Kits | Enables comprehensive profiling of the microbiome (genomics), its functional potential (transcriptomics, proteomics), and metabolic output (metabolomics). | Illumina sequencing kits; mass spectrometry reagents; Nephele 3.0 cloud platform for data analysis [88]. |
| Organ-on-a-Chip | Microfluidic devices that emulate human organ physiology for more predictive drug toxicity and efficacy testing in a human-relevant, in-vitro system. | Emulate Organ Chips (Brain, Liver, Lung, etc.), launched from the Wyss Institute at Harvard [87]. |
| Organ Perfusion Systems | Machines that keep donated human organs physiologically active ex vivo, creating a high-fidelity platform for direct human tissue testing without animal intermediaries. | Revalia Bio's proprietary organ perfusion technology for Phase 0 Human Trials [84] [87]. |
| Computational Model Platforms | Tools for creating in-silico models and digital twins to predict human drug metabolism, toxicity, and clinical trial outcomes, integrating diverse data streams. | Critical Path Institute's Qualified Computational In Vitro Models (CIVMs); Revalia Bio's "Rio" software [87]. |
The evidence demonstrates that the limitations of animal models, particularly their inability to fully support human microbial taxa and their physiological divergence from humans, are a primary contributor to the high failure rates in drug development. A paradigm shift is underway, supported by regulatory changes like the FDA Modernization Act 2.0, which encourages alternatives to animal testing [87]. The future of microbiome and therapeutic research lies not in a single model, but in an integrated toolkit that strategically employs human-relevant systems—including organ-on-chip, ex vivo human organ perfusion, and in-silico models—as the backbone of development pipelines. This approach, which prioritizes human biology from the start, promises to improve translational accuracy and deliver safer, more effective therapies to patients faster [84].
The field of microbiome research stands at a critical juncture, where compelling associations between microbial communities and host health outpace our understanding of their causal mechanisms. This disparity stems from a pervasive reproducibility crisis complicated by interdisciplinary methodologies, technical variations, and inconsistent reporting standards across studies [89] [90]. Establishing causal relationships between microbiome configurations and host phenotypes, particularly when translating findings from animal models to human applications, requires unprecedented methodological rigor [14]. The absence of standardized protocols and reporting frameworks has created significant barriers to comparing results across studies, validating biomarkers, and advancing microbiome-based therapeutics into clinical practice [91] [92].
This guide objectively compares existing approaches and synthesizes emerging consensus recommendations for enhancing reproducibility. We focus specifically on experimental designs that bridge animal model systems and human studies, providing a structured framework for implementing rigorous methodologies that yield translatable, reliable findings. By adopting these standardized approaches, researchers can accelerate the transition from descriptive correlation to mechanistic understanding in microbiome science.
Comparative Analysis of Microbiome Study Approaches
The table below evaluates key methodological approaches in microbiome research based on their capacity to support reproducible and translatable findings.
| Approach | Key Features | Reproducibility Strengths | Reproducibility Limitations | Human Translation Potential |
|---|---|---|---|---|
| Human Microbiota-Associated (HMA) Animal Models | Transplantation of human microbial communities into germ-free or antibiotic-pretreated animals [4] | Allows controlled manipulation of microbial variables; Reduces host genetic variability [4] | Donor selection variability [4]; Incomplete recapitulation of human physiology [14] | High (direct human microbial input) [4] |
| Conventional Animal Models | Animals with intact native microbiomes | Models natural microbiome-host interactions; Established protocols | High inter-facility microbiome variation; Vendor/strain-specific effects [89] | Moderate (limited human relevance of native microbiota) [14] |
| Synthetic Microbial Communities (SynComs) | Defined microbial mixtures in fabricated ecosystems [92] [93] | Maximum control over community composition; Highly reproducible across laboratories [92] [93] | Reduced complexity compared to natural communities [92] | Emerging (enables mechanistic studies) [92] |
| Human Observational Studies | Correlation studies in human populations | Direct human relevance; Identifies natural associations | Cannot establish causality; High confounding factor susceptibility [90] | Direct (but correlative only) |
Standardized Experimental Protocols for Enhanced Reproducibility
Establishment of Human Microbiota-Associated (HMA) Models
The successful generation of HMA models requires strict standardization across multiple stages to ensure donor microbiota engraftment and reproducible experimental outcomes [4].
Donor Screening and Selection: Implement comprehensive inclusion and exclusion criteria that minimize microbial variability. Key exclusion factors include: antibiotic exposure within 2-12 months preceding donation; probiotic, prebiotic, or laxative use within 1-2 months; specific dietary patterns; acute or chronic gastrointestinal disorders; recent pathogen infections; and excessive alcohol or tobacco use [4]. For disease-focused studies, confirm diagnoses through clinical manifestations, laboratory tests, and pathological findings according to established diagnostic criteria [4].
Fecal Sample Processing: Collect samples under anaerobic conditions using standardized timeframes from donation to processing. Add cryoprotectants (e.g., glycerol) before preservation at -80°C. Prepare fecal suspensions through sequential dilution, homogenization, and filtration steps. For multi-donor studies, pool samples from multiple qualified donors to increase microbial diversity and representativeness [4].
Recipient Preparation and Inoculation: Use germ-free animals or generate pseudo-germ-free models through antibiotic cocktail administration. For inoculation, a single gavage of standardized fecal suspension (typically 1×10^5 bacterial cells per animal) may suffice, though multiple administrations over several days significantly improve donor microbiota colonization efficiency [4]. Validate engraftment through 16S rRNA gene sequencing comparing recipient microbial profiles to donor inoculum [4].
Multi-Laboratory Validation Using Synthetic Communities
Recent advances in synthetic microbiome research demonstrate how standardized protocols enable reproducibility across independent facilities [92] [93].
Core Protocol Implementation: The EcoFAB 2.0 system provides a fabricated ecosystem with strictly controlled biotic and abiotic factors. Distribute critical components centrally, including: fabricated ecosystem devices, seeds, synthetic community inocula, and growth media from single manufacturing batches. Accompany shipments with detailed protocols featuring embedded annotated videos to minimize technical variation [92] [93].
Synthetic Community Preparation: Utilize publicly available biobanks (e.g., DSMZ) to source validated bacterial isolates. Prepare SynComs using optical density-to-colony forming unit conversions to ensure precise cell numbers in final inocula. Ship concentrated stocks on dry ice with standardized resuscitation protocols [92] [93].
Cross-Laboratory Quality Control: Implement uniform sterility testing at multiple timepoints using standardized culture conditions and data collection templates. Centralize sequencing and metabolomic analyses to minimize analytical variation. Use environmental data loggers to monitor growth chamber conditions including temperature, humidity, and light intensity across facilities [92] [93].
Reporting Standards and Data Analysis Frameworks
The STORMS Checklist for Comprehensive Reporting
The Strengthening The Organization and Reporting of Microbiome Studies (STORMS) checklist provides a structured framework for reporting microbiome research [90]. This tool, developed through a multidisciplinary consensus process, adapts guidelines from observational and genetic epidemiology studies while incorporating new elements specific to microbiome research.
Core Reporting Components:
- Abstract: Clearly state study design, sequencing methods, and body sites sampled [90]
- Introduction: Describe background evidence and state specific hypotheses or exploratory objectives [90]
- Methods: Detail participant characteristics (environment, lifestyle, diet, demographics, geography), temporal context of recruitment, eligibility criteria with specific inclusion/exclusion criteria, antibiotic exposure information, and sample size justification with reasons for exclusions [90]
- Results: Report data preprocessing methods, batch effect correction approaches, and statistical methods tailored for compositional data [90]
The STORMS checklist emphasizes documentation of factors that influence microbiome composition, including specimen collection methods, and requires transparent reporting of computational and statistical methods to enable independent verification of findings [90].
Standardized Alpha Diversity Assessment
The selection and interpretation of alpha diversity metrics significantly impact study conclusions. Current guidelines recommend a comprehensive approach that captures complementary aspects of microbial communities [94].
Alpha Diversity Metric Categories:
- Richness: Quantifies the number of distinct microbial taxa (e.g., Chao1, ACE, Observed ASVs) [94]
- Phylogenetic Diversity: Incorporates evolutionary relationships among taxa (Faith's Phylogenetic Diversity) [94]
- Dominance/Evenness: Measures the distribution of taxon abundances (e.g., Berger-Parker, Simpson, ENSPIE) [94]
- Information Metrics: Derived from information theory (e.g., Shannon, Pielou, Brillouin) [94]
Rather than selecting a single metric, researchers should report a panel that includes richness, phylogenetic diversity, entropy, dominance measures, and estimates of unobserved microbes to provide a comprehensive characterization of samples [94]. This multi-faceted approach prevents biased interpretations and enables more meaningful cross-study comparisons.
Visualization of Standardized Workflows
Experimental Standardization Logic
HMA Model Generation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below catalogues critical reagents and materials that facilitate reproducible microbiome research based on validated experimental approaches.
| Category | Specific Reagent/Material | Function/Application | Standardization Benefit |
|---|---|---|---|
| Animal Models | Germ-free mice/rats | HMA model recipients | Eliminates confounding native microbiota [4] |
| Antibiotic Cocktails | Ampicillin, vancomycin, neomycin, metronidazole | Pseudo-germ-free model generation | Depletes native microbiota for human microbiota engraftment [4] |
| Fabricated Ecosystems | EcoFAB 2.0 devices | Controlled plant-microbiome studies | Standardized sterile habitats [92] [93] |
| Synthetic Communities | Defined bacterial isolate collections (e.g., DSMZ SynComs) | Reductionist community studies | Reproducible, defined starting communities [92] [93] |
| Cryoprotectants | Glycerol (20%) | Microbial viability preservation | Maintains consistent inoculum viability [4] |
| DNA Extraction Kits | Standardized extraction protocols | Microbial community profiling | Minimizes technical variation in DNA recovery [89] |
| Reference Databases | Greengenes, SILVA | Taxonomic classification | Standardized taxonomic assignment [89] |
The path to improved reproducibility in microbiome research requires concerted implementation of rigorous design and reporting practices across the scientific community. The consensus recommendations presented in this guide provide a framework for enhancing the reliability and translatability of microbiome studies, particularly those bridging animal models and human research. By adopting standardized experimental approaches, comprehensive reporting checklists, and validated analytical methods, researchers can overcome current reproducibility challenges and accelerate the development of microbiome-based diagnostics and therapeutics. The integration of these practices will strengthen causal inference in host-microbiome interactions and foster greater confidence in research outcomes across the field.
From Model to Medicine: Strategies for Validating Biomarkers and Ensuring Clinical Relevance
In the field of microbiome research, the transition from observational studies to clinically actionable insights requires robust analytical frameworks that can handle the unique challenges of metagenomic data. Machine learning (ML) applied to microbiome data faces significant hurdles, including large technical variation, compositionality, sparsity, and high dimensionality. The Statistical Inference of Associations between Microbial Communities And host phenoTypes (SIAMCAT) R package addresses these challenges by providing a specialized toolbox for ML-based comparative metagenomics. Developed specifically for case-control microbiome studies, SIAMCAT standardizes the process of building, evaluating, and interpreting ML models, thereby facilitating more reliable and reproducible microbiome biomarker discovery. This guide examines SIAMCAT's role in enhancing cross-validation and comparative analysis within microbiome research, objectively evaluating its performance against other methodologies and detailing the experimental protocols that underpin its application.
Core SIAMCAT Workflow and Technical Architecture
Standardized Machine Learning Pipeline
SIAMCAT provides a comprehensive ML workflow tailored to metagenomic data characteristics. The standard pipeline incorporates data preprocessing, statistical association testing, machine learning modeling, and result interpretation [95]. This end-to-end approach ensures that analyses properly account for the compositionality and sparsity inherent in microbiome data.
The package interfaces seamlessly with the popular phyloseq R package for data input and integrates core ML functionality through the mlr package [95]. Key workflow steps include unsupervised abundance and prevalence filtering, data normalization specifically adapted for metagenomic data, and implementation of various ML algorithms including LASSO, Elastic Net, and Random Forest.
Advanced Cross-Validation Implementation
SIAMCAT implements rigorous cross-validation schemes to prevent overoptimistic performance estimates. The create.data.split function enables proper setup of cross-validation, while train.model and make.predictions functions handle model training and application to unseen data [95]. Performance evaluation through evaluate.predictions provides standardized assessment metrics, with the Area Under the Receiver Operating Characteristic Curve (AUROC) serving as the primary performance metric.
For cross-study applications, SIAMCAT incorporates a novel control augmentation strategy that addresses the problem of model performance degradation when transferred across studies. This approach involves sampling additional external controls during cross-validation, which has been shown to improve disease specificity and restore model accuracy in cross-disease comparisons [95].
Performance Benchmarking: SIAMCAT vs. Alternative Approaches
Within-Study vs. Cross-Study Classification Performance
Table 1: Performance Comparison of Microbiome-Based Machine Learning Models
| Disease Context | Data Type | Within-Study CV (Average AUC) | Cross-Study Validation (Average AUC) | Performance Drop | Key Findings |
|---|---|---|---|---|---|
| Parkinson's Disease (22 studies) | 16S rRNA | 72.3% (± 11.7) | ~61% | ~11.3% | High variability between studies; models not directly transferable [96] |
| Parkinson's Disease (22 studies) | Shotgun Metagenomics | 78.3% (± 6.5) | ~61% | ~17.3% | Better within-study performance than 16S; similar cross-study degradation [96] |
| Multi-disease Meta-analysis | Shotgun Metagenomics | Varies by disease | Improved with control augmentation | Restored to usable levels | Control augmentation strategy improved disease specificity [95] |
| Inflammatory Bowel Disease | Shotgun Metagenomics | 84.0% (with confounder) | 76.0% (confounder-adjusted) | 8.0% due to confounder | Country of origin confounded disease associations [95] |
Differential Abundance Method Performance
Table 2: Benchmarking of Statistical Methods for Microbiome Data Analysis
| Method Category | Representative Methods | False Discovery Rate Control | Sensitivity | Confounder Adjustment Capability |
|---|---|---|---|---|
| Classical Statistical Methods | Wilcoxon test, t-test, linear models | Proper control | Relatively high | Effective when properly adjusted [97] |
| RNA-Seq Adapted Methods | limma, DESeq2 | Variable | Moderate | Limited effectiveness [97] |
| Microbiome-Specific Methods | fastANCOM | Proper control | Moderate | Effective when properly adjusted [97] |
| Other Microbiome Methods | Multiple others | Poor control | Variable | Limited effectiveness [97] |
Recent benchmarking studies demonstrate that only classic statistical methods (linear models, Wilcoxon test, t-test), limma, and fastANCOM properly control false discoveries while maintaining reasonable sensitivity [97]. These performance characteristics are crucial for generating reliable biomarkers that can translate across studies.
Experimental Protocols for SIAMCAT Implementation
Standardized ML Analysis Workflow
The following detailed protocol outlines a typical SIAMCAT analysis for comparative metagenomics:
Data Input and Preparation: Import feature matrices (taxonomic or functional abundances), group labels (case-control information), and optional metadata using SIAMCAT's compatibility with the
phyloseqpackage [95].Data Preprocessing:
- Apply unsupervised abundance and prevalence filtering (
filter.features) - Implement data normalization using methods tailored for metagenomic data (
normalize.features) - Address zero-inflation and compositionality inherent in microbiome data
- Apply unsupervised abundance and prevalence filtering (
Association Analysis:
- Perform univariate association testing using non-parametric Wilcoxon test (
check.associations) - Calculate generalized fold change as a non-parametric effect size measure
- Visualize distributions, significance, and effect sizes for individual microbial features
- Perform univariate association testing using non-parametric Wilcoxon test (
Machine Learning Modeling:
- Establish cross-validation scheme (
create.data.split) - Train models using implemented algorithms (
train.model) - Make predictions on held-out samples (
make.predictions) - Evaluate performance using AUROC and other metrics (
evaluate.predictions)
- Establish cross-validation scheme (
Model Interpretation:
- Generate feature importance rankings (
model.interpretation.plot) - Visualize normalized feature distributions alongside metadata
- Identify key predictive taxa or functional features
- Generate feature importance rankings (
Cross-Study Validation Protocol
For cross-study applications, the following specialized protocol is recommended:
Initial Within-Study Assessment: Train and evaluate models on individual studies using rigorous cross-validation.
Naive Cross-Study Application: Apply study-specific models to all other available studies without modification to establish baseline cross-study performance.
Control Augmentation Implementation:
- Sample additional control samples from external studies during cross-validation
- Maintain appropriate case-control balance across diverse cohorts
- Retrain models with augmented training sets
Disease Specificity Assessment: Evaluate augmented models against microbiomes from other disease conditions to verify specificity of identified biomarkers [96].
Confounder Analysis Protocol
SIAMCAT provides specific functionality for detecting and addressing confounding:
Confounder Identification:
- Test associations between metadata variables and group labels using Fisher's exact test (categorical) or Wilcoxon test (continuous)
- Identify potential confounders that are unevenly distributed between cases and controls
Confounder Impact Quantification:
- Use
check.confounderfunction to visualize variance explained by label versus confounder for each feature - Compare association results with and without adjusting for confounders
- Use
Confounder-Adjusted Analysis:
- Stratify analysis by confounder levels where appropriate
- Include confounders as covariates in statistical models
- Re-evaluate ML performance after addressing confounding [95]
Visualization and Interpretation Framework
SIAMCAT Machine Learning Workflow: This diagram illustrates the standardized pipeline for comparative metagenomics analysis, from data input through final interpretation.
Table 3: Essential Research Reagents and Computational Tools for Microbiome ML
| Tool/Resource | Category | Primary Function | Application in Comparative Metagenomics |
|---|---|---|---|
| SIAMCAT | Machine Learning Toolbox | ML-based comparative metagenomics | End-to-end workflow for case-control microbiome studies [95] |
| phyloseq | Data Structure | Microbiome data organization | Data import and compatibility with SIAMCAT [95] |
| curatedMetagenomicData | Data Resource | Standardized metagenomic datasets | Access to processed, curated datasets for analysis [95] |
| MetaPhlAn | Taxonomic Profiling | Species-level abundance quantification | Generate input feature matrices for SIAMCAT [96] [98] |
| HUMAnN | Functional Profiling | Metabolic pathway abundance | Functional input data for SIAMCAT [99] |
| MMUPHin | Batch Correction | Cross-study normalization | Address batch effects in meta-analyses [98] |
| MaAsLin2 | Statistical Analysis | Multivariate association testing | Complementary differential abundance testing [98] [99] |
| MicrobiomeStatPlots | Visualization | Advanced plotting capabilities | Enhanced visualization beyond SIAMCAT's built-in plots [99] |
Applications in Disease Research and Biomarker Discovery
Neurodegenerative Disease Applications
In Parkinson's disease research, SIAMCAT-enabled meta-analysis of 4,489 samples across 22 studies revealed that while within-study classification showed promising accuracy (average AUC 71.9% for 16S data, 78.3% for shotgun metagenomics), models transferred poorly across studies (average AUC ~61%) [96]. This highlights both the challenge of cross-study generalization and the need for methods like control augmentation implemented in SIAMCAT.
Similar approaches have been applied to Alzheimer's disease, where microbiome-based ML models successfully predicted population-level disease incidence based on gut microbiome profiles (mean AUC 0.889-0.927) [100]. These models identified specific taxa including Escherichia coli, Haemophilus, and Akkermansia as reproducibly associated with disease incidence across datasets.
Inflammatory and Metabolic Disease Insights
SIAMCAT has been instrumental in revealing disease-specific versus shared microbiome biomarkers across conditions. In inflammatory bowel disease, the toolbox helped identify how country of origin confounded disease associations, with differences between Danish and Spanish samples explaining spurious associations for species like Dorea formicigenerans [95].
For obesity research, integrative metagenomic analysis of 1,351 samples using SIAMCAT and complementary tools identified 38 bacterial species and 1 archaeal species significantly altered in obesity, including decreased Akkermansia muciniphila and increased Ruminococcus gnavus [98]. These findings demonstrate how ML-driven meta-analysis can yield robust biomarkers across diverse populations.
SIAMCAT represents a significant advancement in standardizing machine learning applications for comparative metagenomics. The toolbox addresses critical challenges in microbiome data analysis through rigorous cross-validation, confounder detection, and specialized normalization methods. Performance benchmarks demonstrate that while microbiome-based ML models often show excellent within-study performance, their cross-study application remains challenging without strategies like control augmentation.
The most successful applications of SIAMCAT combine its standardized ML workflows with complementary tools for batch correction, functional analysis, and visualization. As microbiome research progresses toward clinical applications, frameworks like SIAMCAT that emphasize reproducibility, proper validation, and confounder adjustment will be essential for translating microbial signatures into reliable biomarkers for disease diagnosis and therapeutic development.
Researchers should implement the detailed experimental protocols outlined here, particularly the cross-validation and control augmentation strategies, to maximize the robustness and generalizability of their microbiome machine learning models.
In the evolving field of microbiome research, a significant challenge persists in translating findings from animal models to human therapeutic applications. Control augmentation emerges as a sophisticated methodological strategy designed to enhance the disease specificity of experimental models and reduce the false positive outcomes that often plague preclinical studies. This approach involves the systematic enhancement of control arms in experiments through advanced techniques such as synthetic data generation, humanized animal models, and engineered microphysiological systems. These augmented controls create more robust, human-relevant baselines against which disease states and therapeutic interventions can be evaluated with greater precision.
The fundamental premise of control augmentation addresses a critical gap in conventional research methodologies. Traditional animal models, while invaluable, often exhibit limited translational fidelity to human disease states due to inherent physiological differences and simplified microbial ecosystems. Control augmentation strategically strengthens these models by incorporating human-derived microbial communities, generating synthetic data to address class imbalances, and implementing engineered systems that better recapitulate human physiology. This multi-faceted approach enables researchers to distinguish between model-specific artifacts and genuine pathological mechanisms with enhanced resolution, ultimately accelerating the development of targeted microbiome-based therapies.
Comparative Analysis of Control Augmentation Strategies
Control augmentation encompasses several distinct methodological approaches, each with specific advantages, implementation requirements, and performance characteristics. The table below provides a systematic comparison of the primary control augmentation strategies currently advancing microbiome research.
Table 1: Comparative Analysis of Control Augmentation Strategies in Microbiome Research
| Augmentation Strategy | Key Features | Implementation Complexity | Disease Specificity Improvement | False Positive Reduction Potential |
|---|---|---|---|---|
| Human Microbiota-Associated (HMA) Models | Transplantation of human microbial communities into germ-free or antibiotic-pretreated animals [4] | High (requires specialized facilities, stringent donor screening, engraftment validation) | Moderate to High (human-relevant microbial patterns) | High (reduces model-specific microbial artifacts) |
| Synthetic Data Augmentation | Generation of artificial datasets using SMOTE, ADASYN, or Deep-CTGANs to address class imbalance [101] | Moderate (technical expertise in machine learning required) | Variable (depends on data fidelity and task) | High (mitigates bias toward majority classes) |
| Organ-on-Chip Technologies | Microfluidic devices mimicking human intestinal physiology with oxygen gradients, flow rates, and human cell cultures [102] | High (specialized fabrication, multidisciplinary expertise) | High (human physiological relevance) | High (controlled microenvironment reduces confounding variables) |
| Fecal Microbiota Transplantation (FMT) Standardization | Standardized protocols for donor screening, sample processing, and transplantation regimens [103] [4] | Moderate to High (standardization challenges across labs) | Moderate (improved consistency across experiments) | Moderate (reduces variability in control baselines) |
The comparative analysis reveals that each control augmentation strategy offers distinct advantages for different research contexts. HMA models provide perhaps the most direct method for humanizing animal studies by establishing human-relevant microbial ecosystems in controlled laboratory settings. The implementation requires germ-free facilities and rigorous donor screening protocols, excluding donors with recent antibiotic exposure (within 1-2 months), laxative use, or specific medical conditions to ensure microbial integrity [4]. The resulting models demonstrate significantly improved translational potential for studying human-specific host-microbe interactions.
Synthetic data augmentation addresses a fundamentally different challenge – the statistical limitations inherent in analyzing complex, high-dimensional microbiome datasets. Techniques like Deep Conditional Tabular Generative Adversarial Networks (Deep-CTGANs) integrated with ResNet architectures generate synthetic samples that preserve the multivariate relationships in real microbiome data while addressing class imbalances [101]. This approach has demonstrated impressive results in disease prediction tasks, with models trained on synthetic data achieving accuracies exceeding 99% when validated on real clinical datasets [101]. The TabNet architecture, with its sequential attention mechanism, has proven particularly effective for handling these augmented tabular datasets.
Organ-on-chip technologies represent perhaps the most technologically advanced control augmentation strategy, enabling researchers to bypass animal models entirely in certain investigative contexts. These microphysiological systems incorporate human intestinal cells under continuous nutrient flow, with some advanced models featuring peristaltic motions and oxygen gradients that sustain even obligate anaerobic bacteria for extended periods [102]. This capacity to maintain complex microbial communities while precisely controlling the physical and chemical microenvironment significantly enhances disease specificity by eliminating species-specific physiological confounding factors.
Experimental Protocols and Methodologies
Establishment of Human Microbiota-Associated (HMA) Models
The successful implementation of HMA models requires meticulous attention to donor selection, recipient preparation, and transplantation protocols. The following standardized protocol has been validated across multiple research institutions:
Donor Screening and Selection: Implement comprehensive exclusion criteria including recent antibiotic exposure (within 1-2 months), probiotic or laxative use, active neuropsychiatric disorders, excessive alcohol consumption, and smoking [4]. For disease-specific studies, include only donors meeting clinical diagnostic criteria for the condition of interest, while excluding those with comorbidities that might confound results.
Fecal Sample Processing: Collect fresh fecal samples under anaerobic conditions using oxygen-free containers. Process samples immediately upon collection by homogenizing in sterile phosphate-buffered saline with 10% glycerol as a cryoprotectant. Filter through mesh screens to remove large particulate matter, then aliquot and store at -80°C if not used immediately [4]. Pool samples from multiple donors to capture microbial diversity while controlling for inter-individual variation.
Recipient Preparation: Utilize 8-12 week old germ-free mice or antibiotic-induced pseudo-germ-free models. For antibiotic depletion, administer a cocktail of ampicillin (1 mg/mL), vancomycin (0.5 mg/mL), neomycin (1 mg/mL), and metronidazole (1 mg/mL) in drinking water for 2-3 weeks prior to transplantation [4].
Transplantation Protocol: Administer 200μL of standardized fecal suspension (100mg/mL) via oral gavage once daily for 3-5 consecutive days. Monitor engraftment efficiency through 16S rRNA sequencing of fecal samples collected at regular intervals post-transplantation, comparing microbial profiles to the original donor material [4].
Table 2: Essential Research Reagents for HMA Model Establishment
| Reagent/Equipment | Specification | Function in Protocol |
|---|---|---|
| Anaerobic Chamber | Oxygen concentration <1% | Maintains viability of obligate anaerobic bacteria during sample processing |
| Cryoprotectant | 10-20% Glycerol in PBS | Preserves microbial viability during frozen storage |
| Antibiotic Cocktail | Ampicillin, Vancomycin, Neomycin, Metronidazole | Depletes indigenous microbiota in recipient animals |
| DNA Extraction Kit | Optimized for fecal samples (e.g., QIAamp PowerFecal Pro) | Extracts high-quality microbial DNA for engraftment validation |
| 16S rRNA Primers | Targeting V3-V4 hypervariable region | Amplifies microbial genetic material for community profiling |
Synthetic Data Generation for Microbiome Studies
The implementation of synthetic data augmentation requires careful selection of generation techniques appropriate for the specific analytical task and dataset characteristics:
Data Preprocessing: Normalize microbiome abundance data using centered log-ratio transformation to address compositionality. Remove low-prevalence features present in less than 10% of samples, then impute missing values using Bayesian-multiplicative treatment.
Classical Oversampling: Apply Synthetic Minority Oversampling Technique (SMOTE) or Adaptive Synthetic Sampling (ADASYN) for smaller datasets (<1000 samples). These generate synthetic minority class examples by interpolating between existing minority class instances in feature space [101]. Validate synthetic sample quality by visualizing principal components analysis plots comparing real and synthetic distributions.
Deep Generative Models: Implement Deep Conditional Tabular Generative Adversarial Networks (Deep-CTGANs) integrated with ResNet architectures for larger, more complex datasets. This approach effectively captures non-linear dependencies and multi-modal distributions in microbiome data [101]. Train with class-specific conditioning vectors to ensure balanced generation across diagnostic categories.
Validation Framework: Employ the Train on Synthetic, Test on Real (TSTR) validation approach, comparing performance to models trained exclusively on original data. Calculate similarity scores using metrics like the TabSynDex framework, which evaluates fidelity, diversity, and utility of synthetic datasets [101]. Successful generation typically achieves similarity scores of 84-87% between real and synthetic data distributions.
Organ-on-Chip Microbiome Models
Advanced gut-on-chip technologies require specialized fabrication and culture techniques:
Device Fabrication: Utilize polydimethylsiloxane (PDMS) chips with two parallel microchannels separated by a porous membrane (5-10μm pores). The upper channel accommodates intestinal epithelial cells, while the lower channel serves as a vascular compartment [102]. Incorporate lateral vacuum chambers to apply cyclic suction (10-15% strain, 0.15Hz) that mimics peristaltic motions.
Cell Culture: Seed human intestinal epithelial cells (Caco-2 or organoid-derived) at high density (≥1×10^6 cells/cm²) in the upper channel. Differentiate under continuous flow (30-100μL/hour) of complete medium for 7-14 days until tight junction formation and polarization are confirmed via transepithelial electrical resistance (TEER ≥500Ω·cm²).
Microbiota Introduction: Prepare anaerobic bacterial suspensions from fresh fecal samples in pre-reduced PBS. Introduce 50-100μL of bacterial suspension (OD600=1.0) into the luminal channel under anaerobic conditions maintained through continuous nitrogen flushing [102]. For complex community studies, incorporate an oxygen gradient system with <1% oxygen in luminal regions and >10% oxygen in basal regions to support both aerobic host cells and anaerobic microbes.
Parameter Monitoring: Measure TEER regularly to monitor barrier integrity. Sample effluent from both channels for cytokine analysis (IL-6, IL-8, TNF-α) and microbial composition (16S rRNA sequencing). Perform high-resolution microscopy at predetermined intervals to visualize microbial localization and host-cell interactions.
Quantitative Performance Assessment
The efficacy of control augmentation strategies must be evaluated through rigorous quantitative assessment across multiple performance dimensions. The following data, compiled from recent studies, demonstrates the measurable improvements achievable through these methodologies.
Table 3: Performance Metrics of Control Augmentation in Disease Modeling
| Model System | Disease Application | Sensitivity Improvement | Specificity Improvement | False Positive Reduction | Key Metric |
|---|---|---|---|---|---|
| HMA Mouse Model | PCOS [103] | N/A | N/A | 35-40% | Reduced beta diversity discrepancies between model and human patients |
| TabNet with Synthetic Data | Kidney Disease [101] | +4.7% | +3.9% | 42% | 99.4% accuracy with synthetic training data |
| Gut-on-Chip with Microbiota | Inflammatory Response [102] | N/A | N/A | 60-70% | Improved distinction between commensal and pathogenic inflammatory responses |
| Ensemble CNN with Augmentation | Brain Tumor Segmentation [104] | +5.2% | +3.8% | 28% | Dice score improvement from 0.74 to 0.79 with synthetic tumor augmentation |
The performance data reveals consistent improvements across multiple applications and model systems. In PCOS research, HMA models demonstrated significantly reduced beta diversity discrepancies between animal models and human patients, addressing a key limitation in translational research [103]. The incorporation of human microbial communities into animal models created more physiologically relevant systems for studying the gut-brain-ovary axis, potentially explaining previously inconsistent therapeutic responses between preclinical and clinical studies.
In machine learning applications, TabNet classifiers trained on synthetically augmented datasets achieved remarkable accuracy exceeding 99% on real clinical data for disease prediction tasks [101]. The sequential attention mechanism in TabNet architecture proved particularly effective for handling the complex feature interactions in augmented microbiome datasets. Importantly, these models demonstrated substantially improved performance on minority classes, with false positive rates reduced by up to 42% compared to models trained on original imbalanced datasets.
Organ-on-chip systems incorporating human microbiomes showed the most dramatic improvements in reducing false positive responses, particularly in distinguishing between physiological inflammatory signaling and genuine pathological states [102]. The controlled microenvironments in these systems, with precise regulation of oxygen gradients, fluid flow, and mechanical strain, eliminated approximately 60-70% of false positive inflammatory responses observed in conventional cell culture systems. This enhanced specificity is critical for accurately evaluating potential therapeutic interventions.
Integration Framework and Future Directions
The strategic integration of multiple control augmentation approaches presents a promising path forward for enhancing disease specificity in microbiome research. The conceptual framework below illustrates how these methodologies can be combined to create progressively more human-relevant research models.
Diagram 1: Control Augmentation Integration Framework
The integration framework illustrates the synergistic relationship between different control augmentation strategies. HMA models enhance traditional animal models by incorporating human-relevant microbial ecosystems, while simultaneously providing validation benchmarks for organ-on-chip systems. Synthetic data augmentation both informs traditional models by addressing class imbalances and optimizes the integrated validation platform through improved algorithmic performance. This multidisciplinary approach creates a virtuous cycle of refinement that progressively enhances disease specificity and reduces false positives across the research ecosystem.
Future developments in control augmentation will likely focus on several key areas. First, the standardization of HMA protocols across research institutions will be critical for improving reproducibility and enabling meta-analyses [4]. This includes consensus on donor exclusion criteria, sample processing methodologies, and engraftment validation metrics. Second, advances in generative AI will enable more sophisticated synthetic data generation that captures longitudinal dynamics and cross-domain relationships in microbiome-host interactions [101]. Finally, the integration of multi-organ microphysiological systems will create increasingly comprehensive human surrogates for studying systemic diseases with microbiome involvement [102].
The continued refinement and implementation of control augmentation strategies represents a paradigm shift in microbiome research methodology. By systematically addressing the limitations of traditional models through humanization, statistical optimization, and physiological engineering, these approaches promise to significantly accelerate the development of targeted microbiome-based therapeutics with enhanced efficacy and reduced adverse effects in human populations.
The human gut microbiome, a complex ecosystem of bacteria, viruses, fungi, and archaea, plays a pivotal role in maintaining host health and mediating disease pathogenesis. Recent advances in high-throughput sequencing technologies and computational biology have enabled researchers to move beyond single-disease studies to conduct comprehensive cross-disease analyses. These investigations aim to identify both shared microbial signatures that transcend diagnostic boundaries and disease-specific microbial profiles that offer unique diagnostic and therapeutic insights. The identification of such signatures is complicated by significant methodological challenges, including technical variations across studies, population heterogeneity, and the compositional nature of microbiome data [105] [106] [107].
Understanding both common and distinct microbial patterns across diseases provides a crucial foundation for developing novel diagnostic tools, targeted therapies, and personalized treatment approaches. This comparative analysis synthesizes findings from recent large-scale studies to elucidate microbial signatures across gastrointestinal disorders, neurological conditions, metabolic diseases, and autoimmune conditions, while also examining the experimental frameworks that enable these insights.
Methodological Frameworks for Cross-Disease Microbiome Analysis
Meta-Analysis Approaches and Machine Learning Platforms
Robust cross-disease comparison requires specialized computational frameworks that can integrate data from multiple studies while accounting for technical and biological heterogeneity. Several sophisticated platforms have been developed specifically for this purpose:
SIAMCAT (Statistical Inference of Associations between Microbial Communities And host phenoTypes): A comprehensive machine learning toolbox that performs comparative metagenomics using normalization methods adapted for microbiome data's unique characteristics, including compositionality, zero-inflation, and non-Gaussian distributions. It includes functionality for confounder analysis and cross-validation to ensure robust model performance [106].
Melody: A novel meta-analysis framework specifically designed to address the compositional structure of microbiome data, which generates, harmonizes, and combines study-specific summary statistics to identify generalizable microbial signatures. This approach avoids common pitfalls like rarefaction and zero-imputation while recovering absolute abundance associations [107].
MMUPHin (Meta-analysis Methods with Uniform Pipeline for Heterogeneity in Microbiome Studies): This tool enables cross-cohort identification of microbial signatures by performing meta-analysis with random effects models to identify consistent effects across diverse populations. It has been successfully applied to identify core species sets associated with specific diseases [105].
Standardized Processing and Multi-Omic Integration
Beyond specific tools, comprehensive workflows have been established for cross-disease comparisons:
Figure 1: Comprehensive Workflow for Cross-Disease Microbiome Analysis
Recent approaches have emphasized consistent bioinformatics processing across studies using uniform pipelines for quality control, taxonomic profiling with tools like MetaPhlAn, and batch effect correction [105] [108]. Multi-omic integration frameworks have been developed to jointly analyze host transcriptomic data with microbiome profiles, enabling identification of host gene-microbiome associations that depict both shared and disease-specific patterns [109]. These integrated analyses utilize methods like sparse canonical correlation analysis (sparse CCA) and LASSO regression to identify biologically meaningful associations amidst high-dimensional data [109].
Comparative Analysis of Microbial Signatures Across Disease Categories
Gastrointestinal Disorders
Inflammatory bowel disease (IBD) and colorectal cancer (CRC) represent gastrointestinal disorders with both overlapping and distinct microbial signatures:
Table 1: Microbial Signatures in Gastrointestinal Disorders
| Disease | Shared Microbial Features | Disease-Specific Features | Functional Characteristics |
|---|---|---|---|
| Crohn's Disease (CD) | • Enterococcus faecium (enriched)• Bifidobacterium spp. (enriched)• Reduced α-diversity• Depletion of SCFA-producing bacteria (Faecalibacterium prausnitzii, Eubacterium spp.) | • Escherichia coli (specifically enriched)• ESKAPE pathogens: Klebsiella pneumoniae, Staphylococcus aureus• Specific antibiotic resistance genes (efflux pumps)• AIEC virulence factors | • Increased antibiotic resistance potential• Distinct virome changes correlated with bacteriome shifts• Multi-drug resistant bacteria enrichment |
| Ulcerative Colitis (UC) | • Enterococcus faecium (enriched)• Bifidobacterium spp. (enriched)• Reduced α-diversity• Depletion of SCFA-producing bacteria | • Saccharomyces paradoxus (enriched in fungi)• Less pronounced resistome changes compared to CD | • Less extensive antibiotic resistance• Different fungal associations |
| Colorectal Cancer (CRC) | • Depletion of SCFA-producing bacteria | • Parvimonas micra• Clostridium symbiosum• Peptostreptococcus stomatis• Bacteroides fragilis• Gemella morbillorum• Fusobacterium nucleatum | • Pro-inflammatory microbial environment• Microbial communities implicated in carcinogenesis |
The multi-biome signatures and their interactions in UC and CD show high similarities across different geographical populations (Japan, US, Spain, Netherlands, and China), underscoring the robustness of these findings [110]. Machine learning models based on these bacterial signatures can distinguish patients from controls with high accuracy (AUC = 0.87-0.88), maintaining moderate performance in external validation (AUC = 0.62-0.90 across different cohorts) [110].
Neurological, Metabolic, and Autoimmune Disorders
Cross-disease comparisons have revealed unexpected microbial similarities across seemingly unrelated disease categories:
Table 2: Cross-Disease Microbial Similarities Across Different Disorder Categories
| Disease Pair | Similarity Level | Key Shared Microbial Features | Potential Mechanisms |
|---|---|---|---|
| CD vs. CRC | High | Shared enrichment of certain pathobionts | • Immune system modulation• Gut barrier disruption• Chronic inflammation |
| Parkinson's vs. T2D | High | Similar patterns of microbial dysbiosis | • Gut-brain axis disruption• Metabolic pathway alterations• Systemic inflammation |
| Schizophrenia vs. T2D | High | Overlapping dysbiosis patterns | • Gut-brain axis communication• Neuroendocrine signaling alterations |
| AD vs. IBD | Inverse correlation | Opposite microbial abundance patterns | • Distinct immune activation patterns• Different metabolic priorities• Opposing inflammatory responses |
These cross-disease relationships were consistent at both the microbial species level and functional gene level, suggesting they are driven by both the enrichment of pathogenic microbes and depletion of beneficial microbes [108]. The discovery of these shared patterns across traditionally distinct disease categories suggests potential for drug repositioning and novel therapeutic approaches that target shared microbial mechanisms [108].
Experimental Models and Validation Frameworks
Human Microbiota-Associated (HMA) Animal Models
HMA models have become indispensable tools for investigating microbe-host interactions and establishing causal relationships:
- Recipient Preparation: Use of germ-free animals or antibiotic-induced pseudo-germ-free models to create microbial niches for human microbiota engraftment [4]
- Donor Screening Criteria: Exclusion of donors with recent antibiotic, probiotic, or laxative use; comprehensive health screening to eliminate gastrointestinal disorders, recent infections, and chronic illnesses that alter gut microbiome composition [4]
- Transplantation Protocols: Fecal microbiota transplantation (FMT) with single or multiple gavage administrations; multiple frequencies and longer FMT durations significantly improve donor microbiota colonization efficiency [4]
- Engraftment Validation: Microbial community profiling via 16S rRNA gene sequencing represents the primary method for analyzing microbiome composition and verifying microbiota engraftment efficacy [4]
Microbial Risk Score (MRS) Development
For clinical translation, microbial signatures have been integrated into quantitative risk assessment tools:
- MRSα Construction: Based on α-diversity of sub-communities of core species, providing better validation and interpretability compared to summation methods or machine learning algorithms [105]
- CRC-Specific MRS: Incorporating six core species (Parvimonas micra, Clostridium symbiosum, Peptostreptococcus stomatis, Bacteroides fragilis, Gemella morbillorum, and Fusobacterium nucleatum) demonstrated predictive AUC values between 0.619 and 0.824 across eight validation cohorts [105]
- Community-Based Approach: Leverages ecological characteristics of gut microbes by calculating diversity metrics on identified sub-communities of disease-related microbial signatures [105]
Research Reagent Solutions for Microbial Signature Studies
Table 3: Essential Research Reagents and Platforms for Microbial Signature Discovery
| Reagent/Platform | Primary Function | Application in Signature Studies |
|---|---|---|
| MetaPhlAn | Taxonomic profiling from metagenomic data | Species-level annotation across studies; used with curatedMetagenomicData package |
| SIAMCAT | Machine learning-based microbiome analysis | Case-control classification; cross-study validation; confounder analysis |
| Melody | Meta-analysis of microbiome association studies | Identifying generalizable microbial signatures; handling compositionality |
| MMUPHin | Cross-study microbial signature identification | Meta-analysis with random effects models; batch effect correction |
| curatedMetagenomicData R package | Standardized access to processed microbiome data | Cross-study comparisons with uniform processing pipelines |
| Antibiotic Cocktails | Depletion of indigenous microbiota | Creation of pseudo-germ-free animal models for HMA studies |
| Cryopreservation Media | Preservation of fecal samples | Maintain microbial viability for transplantation studies |
Host-Microbe Interaction Pathways in Health and Disease
The relationship between host physiology and microbial communities involves complex, bidirectional communication networks:
Figure 2: Host-Microbe Interaction Pathways in Cross-Disease Patterns
Research has revealed that a common set of host genes and pathways implicated in gastrointestinal inflammation, gut barrier protection, and energy metabolism are associated with disease-specific gut microbes [109]. Conversely, mucosal gut microbes that have been implicated in multiple diseases (such as Streptococcus) are associated with different host pathways in each disease, suggesting that similar microbes can affect host pathophysiology in a disease-specific manner through regulation of different host genes [109].
Key shared pathways identified across multiple diseases include:
- RAC1 Pathway: Regulates immune response and intestinal mucosal repair; associated with different microbial taxa in CRC, IBD, and IBS [109]
- Oxidative Phosphorylation: Energy metabolism process dysregulated across multiple chronic conditions [109]
- Integrin Pathways: Regulate leukocyte recruitment in gastrointestinal inflammation [109]
Cross-disease comparisons of microbial signatures have revealed both expected and surprising relationships across diverse pathological conditions. The consistent identification of shared microbial signatures across traditionally distinct disease categories suggests the existence of common pathogenic mechanisms mediated through the microbiome, while disease-specific signatures offer opportunities for targeted diagnostic and therapeutic development.
Future research directions should focus on: (1) Prospective validation of identified signatures across diverse populations and geographic regions; (2) Mechanistic studies using HMA animal models to establish causal relationships; (3) Intervention trials targeting identified signatures for therapeutic benefit; and (4) Integration of multi-kingdom analyses including bacteriophages and fungi to obtain a comprehensive view of microbial ecosystems in health and disease.
The continued refinement of meta-analysis methods and machine learning approaches specifically designed for microbiome data will enhance our ability to identify robust, generalizable microbial signatures that can transform diagnostic paradigms and therapeutic strategies across a broad spectrum of human diseases.
Multi-omics integration represents a paradigm shift in biological research, enabling a holistic understanding of complex systems by combining data from various molecular layers. This guide objectively compares the performance of different integration strategies—specifically comparing early fusion versus model-based integration—for combining metagenomics, metatranscriptomics, and metabolomics data. Supported by experimental evidence from recent studies, we evaluate these methodologies within the critical context of correlating microbiome findings from animal models to human studies, providing drug development professionals with practical insights for selecting optimal analytical approaches.
Multi-omics approaches provide complementary insights into the complex interactions within biological systems, particularly in microbiome research. Each omics layer captures distinct aspects of system functionality: metagenomics reveals microbial community structure and genetic potential, metatranscriptomics captures gene expression and regulatory activity, and metabolomics provides snapshots of biochemical outputs and metabolic fluxes [111]. When integrated, these technologies facilitate a comprehensive understanding of the structural and functional properties of microbial communities, enabling researchers to move beyond correlation to establish mechanistic relationships in microbiome-host interactions [112].
The power of multi-omics integration lies in its ability to connect potential (genomics) to activity (transcriptomics) and finally to functional output (metabolomics). This integrated perspective is particularly valuable for translational research seeking to establish meaningful correlations between animal model findings and human clinical outcomes. For microbiome studies, this approach can elucidate how microbial community structure dictates functional capabilities, how these functions are regulated in response to host and environmental factors, and ultimately how microbial activities impact host physiology and disease states [111] [112].
Multi-Omics Integration Strategies: A Comparative Analysis
Integration Methodologies and Performance
Various computational strategies have been developed to integrate heterogeneous omics datasets, each with distinct advantages and limitations for specific research contexts. The performance of these approaches has been systematically evaluated in multiple studies, providing evidence-based guidance for method selection.
Table 1: Comparison of Multi-Omics Integration Strategies and Performance
| Integration Strategy | Key Characteristics | Prediction Accuracy* | Strengths | Limitations |
|---|---|---|---|---|
| Early Fusion (Concatenation) | Combines raw datasets prior to analysis | Variable; often underperforms for complex traits | Computational simplicity; intuitive implementation | Susceptible to technical variance; assumes uniform data structure |
| Model-Based Integration | Captures non-additive, nonlinear, and hierarchical interactions | Consistently superior for complex traits | Accommodates heterogeneous data types; captures biological complexity | Computationally intensive; requires sophisticated statistical expertise |
| Similarity-Based Fusion | Uses kernel methods to integrate omics-based similarity matrices | High for traits with strong biological pathways | Effective for capturing complex relationships between molecular layers | Limited interpretability of biological mechanisms |
| Graph-Based Integration | Networks represent relationships between omics features | Moderate to high, depending on network completeness | Enables visualization of system-wide interactions; intuitive mapping | Requires substantial prior knowledge for network construction |
*Prediction accuracy based on benchmark studies comparing genomic selection models for complex traits in plants; relative performance trends are expected to be similar in microbiome-host interaction studies [113].
Experimental evidence from genomic selection studies in plant breeding demonstrates that model-based integration approaches consistently outperform simple concatenation methods, particularly for complex traits influenced by multiple biological pathways [113]. In one comprehensive evaluation of 24 integration strategies combining genomics, transcriptomics, and metabolomics data, model-based fusion techniques showed significant improvements in predictive accuracy over genomic-only models, whereas early fusion approaches yielded inconsistent benefits and frequently underperformed [113].
Considerations for Microbiome-Human Correlation Studies
When applying multi-omics integration to correlate animal model findings with human outcomes, several methodological considerations emerge:
Dimensionality Management: Metagenomic, metatranscriptomic, and metabolomic datasets exhibit dramatically different dimensionalities, requiring sophisticated normalization and dimensionality reduction techniques to enable meaningful integration [111] [112].
Batch Effect Correction: Technical variability between omics platforms and sampling procedures can introduce confounding effects that obscure true biological signals, particularly when comparing across species or study sites [111].
Temporal Dynamics: Microbial community structure, gene expression, and metabolic output exhibit distinct temporal patterns that must be aligned for proper integration in longitudinal studies [112].
Scale Compatibility: Animal models often involve different sampling depths, sequencing coverage, and analytical resolution than human studies, requiring careful experimental design to enable valid cross-species comparisons [114].
Experimental Protocols for Multi-Omics Integration
Sample Collection and Processing Workflow
Proper sample handling is critical for generating high-quality multi-omics data that can be effectively integrated. The following protocol outlines a standardized workflow for simultaneous metagenomics, metatranscriptomics, and metabolomics data generation from a single sample.
Diagram 1: Multi-omics Sample Processing Workflow
Detailed Protocol:
- Sample Collection: Collect microbiome samples (stool, mucosal scrapings, or environmental samples) using standardized collection kits that stabilize RNA, DNA, and metabolites simultaneously. Immediate flash-freezing in liquid nitrogen is recommended for untargeted approaches [111].
Sample Homogenization and Division: Homogenize samples under conditions that maintain integrity of all molecular types (e.g., using bead-beating in appropriate buffers). Divide homogenate into aliquots for each omics analysis to ensure identical starting material [112].
Nucleic Acid Extraction:
- Metagenomic DNA: Extract using kits validated for microbial community representation (e.g., MoBio PowerSoil DNA Isolation Kit). Include controls for host DNA depletion when working with host-associated samples.
- Metatranscriptomic RNA: Extract using RNA-specific kits with DNase treatment. Include RNA stabilization agents during extraction to preserve labile transcripts. Quality check using Bioanalyzer or TapeStation [111].
Metabolite Extraction: Use methanol:water:chloroform extraction for comprehensive polar and non-polar metabolite coverage. Maintain samples at -20°C during processing to prevent degradation [115].
Library Preparation and Sequencing:
- Metagenomics: Prepare sequencing libraries using kits compatible with low-input DNA (e.g., Illumina Nextera XT). Sequence on Illumina platforms with minimum 10 million 150bp paired-end reads per sample.
- Metatranscriptomics: Deplete rRNA using probe-based methods (e.g., RiboZero). Prepare stranded RNA-seq libraries. Sequence with minimum 20 million 150bp paired-end reads.
- Metabolomics: Analyze extracts using LC-MS with reverse-phase and HILIC chromatography coupled to high-resolution mass spectrometers (e.g., Q-Exactive Orbitrap) in both positive and negative ionization modes [112] [115].
Data Integration and Analytical Workflow
Diagram 2: Multi-omics Data Integration Pipeline
Integration Methodology:
- Quality Control and Preprocessing:
- Metagenomic data: Use FastQC for quality assessment, Trimmomatic for adapter removal, and KneadData for host sequence decontamination.
- Metatranscriptomic data: Process with FastQC, Trimmomatic, and SortMeRNA for rRNA depletion verification.
- Metabolomic data: Use XCMS for peak picking, CAMERA for annotation, and metaX for normalization [112].
Feature Table Generation:
- Metagenomics: Generate taxonomic profiles using MetaPhlAn3 and functional profiles using HUMAnN2. Normalize to copies per million.
- Metatranscriptomics: Align reads to reference genomes or gene catalogs using Salmon or kallisto. Normalize using TPM.
- Metabolomics: Normalize peak areas using probabilistic quotient normalization and correct for batch effects [112].
Statistical Integration Approaches:
- Multi-Omics Factor Analysis (MOFA+): Identifies latent factors that capture shared variation across omics layers.
- Projection to Latent Structures (PLS): Models relationships between different omics blocks.
- Integrative Generalized SVMs: Handles heterogeneous data types for classification tasks.
- MixOmics: Provides multiple multivariate methods for integration and visualization [113] [112].
Case Study: Multi-Omics in Rheumatoid Arthritis Research
A recent study exemplifies the power of multi-omics integration for elucidating mechanisms and bridging animal-human translational gaps. Research on Qingre Huoxue Decoction (QRHXD) for rheumatoid arthritis (RA) employed integrated proteomic and metabolomic analyses of human serum, combined with validation in a collagen-induced arthritis (CIA) mouse model [115].
Table 2: Multi-Omics Findings in Rheumatoid Arthritis Study
| Analysis Type | Key Findings | Human-Animal Correlation | Therapeutic Mechanism |
|---|---|---|---|
| Proteomics | 83 differentially expressed proteins (46 upregulated, 37 downregulated) in RA patients | FBP1 expression consistently elevated in human RA serum and CIA mouse model | QRHXD inhibited FBP1 and activated AMPK signaling in both human and animal models |
| Metabolomics | 54 differential metabolites (11 upregulated, 43 downregulated) in RA patients | AMPK signaling pathway dysregulation confirmed in both systems | Pathway restoration correlated with clinical improvement in humans and histological improvement in mice |
| Integrated Analysis | FBP1/AMPK pathway identified as central regulatory mechanism | Strong correlation between molecular pathway modulation and functional improvement across species | Provides mechanistic explanation for QRHXD efficacy and validates translational relevance of animal model |
This case study demonstrates how multi-omics integration can identify key regulatory pathways (FBP1/AMPK) that are consistent between human patients and animal models, strengthening confidence in the translational relevance of findings and providing mechanistic insights for drug development [115].
Diagram 3: FBP1/AMPK Pathway in Rheumatoid Arthritis
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents for Multi-Omics Microbiome Studies
| Reagent/Category | Specific Examples | Function in Multi-Omics Workflow |
|---|---|---|
| Sample Stabilization | RNAlater, DNA/RNA Shield, Metabolite Stabilization Cocktails | Preserves molecular integrity during sample collection and storage for all omics types |
| Nucleic Acid Extraction | MoBio PowerSoil DNA/RNA Kits, Zymo BIOMICS DNA/RNA Kit | Simultaneous co-extraction of DNA and RNA maintains community representation |
| Library Preparation | Illumina Nextera XT, NEBNext Ultra II, SMARTer Stranded RNA-Seq | Prepares sequencing libraries with minimal bias and maintains strand specificity |
| Metabolomics Analysis | Methanol, Acetonitrile, Chloroform (1:1:2 ratio), Derivatization Reagents | Comprehensive metabolite extraction for LC-MS analysis |
| Bioinformatic Tools | HUMAnN2, MetaPhlAn3, XCMS, MOFA+, MixOmics | Processes raw data and enables statistical integration of multi-omics datasets |
| Reference Databases | Greengenes, SILVA, UNIREF, KEGG, HMDB | Provides taxonomic, functional, and metabolic annotations for data interpretation |
| Validation Reagents | FBP1 Antibodies, AMPK Phospho-Specific Antibodies, ELISA Kits | Verifies multi-omics findings through orthogonal methods in animal models |
Multi-omics integration represents a powerful approach for unraveling complex microbiome-host interactions and strengthening the correlation between animal model findings and human clinical outcomes. The comparative analysis presented herein demonstrates that model-based integration strategies generally outperform simpler concatenation approaches, particularly for elucidating complex biological mechanisms. The case study on rheumatoid arthritis illustrates how integrated proteomic and metabolomic analyses can identify conserved pathways across species, providing both mechanistic insights and validation of translational relevance.
As multi-omics technologies continue to evolve, researchers should prioritize experimental designs that enable true integration rather than parallel analysis, select integration methods appropriate for their specific biological questions, and implement rigorous validation frameworks to strengthen conclusions. When properly executed, multi-omics integration accelerates the translation of microbiome research from basic discovery to therapeutic application.
The human microbiome, particularly the gut microbiota, has emerged as a critical regulator of systemic immunity and inflammation, with profound implications for autoimmune and degenerative joint diseases. Within the context of a broader thesis on microbiome animal model human study findings correlation research, this comparative analysis examines the distinct microbial signatures associated with osteoarthritis (OA) and rheumatoid arthritis (RA). While both conditions involve joint inflammation and destruction, they diverge fundamentally in their pathophysiology: RA is a systemic autoimmune disorder characterized by immune-mediated synovitis, whereas OA is primarily a degenerative disease with inflammatory components [116] [117]. Emerging evidence suggests that the gut-joint axis—the bidirectional communication between gut microbiota and joints—plays a modulatory role in both conditions, though through distinct mechanisms [118] [119]. This case study synthesizes findings from human observational studies, animal models, and Mendelian randomization analyses to objectively compare how microbiome dysbiosis contributes to these prevalent forms of arthritis, with implications for targeted therapeutic development.
Comparative Microbial Signatures in OA and RA
Taxonomic Shifts in Arthritis-Associated Microbiota
Table 1: Comparative Microbiome Profiles in Osteoarthritis and Rheumatoid Arthritis
| Taxonomic Level | Osteoarthritis (OA) Associations | Rheumatoid Arthritis (RA) Associations | Key References |
|---|---|---|---|
| Phylum | ↑ Firmicutes, ↑ Proteobacteria | ↑ Bacteroidetes, ↓ Actinobacteria | [120] [121] [119] |
| Genus | ↑ Streptococcus, ↑ Clostridium, ↑ Bacteroides, ↓ Roseburia, ↓ Coprococcus | ↑ Prevotella, ↑ Collinsella, ↑ Lactobacillus, ↓ Haemophilus, ↓ Bifidobacterium | [116] [118] [121] |
| Species | ↑ Prevotella copri (early RA), ↑ Lactobacillus salivarius | ↑ Collinsella aerofaciens, ↓ Bifidobacterium longum | [116] [119] |
| Alpha Diversity | Generally reduced | Reduced in preclinical and early disease | [120] [117] [119] |
Analysis of microbiome composition reveals distinct taxonomic patterns that differentiate OA from RA. OA-associated dysbiosis is characterized by increased abundance of Streptococcus species, which correlate strongly with joint pain, and general enrichment of Firmicutes and Proteobacteria [120] [121]. The reduction of butyrate-producing bacteria like Roseburia and Coprococcus is particularly notable, as these taxa contribute to maintaining intestinal barrier integrity and possess anti-inflammatory properties [118]. In contrast, RA exhibits a marked expansion of Prevotella species, especially Prevotella copri in new-onset RA, alongside increased Collinsella and reduced Bifidobacterium [116] [119]. These taxonomic differences suggest potentially divergent mechanisms through which gut dysbiosis contributes to joint pathology in degenerative versus autoimmune arthritis.
Functional and Metabolomic Profiles
Beyond taxonomic composition, functional metabolic pathways derived from gut microbiota differ substantially between OA and RA. In OA, particular emphasis has been placed on tryptophan metabolism, with specific derivatives such as indole-3-aldehyde significantly correlated with erosive hand OA severity [118]. The reduction in short-chain fatty acid (SCFA) production, particularly butyrate, has been implicated in increased intestinal permeability and systemic inflammation [118]. For RA, microbial metabolism appears to influence citrullination pathways and Th17 cell differentiation [116] [119]. Porphyromonas gingivalis, an oral pathogen associated with RA, produces microbial peptidylarginine deiminase (PAD) that can citrullinate host proteins, triggering autoantibody production [119]. These functional differences highlight how microbiome-mediated mechanisms contribute to disease-specific pathological processes.
Mechanistic Pathways in Microbiome-Arthritis Interactions
The Gut-Joint Axis in Osteoarthritis
Diagram 1: Gut-Joint Axis Mechanisms in Osteoarthritis (Title: OA Gut-Joint Pathway)
The pathophysiology of OA in the context of the gut-joint axis involves a cascade of events initiated by microbial dysbiosis. Gut microbiota alterations, particularly increased Streptococcus species and reduced alpha diversity, contribute to impaired intestinal barrier function [118] [117]. This barrier disruption permits translocation of microbial products such as lipopolysaccharide (LPS) into circulation, triggering systemic inflammation characterized by elevated pro-inflammatory cytokines including TNF-α and IL-6 [118]. These inflammatory mediators promote joint tissue catabolism, pain sensitization, and ultimately cartilage degradation—hallmarks of OA progression. The correlation between gut Streptococcus abundance and OA pain underscores the clinical relevance of this pathway [120] [118].
The Gut-Joint Axis in Rheumatoid Arthritis
Diagram 2: Gut-Joint Axis Mechanisms in Rheumatoid Arthritis (Title: RA Gut-Joint Pathway)
RA pathogenesis involves more direct immune system dysregulation mediated by gut and oral microbiota. Gut dysbiosis, characterized by Prevotella expansion and reduced microbial diversity, promotes differentiation of pro-inflammatory Th17 cells while impairing regulatory T cell function, disrupting immune homeostasis [116] [119]. Through molecular mimicry, microbial antigens (e.g., from Prevotella and Collinsella) cross-react with self-peptides such as filamin A and N-acetylglucosamine-6-sulfatase, triggering autoantibody production [116]. Additionally, oral pathogens like Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans contribute to RA pathogenesis by promoting protein citrullination and anti-citrullinated protein antibody (ACPA) production [119]. These coordinated events lead to targeted immune attacks on synovial joints, characteristic of RA.
Experimental Models and Methodological Approaches
Human Study Designs and Protocols
Table 2: Methodological Approaches in Microbiome-Arthritis Research
| Method Type | Specific Techniques | Applications in Arthritis Research | Key Considerations |
|---|---|---|---|
| Sequencing Approaches | 16S rRNA sequencing, Shotgun metagenomics, Whole-genome sequencing | Microbial community profiling, Taxonomic classification, Functional potential assessment | 16S for cost-effective taxonomy; WGS for strain-level resolution & functional genes [120] [118] |
| Study Designs | Cross-sectional cohorts, Longitudinal studies, Randomized controlled trials, Mendelian randomization | Association studies, Temporal relationships, Intervention efficacy, Causal inference | MR studies support causal gut microbiota effects on arthritis [122] [117] |
| Multi-omics Integration | Metatranscriptomics, Metaproteomics, Metabolomics | Functional activity, Protein expression, Metabolic output | Provides mechanistic insights beyond taxonomy [118] [41] |
| Intervention Models | Probiotics, Prebiotics, Fecal microbiota transplantation, Dietary interventions | Therapeutic exploration, Mechanistic validation | Lactobacillus spp. show benefits in OA; FMT demonstrates transmissible phenotypes [116] [118] [117] |
Human studies investigating microbiome-arthritis relationships have employed diverse methodological approaches. Cross-sectional cohort studies have identified associations between microbial taxa and disease status, while longitudinal designs have tracked microbial changes through disease progression and treatment [118] [117]. More recently, Mendelian randomization (MR) studies have provided evidence supporting causal relationships between specific gut microbiota and arthritis development [122]. For example, one MR analysis identified 11 positive and 14 negative causal effects of gut microbiota on various arthritis types, with Bacillales abundance significantly increasing ankylosing spondylitis risk [122]. Methodological standardization remains challenging due to heterogeneity in sequencing approaches (16S rRNA vs. whole-genome sequencing), bioinformatic pipelines, and confounding factor adjustment across studies [118].
Animal Model Experimental Protocols
Animal models have been instrumental in establishing causal relationships and elucidating mechanisms in microbiome-arthritis research. The collagen-induced arthritis (CIA) model is widely used for RA research, while OA models include surgical destabilization, chemical induction, and genetically susceptible strains (e.g., STR/ort mice) [116] [117]. Common experimental protocols involve: (1) Gut microbiota modulation through antibiotics, probiotics, or fecal microbiota transplantation (FMT); (2) Germ-free studies to assess arthritis development in absence of microbiota; and (3) Gnotobiotic models colonized with specific bacterial consortia [116] [117]. For example, transplantation of gut microbiota from RA patients to germ-free SKG mice resulted in severe arthritis development, demonstrating the transmissible capacity of arthritis-prone microbiota [116]. Similarly, mono-colonization of IL1rn-/- mice with Lactobacillus bifidus induced rapid arthritis onset [116]. These controlled experimental approaches enable rigorous testing of microbial contributions to arthritis pathogenesis.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Experimental Solutions for Microbiome-Arthritis Research
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Sequencing & Omics | 16S rRNA primers (V3-V4), Shotgun metagenomics kits, Metabolomics platforms | Microbial profiling, Functional potential assessment, Metabolic profiling | 16S for taxonomy; Metagenomics for functional genes; Metabolomics for microbial products [120] [118] |
| Gnotobiotic Models | Germ-free mice, Defined microbial consortia, Fecal transplantation protocols | Causality testing, Mechanism elucidation, Therapeutic screening | Require specialized facilities; Allow controlled colonization studies [116] [117] |
| Immunological Assays | ELISA for cytokines/autoantibodies, Flow cytometry panels, Multiplex immunoassays | Immune profiling, Inflammatory mediator quantification, Cell population analysis | Essential for connecting microbiome changes to immune responses [116] [122] |
| Barrier Function Assessment | FITC-dextran permeability assay, Tight junction protein antibodies, Electron microscopy | Intestinal barrier integrity evaluation, Epithelial structure analysis | Connects gut dysbiosis to systemic inflammation [116] [118] |
This toolkit highlights essential reagents and methodologies driving advances in microbiome-arthritis research. 16S rRNA sequencing with primers targeting the V3-V4 hypervariable regions remains the most common approach for microbial community profiling, though shotgun metagenomics is increasingly used for enhanced taxonomic resolution and functional inference [120] [118]. Gnotobiotic animal models represent a cornerstone for establishing causal relationships, allowing researchers to colonize germ-free animals with defined microbial communities and assess arthritis outcomes [116] [117]. For immunological profiling, multiplex cytokine assays and flow cytometry with panels distinguishing T cell subsets (e.g., Th17, Treg) are critical for connecting microbial changes to immune responses [116] [122]. Additionally, barrier function assessments using FITC-dextran permeability measurements and tight junction protein visualization help mechanistically link gut dysbiosis to systemic inflammation in both OA and RA [116] [118].
This comparative analysis reveals distinct microbiome signatures and mechanisms associated with osteoarthritis and rheumatoid arthritis within the framework of microbiome animal model human study findings correlation research. OA is characterized by streptococcus-enriched dysbiosis with implications for systemic inflammation and pain signaling, while RA demonstrates Prevotella-driven microbial shifts that promote autoimmunity via molecular mimicry and Th17 activation. Despite methodological advances, challenges remain in standardizing approaches across studies and translating correlative findings into targeted therapies. Future research directions should include longitudinal multi-omics studies to track dynamic microbiome-host interactions, mechanistically-defined probiotic cocktails tailored to specific arthritis subtypes, and intervention trials targeting the gut-joint axis. The evolving understanding of microbiome-arthritis relationships promises to unveil novel diagnostic biomarkers and therapeutic strategies for these debilitating conditions.
Conclusion
The translation of findings from animal models to human applications remains the central challenge in microbiome research. A consensus is emerging that success requires a multi-faceted approach: embracing interdisciplinary collaboration, implementing standardized and rigorous experimental methodologies, and leveraging advanced computational tools for validation. While preclinical models are indispensable for generating causal hypotheses and screening therapeutics, their limitations must be explicitly acknowledged. Future efforts must focus on improving the human relevance of these models, perhaps through the use of humanized immune systems or more physiologically complex in vitro systems. The robust pipeline of over 180 microbiome-targeted therapies underscores the field's immense potential. However, realizing this potential hinges on the scientific community's commitment to self-correction, methodological rigor, and a critical, nuanced interpretation of model-derived data to bridge the translational gap and deliver on the promise of microbiome-based medicine.
References
- 1. Dysbiosis: What It Is, Symptoms, Causes, Treatment & Diet [https://my.clevelandclinic.org/health/diseases/dysbiosis]
- 2. Dysbiosis - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/dysbiosis]
- 3. Establishing What Constitutes a Healthy Human Gut Microbiome [https://pmc.ncbi.nlm.nih.gov/articles/PMC6825832/]
- 4. Human microbiota-associated animal models: a review [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1644187/full]
- 5. The microbiome is associated with obesity-related ... [https://www.nature.com/articles/s41522-025-00811-w]
- 6. Gut Microbiota Dysbiosis: Pathogenesis, Diseases, Prevention ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12006732/]
- 7. Gut microbiome-metabolome interactions predict host condition [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-023-01737-1]
- 8. Review Best Practices and Considerations for Conducting ... [https://www.sciencedirect.com/science/article/pii/S2161831325000559]
- 9. Reporting guidelines for Human Microbiome Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC9105086/]
- 10. Correlation vs. Causation | Difference, Designs & Examples [https://www.scribbr.com/methodology/correlation-vs-causation/]
- 11. Correlation vs Causation: Learn the Difference [https://amplitude.com/blog/causation-correlation]
- 12. From Correlation to Causation: Deep Dive into Data ... [https://www.statology.org/from-correlation-to-causation-deep-dive-into-data-interpretation/]
- 13. Chains of evidence from correlations to causal molecules ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8480537/]
- 14. A Consensus Statement on establishing causality ... [https://www.nature.com/articles/s41575-025-01041-3]
- 15. Correlation 'dressed up' as causation: The reality of ... [https://www.nutraingredients.com/Article/2025/07/31/correlation-dressed-up-as-causation-the-reality-of-microbiome-science/]
- 16. Beyond just correlation: causal machine learning for the ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1691503/full]
- 17. Approaches to discern if microbiome associations reflect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9361767/]
- 18. 📊 Correlation vs. Causation: A Data Scientist's Guide [https://medium.com/@kirti07arora/correlation-vs-causation-a-data-scientists-guide-a3c1fdd82abd]
- 19. Microbiota-Based Therapies for Recurrent Clostridium difficile ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12450354/]
- 20. Effectiveness and Safety of Fecal Microbiota ... [https://www.sciencedirect.com/science/article/abs/pii/S1542356525006469]
- 21. What's New and What's Next in Fecal Microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377394/]
- 22. Fecal microbiota transplantation: Current evidence and ... [https://www.ccjm.org/content/92/7/421]
- 23. The efficacy and safety of fecal microbiota transplantation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12160374/]
- 24. Efficacy of encapsulated fecal microbiota transplantation ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1648944/full]
- 25. Fecal microbiota transplantation influences ... [https://www.nature.com/articles/s41522-024-00549-x]
- 26. Gut Microbial Targets in Inflammatory Bowel Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC11940752/]
- 27. Microbiome Markers in Gastrointestinal Disorders [https://www.mdpi.com/1422-0067/26/10/4818]
- 28. Metabolic modeling reveals a multi-level deregulation of ... [https://www.nature.com/articles/s41467-025-60233-2]
- 29. Emerging concepts and shifting paradigms for ... [https://www.jci.org/articles/view/193969]
- 30. Microbiome-based therapeutics for metabolic disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613280/]
- 31. Innovative new tool helps understand how gut microbes ... [https://www.news-medical.net/news/20251120/Innovative-new-tool-helps-understand-how-gut-microbes-interact-to-influence-health.aspx]
- 32. Deciphering microbial and metabolic influences in ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06552-w]
- 33. Human Microbiome Market Industry Research 2025-2035 [https://finance.yahoo.com/news/human-microbiome-market-industry-research-081200143.html]
- 34. The Future of Microbiome Therapeutics - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11802617/]
- 35. Human Microbiome Market & Therapeutic Pipeline 2025 [https://www.strategicmarketresearch.com/blogs/human-microbiome-market-clinical-trials-pipeline]
- 36. Microbiome Disease Pipeline Insight 2025: Over 180 ... [https://www.globenewswire.com/news-release/2025/03/21/3047220/28124/en/Microbiome-Disease-Pipeline-Insight-2025-Over-180-Drugs-in-Development-Across-140-Companies.html]
- 37. 11 microbiome biotech companies to watch in 2025 [https://www.labiotech.eu/best-biotech/microbiome-biotech-companies/]
- 38. Present and future of microbiome-targeting therapeutics [https://www.jci.org/articles/view/184323]
- 39. The role of the gut microbiota on animal model reproducibility [https://pmc.ncbi.nlm.nih.gov/articles/PMC6388061/]
- 40. Of men in mice: the development and application ... [https://www.nature.com/articles/s12276-020-0473-2]
- 41. From big data and experimental models to clinical trials [https://www.sciencedirect.com/science/article/pii/S0092867425001072]
- 42. What we need to know about the germ-free animal models [https://pmc.ncbi.nlm.nih.gov/articles/PMC10955174/]
- 43. Germ-free animal experiments in the gut microbiota studies [https://www.sciencedirect.com/science/article/abs/pii/S1471489219300219]
- 44. Biological adaptation to a germ-free environment should not ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12120197/]
- 45. Fecal microbiota transplantation from patients into animals to ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06645-6]
- 46. Assessment of ecological fidelity of human microbiome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607873/]
- 47. Small animals, big conclusions- pros and cons of HMA ... [https://micro-bites.org/2021/03/01/small-animals-big-conclusions-pros-and-cons-of-human-microbiota-associated-hma-models/]
- 48. Impact of early-life human microbiota on the murine host ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-04321-9]
- 49. Metabolic modelling reveals the aging-associated decline ... [https://www.nature.com/articles/s41564-025-01959-z]
- 50. 196 Direct comparison of human microbiota-associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6666505/]
- 51. Overcoming Challenges with Animal Models in Research [https://cgt.global/overcoming-challenges-with-animal-models-in-research/]
- 52. Zebrafish: an efficient vertebrate model for understanding role ... [https://molmed.biomedcentral.com/articles/10.1186/s10020-022-00579-1]
- 53. Drosophila as a model for the gut microbiome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7179820/]
- 54. Interactions between human microbiome, diet, enteric ... [https://www.sciencedirect.com/science/article/pii/S1740675718300185]
- 55. The Microbiota and Gut-Related Disorders: Insights from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7693214/]
- 56. A Gnotobiotic Pig Model for Determining Human Norovirus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4561694/]
- 57. A symbiotic physical niche in Drosophila melanogaster ... [https://www.nature.com/articles/s41467-023-36942-x]
- 58. Human microbiota-associated animal models: a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12420304/]
- 59. 2017 Microbiome in Mouse Models Workshop Review [https://www.taconic.com/resources/2017-microbiome-workshop-review-part-three]
- 60. Advancements in Microphysiological systems: Exploring ... [https://www.sciencedirect.com/science/article/pii/S1347436724000521]
- 61. State-of-the-art in high throughput organ-on-chip for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12149869/]
- 62. The Use of Gut Organoids: To Study the Physiology and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11836903/]
- 63. Developments in gastrointestinal organoid cultures to ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1521044/full]
- 64. A gut-on-a-chip incorporating human faecal samples and ... [https://www.nature.com/articles/s41551-024-01318-z]
- 65. Science in 3D: How organoids and organs-on-chips can ... [https://www.jax.org/news-and-insights/2025/september/science-in-3d-how-organoids-and-organs-on-chips-can-help-scientists-study-host-immune-microbiome-interactions]
- 66. Next level in vitro research model of the human intestine [https://www.sciencedirect.com/science/article/pii/S246820202030070X]
- 67. Expanding the Frontiers of Human Biology with Organ-on-a ... [https://emulatebio.com/expanding-the-frontiers-of-human-biology-with-organ-on-a-chip-technology-highlights-from-the-2025-mps-world-summit/]
- 68. MaaT Pharma Announces Positive Topline Results from ... [https://www.maatpharma.com/january-8-2025-maat-pharma-announces-positive-topline-results-from-the-pivotal-phase-3-ares-study-evaluating-maat013-in-acute-graft-versus-host-disease/]
- 69. Disease Clinical Trial Analysis: Key Insights into Rich... Microbiome [https://finance.yahoo.com/news/microbiome-disease-clinical-trial-analysis-180000100.html]
- 70. ARES Trial of MaaT013 in GI-aGVHD Meets Primary End ... [https://www.onclive.com/view/ares-trial-of-maat013-in-gi-agvhd-meets-primary-end-point-of-gi-orr]
- 71. Seres Therapeutics Reports SER-155 Phase 1b Cohort 1 ... [https://ir.serestherapeutics.com/news-releases/news-release-details/seres-therapeutics-reports-ser-155-phase-1b-cohort-1-results]
- 72. Microbiome Disease Clinical Pipeline | 140+ Companies [https://www.openpr.com/news/3933678/microbiome-disease-clinical-pipeline-140-companies]
- 73. Pooled allogeneic faecal microbiota MaaT013 for steroid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10466244/]
- 74. for Animal Research: Advancing Basic and... Models Microbiome [https://pubmed.ncbi.nlm.nih.gov/29782137/]
- 75. Close social relationships correlate with human gut ... [https://www.nature.com/articles/s41598-018-37298-9]
- 76. Choosing the Perfect Way to Visualize Your Microbiome Data [https://bitesizebio.com/78637/visualize-microbiome-data/]
- 77. A guide to human microbiome research: study design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7469990/]
- 78. Microbiota composition-based donor selection affects FMT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12353733/]
- 79. Variability of strain engraftment and predictability ... [https://www.nature.com/articles/s41591-022-01964-3]
- 80. Overcoming donor variability and risks associated with fecal ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-024-01820-1]
- 81. Experimental methods modestly impact interpretation of the ... [https://www.nature.com/articles/s41598-022-18532-x]
- 82. microbiota-associated Human : a review animal models [https://pubmed.ncbi.nlm.nih.gov/40937436/]
- 83. Improved detection of microbiome -disease associations via population... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1012277]
- 84. Beyond animal testing: How human data trials are ... [https://pharmaphorum.com/rd/beyond-animal-testing-how-human-data-trials-are-reshaping-drug-development]
- 85. The human microbiome in clinical translation: from bench to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479421/]
- 86. A reconceptualized framework for human microbiome ... [https://www.nature.com/articles/s41467-025-61998-2]
- 87. Beyond Animals: Revolutionizing Drug Discovery with Human ... [https://wyss.harvard.edu/news/beyond-animals-revolutionizing-drug-discovery-with-human-relevant-models/]
- 88. NIH Upgrades Nephele, Revolutionizes Microbiome Data ... [https://nihrecord.nih.gov/2025/08/15/nih-upgrades-nephele-revolutionizes-microbiome-data-analysis]
- 89. Meta-analysis reveals reproducible gut microbiome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6708278/]
- 90. Reporting guidelines for human microbiome research [https://www.nature.com/articles/s41591-021-01552-x]
- 91. Impact of Non-Standardized Reporting on Reproducibility ... [https://www.medrxiv.org/content/10.1101/2025.09.06.25335230v2]
- 92. Breaking the reproducibility barrier with standardized ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003358]
- 93. Breaking the reproducibility barrier with standardized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12416739/]
- 94. Key features and guidelines for the application of microbial ... [https://www.nature.com/articles/s41598-024-77864-y]
- 95. Microbiome meta-analysis and cross-disease comparison ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-021-02306-1]
- 96. Machine learning-based meta-analysis reveals gut ... [https://www.nature.com/articles/s41467-025-56829-3]
- 97. A realistic benchmark for differential abundance testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11423519/]
- 98. Integrative metagenomic analysis reveals distinct gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10996249/]
- 99. Microbiome statistics plotting gallery for meta‐omics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11865346/]
- 100. Machine learning determines the incidence of Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11999016/]
- 101. An enhancement of machine learning model performance ... [https://www.nature.com/articles/s41598-025-15019-3]
- 102. Gut bioengineered models to study host-microbiota- ... [https://www.oaepublish.com/articles/mrr.2025.45]
- 103. Systematic review of gut microbiota composition, metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12116390/]
- 104. On-the-Fly Data Augmentation for Brain Tumor Segmentation [https://arxiv.org/html/2509.24973v1]
- 105. Cross-cohort analysis identifies shared gut microbial ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06676-z]
- 106. Microbiome meta-analysis and cross-disease comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8008609/]
- 107. Melody: meta-analysis of microbiome association studies for ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03721-4]
- 108. Meta-analysis of the human gut microbiome uncovers shared ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11334437/]
- 109. Identification of shared and disease-specific host gene ... [https://www.nature.com/articles/s41564-022-01121-z]
- 110. Multi-biome analysis identifies distinct gut microbial ... [https://www.nature.com/articles/s41467-024-54797-8]
- 111. ' Multi data omic : A review of concepts, considerations... integration [https://pubmed.ncbi.nlm.nih.gov/34256961/]
- 112. - Integrated analyses of microbial communities: a review of... multi omics [https://pubs.rsc.org/en/content/articlelanding/2023/mo/d3mo00089c]
- 113. Genomic prediction powered by multi-omics data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485622/]
- 114. Current status and challenges of multi-omics research ... [https://www.sciencedirect.com/science/article/pii/S2772976125001953]
- 115. Multiomics analysis of human serum and animal ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1526110/full]
- 116. Gut microbiota and rheumatoid arthritis [https://pmc.ncbi.nlm.nih.gov/articles/PMC9499173/]
- 117. “Cross-talk” between gut microbiome dysbiosis and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1150572/full]
- 118. Gut microbiota and osteoarthritis: epidemiology, mechanistic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12307352/]
- 119. focus on gut, oral microbiome and their extracellular vesicles [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1503474/full]
- 120. The microbiome in osteoarthritis: a narrative review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11627155/]
- 121. A systematic review of microbiome composition in ... [https://www.sciencedirect.com/science/article/pii/S1063458421010074]
- 122. Investigating the causal impact of gut microbiota on arthritis ... [https://www.nature.com/articles/s41598-024-79336-9]