From Bench to Bedside: The Clinical Translation of the Human Microbiome in Diagnostics and Therapeutics
This article synthesizes the rapid evolution of microbiome science from a research field to a cornerstone of clinical innovation.
From Bench to Bedside: The Clinical Translation of the Human Microbiome in Diagnostics and Therapeutics
Abstract
This article synthesizes the rapid evolution of microbiome science from a research field to a cornerstone of clinical innovation. Aimed at researchers, scientists, and drug development professionals, it explores the foundational mechanisms by which the microbiome influences health and disease, the burgeoning pipeline of microbiome-based diagnostics and live biotherapeutic products (LBPs), and the critical methodological and regulatory challenges that remain. By examining current applications—from FDA-approved therapies for recurrent C. difficile infection to microbiome-based stratification for cancer immunotherapy—and outlining a roadmap for standardization and validation, this review provides a comprehensive overview of the opportunities and hurdles in integrating microbiome science into precision medicine.
The Microbiome Paradigm: From Passive Bystander to Active Therapeutic Target
The human microbiome has undergone a profound conceptual shift, from being considered a passive bystander to being recognized as a dynamic and essential determinant of human physiology [1]. This complex ecosystem of microorganisms actively shapes immunity, metabolism, neurodevelopment, and therapeutic responsiveness across the lifespan through intricate crosstalk with host pathways [1]. Advances in multi-omic technologies and computational approaches have revealed mechanistic insights into how microbial communities modulate host systems across diverse body sites, accelerating the clinical translation of this knowledge for diagnostic and therapeutic applications [1] [2] [3]. This document outlines the core principles, key applications, and detailed methodological protocols for investigating the microbiome's role in human physiology and disease, providing researchers with practical tools for advancing microbiome science toward clinical implementation.
Diagnostic Potential of Microbiome-Associated Metabolites
The microbiome exerts profound influence on host physiology through the production and modulation of metabolites that enter systemic circulation. These microbiome-associated metabolites serve as quantifiable biomarkers for disease risk and progression, offering significant diagnostic potential [2].
Table 1: Key Microbiome-Associated Metabolite Classes and Their Diagnostic Relevance
| Metabolite Class | Representative Metabolites | Physiological Association | Diagnostic Potential |
|---|---|---|---|
| Amino Acid Derivatives | Phenylacetylglutamine, p-cresol-glucuronide, indole-acetate [2] | Compromised glucose homeostasis, Type 2 Diabetes [2] | Predictive biomarkers for metabolic disease progression and treatment response |
| Xenobiotics | Benzoate derivatives, compounds in xanthine/caffeine metabolism [2] | Reflection of dietary habits and microbial adaptation [2] | Indicators of dietary exposure and personalized metabolic profiles |
| Lipid Metabolites | Short-chain fatty acids (SCFAs) and other lipid species [1] [2] | Immune regulation, gut barrier integrity, energy metabolism [1] | Biomarkers for inflammatory states and cardiometabolic health |
| Microbial Biosynthetic Products | Molecules from unexplored Biosynthetic Gene Clusters (BGCs) [3] | Disease-specific associations across body sites [3] | Novel diagnostic signatures and therapeutic targets |
Experimental Protocol: Metabolome-Wide Association Study (MWAS)
Objective: To identify and validate plasma metabolites associated with the gut microbiome and a specific disease phenotype (e.g., impaired glucose control) [2].
Materials:
- Research Reagent Solutions: EDTA plasma collection tubes; LC-MS/MS system with electrospray ionization; Human Metabolome Database (HMDB) for annotation; GBDT/random forest machine learning environments (e.g., R, Python with scikit-learn); Germ-free (GF) and conventionally raised (CONV-R) mouse models [2].
Procedure:
- Cohort Establishment & Sampling: Recruit a well-phenotyped patient cohort, ensuring representation across disease states (e.g., normal glucose tolerance, prediabetes, treatment-naive T2D) and BMI-matching where appropriate to control for confounding [2]. Collect plasma samples using standardized protocols and store at -80°C.
- Metabolomic Profiling: Perform untargeted metabolomic profiling on plasma samples using Liquid Chromatography-Mass Spectrometry (LC-MS). Annotate metabolites against reference databases (e.g., HMDB). The resulting data matrix should contain samples as rows and metabolite relative abundances as columns [2].
- Predictive Modeling of Metabolite Variance: Use a Gradient-Boosted Decision Trees (GBDT) algorithm to model the relationship between feature groups (clinical data, microbial metagenomic species, dietary variables) and each circulating metabolite. Quantify the variance explained (R²) by each feature group to identify microbiome-associated metabolites (e.g., those where microbiome data explains a significant portion of variance) [2].
- Cross-Platform and Cross-Population Validation:
- Technical Validation: Process raw metagenomic data through multiple bioinformatic pipelines (e.g., reference-free canopy clustering, Kraken 2, MetaPhlAn 4) and confirm that microbiome-metabolite associations are consistent across pipelines (Pearson correlation >0.95) [2].
- Population Validation: Replicate significant microbiome-metabolite associations in an independent cohort from a different geographical population (e.g., Swedish findings in an Israeli cohort) [2].
- In Vivo Validation: Measure the identified microbiome-associated metabolites in plasma from GF and CONV-R mice. Confirm that a significant proportion (e.g., >50%) of these metabolites are depleted or altered in GF mice, providing causal evidence of their microbial origin [2].
Therapeutic Strategies for Microbiome Modulation
Therapeutic manipulation of the microbiome presents a promising avenue for treating a wide range of conditions. Current strategies range from entire community transplantation to precisely targeted interventions.
Table 2: Therapeutic Modalities for Microbiome Modulation
| Therapeutic Modality | Description | Key Examples | Clinical Stage/Considerations |
|---|---|---|---|
| Fecal Microbiota Transplantation (FMT) | Transfer of minimally processed donor stool to restore a healthy microbial community [4]. | Treatment for recurrent Clostridioides difficile infection [4]. | Regulatory oversight is evolving; variable efficacy; risk of pathogen transfer [4]. |
| Live Biotherapeutic Products (LBPs) | Defined bacterial strains administered as drugs [1] [4]. | Akkermansia muciniphila (metabolic health), Faecalibacterium prausnitzii (Crohn's disease) [4]. | Require Investigational New Drug (IND) application; complex manufacturing (CMC) [4]. |
| Phage Therapy | Use of bacteriophage cocktails to selectively target and suppress disease-contributing pathobionts [1] [4]. | Cocktails targeting Klebsiella pneumoniae strains in IBD [1] [4]. | First-in-human trials show viability and safety; requires careful cocktail design to prevent resistance [4]. |
| Precision Nutrition | Dietary interventions tailored to an individual's microbiome to modulate its composition and function [1] [2]. | Interventions based on personalized microbiome-metabolite profiles to improve glucose control [2]. | High personalization potential; integrates with other omics data for "biological BMI" [4]. |
| Defined Microbial Consortia | Synthetically assembled communities of known bacterial strains [4]. | Complex defined consortia (>100 strains) for reliable engraftment and diverse metabolic functions [4]. | Designed to overcome FMT variability; highly engineerable but face engraftment challenges [4]. |
Experimental Protocol: Phage Cocktail Preparation and Administration for Targeted Pathobiont Suppression
Objective: To develop and test an orally administered bacteriophage cocktail for the targeted suppression of a specific disease-contributing pathobiont (e.g., Klebsiella pneumoniae in Inflammatory Bowel Disease) [4].
Materials:
- Research Reagent Solutions: Bacterial isolates of the target pathobiont from patient cohorts; environmental phage libraries or clinical samples for phage isolation; cell culture materials for phage propagation (host bacteria, growth media, filters); germ-free or gnotobiotic mouse models; capsule-based oral delivery system for phages [4].
Procedure:
- Target Identification & Phage Isolation: Identify a specific pathobiont clade consistently expanded in patient cohorts (e.g., K. pneumoniae clade 2 in IBD) [4]. Isolate bacteriophages that infect this target by enriching environmental or clinical samples with the bacterial strain. Isolate individual plaques and purify through successive streaking.
- Phage Cocktail Design: Select at least 3-4 phages that attack the same bacterial strain but utilize different host receptors for entry. This multi-receptor strategy is critical to minimize the development of phage resistance in the target bacterium [4].
- In Vitro Efficacy and Specificity Testing: Test the phage cocktail's efficacy in killing the target pathobiont in vitro. Co-culture the phage cocktail with human fecal samples ex vivo to confirm target suppression and assess off-target effects on the rest of the microbial community, aiming for minimal dysbiosis [4].
- Preclinical Animal Testing: Administer the phage cocktail orally to germ-free mice that have been humanized with the target pathobiont or to gnotobiotic models. Monitor phage viability through the GI tract, target bacterial load reduction, and markers of inflammation and tissue damage to establish proof-of-concept [4].
- Clinical Trial Formulation and Testing: For human trials, formulate phages in a capsule resistant to gastric acid to ensure delivery to the lower gut. A first-in-human Phase I clinical trial should first establish the safety and viability of the phages in the human gastrointestinal tract before proceeding to efficacy studies for the disease indication [4].
Essential Methodologies and Reporting Standards
Robust and reproducible microbiome science requires standardized methodologies from the bench to computational analysis.
The Scientist's Toolkit: Key Research Reagents and Platforms
Table 3: Essential Tools for Microbiome Research and Analysis
| Tool Category | Specific Tool / Solution | Function and Application |
|---|---|---|
| Sequencing & Profiling | Shotgun Metagenomic Sequencing [3] [5] | Provides a comprehensive view of all genetic material, allowing for taxonomic and functional profiling. |
| LC-MS/MS Metabolomics Platform [2] | Identifies and quantifies small molecule metabolites in biofluids, linking microbial function to host phenotype. | |
| Bioinformatic Analysis | iNAP (Integrated Network Analysis Pipeline) [6] | Online pipeline for constructing and analyzing intra- and inter-domain microbial ecological networks from abundance data. |
| SparCC, SPIEC-EASI, eLSA [6] | Statistical methods within iNAP and other tools to infer robust microbial associations from compositional data. | |
| Reporting Framework | STORMS Checklist [7] | A 17-item checklist for organizing and reporting microbiome studies to ensure completeness and reproducibility. |
| Reference Materials | Human Fecal Reference Material [4] | Standardized reference material (e.g., from NIST) to control for technical bias in sample processing and sequencing. |
| Experimental Models | Germ-Free (GF) Mouse Models [2] | In vivo models to conclusively demonstrate the microbial origin of specific metabolites or physiological effects. |
Experimental Protocol: Standardized Metagenomic Sequencing and Reporting
Objective: To generate high-quality, reproducible metagenomic data from human specimens and report it in accordance with community standards [7] [3].
Materials: Specimen collection kits (e.g., stool, saliva, skin swabs); DNA extraction kits optimized for microbial lysis; library preparation kits; high-throughput sequencer (e.g., Illumina); STORMS checklist [7].
Procedure:
- Standardized Sample Collection and Biobanking: Collect specimens from multiple body sites (e.g., stool, saliva, plaque, skin, throat) using a standardized protocol across all recruiting sites [3]. Immediately freeze samples at -80°C, as this preservation method is considered most appropriate for maintaining microbiome integrity [4].
- DNA Extraction and Sequencing: Extract DNA using a method that efficiently lyses both Gram-positive and Gram-negative bacteria. Perform shotgun metagenomic library preparation and sequence to a sufficient depth (e.g., an average of 5.3 gigabases per sample) to achieve comprehensive coverage [3].
- Quality Control and Human DNA Depletion: Apply stringent quality control to raw sequencing data. Remove reads that align to the human genome to reduce host contamination and protect patient privacy. Retain only high-quality metagenomes for downstream analysis [3].
- Taxonomic and Functional Profiling: Process non-human sequencing reads through a standardized bioinformatic pipeline for taxonomic binning (e.g., to Species-level Genome Bins - SGBs) and functional annotation (e.g., of Kyoto Encyclopedia of Genes and Genomes orthologies and Biosynthetic Gene Clusters) [2] [3].
- Compliant Study Reporting: During manuscript preparation, use the STORMS checklist to ensure all critical elements are reported [7]. This includes detailed descriptions of participants (including geography and diet), specimen collection dates, DNA extraction and sequencing methods, bioinformatic tools and parameters, and statistical approaches used for association testing.
Integrated Workflow and Analytical Pipelines
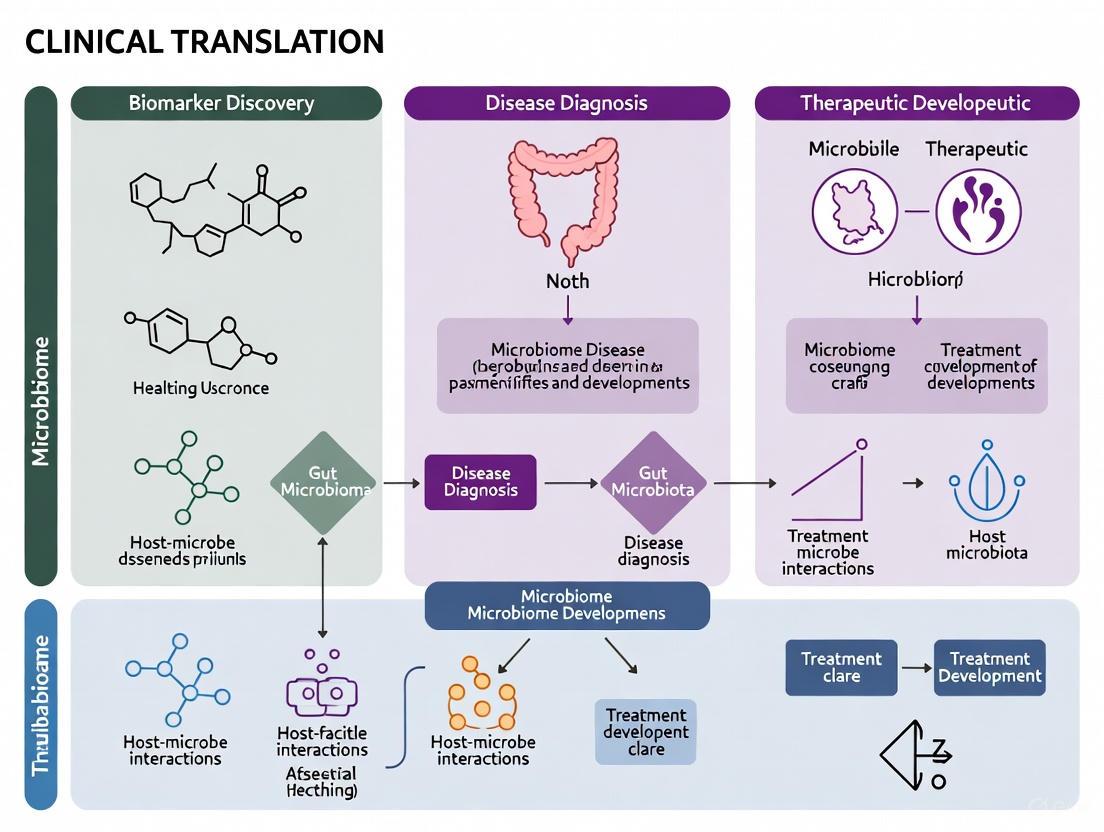
The following diagram illustrates the integrated multi-omics workflow for discovering and validating microbiome-based diagnostic and therapeutic targets, from initial sampling to clinical application.
Integrated Workflow for Microbiome Research and Translation
This integrated workflow underscores the necessity of combining standardized multi-omic data generation with advanced computational modeling and rigorous validation to successfully translate microbiome research into clinical applications [1] [2] [3]. The pathway highlights key stages from initial sampling through to the discovery of diagnostic biomarkers and therapeutic targets, culminating in clinical trials governed by regulatory standards [4].
The human microbiome, a complex ecosystem of microorganisms, is now recognized as a dynamic and essential determinant of human physiology, shaping immunity, metabolism, neurodevelopment, and therapeutic responsiveness across the lifespan [1]. The clinical translation of microbiome science represents a paradigm shift in precision medicine, transforming concepts of disease etiology and therapeutic design [1]. This Application Note delineates the key mechanistic pathways—immune signaling, metabolic interactions, and host-microbe crosstalk—underpinning microbiome-host symbiosis and its translational applications. We provide detailed experimental frameworks and analytical protocols to facilitate research in microbiome diagnostics and therapeutic development.
Key Mechanistic Pathways in Microbiome-Host Interactions
Immune Signaling Pathways
The immune system and microbiome engage in continuous, bidirectional communication critical for maintaining homeostasis and mounting appropriate responses to challenges [8]. Microbial communities play a fundamental role in training and developing both innate and adaptive immunity, while the immune system orchestrates the maintenance of host-microbe symbiosis [8].
Table 1: Key Microbial Modulators of Host Immune Signaling
| Microbial Component | Immune Receptor | Downstream Signaling | Biological Outcome |
|---|---|---|---|
| Polysaccharide A (PSA) from Bacteroides fragilis | TLR2/TLR1 with Dectin-1 | PI3K pathway → GSK3β inactivation → CREB activation [8] | Anti-inflammatory gene expression; systemic T cell maturation [8] |
| Segmented Filamentous Bacteria (SFB) antigens | Not specified (epithelial adhesion) | STAT3 signaling → RORγt activation [8] | Th17 cell differentiation in small intestine lamina propria [8] |
| Microbial metabolites (SCFAs) | GPR43, GPR109A | Inhibition of HDACs; NF-κB modulation [9] [8] | Treg differentiation; anti-inflammatory effects; barrier integrity [9] [8] |
| Flagellin | TLR5 | MyD88/NF-κB signaling [8] | Innate immune activation; microbiota composition shaping [8] |
Diagram Title: Microbiome-Mediated Immune Signaling Pathway
Metabolic Interactions and Cross-Feeding
Metabolism forms the central pillar of host-microbe relationships, with microbial metabolites serving as crucial signaling molecules and energy sources [9]. The intestinal epithelium and gut microbiota maintain a cyclical relationship of mutual metabolic benefit—host epithelial metabolism provides a hypoxic niche for obligate anaerobes, while microbial metabolites like butyrate serve as the primary energy source for colonocytes [9].
Table 2: Key Microbial Metabolites and Host Functions
| Metabolite | Producing Microbes | Host Receptor/Target | Biological Function |
|---|---|---|---|
| Butyrate | Faecalibacterium prausnitzii, Roseburia spp. | HDACs; PPARγ [9] | Primary colonocyte energy source; maintenance of hypoxic lumen; anti-inflammatory [9] |
| Acetate | Bifidobacterium spp., Bacteroides spp. | GPR43 [9] | Substrate for butyrogenesis; cholesterol metabolism; anti-inflammatory [9] |
| Propionate | Bacteroides spp., Akkermansia spp. | GPR41, GPR43 [9] | Gluconeogenesis; satiety signaling; immune regulation [9] |
| Lactate | Lactic acid bacteria (LAB) | GPR81 [9] | Intestinal stem cell differentiation via Wnt signaling; epithelial repair [9] |
| Indolepropionic acid (IPA) | Clostridium sporogenes | Aryl hydrocarbon receptor (AhR) [9] | Enhancement of epithelial barrier function [9] |
Diagram Title: Host-Microbe Metabolic Cross-Feeding Cycle
Host-Microbe Crosstalk in Disease and Therapeutics
Imbalances in microbiota-immunity interactions contribute to pathogenesis across a spectrum of disorders, including inflammatory bowel disease, metabolic syndrome, cancer, and neurodegenerative diseases [8] [10] [11]. The microbiota-gut-brain axis represents a particularly important regulatory system where microbial metabolites and neuroactive compounds influence glial function and neuroinflammation [11].
Table 3: Microbiome-Based Therapeutic Strategies and Mechanisms
| Therapeutic Approach | Mechanism of Action | Target Conditions |
|---|---|---|
| Fecal Microbiota Transplantation (FMT) | Restoration of diverse microbial community; niche competition [12] | Recurrent C. difficile infection; IBD; hepatic encephalopathy [12] |
| Probiotics (single or multi-strain) | Direct microbial antagonism; barrier enhancement; immunomodulation [12] | NEC in preterm infants; immune dysregulation; metabolic disorders [1] [12] |
| Prebiotics (HMOs, fiber) | Selective stimulation of beneficial microbes; SCFA production [1] | Infant development; metabolic syndrome; inflammatory conditions [1] |
| Phage Therapy | Targeted elimination of pathogenic bacteria [1] | Antibiotic-resistant infections; inflammatory bowel disease [1] |
| Engineered Live Biotherapeutics | Delivery of therapeutic molecules (e.g., immunomodulators, enzymes) [12] | Metabolic disorders; cancer; autoimmune diseases [12] |
Experimental Protocols for Investigating Host-Microbe Interactions
Protocol: Gnotobiotic Mouse Model for Microbiome-Function Studies
Purpose: To establish causal relationships between specific microbial taxa and host physiological responses using germ-free (GF) mouse models.
Materials:
- Germ-free isolators and housing equipment
- Sterilized food, water, and bedding
- Anaerobic chamber for microbial culture
- Specific pathogen-free (SPF) or defined microbial consortia
- DNA/RNA extraction kits
- Metabolomic analysis equipment (LC-MS, GC-MS)
Procedure:
- Animal Preparation: House GF mice in flexible film isolators with sterilized diet and water ad libitum.
- Microbial Inoculation:
- Prepare defined microbial consortium in anaerobic chamber under strict oxygen-free conditions.
- Administer 200μL of bacterial suspension (10^9 CFU/mL) via oral gavage to 6-8 week old GF mice.
- Include control groups: GF (no inoculation) and SPF (complex microbiota) controls.
- Monitoring and Sampling:
- Collect fecal samples at days 0, 3, 7, 14, 21 post-inoculation for microbial analysis.
- Monitor body weight, food intake, and behavioral parameters daily.
- Tissue Collection:
- At endpoint, euthanize mice and collect intestinal tissues, mesenteric lymph nodes, liver, and blood.
- Preserve tissues for: (i) flow cytometry (RPMI medium), (ii) gene expression (RNA later), (iii) histology (formalin fixation).
- Analysis:
- Verify microbial colonization via 16S rRNA sequencing and qPCR.
- Assess immune cell populations by flow cytometry (focus on Treg, Th17, dendritic cells).
- Measure metabolite profiles in cecal content and serum by LC-MS/GC-MS.
- Evaluate epithelial barrier function (Ussing chamber) and gene expression (RNA-seq).
Applications: This protocol enables researchers to determine causal mechanisms of specific microbes on host immunity, metabolism, and disease susceptibility [8].
Protocol: Flux Balance Analysis for Host-Microbe Metabolic Modeling
Purpose: To predict metabolic interactions between host and microbiota using constraint-based modeling approaches.
Materials:
- Genome-scale metabolic reconstructions (e.g., Recon3D for human, AGORA for microbes)
- COBRA Toolbox or similar metabolic modeling software
- High-performance computing resources
- Bacterial genome annotations
- Physiological constraint data (dietary intake, metabolic fluxes)
Procedure:
- Model Reconstruction:
- Obtain genome-scale metabolic reconstruction for host (Human1 or Recon3D) and microbial species of interest.
- For unannotated microbes, use ModelSEED or RAVEN toolbox for draft reconstruction.
- Network Integration:
- Create a compartmentalized model with separate spaces for: host cytosol, microbial cytosol, and gut lumen.
- Define metabolite exchange reactions between compartments.
- Set appropriate constraints for reaction fluxes based on physiological data.
- Simulation Setup:
- Define objective functions (e.g., maximize biomass production, maximize ATP yield, or maximize butyrate production).
- Apply dietary constraints based on experimental conditions.
- Implement parsimonious enzyme usage FBA (pFBA) to obtain realistic flux distributions.
- Simulation and Analysis:
- Perform flux balance analysis to predict metabolic fluxes under steady-state conditions.
- Conduct gene essentiality analysis by simulating single gene knockouts.
- Predict community metabolic output with different microbial compositions.
- Validate predictions with experimental metabolomics data.
Applications: FBA enables prediction of metabolic dependencies in host-microbe systems, identification of essential nutrients, and simulation of dietary or therapeutic interventions [13].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Microbiome-Host Interaction Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Gnotobiotic Models | Germ-free mice; OMM^12 mice; Altered Schaedler Flora | Controlled colonization studies; causal mechanism investigation [8] |
| Cell Culture Systems | Organoids; transwell epithelial systems; co-culture models | Barrier function studies; host-microbe interface modeling [1] |
| Sequencing Reagents | 16S rRNA primers (V3-V4); metagenomic library preps; RNA-seq kits | Microbial community profiling; functional potential assessment [14] |
| Metabolomics Standards | SCFA standards; bile acids; tryptophan metabolites; internal standards | Quantification of microbial metabolites in biological samples [9] [13] |
| Immunological Assays | ELISA for IgA, cytokines; flow cytometry antibodies (CD4, CD8, Treg panels) | Immune phenotyping; mucosal immunity assessment [8] |
| Bioinformatics Tools | QIIME 2; PICRUSt2; MetaPhlAn; HUMAnN; COBRA Toolbox | Microbiome data analysis; metabolic modeling [13] [14] |
The mechanistic understanding of immune signaling, metabolic interactions, and host-microbe crosstalk provides a robust foundation for developing microbiome-based diagnostics and therapeutics. The experimental protocols and research tools outlined herein enable systematic investigation of these mechanisms, accelerating the translation of microbiome science into clinical applications. As the field advances, integrating multi-omics data with computational models will be essential for personalizing microbiome-targeted interventions and realizing the full potential of microbiome medicine.
The human microbiome, particularly the gut microbiota, functions as a virtual endocrine organ that is essential for maintaining host homeostasis. Dysbiosis, defined as an imbalance in the microbial community structure, has been implicated in a vast spectrum of diseases through complex crosstalk along the gut-brain-immune axis [15] [16]. The clinical translation of microbiome science represents a paradigm shift in understanding disease etiology, introducing innovative diagnostic and therapeutic approaches for gastrointestinal, metabolic, immune, and neurological disorders [1] [17]. This application note synthesizes current evidence and provides structured protocols for investigating dysbiosis across disease contexts, framed within the broader thesis of advancing microbiome clinical translation for diagnostic and therapeutic applications.
Quantitative Associations Between Dysbiosis and Disease
Table 1: Gut Microbiota Alterations in Autoimmune Neurological Diseases (Meta-Analysis Findings)
| Disease Category | α-Diversity (Chao1 Index) | Key Bacterial Changes (Decreased) | Key Bacterial Changes (Increased) | Consistent β-Diversity Changes |
|---|---|---|---|---|
| Autoimmune Encephalitis (AIE) | Small decrease (SMD = -0.26) | Faecalibacterium, Roseburia | Streptococcus, Escherichia-Shigella | Inconsistent across studies |
| Neuromyelitis Optica Spectrum Disorders (NMOSD) | Small decrease (SMD = -0.26) | Faecalibacterium, Roseburia | Streptococcus, Escherichia-Shigella | Consistent differences observed |
| Myasthenia Gravis (MG) | Small decrease (SMD = -0.26) | Faecalibacterium, Roseburia | Streptococcus, Escherichia-Shigella | Inconsistent across studies |
| Multiple Sclerosis (MS) | Small decrease (SMD = -0.26) | Faecalibacterium, Roseburia | Streptococcus, Escherichia-Shigella | Inconsistent across studies |
| Healthy Controls | Reference range | High SCFA-producing bacteria | Low pathogenic bacteria | Reference community structure |
Data derived from systematic review and meta-analysis of 62 studies (n=3,126 patients, n=2,843 controls) [18]
Table 2: Dysbiosis-Associated Functional Metabolite Changes in Disease
| Disease Category | SCFA Production | Bile Acid Metabolism | Neuroactive Metabolites | Inflammatory Mediators |
|---|---|---|---|---|
| GI Dysmotility (IBS/SIBO) | Decreased butyrate | Altered deconjugation | Serotonin imbalance | Increased LPS, TNF-α |
| Metabolic Disorders (T2D) | Decreased butyrate | Impaired signaling | GABA/5-HT alterations | Low-grade inflammation |
| Neurodegenerative (AD/PD) | Significantly reduced | Dysregulated | Dopamine/GABA deficits | IL-6, IL-1β elevation |
| Autoimmune Neurological | Reduced (Faecalibacterium) | Not reported | Not reported | Systemic inflammation |
| Drug-Induced Brain Injury | Depleted butyrate | Not reported | Serotonin, dopamine disruption | Oxidative stress, ROS |
SCFAs: Short-chain fatty acids; LPS: Lipopolysaccharide; ROS: Reactive oxygen species; Data compiled from multiple sources [15] [16] [19]
Experimental Protocols for Dysbiosis Research
Protocol: Multi-Omic Profiling of Gut Microbiota in Disease Cohorts
Application: Comprehensive characterization of microbial dysbiosis in patient populations for biomarker discovery and mechanistic insights.
Materials and Reagents:
- Stool collection kits (DNA/RNA stabilizer)
- DNA extraction kits (e.g., QIAamp PowerFecal Pro DNA Kit)
- Library preparation reagents (Illumina compatible)
- LC-MS/MS equipment for metabolomics
- Bioinformatics pipelines (QIIME 2, LEfSe, MetaPhlAn)
Procedure:
- Patient Recruitment and Stratification: Recruit well-characterized patient cohorts and matched controls. Record clinical metadata, disease activity, medication use, and dietary patterns.
- Sample Collection and Preservation: Collect fresh stool samples using standardized collection kits with DNA/RNA stabilizers. Aliquot samples for various analyses and store at -80°C.
- DNA Extraction and Quality Control: Perform standardized DNA extraction with bead beating for mechanical lysis. Verify DNA quality and quantity using spectrophotometry and gel electrophoresis.
- Shotgun Metagenomic Sequencing: Prepare sequencing libraries targeting 20-50 million reads per sample. Sequence on Illumina platform (2x150bp). Include positive and negative controls.
- Metabolomic Profiling: Extract metabolites using methanol:water:chloroform. Analyze SCFAs, bile acids, and tryptophan metabolites via LC-MS/MS with internal standards.
- Bioinformatic Analysis: Process sequencing data through quality filtering, host DNA removal, and taxonomic profiling. Conduct functional annotation (KEGG, MetaCyc). Integrate with metabolomic data using multivariate statistics.
- Validation: Confirm key findings using qPCR for specific bacterial taxa or targeted metabolomics in independent validation cohort.
Quality Controls: Include extraction blanks, positive control communities (ZymoBIOMICS), and sample replicates to monitor technical variability [18] [4] [20].
Protocol: Assessing Gut-Brain Axis Communication in Preclinical Models
Application: Mechanistic investigation of microbiota-host interactions in neurological disorders.
Materials and Reagents:
- Germ-free or gnotobiotic mouse models
- Fecal microbiota transplantation (FMT) equipment
- Behavioral testing apparatus
- Immunoassay kits for cytokines
- Tissue processing reagents for histology
Procedure:
- Model Establishment: Use germ-free mice or antibiotic-treated specific pathogen-free mice to create manipulated microbiota states.
- Fecal Microbiota Transplantation: Prepare donor inoculum from human patients or characterized mouse models. Administer via oral gavage to recipient mice (200μL daily for 3 days).
- Behavioral Phenotyping: Conduct standardized tests at consistent time points: open field (anxiety), forced swim (depression-like), Y-maze (cognition), and motor coordination tests.
- Tissue Collection and Processing: Collect brain, gut, and blood samples. Perfuse animals with PBS before tissue collection for optimal preservation.
- Immunological Profiling: Measure cytokine levels (IL-6, TNF-α, IL-1β) in plasma and brain homogenates using ELISA or multiplex assays. Analyze immune cell populations in brain and gut by flow cytometry.
- Blood-Brain Barrier Assessment: Evaluate BBB integrity using Evans Blue extravasation and tight junction protein expression (claudin-5, occludin) via immunohistochemistry.
- Histopathological Analysis: Examine brain sections for microglial activation (Iba1 staining), neuronal damage, and pathological protein aggregation.
Validation: Confirm microbial engraftment via 16S rRNA sequencing of recipient fecal samples. Correlate behavioral changes with microbial and immunological parameters [21] [19] [20].
Signaling Pathways in Microbiota-Host Communication
Figure 1: Gut-Brain-Immune Axis Signaling in Dysbiosis
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Microbiome-Disease Research
| Research Tool | Application | Specific Examples | Function in Experimental Design |
|---|---|---|---|
| DNA Stabilization Kits | Sample preservation | DNA/RNA Shield, RNAlater | Maintains nucleic acid integrity during storage and transport |
| Metagenomic Kits | Community profiling | QIAamp PowerFecal Pro, DNeasy PowerSoil | Comprehensive DNA extraction from complex samples |
| SCFA Standards | Metabolite quantification | Acetate, propionate, butyrate reference standards | Quantification of key microbial metabolites via LC-MS/MS |
| Cytokine Panels | Immune profiling | Luminex multiplex assays, ELISA kits | Measurement of inflammatory mediators in serum and tissues |
| Gnotobiotic Models | Mechanistic studies | Germ-free mice, Humanized microbiota mice | Establish causal relationships between microbiota and disease |
| Biotherapeutic Strains | Intervention studies | Akkermansia muciniphila, Faecalibacterium prausnitzii | Test therapeutic potential of specific commensals |
| Phage Cocktails | Targeted depletion | Klebsiella pneumoniae-targeting phages | Selective elimination of pathobionts |
| Tight Junction Antibodies | Barrier integrity | Anti-occludin, anti-claudin-5 | Assess gut and blood-brain barrier function |
Compiled from experimental methodologies across cited references [21] [18] [4]
The systematic investigation of dysbiosis across gastrointestinal, metabolic, immune, and neurological disorders reveals both shared and disease-specific alterations in microbial communities and their functional outputs. The quantitative data and standardized protocols provided in this application note establish a framework for advancing microbiome research from associative studies to mechanistic investigations and therapeutic applications. As the field moves toward clinical translation, rigorous experimental design, standardized methodologies, and multi-modal data integration will be essential for developing microbiome-based diagnostics and therapeutics that can be implemented in routine clinical care [17] [22]. The continued elucidation of microbiota-host signaling pathways will undoubtedly yield novel therapeutic targets for a wide spectrum of dysbiosis-associated diseases.
The initial colonization and subsequent development of the gut microbiome during early life represent a critical developmental window with profound implications for long-term health. Early-life gut microbiome (GM) development plays a pivotal role in shaping the immune system, developing the intestinal tract, and influencing host metabolism [23]. This process is strongly influenced by several determinants, including gestational age at birth, mode of delivery, neonatal feeding practices, early-life stress, and exposure to perinatal antibiotics [23]. The establishment of the GM after birth evolves throughout the host's lifespan, from infancy to advanced age, ultimately achieving homeostasis through complex ecological and trophic interrelationships between microbial members and the human host [23]. However, disruptions during this critical period through GM dysbiosis may alter developmental programming, leading to long-term adverse health outcomes including allergic diseases, metabolic disorders, type 1 diabetes, inflammatory bowel disorders, and atherosclerotic cardiovascular diseases [23]. This Application Note provides a comprehensive framework for investigating early-life microbiome development, with standardized protocols and analytical tools to advance research in microbiome clinical translation, diagnostics, and therapeutic applications.
Foundational Concepts and Determinants
The establishment of the neonatal gut microbiome commences through maternal microbial transmission, with recent evidence challenging the historical "sterile womb paradigm" [23]. While the intrauterine environment remains a subject of scientific debate, substantial microbial colonization occurs during and immediately after birth, primarily sourced from maternal gut, vaginal, and placental reservoirs [24]. Microbial source-tracking analyses using algorithms like FEAST indicate that the maternal gut and placenta serve as major contributors to neonatal meconium colonization, with gut-derived input increasing over time [24].
Early microbial succession patterns demonstrate remarkable conservation across diverse human populations, suggesting universal developmental trajectories [25]. Large-scale meta-analyses of 3,154 shotgun-sequenced samples from 1,827 infants across 12 countries reveal that gut microbial taxonomic profiles can predict infant age with high temporal resolution (±3 months) for the first 1.5 years of life [25]. This predictable succession pattern provides a normative benchmark of "microbiome age" for assessing gut maturation alongside other measures of child development.
Table 1: Key Determinants of Early-Life Microbiome Development
| Determinant Category | Specific Factors | Impact on Microbiome Composition | Long-Term Health Associations |
|---|---|---|---|
| Perinatal Factors | Mode of delivery (vaginal vs. cesarean) | Alters initial microbial inoculum; vaginal delivery provides maternal vaginal and fecal microbes | Immune-mediated diseases; metabolic disorders |
| Gestational age at birth | Preterm birth associated with delayed colonization and reduced diversity | Neurodevelopmental impairments; necrotizing enterocolitis | |
| Maternal microbiome status | Determines microbial sources available for vertical transmission | Allergic diseases; immune programming | |
| Postnatal Exposures | Feeding practices (breastfeeding vs. formula) | Breastfeeding promotes Bifidobacterium; formula feeding increases diversity earlier | Immune development; metabolic programming |
| Antibiotic exposure | Reduces microbial diversity and SCFA production; promotes antimicrobial resistance | Allergic diseases; obesity; neurodevelopmental conditions | |
| Early-life stress | Reduces key SCFA-producing taxa; alters microbiome metabolic output | Mental health disorders; inflammatory diseases | |
| Interventions | Probiotic supplementation | Transiently alters composition; enhances microbial stability | Reduced eczema incidence; improved immune markers |
| Prebiotic supplementation | Promotes growth of beneficial taxa (Bifidobacterium, Lactobacillus) | Enhanced gut barrier function; immune modulation |
Quantitative Models and Normative Benchmarks
The development of quantitative models for gut microbiome maturation provides powerful tools for assessing normative development and identifying deviations associated with disease states. Recent research has established a random forest model using gut microbial taxonomic relative abundances from metagenomes that achieves high temporal resolution (±3 months) for the first 1.5 years of life, with a root mean square error of 2.56 months [25]. This model was trained on 3,154 samples from 1,827 infants across 12 countries, demonstrating conserved microbial succession patterns across diverse populations [25].
Key taxonomic predictors of microbiome age include declines in Bifidobacterium spp. and increases in Faecalibacterium prausnitzii and Lachnospiraceae species [25]. Alpha-diversity, measured as the Shannon index, serves as the third most important predictor (4.86% of total importance, R(age) = +0.52) [25]. These patterns reflect feeding transitions and dietary exposures, with functional analysis confirming trends in key microbial genes involved in these developmental milestones.
Table 2: Key Taxonomic Predictors of Microbiome Age in Early Development
| Taxonomic Predictor | Direction with Age | Relative Importance | Functional Significance |
|---|---|---|---|
| Faecalibacterium prausnitzii | Positive | High (17.3% combined with A. hadrus) | Butyrate production; anti-inflammatory properties |
| Anaerostipes hadrus | Positive | High (17.3% combined with F. prausnitzii) | SCFA production; metabolic health |
| Bifidobacterium longum | Negative | 2.2% combined with B. breve | Human milk oligosaccharide metabolism; immune modulation |
| Bifidobacterium breve | Negative | 2.2% combined with B. longum | Early gut colonizer; probiotic candidate |
| Lachnospiraceae species | Positive | Variable | Plant polysaccharide digestion; SCFA production |
| Dorea longicatena | Positive | Variable | Geographic variation; elevated in South African cohorts |
| Escherichia coli | Variable | Variable | Elevated in Brazilian cohorts; potential pathobiont |
| Shannon α-diversity | Positive | 4.86% | Overall community richness and evenness |
Mechanistic mathematical models representing the interplay between gut ecology and adaptive immunity provide insights into the ontogeny of immune tolerance [26]. These models integrate exogenous inputs into the gut lumen with endogenous dynamics in the gut lumen and organized gut-associated lymphoid tissue (GALT) inductive sites. Such frameworks formalize the concept of 'immune education' during early life, enabling exploration of diagnostic markers, clinical intervention strategies, and preventive measures before pathological trajectories are imprinted [26].
Experimental Protocols and Methodologies
Protocol: Longitudinal Microbiome Sampling in Neonatal Populations
Application: This protocol standardizes the collection, processing, and storage of neonatal microbiome samples for longitudinal studies, enabling robust multi-omics integration.
Materials:
- Sterile fecal collection kits with nucleic acid preservatives (e.g., RNA/DNA Shield)
- Vaginal swab kits (e.g., ESwab collection system)
- Placental tissue collection: sterile surgical scissors, scalpels, cryovials
- DNA/RNA-free consumables
- -80°C freezer or liquid nitrogen storage system
Procedure:
- Maternal Sample Collection:
- Collect maternal fecal samples (1-2 g) in 50 mL centrifuge tubes during defecation
- Obtain vaginal samples by trained professionals using sterile swabs
- Collect placental tissue within 10 minutes of delivery under strict aseptic conditions
Neonatal Sample Collection:
- Collect meconium (day 1) and fecal samples (days 3, 14, and longitudinally through 6 months)
- For preterm infants in NICU settings, consider daily sampling when possible
- Aliquot samples at source when immediate cold chain unavailable
Sample Processing:
- Extract genomic DNA using CTAB/SDS method or commercial kits
- Assess DNA purity and concentration by 1% agarose gel electrophoresis
- Amplify V3-V4 hypervariable region of 16S rRNA gene using primers 341F/806R
- Perform library construction using Ion Plus Fragment Library Kit
- Sequence on Ion S5 XL platform or comparable system
Quality Control:
- Include no-template controls during amplification
- Monitor for contamination through extraction blanks
- Rarefy to even sequencing depth (minimum 5,338 reads/sample) for diversity analyses [24]
Analytical Workflow:
- Process sequence data through standardized bioinformatics pipeline (e.g., BioBakery V3) [25]
- Cluster sequences into OTUs at 97% similarity threshold using UPARSE
- Perform taxonomic annotation using Silva Database via Mothur
- Conduct microbial source tracking using FEAST algorithm
- Integrate with metabolomic and proteomic data for multi-omics analysis
Protocol: Probiotic Intervention during Pregnancy and Early Infancy
Application: Evaluate the impact of prenatal and early-life probiotic supplementation on maternal-to-neonatal microbial transmission and infant gut development.
Materials:
- Probiotic formulation (e.g., Bifidobacterium longum, Lactobacillus delbrueckii bulgaricus, Streptococcus thermophilus)
- Placebo tablets identical in appearance
- Standardized dietary record forms
- Compliance assessment tools (pill counts, participant diaries)
Procedure:
- Participant Recruitment:
- Recruit pregnant women before 32nd gestational week
- Apply inclusion criteria: singleton pregnancy, first-time pregnancy, gestational age ≥37 weeks at delivery
- Exclude participants with regular probiotic/prebiotic consumption, antibiotic use, or pregnancy complications
Randomization and Intervention:
- Randomize participants to probiotic or control group
- Administer probiotic supplement (e.g., Golden Bifid tablets) twice daily from gestational week 32 until delivery
- Control group receives no intervention or placebo
- Monitor for gastrointestinal symptoms and assess compliance through returned packaging
Sample Collection and Analysis:
- Collect maternal fecal, vaginal, and placental samples at full term
- Obtain neonatal fecal samples longitudinally (days 1, 3, 14, 6 months)
- Perform 16S rRNA gene sequencing and microbial community profiling
- Conduct volatility analysis to assess microbial stability
- Perform source-tracking analysis using FEAST algorithm
Outcome Measures:
- Alpha and beta diversity metrics of neonatal meconium microbiota
- Relative contributions of maternal microbial sources to neonatal gut colonization
- Microbial stability during early colonization period (days 1-3)
- Persistence of intervention effects through 6 months postpartum
Signaling Pathways and Mechanistic Insights
The gut-brain axis represents a critical signaling network through which the early-life microbiome influences neurodevelopment, particularly in vulnerable preterm populations. Five primary mechanistic pathways link microbial disturbances to adverse neurodevelopmental outcomes: (1) immune activation and white matter injury; (2) short-chain fatty acids (SCFAs)-mediated neuroprotection; (3) tryptophan-serotonin metabolic signaling; (4) hypothalamic-pituitary-adrenal (HPA) axis modulation; and (5) integrity of intestinal and blood-brain barriers [27].
Diagram 1: Gut-Brain Axis Signaling Pathways in Early-Life Neurodevelopment. This diagram illustrates the primary mechanistic pathways through which early-life microbiome disruptions influence neurodevelopmental outcomes, particularly in preterm infants.
The immune-mediated pathway involves microbiome-driven activation of systemic immune responses that can lead to white matter injury in the developing brain [27]. SCFAs, including acetate, propionate, and butyrate, serve as crucial microbial metabolites that exert neuroprotective effects through multiple mechanisms, including histone deacetylase inhibition and support of mitochondrial function [28] [27]. The tryptophan-serotonin pathway demonstrates how microbial metabolism influences neurotransmitter systems critical for mood, cognition, and behavior [27]. Early-life stress and dysbiosis can persistently alter HPA axis function, affecting stress responsiveness and emotional regulation throughout life [28]. Finally, microbiome composition directly influences the integrity of both intestinal and blood-brain barriers, potentially permitting increased translocation of inflammatory mediators into the CNS [27].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Early-Life Microbiome Studies
| Reagent Category | Specific Product/Strain | Application | Key Considerations |
|---|---|---|---|
| Probiotic Strains | Bifidobacterium longum BB536 | Prenatal supplementation studies | Reduces Crohn's disease severity; repairs mucus integrity [12] |
| Lactobacillus rhamnosus GG (LGG) | Early-life interventions | Modulates immune responses; affects gut bifidobacterial diversity [23] | |
| Bifidobacterium adolescentis & B. bifidum | Allergy prevention studies | Colonization patterns differ in allergic vs. non-allergic mothers [23] | |
| DNA Extraction Kits | CTAB/SDS method | Microbial community analysis | Provides high-quality DNA for low-biomass samples [24] |
| Sequencing Primers | 341F (CCTACGGGNGGCWGCAG) & 806R (GGACTACHVGGGTWTCTAAT) | 16S rRNA gene amplification (V3-V4 region) | Standardized for Illumina platforms; enables cross-study comparisons [24] |
| Bioinformatics Tools | BioBakery V3 pipeline | Metagenomic analysis | Harmonized computational processing for cross-study analyses [25] |
| FEAST algorithm | Microbial source tracking | Quantifies contributions of maternal microbial sources to neonatal gut [24] | |
| Cell Culture Media | Custom SCFA mixtures (acetate, propionate, butyrate) | Mechanistic in vitro studies | Physiological concentrations (μM to mM range); pH adjustment critical [28] |
Clinical Translation and Therapeutic Applications
Microbiome therapeutics represent a promising frontier for addressing early-life programming of long-term health outcomes. Current approaches include additive therapy (probiotics, fecal microbiota transplantation), subtractive therapy (antibiotics, bacteriophages), and modulatory therapy (prebiotics, microbial metabolites) [12]. Fecal microbiota transplantation (FMT) has demonstrated remarkable efficacy in recurrent Clostridioides difficile infection, with recovery rates exceeding 90% [12]. However, its application in other conditions like ulcerative colitis shows variable success, highlighting the need for optimized, targeted approaches.
Probiotic interventions during pregnancy and early infancy show potential for preventing specific conditions. Prenatal supplementation with Lactobacillus rhamnosus GG has been associated with reduced atopic dermatitis incidence, while combinations of multiple strains may enhance microbial stability in early colonization [23] [24]. The timing and duration of interventions appear critical, with transient effects observed in many studies and sustained changes requiring ongoing exposure or critical window targeting.
Emerging frontiers in microbiome therapeutics include engineered microbial consortia designed for specific functions and pharmacomicrobiomics – understanding how microbiome variations influence individual drug responses [10]. This integration of microbiome science with pharmacology holds particular promise for precision medicine approaches to pediatric and lifelong health.
Concluding Remarks and Future Directions
The critical window of early-life microbiome development represents both vulnerability and opportunity – a period when interventions may have disproportionate and lasting effects on health trajectories. The standardized protocols, analytical frameworks, and mechanistic insights provided in this Application Note establish a foundation for advancing research in microbiome clinical translation. Future directions should focus on validating multi-omics biomarkers across diverse populations, developing targeted therapeutic approaches for specific dysbiosis patterns, and establishing safety and efficacy guidelines for early-life microbiome interventions. As our understanding of microbial succession patterns and host-microbe interactions deepens, the potential grows for harnessing early-life programming to promote lifelong health and prevent disease.
Microbiome Modulators in the Clinic: From FMT to Next-Generation Biotherapeutics
Recurrent Clostridioides difficile infection (rCDI) represents a profound clinical challenge characterized by a destructive cycle of antibiotic treatments and subsequent recurrences that stem from persistent dysbiosis of the gut microbiome. The recent approval of two live biotherapeutic products—REBYOTA (fecal microbiota, live - jslm) and VOWST (fecal microbiota spores, live - brpk)—marks a transformative advancement in microbiome-based therapeutics, offering the first standardized, FDA-approved approaches to microbiome restoration [29]. These products represent the successful clinical translation of decades of research on the gut microbiome's crucial role in pathogen resistance, moving fecal microbiota transplantation from a largely unregulated procedure to a rigorously controlled pharmaceutical paradigm [30] [29]. This article provides detailed application notes and experimental protocols for these groundbreaking therapies within the context of microbiome clinical translation, offering researchers and drug development professionals comprehensive guidance on their mechanisms, efficacy, and implementation.
Product Profiles and Comparative Analysis
REBYOTA: Single-Dose Rectal Microbiota Suspension
REBYOTA is a pre-packaged, single-dose 150 mL microbiota suspension for rectal administration consisting of a liquid mix of up to trillions of live microbes, including Bacteroides [31]. It is the first FDA-approved single-dose fecal microbiota transplant (FMT) indicated for the prevention of recurrence of CDI in individuals 18 years and older following antibiotic treatment for recurrent CDI [31] [30]. The product's standardized manufacturing process adheres to good manufacturing practices (GMP) and employs consistent, rigorous health screening of donors with each dose comprising a single donor's donation for ease of traceability [32].
VOWST: Orally Administered Fecal Microbiota Spores
VOWST represents the first orally administered fecal microbiota product approved by the FDA for prevention of rCDI recurrence in adults [33]. Its dosing regimen consists of four capsules taken once a day for three consecutive days [33]. VOWST is characterized as a purified bacterial spore suspension sourced from qualified donors and composed of Firmicutes spores, containing between 1×10^6 and 3×10^7 Firmicutes spore colony forming units [34]. The manufacturing process includes ethanol inactivation designed to help remove vegetative/pathogenic bacteria, fungi, parasites, and viruses, followed by filtration and centrifugation to remove solids and residual ethanol [34].
Table 1: Comparative Profile of FDA-Approved Microbiome Therapies for rCDI
| Parameter | REBYOTA | VOWST |
|---|---|---|
| FDA Approval Date | November 30, 2022 [30] | April 26, 2023 [33] [35] |
| Administration | Single-dose rectal suspension [31] | 4 capsules daily for 3 consecutive days (oral) [33] |
| Composition | Liquid mix of live microbes including Bacteroides and Firmicutes [32] | Purified Firmicutes spores [34] |
| Microbial Load | 15 billion to 7.5 trillion CFU per dose [32] | 1×10^6 to 3×10^7 Firmicutes spore CFU [34] |
| Key Clinical Trial | PUNCH CD3 Phase 3 [30] | ECOSPOR III Phase 3 [35] [36] |
| Treatment Success at 8 Weeks | 70.6% (vs 57.5% placebo) [30] | 88% (vs 60% placebo) [36] |
Table 2: Clinical Efficacy and Safety Profile Comparison
| Parameter | REBYOTA | VOWST |
|---|---|---|
| Sustained Response (6 months) | >90% (in responders) [30] | 79% recurrence-free [36] |
| Real-World Effectiveness | 75%-82.9% treatment success at 8 weeks [37] | 91% recurrence-free at 8 weeks (ECOSPOR IV) [36] |
| Most Common Adverse Events | Abdominal pain (8.9%), diarrhea (7.2%), bloating (3.9%), gas (3.3%), nausea (3.3%) [31] | Abdominal bloating (31.1%), fatigue (22.2%), constipation (14.4%), chills (11.1%), diarrhea (10.0%) [33] [35] |
| IBD Patient Efficacy | 78.9% treatment success at 8 weeks [38] | Limited data available |
| Mechanistic Insights | Increases beneficial Bacteroidia and Clostridia; decreases Gammaproteobacteria and Bacilli [31] | Engraftment of dose species greater than antibiotics alone through 8 weeks [34] |
Mechanism of Action and Engraftment Analysis
Microbiome Restoration Pathways
The therapeutic efficacy of both REBYOTA and VOWST centers on restoring a balanced gut microbiome to reestablish colonization resistance against C. difficile. In the case of REBYOTA, analysis of the Phase 3b CDI-SCOPE study demonstrated that microbiome composition and the Microbiome Health Index for post-antibiotic dysbiosis (MHI-A) shifted significantly toward the REBYOTA composition among responders [31]. Specifically, beneficial bacteria (Bacteroidia and Clostridia) increased in abundance, while disease-causing bacteria (Gammaproteobacteria and Bacilli) decreased following administration [31]. Importantly, MHI-A values increased from baseline to 6 months after treatment, indicating a sustained shift toward a healthier microbiome state [31].
For VOWST, which utilizes a purified spore approach, engraftment data from exploratory analysis in ECOSPOR III demonstrated that numbers of engrafting VOWST dose species were greater than antibiotics alone at week 1 and remained higher through week 8 [34]. The mechanism is thought to involve rapid facilitation of gut microbiome restoration and inhibition of spore germination that can perpetuate the cycle of C. difficile recurrence [34].
Diagram 1: Mechanism of Action Pathways for REBYOTA and VOWST
Engraftment Dynamics and Microbiome Metrics
Assessment of engraftment success requires specialized methodologies and biomarkers. For REBYOTA, investigators analyzed microbiome composition, diversity of bacterial populations, and the Microbiome Health Index for post-antibiotic dysbiosis (MHI-A) in participants with stool samples provided between baseline and 6 months [31]. The significant shift in MHI-A values toward healthier states provides a quantifiable metric for therapeutic response [31].
For VOWST, stool specimens for whole metagenomic sequencing were obtained at baseline and at weeks 1, 2, and 8 in the ECOSPOR III trial [34]. Of the 182 participants, 29 were excluded from analyses because of missing specimens or protocol deviations, highlighting the importance of rigorous sample collection protocols in engraftment studies [34]. The relationship between these engraftment data and efficacy or safety has not been definitively established, representing an area of ongoing investigation [34].
Experimental Protocols and Methodologies
Clinical Trial Design for Microbiome Therapeutics
The pivotal clinical trials for REBYOTA and VOWST provide robust templates for future microbiome therapeutic development:
PUNCH CD3 Trial Protocol (REBYOTA):
- Design: Randomized, double-blind, placebo-controlled Phase 3 trial
- Participants: 262 patients with recurrent CDI; 177 received REBYOTA, 85 received placebo
- Primary Endpoint: Absence of CDI diarrhea for eight weeks following antibiotic treatment
- Statistical Analysis: Bayesian model estimating treatment success rate
- Results: 70.6% success rate for REBYOTA vs. 57.5% for placebo (99.1% posterior probability of superiority)
- Long-term Follow-up: >90% of participants maintaining remission through 6 months post-treatment [30]
ECOSPOR III Trial Protocol (VOWST):
- Design: Multicenter, randomized, placebo-controlled trial across 50+ sites in U.S. and Canada
- Participants: Adults with recurrent CDI
- Primary Endpoint: CDI recurrence at eight weeks post-treatment
- Results: 88% of VOWST group recurrence-free at 8 weeks vs. 60% for placebo; 79% recurrence-free at 6 months vs. 53% for placebo [36]
- Open-label Extension: ECOSPOR IV study showed 91% recurrence-free at 8 weeks and 86% at 24 weeks [36]
Microbiome Sampling and Analysis Protocol
Sample Collection:
- Collect stool specimens at baseline (pre-treatment) and at predetermined intervals post-treatment (weeks 1, 2, 8, and 24)
- Immediately freeze samples at -80°C to preserve microbial viability and genetic integrity
- Document and track any protocol deviations or missing specimens that may affect analysis
DNA Extraction and Sequencing:
- Perform standardized DNA extraction using commercially available kits designed for microbial diversity studies
- Conduct whole metagenomic sequencing using Illumina or comparable platforms
- Include appropriate controls for contamination and sequencing depth
Bioinformatic Analysis:
- Process raw sequencing data through quality control (FastQC), adapter trimming, and host DNA depletion
- Perform taxonomic profiling using reference databases (Greengenes, SILVA)
- Calculate diversity metrics (alpha and beta diversity) and differential abundance testing
- For VOWST specifically, track engraftment of dose species compared to baseline [34]
- For REBYOTA, analyze Microbiome Health Index for post-antibiotic dysbiosis (MHI-A) [31]
Diagram 2: Clinical Trial Workflow for Microbiome Therapies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Microbiome Therapeutic Development
| Reagent/Resource | Function/Application | Specifications/Alternatives |
|---|---|---|
| Stool Collection Kits | Standardized sample acquisition for microbiome analysis | Includes DNA/RNA stabilizing buffers, temperature control during transport |
| DNA Extraction Kits | Microbial DNA isolation for metagenomic sequencing | MoBio PowerSoil Kit or equivalent; optimized for Gram-positive bacteria |
| Whole Metagenomic Sequencing | Comprehensive taxonomic and functional profiling | Illumina NovaSeq, PacBio, or Oxford Nanopore platforms |
| Bioinformatic Pipelines | Analysis of microbial community data | QIIME 2, mothur, or custom workflows for taxonomic assignment |
| Cdiff32 Instrument | Health-related quality of life assessment in CDI patients | Validated survey instrument capturing physical, mental, social functioning [37] |
| Anaerobic Chambers | Cultivation of oxygen-sensitive gut microorganisms | Coy Laboratory Type B Vinyl Anaerobic Chambers or equivalent |
| Gnotobiotic Mouse Models | In vivo assessment of microbiome engraftment and function | Germ-free facilities for human microbiota transplantation studies |
| Cell-Based Assays | Assessment of bacterial sporulation, germination, and cytotoxicity | Caco-2 cell lines for epithelial barrier function; Vero cells for toxin testing |
Future Directions and Research Applications
The development of REBYOTA and VOWST represents just the beginning of microbiome-based therapeutics. Ongoing clinical trials continue to explore the efficacy of these products in special populations, including patients with inflammatory bowel disease (IBD). A recent subgroup analysis of PUNCH CD3-OLS demonstrated that REBYOTA was safe and efficacious in patients with IBD, showing a 78.9% treatment success rate at 8 weeks and 91.1% sustained clinical response at 6 months, similar to rates in non-IBD participants [38]. This is particularly significant as IBD is a common risk factor for rCDI, yet patients with IBD are often excluded from prospective trials [38].
Future research directions include:
- Optimizing Administration Protocols: Investigating extended antibiotic washout periods beyond the standard 24-72 hours [31]
- Novel Formulations: Developing next-generation products with enhanced stability and administration profiles
- Mechanistic Studies: Delineating precise microbial shifts and metabolic changes associated with successful treatment
- Combination Therapies: Exploring microbiota restoration in conjunction with immunomodulatory agents
- Expanded Indications: Investigating applications in other gastrointestinal disorders, metabolic conditions, and neurological diseases [30] [35]
The standardized manufacturing processes, rigorous donor screening protocols, and robust clinical evidence supporting REBYOTA and VOWST establish a benchmark for future microbiome-based therapeutics, paving the way for expanded applications in gastrointestinal and extraintestinal disorders linked to dysbiosis [29].
The field of Live Biotherapeutic Products (LBPs) has progressed from a scientific concept to a validated therapeutic modality, with the global human microbiome market projected to exceed USD 5.1 billion by 2030 [39]. Following the landmark approvals of Rebyota and Vowst for recurrent Clostridioides difficile infection (rCDI), the pipeline has expanded dramatically, now encompassing over 240 candidates in development across more than 100 companies [39]. This article provides a detailed overview of the current LBP pipeline and experimental frameworks essential for advancing these next-generation therapeutics.
LBP Pipeline and Therapeutic Landscape
The LBP pipeline reflects a strategic diversification from initial infectious disease applications into complex chronic conditions, including oncology, metabolic, and neurodegenerative diseases [39]. The table below summarizes selected prominent LBP candidates in development.
Table 1: Selected Live Biotherapeutic Products (LBPs) in Clinical Development
| Company / Product | Indication(s) | Modality & Mechanism | Development Stage |
|---|---|---|---|
| Seres Therapeutics – Vowst (SER-109) [39] | rCDI; exploring ulcerative colitis | Oral LBP; purified Firmicutes spores that recolonize the gut and restore bile acid metabolism | Approved (FDA) |
| Ferring Pharma/Rebiotix – Rebyota (RBX2660) [39] | rCDI | Rectally administered microbiota suspension; restores broad microbial diversity | Approved (FDA) |
| Vedanta Biosciences – VE303 [40] [39] | rCDI | Defined eight-strain bacterial consortium; promotes colonization resistance | Phase III |
| Vedanta Biosciences – VE202 [39] | Ulcerative Colitis (IBD) | Eight-strain consortium designed to induce regulatory T-cell responses | Phase II |
| 4D Pharma – MRx0518 [39] | Oncology (solid tumors) | Single-strain Bifidobacterium longum engineered to activate innate and adaptive immunity | Phase I/II |
| MaaT Pharma – MaaT013 [39] | Graft-versus-host disease | Pooled, high-richness microbiome ecosystem therapy to restore immune homeostasis | Phase III |
| Synlogic – SYNB1934 [39] | Phenylketonuria (PKU) | Engineered E. coli Nissle expressing phenylalanine ammonia lyase to metabolize phenylalanine | Phase II |
| Akkermansia Therapeutics – Ak02tm [39] | Metabolic disorders | Pasteurized Akkermansia muciniphila for improving insulin sensitivity | Phase I/II |
| Finch Therapeutics – CP101 [40] [39] | rCDI; exploring IBD | Full-spectrum microbiota consortium delivered via oral capsules | Phase II/III |
| BiomX – BX003 [39] | Atopic dermatitis & acne | Topical bacteriophage cocktail targeting Cutibacterium species | Phase II |
The distribution of candidates across development stages indicates a sector still in its early clinical translation. An estimated 60% of microbiome therapeutics are in preclinical stages, while Phase I, Phase II, and Phase III trials represent approximately 20%, 15%, and less than 5% of the pipeline, respectively [39]. This distribution underscores the significant growth and future attrition expected as programs advance.
Key Therapeutic Areas and Modalities
- Gastrointestinal Disorders: While rCDI remains a cornerstone, development has actively expanded into inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS) [39] [41]. For complex diseases, the therapeutic rationale moves beyond simple ecosystem restoration to precise immunomodulation [42].
- Oncology: LBPs are being developed as adjuvants to enhance response to checkpoint inhibitors and manage complications like graft-versus-host disease (GvHD) [39] [42].
- Metabolic and Neurodegenerative Diseases: Strains like Akkermansia muciniphila are being evaluated for metabolic benefits [39], while the microbiota-gut-brain axis is a target for conditions like Parkinson's disease [40] [11].
- Product Architectures: Three distinct LBP architectures have emerged to address different clinical needs [42]:
- Whole-Community Products: Designed to replicate the ecosystem restoration of FMT (e.g., Rebyota).
- Partial-Community or Enriched Products: Balance diversity with manufacturing control (e.g., Vowst, MaaT013).
- Defined-Strain Products: Target specific mechanisms of action using rationally selected single strains or consortia (e.g., VE303, MRx0518).
Experimental Protocols for LBP Development
Advancing LBPs requires specialized protocols that address the unique challenges of working with live microorganisms. The following sections detail key methodologies for strain selection and efficacy assessment.
Protocol: Genome-Scale Metabolic Model (GEM)-Guided Strain Screening
Application Note: This in silico protocol uses GEMs to rationally shortlist LBP candidate strains from public databases like AGORA2 (which contains 7,302 curated strain-level GEMs of gut microbes) based on predicted therapeutic functions [40]. It efficiently narrows down candidates for experimental validation.
Table 2: Key Reagents for GEM-Guided Screening
| Research Reagent / Tool | Function / Explanation |
|---|---|
| AGORA2 Model Resource [40] | A library of curated, strain-level genome-scale metabolic models for gut microbes; serves as the starting database for in silico screening. |
| Flux Balance Analysis (FBA) [40] | A computational method used to simulate metabolic flux and predict growth rates, nutrient uptake, and metabolite secretion under defined constraints. |
| Therapeutic Metabolite List | A user-defined list of disease-relevant beneficial (e.g., butyrate) or detrimental metabolites used to query model outputs. |
| Pairwise Interaction Simulation | In silico method to predict mutualistic, competitive, or neutral interactions between a candidate LBP strain and key resident gut microbes. |
Procedure:
- Define Therapeutic Objective: Based on disease pathophysiology (e.g., butyrate deficiency in IBD), define the desired metabolic output or function for the LBP [40].
- Retrieve and Constrain GEMs: Select relevant microbial GEMs from AGORA2 or reconstruct new ones. Apply constraints to simulate the disease-relevant gut environment (e.g., nutrient availability) [40].
- In Silico Phenotype Screening:
- Simulate growth and metabolic secretion profiles for each model.
- Screen for strains with a high production potential for beneficial postbiotics (e.g., short-chain fatty acids) and a low potential for detrimental metabolites [40].
- Evaluate Microbial Interactions:
- Perform pairwise in silico growth simulations between candidate strains and representative resident or pathogenic microbes.
- Identify candidates that exhibit antagonism against specific pathogens (e.g., Escherichia coli) or synergistic relationships with beneficial commensals [40].
- Generate Candidate Shortlist: Rank strains based on a combined score of production potential and beneficial interaction profile. The output is a prioritized list for in vitro and in vivo testing.
The following diagram illustrates the logical workflow and decision points in this screening protocol.
Protocol: Assessing LBP Efficacy via the Microbiota-Gut-Brain Axis
Application Note: This protocol outlines a mechanistic in vivo workflow to evaluate the efficacy of an LBP for neurodegenerative diseases, using the microbiota-gut-brain axis as a framework [11]. It focuses on measuring glial cell responses and key metabolites.
Procedure:
- Animal Model and LBP Administration:
- Use a relevant transgenic or chemically-induced mouse model of neurodegeneration (e.g., 5xFAD for Alzheimer's disease) [11].
- Randomize animals into LBP treatment and control groups. Administer the LBP (e.g., a defined bacterial consortium) via oral gavage over a predefined treatment period.
- Behavioral and Cognitive Testing: Conduct behavioral assays relevant to the disease model (e.g., maze tests for memory and learning) at baseline and post-treatment [11].
- Sample Collection and Tissue Processing:
- Collect fresh fecal samples for microbiome (16S rRNA sequencing) and metabolome (LC-MS) analysis.
- Following perfusion, dissect and harvest brain regions of interest (e.g., hippocampus, cortex). Process tissue for immunohistochemistry, flow cytometry, or RNA sequencing.
- Immunohistochemical Analysis of Glial Cells:
- Stain brain sections with antibodies against Iba1 (for microglia) and GFAP (for astrocytes).
- Quantify glial activation states based on morphological changes: ramified (resting) vs. amoeboid (activated) microglia, and hypertrophy of astrocytes [11].
- Metabolomic and Immunological Profiling:
- Quantify levels of gut microbiota-derived metabolites (e.g., short-chain fatty acids, bile acids) in serum and brain tissue using targeted mass spectrometry [11].
- Measure plasma levels of inflammatory cytokines (e.g., IL-1β, TNF-α) and gut hormones (e.g., GLP-1) via multiplex immunoassays.
- Correlative Data Integration: Statistically correlate changes in the gut microbiome composition, key metabolite levels, glial activation status, and cognitive performance scores to infer mechanism of action.
The diagram below maps the key pathways of the microbiota-gut-brain axis that this protocol investigates.
The Scientist's Toolkit: Essential Reagents and Solutions
Successful LBP development relies on specialized reagents and tools to address unique challenges in manufacturing and analysis.
Table 3: Essential Research Reagents and Solutions for LBP Development
| Research Reagent / Solution | Function / Application in LBP Development |
|---|---|
| Chemically Defined Media | Supports consistent, scalable GMP fermentation; requires optimization to eliminate undefined/animal-derived components for robust anaerobic growth [40] [42]. |
| Cryoprotectants & Lyophilization Formulations | Protects strain viability during freeze-drying and long-term storage; formulation is highly strain-specific and requires parameter optimization [42]. |
| Anaerobic Chamber & GMP Fermenters | Essential for cultivating oxygen-sensitive, obligate anaerobes; specialized equipment maintains strict anaerobic conditions from culture to final product fill [43]. |
| Strain-Specific Phenotypic Assays | Functional tests (e.g., bile acid conversion, bacteriocin production) to confirm strain-level potency and mechanism of action beyond genetic identification [42]. |
| GMP-Grade Caspules with Oxygen Barrier | Protects viability of lyophilized live products for oral delivery; requires low moisture content and excellent oxygen barrier properties [43]. |
| Pan-Microbiome Profiling Tools (16S rRNA, Shotgun Metagenomics) | For assessing in vivo engraftment, batch-to-batch quality control, and patient stratification based on baseline microbiome composition [39]. |
| Pathogen Screening Assays | Comprehensive, multi-target PCR and NGS-based tests for donor and product safety screening to exclude known pathogens and virulence factors [42]. |
| Immunomodulation Readout Systems | In vitro cell-based assays (e.g., PBMC or dendritic cell co-culture) to quantify strain-specific immunomodulatory effects (e.g., Treg induction) [42]. |
The LBP pipeline, now exceeding 180 drugs in development, represents a fundamental expansion of the pharmaceutical landscape. The transition from whole-community products to rationally designed, defined-strain consortia and engineered microbes underscores a maturation of the field. Success in this complex modality hinges on the integrated application of robust experimental protocols—from in silico strain selection using GEMs to mechanistic efficacy studies via the gut-brain axis—along with a deep understanding of the associated manufacturing and regulatory challenges. As the pipeline continues to evolve, these detailed application notes and protocols provide a critical foundation for researchers and drug development professionals aiming to translate microbiome science into novel therapeutics.
The translation of microbiome-based therapies from bench to bedside is accelerating, with all three modalities showing promising results in clinical and preclinical settings for a range of conditions. The tables below summarize key quantitative findings and developmental status.
Table 1: Clinical and Preclinical Outcomes of Novel Therapeutic Modalities
| Therapeutic Modality | Target Condition / Model | Key Efficacy Findings | Reference / Trial Stage |
|---|---|---|---|
| Personalized Inhaled Phage Therapy | Cystic Fibrosis (CF) with MDR/PDR Pseudomonas aeruginosa [44] | - Sputum P. aeruginosa decreased by a median of 104 CFU mL-1 post-therapy [44]- Mean improvement of 8% in ppFEV1 (lung function) [44] | Nature Medicine 2025; Compassionate Use [44] |
| Engineered E. coli Nissle 1917 | Phenylketonuria (PKU) [45] | Engineered to produce PAL and LAAD enzymes for degradation of excess phenylalanine in the gut [45] | Preclinical / Engineering Validation [45] |
| Engineered Lactococcus lactis | Inflammatory Bowel Disease (IBD) - Colitis Model [45] | Secretion of human interleukin-10 leading to successful alleviation of colitis in murine models [45] | Preclinical (Murine Model) [45] |
| Defined Bacterial Consortium | Necrotizing Enterocolitis (NEC) in Preterm Infants [46] | 27% reduction in all-cause mortality in a phase 3 trial of 2,158 premature infants [47] | Phase 3 Clinical Trial (IBP-9414) [47] |
| Phage-Antibiotic Synergy (PAS) | Diverse Infections (Pulmonary, Soft Tissue, etc.) [48] | Combination therapy showed ~70% superior eradication rates compared to phage monotherapy [48] | Multicenter Cohort Study [48] |
Table 2: Market Analysis and Developmental Status of Microbiome Therapeutics
| Parameter | Phage Therapy | Engineered Strains | Defined Consortia |
|---|---|---|---|
| Market Valuation & Growth (2025) | $38 million; 17.6% CAGR projected [49] | N/A (Primarily preclinical/early clinical) | N/A (Varies by product and stage) |
| Key Developmental Challenges | Regulatory pathways, host immune responses, bacterial resistance [48] [50] | Genetic stability, biocontainment, regulatory hurdles [51] [52] | Consistent manufacturing, safety in vulnerable populations [46] |
| Notable Companies / Entities | Adaptive Phage Therapeutics, Intralytix [49] | Eligo Bioscience (CRISPR-based editing) [47] | BiomeBank, MaaT Pharma, Infant Bacterial Therapeutics [47] |
| Representative Clinical Focus | MDR respiratory, GI, and wound infections [48] [44] | IBD, metabolic disorders, in-situ drug production [51] [45] | Recurrent C. difficile, IBD, GvHD, NEC [47] |
Experimental Protocols
Protocol 1: Personalized Phage Therapy for Multidrug-Resistant Respiratory Infections
This protocol details the methodology for the compassionate-use, nebulized phage therapy study that successfully treated cystic fibrosis patients with MDR P. aeruginosa [44].
Key Research Reagent Solutions
Table 3: Essential Reagents for Personalized Phage Therapy
| Research Reagent / Material | Function / Explanation |
|---|---|
| Lytic Phage Library | A pre-characterized collection of naturally occurring lytic phages targeting various bacterial receptors (e.g., efflux pumps, LPS, pili) [44]. |
| Bacterial Isolates (Patient Sputum) | The target MDR pathogen isolated from the patient for in vitro phage susceptibility testing [44]. |
| Plaque Assay Materials | A double-layer agar technique used to quantify phage concentration (PFU mL-1) and confirm bacterial lysis [48]. |
| Jet Nebulizer | A device used to generate an aerosol of the phage preparation for inhalation, ensuring delivery to the lower respiratory tract [44]. |
Step-by-Step Methodology
- Patient Strain Isolation and Phenotyping: Spontaneously expectorated sputum is collected from the patient. The target MDR pathogen (e.g., P. aeruginosa) is isolated and identified using standard microbiological culture techniques and antibiotic susceptibility profiling [44].
- Phage Susceptibility Testing (Plaque Assay): The isolated bacterial strain is tested against a library of characterized lytic phages using a dual-layer plaque assay. Phages that produce clear lytic zones (plaques) are selected as candidates [48] [44].
- Phage Cocktail Formulation: A personalized cocktail is formulated based on susceptibility results. Phages are chosen not only for their lytic activity but also for their ability to bind to specific bacterial receptors (e.g., efflux pumps, LPS) where resistance mutations may cause evolutionary trade-offs, such as resensitization to antibiotics or reduced virulence [44].
- Phage Preparation and Administration: Selected phages are amplified, purified, and prepared in a sterile, pyrogen-free buffer. A total dose of 1 × 1010 Plaque-Forming Units (PFU) is administered via a jet nebulizer twice daily (inpatients) or daily (outpatients) for 7-10 days [44].
- Efficacy Monitoring: Sputum bacterial density (CFU mL-1) and lung function (percent predicted FEV1) are measured before and after the treatment course to assess microbiological and clinical outcomes [44].
Figure 1: Personalized Phage Therapy Workflow
Protocol 2: Engineering a Probiotic Chassis for Targeted Metabolite Degradation
This protocol outlines the synthetic biology approach to engineer probiotic bacteria, using E. coli Nissle 1917 (EcN) as a chassis, for therapeutic functions such as metabolite degradation [45].
Key Research Reagent Solutions
Table 4: Essential Reagents for Probiotic Engineering
| Research Reagent / Material | Function / Explanation |
|---|---|
| CRISPR-Cas System | A genome-editing tool (e.g., Cas9, Cas12a) used for precise gene knock-outs (e.g., wecB, endA) or knock-ins in the bacterial chassis [45]. |
| Stable Plasmid Vectors / Expression Cassettes | Genetic constructs carrying the therapeutic genes (e.g., lgtA, PAL, LAAD) along with promoters optimized for gut anaerobes [45]. |
| Anaerobic Chamber | An oxygen-free workstation essential for cultivating and manipulating obligate or facultative anaerobic gut commensals [45]. |
| Model Host Organism | An animal model (e.g., murine) used for in vivo testing of the engineered strain's colonization, safety, and therapeutic efficacy [45]. |
Step-by-Step Methodology
- Therapeutic Circuit Design: Identify the desired function (e.g., degradation of phenylalanine for PKU). Select appropriate therapeutic genes (e.g., phenylalanine ammonia-lyase, PAL) and design genetic circuits with suitable promoters and secretion signals for function in the gut environment [45].
- Chassis Selection and Preparation: Select a well-characterized probiotic chassis like E. coli Nissle 1917 (EcN). Prepare the chassis by using CRISPR-Cas to knockout genes that may compete with the new pathway (e.g., wecB to alter UDP-GlcNAc flux) or to improve genetic stability (e.g., endA inactivation to boost transformation efficiency) [45].
- Vector Construction and Transformation: Clone the therapeutic genetic circuit into a stable, gut-adapted plasmid vector. Transform the constructed vector into the prepared probiotic chassis via electroporation or other methods [45].
- In Vitro Functional Validation: Cultivate the engineered strain and validate therapeutic protein expression and function in vitro. For example, measure the degradation of the target metabolite (e.g., phenylalanine) in culture supernatants using HPLC or other analytical methods [45].
- In Vivo Efficacy and Safety Testing: Administer the validated engineered strain to a disease model organism (e.g., a PKU mouse model) orally. Monitor the reduction of systemic metabolite levels, assess gut colonization, and evaluate any potential adverse effects or immune responses [45].
Figure 2: Probiotic Engineering Workflow
Mechanistic Insights and Signaling Pathways
Phage-Antibiotic Synergy (PAS) and Evolutionary Trade-offs
The efficacy of phage therapy is not limited to direct bacterial lysis. A key advanced concept is Phage-Antibiotic Synergy (PAS), where sub-inhibitory concentrations of certain antibiotics can enhance phage replication and bacterial killing [48]. Furthermore, a sophisticated strategy involves selecting phages that exploit bacterial receptors critical for both phage entry and pathogenicity.
For instance, phage OMKO1 uses the multidrug efflux pump system (e.g., MexXY) of P. aeruginosa as its receptor [44]. When the bacterium evolves resistance by mutating or downregulating this pump to prevent phage adsorption, it concurrently becomes more susceptible to antibiotics that the pump would normally efflux (e.g., ceftazidime, ciprofloxacin) [48] [44]. This creates a therapeutic "trade-off," where phage pressure selects for less antibiotic-resistant bacterial populations.
Figure 3: Phage-Driven Evolutionary Trade-off
Engineered Bacterial Sensing and Response Circuitry
Engineered strains can be designed as "smart" living therapeutics using synthetic gene circuits that enable them to sense pathological signals and respond with a therapeutic action in a closed-loop system [51].
A foundational workflow for such a circuit, applicable to conditions like Inflammatory Bowel Disease (IBD), involves:
- Sensing: The engineered bacterium is programmed to detect a disease-specific biomarker, such as the inflammatory cytokine TNF-α or tetrathionate, which is produced during gut inflammation [51].
- Signal Processing: An intracellular genetic logic gate (e.g., an AND gate) processes this sensory input. The circuit is activated only when the specific biomarker is present above a certain threshold [51].
- Therapeutic Output: Upon activation, the circuit triggers the expression and secretion of a therapeutic molecule, such as the anti-inflammatory cytokine IL-10 or an enzyme that produces the protective metabolite butyrate [51] [45]. This localized, on-demand delivery system minimizes off-target effects.
Figure 4: Engineered Bacteria Logic Circuit
The human microbiome, the complex ecosystem of microorganisms inhabiting our bodies, has emerged as a critical determinant of health and disease. Once regarded as a passive passenger, it is now recognized as a dynamic interface that actively shapes host physiology, immunity, metabolism, and therapeutic responsiveness [53]. The field of metagenomics, which examines all genetic material recovered directly from environmental or living samples, has matured alongside next-generation sequencing technologies, enabling comprehensive characterization of microbial communities without the need for cultivation [54]. This technological revolution has facilitated the discovery of microbial biomarkers—specific taxonomic compositions, functional genes, or metabolic products—associated with disease susceptibility, progression, and treatment outcomes.
Microbiome-based diagnostics represent a paradigm shift in clinical medicine, moving beyond classic models of single-pathogen causation to understanding how microbial community imbalances influence diverse conditions including obesity, diabetes, cardiovascular disease, oncogenesis, cancer therapy response, and neurodegenerative conditions [54]. The clinical translation of this knowledge is spearheaded by Food and Drug Administration (FDA)-approved microbiome therapies for recurrent Clostridioides difficile infections and emerging diagnostic platforms that leverage microbial signatures for disease risk stratification [17]. These developments highlight the transformative potential of microbiome analysis in precision medicine, where microbial biomarkers can inform personalized therapeutic strategies and preventive healthcare interventions.
However, the field faces significant challenges in standardization, validation, and clinical implementation. Microbiome studies produce vast amounts of data that necessitate sophisticated computational tools, and the technologies utilized are rapidly evolving [54]. Moreover, many mathematical tools available provide assessments of association rather than causation, requiring complementary experimental validation. This application note provides a comprehensive framework for developing robust microbiome-based diagnostics, encompassing methodological considerations, analytical workflows, and clinical validation strategies to advance their translation into routine clinical practice.
Analytical Frameworks and Methodologies
Sequencing Technologies and Platforms
Microbiome analysis employs two primary sequencing approaches: targeted marker gene analysis and whole-genome shotgun metagenomics. Each method offers distinct advantages and limitations for diagnostic applications, with selection dependent on research questions, sample types, and computational resources.
Marker gene analysis, particularly 16S ribosomal RNA (rRNA) gene sequencing for bacteria and internal transcribed spacer (ITS) region sequencing for fungi, provides a cost-effective method for taxonomic profiling of microbial communities [54]. These highly conserved genes contain hypervariable regions that serve as unique barcodes for taxonomic assignment. Current 16S and ITS sequencing primarily utilizes the Illumina MiSeq platform, frequently leveraging the 2×300 sequencing length to cover multiple variable regions [54]. Emerging approaches employ PacBio or Oxford Nanopore technologies for full-length 16S and ITS sequencing, though reference databases for these longer reads currently lag behind technological capabilities.
A significant challenge in marker gene analysis is defining biologically relevant sequence units. The field has adopted operational taxonomic units (OTUs), which bin sequences using arbitrary divergence thresholds (typically 97% or 99%) that may not align with biologically relevant cutoffs [54]. Taxonomy is assigned via machine learning methods such as the RDP classifier or mapping to reference databases like Greengenes and SILVA [54]. Standard analysis packages including Mothur, QIIME, and DADA2 provide integrated workflows for sequence processing, OTU clustering, and taxonomic assignment [54].
Shotgun metagenomics approaches utilize untargeted sequencing to capture all microbial genomes present within a sample, enabling simultaneous analysis of bacteria, fungi, DNA viruses, and other microbes [54]. This comprehensive genetic capture permits both taxonomic profiling and functional potential assessment through gene coding sequence identification [54]. Shotgun methods primarily rely on Illumina sequencing platforms (HiSeq or NovaSeq families) due to high throughput and low cost per base, though PacBio and Oxford Nanopore technologies are gaining traction for their longer read lengths that aid gene calling and genetic mapping [54].
Metagenomic assembly presents substantial computational challenges, with no current consensus regarding optimal methods. Approaches include de novo assembly using de Bruijn graph methods (e.g., MetaVelvet, IDBA-UD, metaSPAdes, MEGAHIT), reference-guided assembly (e.g., MetaCompass), and read-based profiling using tools like Kraken (utilizing k-mer distributions) or MetaPhlAn2 (using clade-specific marker genes) for taxonomic assignment [54]. Each method presents trade-offs between computational demands, reference dependence, and resolution.
Table 1: Comparison of Microbiome Sequencing Approaches
| Feature | 16S/ITS Amplicon Sequencing | Shotgun Metagenomics |
|---|---|---|
| Target Region | Specific marker genes (16S rRNA, ITS) | All microbial DNA |
| Sequencing Depth | 10,000-100,000 reads/sample | 10-50 million reads/sample |
| Taxonomic Resolution | Genus to species level | Species to strain level |
| Functional Information | Limited (inferred) | Comprehensive (direct) |
| Cost per Sample | $50-$200 | $100-$500 |
| Computational Requirements | Moderate | High |
| Reference Database Dependence | High for taxonomy | High for both taxonomy and function |
| Primary Applications | Taxonomic profiling, diversity studies | Pathway analysis, gene content, strain tracking |
Beyond Genomics: Multi-Omic Integration
Comprehensive microbiome analysis increasingly integrates multiple analytical layers—genomic, transcriptomic, proteomic, and metabolomic—to capture functional activities and host-microbe interactions that genomic composition alone cannot reveal.
Metatranscriptomics captures RNA transcribed from microbial cells, enabling assessment of microbial community transcriptional activities [54]. Standard workflows involve total RNA isolation from microbiome samples, RNA enrichment, fragmentation, cDNA synthesis, and preparation of transcriptome libraries for sequencing [54]. RNA sequence reads are mapped to genomes and metabolic pathways (e.g., KEGG) to identify taxonomically assigned transcriptionally active organisms and their expressed gene functions [54]. Bioinformatics tools like SOAPdenovo-Trans are used for alignment and assembly of metatranscriptomic data, with comparisons between experimental groups to identify differentially regulated pathways across health and disease states [54].
Metaproteomics focuses on identifying and quantifying proteins present within a microbiome, providing direct evidence of functional molecular mechanisms [54]. This approach typically utilizes mass spectrometry to characterize protein expression patterns, microbial community structure, and host response proteins [54]. Similarly, metabolomics profiles the metabolites microbiota produce and how these molecular products interact with both microbial and host metabolic pathways [54]. Metabolomic analyses also employ mass spectrometry to identify known metabolites, including antibiotics, antibiotic biproducts, and host-bacterial metabolic intermediates [54].
Integration of these multi-omic datasets provides a systems-level understanding of microbiome function, moving beyond correlation to mechanistic insights. However, this integration presents substantial computational and statistical challenges, requiring specialized bioinformatics pipelines and appropriate multiple testing corrections to avoid false discoveries.
Quantitative Microbial Measurement Framework
Absolute vs. Relative Abundance Analysis
A critical advancement in microbiome diagnostics is the shift from relative to absolute abundance measurements. Standard 16S rRNA gene amplicon sequencing and shotgun metagenomics typically yield relative abundance data, where the proportion of each taxon depends on the abundance of all other taxa in the community [55]. This compositional nature introduces interpretation challenges, as an increase in one taxon's relative abundance could result from its actual expansion or the reduction of other community members [55].
Absolute quantification methods overcome these limitations by measuring the actual abundance of microbial taxa, enabling accurate assessment of direction and magnitude of changes between experimental conditions [55]. These approaches use "anchor" points to convert relative data to absolute values, including spiked standards (exogenous DNA of known concentration), flow cytometry (total cell counts), total DNA quantification, or quantitative PCR (qPCR) [55]. Each method presents distinct advantages and limitations regarding required sample input, compatibility with different sample types, and susceptibility to amplification biases.
Digital PCR (dPCR) has emerged as a particularly robust anchoring method due to its precision in nucleic acid quantification without requirement for standard curves [55]. By dividing a PCR reaction into thousands of nanoliter droplets and counting positive amplifications, dPCR provides absolute quantification of target genes, enabling conversion of relative sequencing data to absolute taxon abundances [55]. This approach has demonstrated approximately 2x accuracy in DNA extraction across diverse tissue types when total 16S rRNA gene input exceeds 8.3×10^4 copies, with lower limits of quantification of 4.2×10^5 16S rRNA gene copies per gram for stool/cecum contents and 1×10^7 copies per gram for mucosa [55].
Table 2: Absolute Quantification Methods in Microbiome Analysis
| Method | Principle | Lower Limit of Quantification | Compatible Samples | Key Limitations |
|---|---|---|---|---|
| Digital PCR (dPCR) | Partitions PCR reaction to count single molecules | 4.2×10^5 copies/gram (stool); 1×10^7 copies/gram (mucosa) | Stool, mucosa, lumenal contents | Requires optimization of extraction efficiency |
| Spike-in Standards | Adds known quantity of exogenous DNA | Depends on spike-in concentration and sample biomass | Stool, saliva, other high-biomass samples | Potential amplification bias between spike-in and native DNA |
| Flow Cytometry | Direct cell counting | ~10^4 cells/gram | Liquid samples, dissociable solids | Requires single-cell dissociation; difficult for complex matrices |
| qPCR with Standard Curve | Quantification against DNA standards | ~10^3 gene copies/gram | Most sample types | Standard curve inaccuracies; amplification efficiency variations |
| Total DNA Quantification | Measures total DNA as reference | Varies by sample type | Samples with minimal host DNA (e.g., stool) | Inappropriate for host-contaminated samples (e.g., mucosa) |
Quantitative Sequencing Protocol
The following protocol details a rigorous framework for absolute quantification of mucosal and lumenal microbial communities using dPCR anchoring, adapted from a validated methodology [55]:
Sample Preparation and DNA Extraction:
- Sample Collection: Collect luminal contents and mucosal tissues from gastrointestinal sites of interest. For mucosal samples, gently wash with sterile PBS to remove non-adherent bacteria.
- Sample Homogenization: Homogenize samples in appropriate lysis buffer using bead-beating with 0.1mm glass beads for 5 minutes at maximum speed to ensure complete cell disruption.
- DNA Extraction: Perform column-based DNA extraction using a maximum of 200mg stool/cecal content or 8mg mucosal tissue to prevent column saturation. Include extraction controls without sample to monitor contamination.
- DNA Quantification: Measure DNA concentration using fluorometric methods (e.g., Qubit dsDNA HS Assay) to assess total nucleic acid yield.
Extraction Efficiency Validation:
- Spike-in Community: Prepare a defined 8-member microbial community with known concentrations (1.4×10^9 to 1.4×10^5 CFU/mL) in germ-free mouse GI samples.
- Efficiency Calculation: Extract DNA from spiked samples and quantify recovery via dPCR targeting 16S rRNA genes. Calculate extraction efficiency as (measured copies/expected copies) × 100%.
- Acceptance Criterion: Maintain extraction efficiency between 80-120% across the quantification range.
Digital PCR Quantification:
- Reaction Setup: Prepare dPCR reactions with 16S rRNA gene primers (e.g., 515F/806R) and sample DNA. Partition reactions using a microfluidic dPCR system.
- Amplification: Run amplification with the following protocol: 95°C for 10 min (enzyme activation), 40 cycles of 95°C for 15 sec (denaturation) and 60°C for 60 sec (annealing/extension).
- Absolute Quantification: Calculate total 16S rRNA gene copies/μL directly from the fraction of positive partitions using Poisson statistics.
Library Preparation and Sequencing:
- Amplicon PCR: Amplify V4 region of 16S rRNA gene using dual-indexed primers with Illumina adapters. Monitor reactions with real-time qPCR and stop in late exponential phase (typically 20-25 cycles) to limit chimera formation.
- Library Purification: Clean amplified libraries with solid-phase reversible immobilization (SPRI) beads.
- Quality Control: Assess library quality using bioanalyzer or tape station and quantify by fluorometry.
- Sequencing: Pool libraries at equimolar concentrations and sequence on Illumina MiSeq (2×250 bp) or NovaSeq (2×150 bp) platform.
Data Analysis:
- Sequence Processing: Process raw sequences using DADA2 to infer amplicon sequence variants (ASVs) instead of OTUs for higher resolution.
- Absolute Abundance Calculation: Convert relative ASV abundances to absolute counts using the formula: Absolute abundance (copies/gram) = (ASV relative abundance × total 16S rRNA gene copies from dPCR) / sample weight.
- Statistical Analysis: Perform differential abundance testing using methods appropriate for absolute count data (e.g., DESeq2, negative binomial models).
Experimental Design and Workflow Visualization
Diagnostic Biomarker Development Workflow
The development of robust microbiome-based diagnostics requires a systematic approach from study design through clinical validation. The following diagram illustrates the complete workflow for diagnostic biomarker development:
Diagram 1: Microbiome Diagnostic Development Workflow
Multi-omic Integration Framework
Advanced microbiome diagnostics increasingly integrate multiple data layers to capture comprehensive biological insights. The following diagram illustrates the multi-omic integration framework for biomarker discovery:
Diagram 2: Multi-omic Integration Framework
Essential Research Reagents and Materials
Successful implementation of microbiome-based diagnostics requires carefully selected reagents and materials validated for specific sample types and analytical approaches. The following table details essential research reagent solutions for microbiome studies:
Table 3: Research Reagent Solutions for Microbiome Diagnostics
| Category | Specific Product/Kit | Application | Key Considerations |
|---|---|---|---|
| Sample Collection & Storage | OMNIgene•GUT, DNA/RNA Shield, PAXgene | Fecal sample stabilization | Stability at room temperature; compatibility with downstream analyses |
| DNA Extraction | QIAamp PowerFecal Pro, DNeasy PowerLyzer, MoBio Powersoil | Microbial DNA isolation | Efficiency for Gram-positive/Gram-negative; inhibitor removal; yield consistency |
| DNA Quantification | Qubit dsDNA HS Assay, PicoGreen | Nucleic acid measurement | Specificity for double-stranded DNA; detection limit; sample volume requirements |
| 16S rRNA Amplification | Earth Microbiome Project primers (515F/806R), Platinum Taq | Amplicon generation | Coverage breadth; amplification bias; chimera formation rates |
| Shotgun Library Prep | Nextera XT, KAPA HyperPlus | Whole metagenome sequencing | Insert size distribution; GC bias; duplicate rates |
| Spike-in Controls | ZymoBIOMICS Spike-in Control, External RNA Controls Consortium (ERCC) | Quantification normalization | Phylogenetic distance from sample; extraction efficiency; amplification efficiency |
| qPCR/dPCR Reagents | TaqMan Microbial Assays, EvaGreen, Bio-Rad ddPCR Supermix | Absolute quantification | Specificity; dynamic range; multiplexing capability |
| Standards & Controls | ZymoBIOMICS Microbial Community Standard, ATCC Mock Microbial Communities | Method validation | Community complexity; evenness; reference genome availability |
Additional specialized reagents may be required for specific applications, including:
- Metatranscriptomics: RNase inhibitors, ribosomal RNA depletion kits (MICROBEnrich, RiboZero)
- Metaproteomics: Protease inhibitors, protein extraction reagents (SDS, urea), trypsin/Lys-C for digestion
- Metabolomics: Methanol/acetonitrile for metabolite extraction, derivatization reagents (e.g., MSTFA for GC-MS)
- Culture-based Validation: Anaerobic culture systems, specific growth media for fastidious organisms
Standards and Reporting Guidelines
Robust reporting of microbiome studies is essential for reproducibility, comparative analysis, and clinical translation. The STORMS (Strengthening The Organization and Reporting of Microbiome Studies) checklist provides comprehensive guidance for reporting human microbiome research [7]. This 17-item checklist is organized into six sections corresponding to typical scientific publication sections and includes both elements adapted from existing observational and genetic epidemiology guidelines (STROBE and STREGA) and new elements specific to microbiome studies [7].
Key reporting considerations for microbiome-based diagnostics include:
Study Population and Design:
- Clearly describe inclusion/exclusion criteria, particularly regarding antibiotics, probiotics, or other interventions that might affect microbiome composition [7]
- Report temporal context including recruitment dates, follow-up duration, and data collection periods [7]
- Document participant characteristics including environment, lifestyle, diet, biomedical interventions, demographics, and geography [7]
Laboratory Methods:
- Specify sample collection, handling, and storage conditions [7]
- Detail DNA extraction method and any modifications to manufacturer protocols
- Report sequencing platform, region targeted (for amplicon sequencing), and sequencing depth [54]
- Describe quality control measures including extraction controls, PCR negatives, and positive controls
Bioinformatic Processing:
- Specify software and parameters for quality filtering, OTU/ASV picking, and taxonomy assignment [54]
- Report database and version used for taxonomic assignment (e.g., SILVA, Greengenes) [54]
- For shotgun metagenomics, describe assembly methods, gene calling, and functional annotation pipelines [54]
Statistical Analysis:
- Describe normalization methods and approaches for handling compositional data [7]
- Report diversity metrics (alpha and beta diversity measures) and statistical methods for group comparisons [54]
- Detail multiple testing correction procedures for high-dimensional data
- For predictive models, report performance metrics (AUC, sensitivity, specificity) and validation approach
Adherence to these reporting standards facilitates manuscript preparation, peer review, reader comprehension, and comparative analysis of published results, ultimately accelerating the translation of microbiome research into clinical diagnostics [7].
Microbiome-based diagnostics represent a transformative approach to disease risk assessment and treatment response prediction. The field has progressed from descriptive associations to mechanistic insights enabled by multi-omic technologies, quantitative measurement frameworks, and advanced computational methods. However, successful clinical translation requires rigorous standardization, validation in diverse populations, and integration with host factors.
Future advancements will likely include:
- Development of standardized reference materials for method calibration
- Integration of host genetic, immunological, and clinical data with microbial biomarkers
- Point-of-care sequencing technologies for rapid diagnostic applications
- Machine learning approaches for multi-omic data integration and predictive modeling
- Expansion to understudied body sites and populations to improve health equity
As these developments unfold, microbiome-based diagnostics will increasingly inform personalized therapeutic strategies, enabling a new era of precision medicine that leverages our microbial counterparts for improved human health.
Precision nutrition represents a transformative approach that moves beyond universal dietary guidelines to provide individualized nutritional strategies based on a person's genetic makeup, metabolic profile, lifestyle, and gut microbiome composition [56]. The gut microbiome, a highly complex and individualized community of microorganisms in the gastrointestinal tract, has emerged as a key factor influencing how individuals respond to diet [57]. This interaction creates a dynamic relationship where diet shapes microbial composition, and the microbiome, in turn, modulates the host's metabolic response to dietary intake [58]. Understanding this reciprocity is fundamental to developing effective precision nutrition interventions that target the microbiome for improving human health.
The distinction between the gut microbiome's role as a mediator versus an effect modifier is crucial for research design and interpretation [58]. As a mediator, diet directly alters gut microbiota composition or function (post-intervention microbiome), which then influences host metabolism. As an effect modifier, the baseline state of the microbiome determines the metabolic response to a dietary intervention. This distinction helps avoid circular logic when investigating the relationship between diet, microbiome, and health outcomes. Most therapeutic applications focus on the microbiome's role as a modifier that can be targeted to steer individual responses to diet [58] [59].
Key Mechanistic Pathways for Dietary Intervention
Dietary components influence host physiology through multiple microbiome-dependent pathways. The primary mechanisms include modulation of energy harvest, production of microbial metabolites, and regulation of inflammatory pathways. Understanding these mechanisms is essential for designing targeted interventions.
Table 1: Key Microbiome-Dependent Pathways in Precision Nutrition
| Pathway | Key Actors | Physiological Impact | Dietary Modulators |
|---|---|---|---|
| Energy Harvest | Firmicutes, Bacteroidetes [59] | Modulates caloric extraction from indigestible carbohydrates [57] | Dietary fiber, resistant starch [59] |
| SCFA Production | Faecalibacterium prausnitzii, Roseburia spp. [59] | Energy supply, appetite regulation, anti-inflammatory effects, gut barrier integrity [59] | Prebiotics (e.g., inulin, FOS), fiber-rich foods [59] [60] |
| Bile Acid Metabolism | Bile salt hydrolases (BSH) from gut bacteria [59] | Alters host lipid metabolism, glucose regulation, and FXR/TGR5 signaling [59] | Dietary fats, fiber |
| Bioactive Metabolite Production | Tryptophan-metabolizing bacteria [61] | Production of neuroactive (e.g., IPA) and immunomodulatory compounds [61] [60] | Tryptophan-rich proteins, polyphenols [61] |
The following diagram illustrates the core conceptual relationship between diet, the gut microbiome, and host metabolism, which forms the basis for precision nutrition interventions.
Application Notes: Experimental Framework and Data
Translating microbiome science into actionable precision nutrition requires a structured experimental framework. This involves specific study designs, response criteria, and advanced analytical methods to account for high inter-individual variability.
Table 2: Summary of Experimental Designs in Microbiome-Focused Precision Nutrition Studies
| Dietary Intervention | Study Model | Design | Primary Response Criteria | Key Findings |
|---|---|---|---|---|
| High-Fiber Diets [58] | Humans (obese/metabolic syndrome) | Randomized Controlled | >10% change in cholesterol, HOMA [58] | Microbiome stability correlates with clinical response [58] |
| Barley Kernel Bread [58] | Humans (healthy) & Gnotobiotic Mice | Randomized Cross-over | ≥25% decrease in glucose iAUC [58] | Baseline P/B ratio predicted glycemic improvement [58] |
| WTP Diet (High-Fiber) [58] | Humans (T2D) | Randomized Parallel | Decrease in HbA1c [58] | High-fiber diet promoted beneficial SCFAs and glycemic control [58] |
| Bifidobacterium longum APC1472 [60] | Humans (overweight/obesity) | Supplementation | Body weight, metabolic markers [60] | Attenuated weight-related parameters and hypothalamic molecular alterations [60] |
| Carrot Rhamnogalacturonan-I (cRG-I) [61] | Human cohort ex vivo (SIFR technology) | Nutrient Challenge | Microbiome metabolite production [61] | Consistently increased microbial production of indole-3-propionic acid (IPA) across all subjects [61] |
Key Considerations for Intervention Design
- Responder Stratification: A critical step is defining responder (R) vs. non-responder (NR) status a priori based on clear, quantifiable metrics. Examples include a ≥25% decrease in glucose incremental Area Under the Curve (iAUC) for glycemic interventions [58], or a >10% change in cholesterol or HOMA-IR for metabolic syndrome studies [58].
- Baseline Microbiome Profiling: The pre-intervention microbial state is a key effect modifier. Features like a high Prevotella-to-Bacteroides (P/B) ratio have been associated with greater improvements in glycemic response to fiber-rich diets and greater production of health-promoting short-chain fatty acids (SCFAs) [58].
- Microbiome Stability: The resilience of an individual's microbiome (measured by similarity indices between baseline and post-intervention samples) can also be a predictor of clinical response, such as changes in cholesterol or insulin sensitivity [58].
Experimental Protocols
Protocol: Microbiome-Mediated Glycemic Response Intervention
This protocol outlines a method to test the efficacy of a fiber-rich dietary intervention, using baseline microbiome features to predict glycemic response.
Objective: To assess the effect of a high-fiber intervention (e.g., barley kernel bread) on postprandial glycemic response and to determine if baseline microbiome composition (e.g., P/B ratio) predicts intervention success [58].
Materials:
- Test diet (e.g., Barley Kernel Bread) and control diet (e.g., White Wheat Bread)
- Continuous glucose monitors or resources for frequent blood sampling
- DNA extraction kit (e.g., DNeasy PowerSoil Kit)
- 16S rRNA or shotgun metagenomic sequencing pipelines
- Bioinformatic software (QIIME 2, MOTHUR, or similar)
Procedure:
- Screening & Baseline Phase (Week 1):
- Recruit eligible subjects (e.g., healthy or prediabetic).
- Collect baseline stool sample for microbiome sequencing.
- Perform an initial standardized meal test to measure baseline glycemic response.
Intervention Phase (Randomized Cross-over, Weeks 2-4):
- Administer test diet and control diet in randomized order. Each intervention period should last a minimum of 3 days, with a washout period in between [58].
- During each period, use continuous glucose monitors to track postprandial glycemic responses to standardized meals.
Sample Collection & Analysis (Ongoing):
- Collect stool samples at the end of each intervention period.
- Extract genomic DNA from stool and perform 16S rRNA gene sequencing (e.g., V4 region) or shotgun metagenomics.
- Process sequencing data: perform quality control, OTU/ASV picking, taxonomic assignment, and diversity analysis.
Data Integration & Responder Analysis:
- Calculate glycemic response (e.g., iAUC) for each subject during test and control periods.
- Classify subjects as Responders (R) if iAUC decreases by ≥25% during the test period compared to control [58].
- Correlate baseline microbial features (e.g., P/B ratio, specific taxa) with responder status using statistical models (e.g., linear regression, machine learning).
The workflow for this protocol is summarized in the following diagram:
Protocol: Ex Vivo Microbiome Metabolite Production Assay
This protocol uses an ex vivo fermentation system to predictably assess the functional response of an individual's microbiome to a specific dietary component prior to in vivo testing.
Objective: To evaluate the ability of a specific dietary component (e.g., a prebiotic fiber like cRG-I) to consistently modulate the production of a health-promoting microbial metabolite (e.g., Indole-3-Propionic Acid (IPA)) across a diverse human cohort [61].
Materials:
- SIFR (Systemic Intestinal Fermentation Research) technology or similar ex vivo fermentation system [61]
- Anaerobic workstation
- Dietary compound of interest (e.g., carrot-derived rhamnogalacturonan-I (cRG-I))
- Fresh stool samples from human donors
- Culture media
- Untargeted metabolomics platform (e.g., LC-MS)
- 16S rRNA amplicon sequencing reagents
Procedure:
- Sample Inoculum Preparation:
- Collect and process fresh fecal samples from multiple healthy donors under anaerobic conditions.
- Prepare a standardized fecal slurry in anaerobic culture medium.
Ex Vivo Fermentation:
- Inoculate the fermentation vessels (e.g., in the SIFR system) with the standardized fecal slurry.
- Add the test dietary compound (e.g., cRG-I at 0.3 g/d and 1.5 g/d equivalent doses) to treatment vessels. Include a control vessel without the supplement.
- Allow fermentation to proceed for a set period (e.g., 24-48 hours) under controlled anaerobic conditions.
Post-Fermentation Analysis:
- Microbiome Analysis: Extract DNA from fermentation contents pre- and post-fermentation. Perform 16S rRNA sequencing to assess changes in microbial composition and diversity.
- Metabolite Analysis: Collect supernatant from fermented material. Analyze using untargeted metabolomics (LC-MS) to quantify the production of target metabolites like IPA and SCFAs.
Data Integration:
- Correlate changes in specific bacterial taxa (e.g., absolute levels of Bifidobacterium longum) with increases in target metabolites (e.g., IPA) [61].
- Use the "community modulation score" to assess the impact of the intervention on microbial diversity while maintaining high alpha-diversity, a factor linked to elevated IPA production [61].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Technologies for Microbiome-Focused Precision Nutrition Research
| Category / Item | Specific Examples | Function & Application |
|---|---|---|
| DNA Sequencing Kits | DNeasy PowerSoil Kit, 16S rRNA Amplification Kits | High-quality microbial DNA extraction and amplification for community profiling [58] |
| 'Biotics' Reagents | Inulin, Fructo-oligosaccharides (FOS), Carrot Rhamnogalacturonan-I (cRG-I), Bifidobacterium longum APC1472 [61] [60] | Prebiotic and probiotic compounds used to test targeted modulation of the gut microbiome [61] [60] |
| Ex Vivo Fermentation Systems | SIFR (Systemic Intestinal Fermentation Research) Technology [61] | Provides a highly controlled, human-relevant environment for screening dietary compounds prior to costly clinical trials [61] |
| Metabolomics Platforms | LC-MS (Liquid Chromatography-Mass Spectrometry) | Quantifies microbial functional output by measuring metabolites like SCFAs and IPA [61] |
| Bioinformatics Suites | QIIME 2, MOTHUR, MetaPhlAn, HUMAnN | Processes and analyzes sequencing data for taxonomic and functional profiling [58] [59] |
| AI/ML Modeling Tools | Random Forest, Support Vector Machines (SVM) | Integrates multi-omics data to predict individual responses to dietary interventions [59] |
Integrated Data Analysis and Translation
The final and most critical phase involves integrating multi-omics data to build predictive models and translating these findings into clinically actionable insights.
Multi-Omics Data Integration: The combination of microbiome data (genomics), host biomarkers (e.g., clinical chemistry, proteomics), and metabolite profiles (metabolomics) is essential for a systems-level understanding [56] [59]. This integration helps elucidate the mechanistic links between dietary intake, microbial shifts, and host physiological outcomes.
Artificial Intelligence and Machine Learning: AI and ML algorithms are increasingly used to handle the complexity and high-dimensionality of multi-omics data. These tools can identify subtle patterns that predict an individual's response to a specific diet, enabling the development of highly personalized nutrition recommendations [59] [62]. For instance, machine learning models can integrate baseline microbiome data, host genetic markers, and dietary intake to forecast postprandial glycemic responses more accurately than traditional methods [56].
The overarching framework from data collection to clinical application is visualized below:
Challenges and Future Directions: Despite promising advances, challenges remain in translating microbiome-based precision nutrition to widespread clinical practice. These include the need for cost-effective and accessible omics technologies, validation of predictive algorithms in large, diverse populations, and the development of standardized protocols for microbiome modulation [59] [63]. Future research must focus on rigorous clinical trials that not only demonstrate efficacy but also cost-effectiveness, particularly for low-income populations [59] [64]. The ultimate goal is to integrate these sophisticated, data-driven approaches into comprehensive weight management and public health paradigms to combat global issues like obesity and related metabolic diseases [57] [59].
Navigating the Translational Gap: Standardization, Trials, and Commercialization
Addressing Interindividual Variability and the Search for Validated Biomarkers
The clinical translation of microbiome research represents a paradigm shift in personalized medicine, offering novel diagnostic and therapeutic avenues for complex diseases. However, this promise is constrained by two fundamental challenges: significant interindividual variability in microbiome composition and function, and the pressing absence of robust, validated biomarkers for predicting disease risk, progression, and therapeutic response [65] [1]. Interindividual variability, driven by factors such as host genetics, diet, geography, and age, complicates the development of universally applicable diagnostic tools and therapeutics [1]. This application note details the core challenges posed by this variability, outlines structured frameworks for biomarker discovery and validation, and provides detailed experimental protocols for developing microbiome-based diagnostics and therapeutics that account for human diversity.
Core Challenges: Quantifying Variability and Biomarker Types
The path to clinical translation requires a clear understanding of the sources of variability and the distinct roles biomarkers can play. The tables below summarize key concepts essential for framing research in this field.
Table 1: Major Sources of Interindividual Variability in Microbiome Studies
| Source of Variability | Impact on Microbiome & Host | Considerations for Study Design |
|---|---|---|
| Host Genetics | Influences immune-microbe interactions and niche availability for specific taxa [1]. | Family/twin studies; GWAS integration with microbiome data. |
| Diet & Nutrition | Rapidly alters microbial community structure and metabolite production (e.g., SCFAs) [65]. | Detailed dietary records; controlled feeding studies. |
| Early-Life Exposures | Delivery mode (vaginal vs. C-section) and feeding (breast vs. formula) seed and shape the nascent microbiome, with long-term health effects [1]. | Longitudinal birth cohorts; analysis of maternal factors. |
| Geography & Environment | Introduces vast differences in microbial exposures, diversity, and functional capacity [1]. | Multi-center, international studies; standardized protocols. |
| Medication History | Antibiotics cause profound, sometimes persistent, disruptions; other drugs (e.g., metformin) also have microbiome effects [1]. | Detailed medication history; prospective monitoring. |
Table 2: Classification and Definitions of Key Biomarker Types
| Biomarker Type | Definition | Role in Microbiome Clinical Translation | Example |
|---|---|---|---|
| Prognostic | Identifies individuals with differing risks of a specific clinical outcome (e.g., disease progression), regardless of therapy [66]. | Stratify patients by disease risk or severity based on baseline microbiome features. | A specific microbial signature predicting progression from prediabetes to type 2 diabetes. |
| Predictive | Identifies individuals likely to respond differentially to a specific therapy or treatment [66]. | Guide the choice of microbiome-targeted or microbiome-interacting therapies. | Gut microbial genes encoding enzymes that metabolize a drug, predicting efficacy or toxicity [66]. |
| Pharmacodynamic | A marker used to demonstrate a biological response to a therapeutic intervention [66]. | Provide proof-of-mechanism for microbiome-targeted interventions in early-phase trials. | Change in levels of a microbial metabolite (e.g., a bile acid) following treatment with a probiotic. |
Experimental Protocols for Biomarker Discovery and Validation
A robust, multi-stage process is required to move from initial discovery to clinically validated biomarkers.
Protocol: Multi-omics Biomarker Discovery Workflow
Objective: To identify candidate microbiome-derived biomarkers associated with a clinical phenotype (e.g., disease state, treatment response).
Materials:
- Research Reagent Solutions: See Table 3 for essential reagents and tools.
- Sample Types: Fecal, mucosal, or other niche-specific samples from deeply phenotyped cohorts.
- Key Equipment: High-throughput sequencer (e.g., Illumina), LC-MS/MS system, high-performance computing cluster.
Table 3: Research Reagent Solutions for Multi-omics Discovery
| Item | Function/Application |
|---|---|
| DNA Extraction Kits (e.g., MoBio PowerSoil) | Standardized microbial genomic DNA isolation for metagenomic sequencing. |
| RNA Stabilization Reagents (e.g., RNAlater) | Preserves microbial transcriptomic profiles immediately upon sample collection. |
| Metabolite Extraction Solvents (e.g., Methanol) | For comprehensive extraction of polar and non-polar metabolites for metabolomics. |
| 16S rRNA Gene Primers (e.g., 515F/806R) | For targeted amplification of bacterial 16S rRNA genes for taxonomic profiling. |
| Shotgun Metagenomic Library Prep Kits | Preparation of sequencing libraries for whole-genome shotgun metagenomics. |
| Bioinformatic Suites (e.g., QIIME 2, HUMAnN 2, MetaPhlAn) | Processing and analysis of raw sequencing data into taxonomic and functional profiles. |
Procedure:
- Cohort Design & Sampling: Employ a prospective, longitudinal study design with nested case-controls. Collect serial samples from a large, diverse cohort to capture variability and temporal dynamics [66].
- Sample Processing: a. Metagenomics: Extract high-quality DNA. For taxonomic and functional profiling, use shotgun sequencing. For cost-effective diversity screening, use 16S rRNA gene amplicon sequencing [65]. b. Metatranscriptomics: Extract total RNA, remove rRNA, and sequence the mRNA-enriched fraction to profile actively expressed microbial genes [65]. c. Metabolomics: Perform untargeted metabolomics on bio-specimens (e.g., serum, feces) using mass spectrometry to quantify microbial and host metabolites [65].
- Data Integration & Analysis: a. Process raw data through established bioinformatic pipelines to generate taxonomic tables, gene abundance profiles, and metabolite abundance matrices. b. Integrate multi-omics datasets using multivariate statistical models (e.g., MOFA) and machine learning algorithms (e.g., random forests) to identify co-varying features that strongly associate with the clinical outcome [65]. c. Validate candidate biomarkers in a held-out test set from the same cohort to assess initial reproducibility.
Diagram 1: Biomarker development and validation workflow.
Protocol: Analytical and Clinical Validation of Candidate Biomarkers
Objective: To establish the analytical robustness and clinical utility of a candidate biomarker signature.
Procedure:
- Assay Development: Translate the multi-omics signature into a targeted, quantitative, and high-throughput assay (e.g., qPCR for specific taxa, targeted MS for metabolites).
- Analytical Validation: Assess the assay's performance characteristics, including:
- Analytical Specificity/Sensitivity: Ensure the assay accurately detects the intended target.
- Precision: Determine intra- and inter-assay coefficient of variation.
- Linearity and Range: Establish the dynamic range of quantification.
- Clinical Validation: Test the validated assay in a large, independent, and prospective validation cohort. The study design must be appropriate for the biomarker's intended use (prognostic or predictive), with randomized controlled trials being the gold standard for predictive biomarkers [66].
- Statistical Analysis: Evaluate the biomarker's clinical performance by calculating metrics such as sensitivity, specificity, positive/negative predictive values, and the C-statistic. Correct for multiple testing to avoid false positives [66].
Computational Modeling to Decode Variability
Computational systems biology approaches are indispensable for moving beyond associations to predictive, mechanistic models that account for variability.
Protocol: Building Predictive Models of Host-Microbiome Interactions
Objective: To create computational models that simulate the impact of interindividual variability on host-microbiome-drug interactions.
Procedure:
- Data Compilation: Integrate patient-specific data layers: microbiome composition (genomics), community metabolic models (from metagenomics), host gene expression (transcriptomics), and clinical metadata.
- Constraint-Based Modeling: Construct Genome-Scale Metabolic Models (GEMs) for prevalent microbial species. Combine them into a community model (e.g., using the MICOM toolkit) to predict the production of key metabolites (e.g., SCFAs, bile acids) for a given individual's microbiome [65].
- Host-Tissue Modeling: Integrate microbial metabolite fluxes with host tissue-specific metabolic models to simulate systemic physiological impacts.
- Machine Learning Integration: Use the outputs of mechanistic models (e.g., predicted metabolite levels) as features in machine learning classifiers (e.g., gradient boosting) to build robust, interpretable predictors of clinical outcomes or therapeutic responses [65].
Diagram 2: Integrating metabolic modeling and machine learning.
Application in Therapeutic Development: Engineered Probiotics
The ultimate test for a validated biomarker is its integration into therapeutic development, enabling patient stratification and personalized treatment.
Case Study: ACE2-Delivering Probiotics for Diabetic Retinopathy
- Therapeutic Rationale: Angiotensin-converting enzyme 2 (ACE2) counteracts retinal inflammation and oxidative stress in Diabetic Retinopathy (DR). Systemic delivery is challenging, but the gut-retina axis offers an alternative route [65].
- Engineering Strategy: Lactobacillus paracasei is engineered as a chassis to express and deliver human ACE2 protein to the gut mucosa [65].
- Addressing Variability & Biomarker Integration:
- Stratification: A predictive biomarker signature (e.g., based on pre-treatment gut microbiome composition and host inflammatory markers) is used to identify patients most likely to respond to the probiotic.
- Dosing Control: Pharmacodynamic biomarkers (e.g., levels of ACE2 product Ang(1-7) in serum) are monitored to guide dosing, as probiotic survival and protein production vary between individuals [65].
- Safety Monitoring: Pre- and post-treatment metagenomic sequencing is used as a safety biomarker to monitor for unintended perturbations to the gut microbial ecosystem [65].
Successfully addressing interindividual variability and establishing validated biomarkers are interdependent challenges at the heart of microbiome clinical translation. A rigorous, multi-stage approach—spanning from deeply phenotyped cohorts and integrated multi-omics to robust computational modeling and biomarker-stratified clinical trials—is essential. By adopting these detailed protocols and frameworks, researchers can advance the development of reliable microbiome-based diagnostics and personalized therapeutics, ultimately fulfilling the promise of precision medicine.
The clinical translation of microbiome research represents a paradigm shift in modern medicine, transforming our understanding of human health and disease etiology. The human microbiome, once regarded as a passive passenger, is now recognized as a dynamic and essential determinant of human physiology, shaping immunity, metabolism, neurodevelopment, and therapeutic responsiveness across the lifespan [1]. Despite rapid advancements, the field faces significant challenges in reproducibility and comparability of findings, largely driven by high interindividual variability and methodological inconsistencies [1] [67]. This application note addresses the imperative for standardized methodologies and international harmonization to accelerate the translation of microbiome research into clinically actionable diagnostics and therapeutics.
The absence of validated microbial biomarkers and incomplete functional annotation of microbial "dark matter" remain substantial barriers to clinical implementation [1]. Here, we outline a systematic framework for understanding the microbiome in human health and disease, from basic principles to clinical translation, with emphasis on standardized protocols that can enhance reproducibility across research settings [67].
Current Landscape of Microbiome Research and Standardization Gaps
Key Challenges in Microbiome Clinical Translation
Table 1: Major Challenges in Microbiome Clinical Translation and Standardization Needs
| Challenge Category | Specific Limitations | Impact on Clinical Translation | Standardization Priority |
|---|---|---|---|
| Methodological Variability | Inconsistent sampling, DNA extraction, sequencing protocols, and bioinformatic analyses | Reduces reproducibility and cross-study comparability | High - Establishment of SOPs across pre-analytical, analytical, and post-analytical phases |
| Biomarker Validation | Lack of validated microbial biomarkers for disease diagnosis and prognosis | Limits development of clinical diagnostics | High - Rigorous analytical and clinical validation frameworks |
| Functional Characterization | Incomplete annotation of microbial genes and pathways (~70% of microbial genes are of unknown function) | Hinders mechanistic understanding and drug target identification | Medium-High - Multi-omics integration and reference database expansion |
| Regulatory Frameworks | Absence of harmonized regulatory pathways for microbiome-based therapeutics | Creates uncertainty in product development and approval | High - International harmonization of regulatory requirements |
| Clinical Trial Design | Heterogeneity in patient stratification, endpoints, and intervention protocols | Complicates evidence generation and meta-analyses | High - Consensus on core outcome sets and trial designs |
International Standardization Initiatives
While the search results do not contain specific details on the STORMS initiative, the documented efforts by large-scale consortia like the Human Microbiome Project (HMP) and Integrative HMP (iHMP) have laid crucial groundwork for standardization in microbiome research [67]. These initiatives have developed standardized protocols for sample collection, processing, and data analysis that enable cross-study comparisons. The European MetaHIT project and American Gut Project have further contributed to establishing reference datasets and methodologies [67]. Recent efforts have focused on broadening representation in microbial reference datasets to advance health equity, recognizing that geographic and demographic diversity is essential for globally applicable diagnostics and therapeutics [1].
Standardized Experimental Workflows for Microbiome Research
Sample Collection and Preservation Standard Operating Procedure (SOP)
Principle: Consistent pre-analytical sample handling is critical for reproducible microbiome data, as variations in collection methods, stabilization, and storage can introduce significant bias [67].
Materials:
- DNA/RNA Shield (Zymo Research) or similar nucleic acid stabilization buffer
- Sterile polypropylene collection tubes (e.g., DNA-free certified)
- Disposable nitrile gloves
- Alphanumeric barcode labels
- -80°C freezer or dry shipper for transport
- Standardized dietary and medication questionnaire
Procedure:
- Pre-collection documentation: Complete standardized questionnaire covering recent (48-hour) dietary intake, medication use (especially antibiotics), and clinical symptoms.
- Sample collection:
- Fecal samples: Collect using standardized collection kit with stabilizer buffer in a 5:1 buffer:sample ratio [67].
- Mucosal samples: For invasive collections (e.g., biopsies), follow institution-approved clinical procedures with simultaneous collection for microbiome analysis and histology.
- Skin/oral samples: Use standardized swabbing technique with pre-moistened swabs and consistent pressure across collections.
- Immediate processing: Mix samples thoroughly with stabilization buffer within 15 minutes of collection.
- Temporary storage: Flash-freeze in liquid nitrogen or place at -20°C for ≤24 hours if -80°C unavailable.
- Long-term storage: Transfer to -80°C within 24 hours with complete chain-of-custody documentation.
- Quality assessment: Perform visual inspection and record any deviations from protocol.
Validation Parameters:
- Sample stability: Demonstrate nucleic acid integrity after 7-day room temperature storage with stabilizer
- Microbial community stability: Compare fresh versus stabilized samples using beta-diversity metrics (Bray-Curtis dissimilarity <0.1)
DNA Extraction and Library Preparation Protocol
Principle: Standardized nucleic acid extraction is essential for minimizing technical variation and enabling meaningful cross-study comparisons [67].
Materials:
- DNeasy PowerSoil Pro Kit (Qiagen) or similar standardized extraction kit
- Qubit dsDNA HS Assay Kit (Thermo Fisher Scientific)
- Agencourt AMPure XP beads (Beckman Coulter)
- Illumina DNA Prep kit with unique dual indexes
- Certified DNA-free consumables
Procedure:
- Cell lysis: Process 200-250 mg of sample using bead-beating homogenization at 4°C for 10 minutes.
- DNA extraction: Follow manufacturer's protocol with these modifications:
- Include extraction controls: positive (ZymoBIOMICS Microbial Community Standard) and negative (water)
- Elute in 50 μL nuclease-free water
- Quality control:
- Quantify DNA using Qubit fluorometer
- Assess purity (A260/A280 ratio: 1.8-2.0)
- Verify integrity by agarose gel electrophoresis
- Library preparation:
- Normalize input DNA to 5 ng/μL
- Amplify V3-V4 region of 16S rRNA gene with primers 341F/806R or perform shotgun library prep
- Clean up with AMPure XP beads (0.8X ratio)
- Library QC:
- Fragment analysis (size distribution: 300-600 bp)
- Quantify by qPCR (Kapa Library Quantification Kit)
- Sequencing: Pool libraries at equimolar concentrations and sequence on Illumina platform (minimum 10,000 reads/sample for 16S; 20 million reads/sample for shotgun)
Validation Parameters:
- Extraction efficiency: >90% recovery from spiked-in control communities
- Inhibition testing: PCR amplification threshold <30 cycles
- Inter-batch CV: <15% for alpha-diversity metrics
Analytical Framework and Bioinformatics Standardization
Bioinformatics Processing Workflow
The transition from raw sequencing data to biologically meaningful insights requires standardized computational pipelines. The diagram below outlines a consensus workflow for microbiome data analysis:
Standardized Analytical Outputs and Metrics
Table 2: Core Microbiome Metrics and Analytical Standards for Clinical Translation
| Analytical Category | Core Metrics | Standardized Tools/Pipelines | Clinical Interpretation |
|---|---|---|---|
| Alpha Diversity | Shannon Index, Faith's PD, Observed Features | QIIME 2, mothur, phyloseq | Microbial community richness and evenness; decreased diversity associated with dysbiosis |
| Beta Diversity | Weighted/Unweighted UniFrac, Bray-Curtis | PERMANOVA, ANOSIM in QIIME 2 | Between-sample dissimilarity; quantifies shifts in community structure |
| Differential Abundance | Log2 fold change, FDR-adjusted p-values | ANCOM-BC, DESeq2, MaAsLin2 | Identifies specific taxa associated with clinical phenotypes |
| Functional Potential | MetaCyc pathway abundance, enzyme commissions | HUMAnN3, PICRUSt2 | Predicts metabolic capabilities despite taxonomic variation |
| Validation | Sensitivity, specificity, AUC for biomarker panels | ROC analysis, cross-validation | Diagnostic performance of microbial signatures |
Microbiome-Host Interaction Pathways: Visualization of Key Mechanisms
Understanding the mechanistic basis of microbiome-host interactions is essential for developing targeted therapies. The diagram below illustrates the primary signaling pathways through which gut microbiota influence host physiology:
Essential Research Reagents and Materials for Standardized Microbiome Research
Table 3: Essential Research Reagents for Microbiome Investigations
| Reagent Category | Specific Products | Application | Quality Control Requirements |
|---|---|---|---|
| Nucleic Acid Stabilization | DNA/RNA Shield (Zymo Research), RNAlater | Preserves microbial community structure during sample storage | Demonstration of community stability across storage conditions |
| DNA Extraction Kits | DNeasy PowerSoil Pro (Qiagen), MagMAX Microbiome Kit | Standardized cell lysis and DNA purification | Consistent recovery across Gram-positive and negative bacteria |
| PCR Reagents | KAPA HiFi HotStart ReadyMix, Platinum SuperFi DNA Polymerase | Amplification of target regions with high fidelity | Low error rate, minimal amplification bias |
| Reference Standards | ZymoBIOMICS Microbial Community Standard, mock communities | Quality control and cross-study normalization | Certified composition and abundance values |
| Sequencing Kits | Illumina DNA Prep, 16S Metagenomic Sequencing Library Prep | Library preparation for high-throughput sequencing | Lot-to-lot consistency in library complexity |
| Bioinformatic Databases | SILVA, Greengenes, GTDB, KEGG, MetaCyc | Taxonomic classification and functional annotation | Regular updates with curated entries |
Clinical Translation Framework: From Biomarker Discovery to Therapeutic Development
Pathway for Microbiome-Based Diagnostic Development
The development of clinically applicable microbiome-based diagnostics requires rigorous validation across multiple cohorts. The following framework outlines a standardized approach:
Discovery Phase:
- Case-control design with well-phenotyped participants (minimum n=100/group)
- Multi-omics profiling (16S rRNA gene sequencing, metagenomics, metabolomics)
- Identification of candidate biomarkers with effect size >2.0 and FDR <0.05
Verification Phase:
- Technical validation using targeted approaches (qPCR, mass spectrometry)
- Analytical validation of sensitivity, specificity, precision, and linearity
- Establishment of standardized operating procedures for assay implementation
Validation Phase:
- Prospective blinded studies in independent cohorts
- Demonstration of clinical utility for prediction, diagnosis, or monitoring
- Development of clinical decision thresholds and interpretation guidelines
Implementation Phase:
- Regulatory approval (FDA, EMA) as laboratory-developed test or in vitro diagnostic
- Health economics assessment and development of reimbursement strategies
- Integration into clinical workflows with appropriate decision support
Microbiome-Targeted Therapeutic Development Pathways
Several therapeutic approaches are emerging for microbiome modulation, each with distinct development pathways:
Live Biotherapeutic Products (LBPs):
- Defined bacterial consortia with specific functional attributes
- Manufacturing challenges: viability maintenance, formulation stability
- Regulatory classification: biologics with requirements for strain characterization, safety testing, and potency assays
Microbiota Transplantation:
- Standardized donor screening and material processing protocols
- Indication-specific efficacy demonstration (beyond C. difficile infection)
- Regulatory status: tissue product with requirements for infectious disease testing
Phage Therapies:
- Targeted bacterial depletion with minimal collateral damage to commensals
- Specificity validation and resistance monitoring
- Regulatory pathway: complex biological product with customized requirements
Prebiotics and Synbiotics:
- Selective microbial stimulation with defined substrates
- Structure-function relationship establishment
- Regulatory classification: dietary ingredients or drugs depending on claims
The clinical translation of microbiome research holds tremendous promise for revolutionizing personalized medicine, yet this potential can only be realized through rigorous standardization and international harmonization. By implementing the protocols and frameworks outlined in this application note, researchers can enhance the reproducibility, comparability, and clinical utility of microbiome studies. The ongoing development of international standards through initiatives like STORMS and the continued evolution of the Human Microbiome Action framework will be critical for establishing microbiome-based diagnostics and therapeutics as mainstream clinical tools. As the field advances, continued collaboration between academic researchers, industry partners, and regulatory bodies will be essential for building the evidentiary foundation required to integrate microbiome-based approaches into clinical practice.
The field of microbiome-based therapeutics is transforming modern medicine, offering innovative ways to treat conditions ranging from gastrointestinal disorders to oncology and metabolic diseases [68]. However, the unique nature of living biological therapeutics presents distinct challenges for clinical trial design, particularly in the absence of well-defined regulatory guidelines. This complexity is reflected in the significant gap between promising research findings and demonstrated clinical efficacy, with many live microbial therapeutics showing limited success in treating conditions characterized by chronic inflammation [69]. The transition from non-clinical endpoints to clinically relevant outcomes represents a critical pathway for advancing microbiome science from laboratory research to routine clinical care [22].
The fundamental challenge in microbiome clinical translation lies in bridging the divide between mechanistic understanding and patient-centered outcomes. While metagenomic analyses have identified robust microbial signatures associated with various diseases, the clinical implementation of these findings remains limited by methodological variability, lack of standardized protocols, and insufficient validation across diverse populations [70]. This article provides a comprehensive framework for designing robust clinical trials that effectively translate microbiome research into clinically meaningful interventions, with specific focus on endpoint selection, trial design considerations, and practical methodologies for researchers and drug development professionals.
Key Challenges in Microbiome Clinical Trial Design
The Inflammation Barrier to Therapeutic Efficacy
A critical biological constraint emerging from recent meta-analyses is that intestinal inflammation significantly undermines the efficacy of live biotherapeutic products (LBPs). Cochrane meta-analyses reveal that approximately 90% of concluded probiotics and LBPs lack clinical efficacy in treating inflammatory bowel disease (IBD), a condition characterized by chronic intestinal inflammation [69]. Rank-biserial correlation tests have demonstrated a negative correlation between the presence of intestinal inflammation and positive clinical outcomes, whereas the absence of inflammation correlates with therapeutic success [69].
This pattern is exemplified by Escherichia coli Nissle 1917 (EcN), which shows efficacy in maintaining remission of ulcerative colitis comparable to frontline therapies yet fails to demonstrate clear benefit in treating active disease [69]. The proposed mechanism for this efficacy gap is the poor ability of therapeutic microbes to persist and colonize the inflamed intestine, highlighting how the disease state itself can create a biological barrier to engraftment and function.
Endpoint Selection Challenges
Microbiome-based therapies present unique challenges in endpoint selection due to their complex mechanisms of action and the multifactorial nature of host-microbe interactions. Traditional drug development endpoints, like pharmacokinetics, are often irrelevant for products that function through ecological modulation rather than systemic absorption [68]. This necessitates innovative approaches to endpoint selection that capture both mechanistic and clinical outcomes.
Table 1: Endpoint Categories in Microbiome Clinical Trials
| Endpoint Category | Examples | Utility | Limitations |
|---|---|---|---|
| Non-Clinical Endpoints | Microbial engraftment, Metagenomic signatures, Metabolite production | Mechanism of action, Early efficacy signals | Limited regulatory acceptance, Uncertain clinical relevance |
| Surrogate Endpoints | Fecal calprotectin reduction, Short-chain fatty acid increase, Bile acid modulation | Objective biomarkers, Pathophysiological relevance | Requires clinical validation, Context-dependent significance |
| Clinical Endpoints | Symptom improvement (e.g., stool consistency), Disease activity indices (e.g., Mayo score for UC), Endoscopic healing | Regulatory acceptance, Direct patient relevance | May require larger sample sizes, Subject to placebo effects |
Methodological and Regulatory Hurdles
The translation of microbiome science into clinical practice faces significant methodological challenges, including lack of standardized protocols, analytical heterogeneity, and insufficient representation of global populations in research cohorts [22] [70]. Direct-to-consumer (DTC) microbiome testing has further complicated the landscape, with significant analytical and methodological heterogeneity between providers, and health risk assessments that often lack robust scientific substantiation [22].
Regulatory frameworks for microbiome-based products continue to evolve, with the European Union recently classifying microbiota as a "substance of human origin," representing an important step toward harmonized regulatory approaches [22]. However, the absence of standardized guidelines means that close collaboration with regulatory authorities such as the FDA, EMA, or MHRA remains crucial throughout the drug development process [68].
Framework for Endpoint Selection and Validation
Integrating Non-Clinical and Clinical Endpoints
Effective trial design for microbiome-based products requires a strategic integration of non-clinical and clinical endpoints that captures the multifaceted nature of these interventions. Engraftment—the process by which a therapeutic microbiome integrates with or replaces the existing microbiome—represents a critical endpoint unique to these trials [68]. Successful engraftment can indicate potential efficacy but also raises safety concerns about disrupting the balance of the native microbiome, necessitating careful monitoring of short- and long-term effects.
Product-specific efficacy endpoints must align with the intended function and site of action. For gastrointestinal applications, this may include symptom improvement such as changes in stool consistency or reduced abdominal pain, while for dermatological applications, reduced skin inflammation or lesion counts would be more relevant [68]. The production or reduction of metabolites associated with the therapy's function provides an important intermediate endpoint that bridges mechanism and clinical effect.
Strategic Endpoint Progression Through Trial Phases
A phased approach to endpoint selection allows for efficient resource allocation while building compelling evidence for product efficacy. Early-phase trials can prioritize proof-of-concept through non-clinical endpoints, while later phases must transition to clinically relevant outcomes that support regulatory approval and clinical adoption.
Table 2: Endpoint Progression in Microbiome Clinical Development
| Trial Phase | Primary Endpoints | Secondary Endpoints | Exploratory Endpoints |
|---|---|---|---|
| Phase 1 | Safety, Tolerability | Engraftment, Microbiome modulation | Metabolite changes, Immunological markers |
| Phase 2 | Clinical response, Biomarker validation | Safety, Dose-response, Engraftment stability | Host-microbe interactions, Mechanistic pathways |
| Phase 3 | Clinically relevant endpoints (e.g., remission rates) | Quality of life, Safety, Biomarker correlation | Subgroup analyses, Long-term modulation |
For microbiome-based diagnostics, endpoint selection must focus on clinical utility, including predictive value for treatment response or disease risk stratification. Recent research has demonstrated this potential, with metagenomic analyses identifying microbial signatures that enhance the diagnostic accuracy of fecal occult blood tests for colorectal cancer [22]. Large cohort studies have further identified distinct microbiome signatures for CRC precursors, highlighting the potential of microbiome-based diagnostics for early detection and screening [22].
Methodologies and Experimental Protocols
Core Methodological Framework
Robust methodologies are essential for generating reliable, reproducible data in microbiome clinical trials. The following protocols provide a standardized approach for key experimental procedures:
Protocol 1: Longitudinal Stool Collection and Metagenomic Sequencing
- Sample Collection: Collect stool samples using standardized collection kits containing DNA/RNA stabilizers to preserve microbial composition. Record collection time, method, and storage conditions.
- DNA Extraction: Use mechanical lysis with bead-beating followed by commercial DNA extraction kits validated for microbiome studies. Include extraction controls and reference materials.
- Library Preparation: Employ PCR-free library preparation methods to reduce amplification bias. For shotgun metagenomics, fragment DNA to 350-500bp and use dual-indexed adapters.
- Sequencing: Perform sequencing on Illumina platforms (minimum 10 million 150bp paired-end reads per sample) or Oxford Nanopore Technologies for real-time analysis.
- Bioinformatic Analysis: Process raw sequences through quality control (FastQC), adapter removal (Trimmomatic), host DNA depletion (Bowtie2), and metagenomic assembly (MEGAHIT). Perform taxonomic profiling (Kraken2, MetaPhlAn) and functional annotation (HUMAnN3).
Protocol 2: Engraftment Monitoring
- Strain Tracking: For defined consortia, use strain-specific markers or genome sequencing to distinguish administered strains from endogenous microbiota.
- Longitudinal Sampling: Collect samples at baseline, during intervention, and post-cessation to monitor persistence. Optimal sampling frequency: weekly during intervention, biweekly post-cessation.
- Quantification: Apply quantitative PCR for specific strains or metagenomic sequencing with spike-in controls for absolute abundance quantification.
- Ecological Analysis: Calculate engraftment success using colonization resistance metrics, community similarity indices, and persistence duration.
Protocol 3: Multi-omics Integration for Mechanism Elucidation
- Metabolomic Profiling: Perform untargeted metabolomics on stool and serum samples using UHPLC-MS platforms. Include quality control pools and reference standards.
- Data Integration: Construct microbiome-metabolome correlation networks using platforms like MixOmics or MMINP. Identify key metabolites associated with microbial taxa.
- Pathway Analysis: Map metabolites to biochemical pathways (KEGG, MetaCyc) and integrate with metagenomic functional predictions.
- Validation: Confirm key findings using targeted approaches (quantitative metabolomics) in independent cohorts.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for Microbiome Clinical Trials
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| DNA/RNA Stabilizers | RNAlater, DNA/RNA Shield | Preserves nucleic acid integrity during sample storage/transport | Compatibility with downstream applications, Safety profile |
| DNA Extraction Kits | QIAamp PowerFecal Pro, DNeasy PowerSoil | Efficient microbial lysis and DNA purification | Yield, Inhibition resistance, Reproducibility |
| Reference Materials | NIST Stool Reference Material, ZymoBIOMICS Spike-in | Quality control, Quantification standardization | Commutability, Stability, Matrix matching |
| Library Prep Kits | Illumina DNA Prep, Nextera XT | Sequencing library construction | Bias minimization, Input DNA requirements, Cost |
| Cell Culture Media | Reinforced Clostridial Medium, BHI | Microbial viability assessment, Culturomics | Fastidious growth requirements, Aerobic/anaerobic conditions |
Visualization of Experimental Workflows
Microbiome Clinical Trial Workflow
Endpoint Validation Pathway
Advanced Considerations and Future Directions
Innovative Trial Designs for Complex Interventions
Microbiome-based therapeutics often require innovative trial designs that account for their unique mechanisms of action and the complex interplay between intervention, host, and environment. Adaptive trial designs can provide flexibility to adjust dosage or patient selection based on interim analyses of engraftment or biomarker data [68]. Platform trials, which evaluate multiple interventions simultaneously, may be particularly efficient for testing defined microbial consortia with varying compositions.
For companies facing financial constraints, particularly startups in the microbiome sector, cost-effective single-cohort trials that combine safety, tolerability, and efficacy assessments can provide crucial proof-of-concept data to secure additional funding [68]. While this approach may extend development timelines, it offers a financially feasible pathway to progress without compromising data quality.
Personalized Microbiome Medicine
The field is rapidly evolving toward personalized microbiome-based interventions, recognizing the significant inter-individual variation in microbial compositions and their functional capacities [71]. This includes tailored probiotics and synbiotics based on individual gut flora, microbiome profiling to guide treatment decisions, and customized dietary recommendations to optimize gut health and disease prevention [71].
Enterotyping—stratifying individuals by microbiome composition—adds a valuable dimension for precision diagnostics and treatment selection [70]. Recent studies have demonstrated that predicting treatment response is possible when stratifying participants by microbiome characteristics, opening the potential role of incorporating gut microbiome information for disease stratification, biomarkers, or add-on therapy [72].
Combination Therapies and Host-Microbe Targeting
Emerging evidence suggests that combining microbiome-based therapies with host-directed therapies may offer synergistic benefits by targeting both host and microbiome determinants of disease [22]. This approach represents a paradigm shift from targeting single pathways to modulating complex biological systems.
In oncology, for example, research has demonstrated that the gut microbiome plays a crucial role in modulating immune responses, which directly impacts the efficacy of immunotherapies [71]. Certain gut microbiota strains have been found to enhance the effectiveness of immune checkpoint inhibitors, leading to improved patient outcomes [71]. Clinical trials are currently investigating how gut microbiota composition influences cancer progression and response to therapy.
Designing robust clinical trials for microbiome-based products requires a fundamental shift from traditional drug development approaches. The successful translation from non-clinical endpoints to clinically relevant outcomes depends on strategic endpoint selection, methodological rigor, and acknowledgment of the unique biological challenges presented by living therapeutics. Particular attention must be paid to the inflammatory context of target diseases, as intestinal inflammation has been consistently identified as a barrier to therapeutic efficacy.
The future of microbiome clinical translation will be shaped by continued standardization efforts, improved clinical trial design, and enhanced collaboration between academia, industry, and regulatory bodies. International initiatives such as the Human Microbiome Action, the Strengthening the Organization and Reporting of Microbiome Studies (STORMS) checklist, and the Microbiome Quality Control Project are critical steps toward harmonized methodologies and reporting standards [22]. As these efforts mature, microbiome-based diagnostics and therapeutics will increasingly fulfill their potential to transform patient care across a spectrum of diseases.
Regulatory Hurdles and the Path to Market for Microbiome-Based Products
The emergence of microbiome-based therapies (MbTs) represents a paradigm shift in modern therapeutics, introducing unique regulatory challenges that traditional frameworks are adapting to address. These products encompass a broad spectrum, from microbiota transplantation (MT) to live biotherapeutic products (LBPs), each occupying a distinct position on a continuum of complexity and manufacturing control [73]. The regulatory status of a microbiome-based product is critically determined by its intended use—specifically, the objective intent of the persons responsible for its labeling as shown by claims, advertising, or design—which ultimately dictates whether it is regulated as a medicinal product, food supplement, or other product category [73].
Global regulatory bodies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), are actively refining guidelines to balance patient safety with scientific innovation, giving rise to the specialized field of microbiome regulatory science [73]. This evolution is evidenced by recent landmark approvals, such as Rebyota and VOWST, for preventing recurrent Clostridioides difficile infections (rCDI), which have paved a regulatory pathway for subsequent products [73] [74]. This application note delineates the current regulatory frameworks, details essential characterization protocols, and provides a strategic roadmap for the successful clinical translation and commercialization of microbiome-based products.
Regulatory Framework and Classification
The Microbiome Therapy Continuum and Regulatory Implications
Microbiome-based therapies are not a monolithic category but exist on a spectrum defined by their complexity and degree of manufacturing manipulation. This continuum directly influences their associated regulatory pathways and the specific challenges they face.
Table 1: The Microbiome-Based Therapy (MbT) Continuum and Regulatory Considerations [73]
| Therapy Category | Description | Key Regulatory Considerations |
|---|---|---|
| Microbiota Transplantation (MT) | Transfer of a minimally manipulated microbial community from a human donor to a human recipient. | High donor screening importance; pathogen transmission risk; complex characterization challenges. |
| Donor-Derived Microbiome-Based Medicinal Products | Whole or highly complex ecosystems derived from human microbiome samples with industrial manufacturing. | Need for harmonized terminology; controlled manufacturing processes; analytical method validation. |
| Rationally Designed Ecosystem-Based Medicinal Products | Controlled ecosystems of multiple strains produced via co-fermentation from clonal cell banks. | Batch-to-batch consistency; process qualification; thorough strain characterization and potency testing. |
| Live Biotherapeutic Products (LBPs) | Defined single strain or consortium of strains, fermented separately and blended, produced from clonal cell banks. | Donor impact minimal; requires full characterization, purity, potency, and identity testing per FDA/EMA guidance. |
A pivotal concept in regulation is the donor/origin impact. For complex, minimally manipulated products like MT, the donor's profile is a major component of the risk-benefit assessment. In contrast, for highly defined products like LBPs, the impact of the original donor diminishes significantly, replaced by the critical need for process control and validation [73]. Furthermore, a key regulatory distinction exists between donor-derived products (e.g., Rebyota) and donor-independent LBPs manufactured from defined clonal cell banks. The latter category faces a more complex regulatory path, as no such products have yet received market approval, leading to less standardized guidance [74].
Evolving Global Regulatory Guidance
The regulatory environment is dynamic, with authorities working to close guidance gaps. The FDA's 2016 LBP guidance remains a foundational document, but the field requires further refinement and standardization [74]. A significant development is the European Union's new Regulation on Substances of Human Origin (SoHO), which directly impacts the development of microbiome-based therapies [73]. Simultaneously, international consortia, such as the Asia-Pacific Microbiota Consortium, have released updated guidelines in 2025, emphasizing the use of human-derived and food-sourced strains for their inherent safety, and outlining requirements for preclinical evaluation, cell banking, and genetic monitoring [75].
Engagement with regulatory agencies through pre-submission meetings is highly recommended. The Microbiome Therapeutics Innovation Group (MTIG) exemplifies how industry-wide collaboration can help catalyze improvements in LBP analytics and refine the regulatory landscape [74]. The following diagram illustrates the interconnected challenges and potential solutions throughout the product development lifecycle.
Market Outlook and Quantitative Analysis
The microbiome therapeutic market is experiencing significant growth, driven by increased recognition of the microbiome's role in chronic diseases and rising investments in precision medicine.
Table 2: Microbiome Therapeutic Market Forecast and Regional Growth Analysis (2025-2035) [76]
| Region/Country | Projected CAGR (%) (2025-2035) | Key Market Drivers & Regional Focus |
|---|---|---|
| Global Market | 14.2% | Rising chronic disease prevalence; investment in precision medicine and biotech innovation. |
| United States | 10.4% | Focus on personalized medicine, gut health research, and AI-based microbiome profiling. |
| China | 11.6% | Rapid economic growth, large patient base, thriving biotech sector, and government support. |
| South Korea | 9.8% | Advanced biotech infrastructure, government backing, and cultural inclination toward holistic wellness. |
| European Union (e.g., UK, Germany, France) | 8.8% - 9.3% | Strong biomedical research, clinical practice emphasis, and green production innovations. |
This robust growth, from a valued of USD 823.5 million in 2025 to a projected USD 3,121.8 million by 2035, underscores the commercial viability of the sector [76]. Industry surveys indicate that 81% of stakeholders are prioritizing robust clinical validation frameworks, while 76% highlight the need for transparent, customized regulatory pathways for LBPs [76]. The market is also expanding beyond gastrointestinal applications into oncology, mental health, and autoimmune disorders, demanding even more specialized regulatory and clinical strategies [76].
Experimental Protocols for Product Characterization
Protocol 1: Microbial Identification and Characterization
Objective: To unambiguously identify and characterize the microbial strain(s) in a Live Biotherapeutic Product (LBP) using complementary methods to meet regulatory requirements for identity testing [74].
Background: Regulatory agencies recommend at least two complementary methods for microbial identification (ID) and active ingredient assessment. Traditional phenotypic methods are often insufficient for LBPs, especially multi-strain consortia [74].
Materials:
- Research Reagent Solutions & Essential Materials:
- Strain-specific qPCR Assays: For precise identification and quantification of strains with highly similar 16S sequences [74].
- 16S rRNA Gene Sequencing Primers & Reagents: For broad-spectrum taxonomic classification [74].
- MALDI-TOF Mass Spectrometry System: For rapid, high-throughput identification based on protein profiles [74].
- Selected Growth Media: A range of media types (e.g., selective, differential) tailored to the growth requirements of each strain in the LBP [74].
- "Spike-in" Sequencing Controls: Defined microbial communities or synthetic DNA controls to monitor technical variability and validate sequencing assay performance [74].
Procedure:
- Culture Revival: Revive the bacterial strain from the master cell bank onto appropriate non-selective solid media. Incubate under optimal conditions (e.g., 37°C, anaerobic).
- Colony Picking: Select isolated colonies for analysis.
- DNA Extraction: Perform genomic DNA extraction using a standardized kit suitable for Gram-positive and Gram-negative bacteria.
- 16S rRNA Gene Sequencing: Amplify the 16S rRNA gene using universal primers (e.g., 27F/1492R). Purify the PCR product and sequence it using Sanger sequencing. Analyze the resulting sequence by comparing it to a curated database (e.g., SILVA, Greengenes) for taxonomic assignment.
- Strain-Level Confirmation: If higher resolution is needed (e.g., to distinguish between strains of the same species), perform a strain-specific qPCR assay or whole-genome sequencing.
- Phenotypic Correlation (Optional but Recommended): Analyze the same isolate using MALDI-TOF MS to create a protein fingerprint profile for future rapid identification and quality control.
- Data Analysis and Reporting: Compile results from all methods. The identity is confirmed when results from at least two orthogonal methods are concordant.
Protocol 2: Potency and Viability Testing via Colony Forming Unit (CFU) Enumeration
Objective: To determine the viable count of each active microbial strain in a single- or multi-strain LBP for potency release and stability testing.
Background: Potency is a critical quality attribute. A viable cell count (CFU) is often used as a potency measure, especially when the mechanism of action is linked to live bacteria. For multi-strain products, this requires meticulous method development [74].
Materials:
- Research Reagent Solutions & Essential Materials:
- Strain-Selective Media: Formulated to allow growth of the target strain while inhibiting others in a consortium. Requires validation for specificity.
- Automated Colony Counters: For objective and reproducible enumeration.
- Controlled Atmosphere Workstation (Anaerobic Chamber): Essential for cultivating obligate anaerobes under strict atmospheric conditions.
- Cryopreservation Solutions: Like glycerol stocks, for maintaining long-term viability of cell banks and reference standards.
Procedure:
- Sample Preparation: Thaw or resuspend the LBP sample in an appropriate reduced transport fluid or dilution medium. Serially dilute the sample (e.g., 10-fold serial dilutions) to achieve a countable range (30-300 colonies per plate).
- Plating: For a single-strain LBP, plate dilutions onto non-selective media in duplicate. For a multi-strain LBP, plate identical dilutions onto both a non-selective medium and each strain-specific selective medium.
- Incubation: Incubate plates under optimal conditions for each strain (specific temperature, time, and atmosphere, e.g., anaerobic for gut microbes).
- Enumeration and Identification: Count colonies on each plate.
- Non-selective plates: Total viable count and observation of colony morphologies.
- Selective plates: Count of the specific target strain.
- Confirmation: Pick colonies from non-selective plates and identify them via a rapid method (e.g., MALDI-TOF) to confirm purity and assess strain-to-strain interference.
- Calculation: Calculate the CFU per mL or per dosage form for each strain, applying the dilution factor.
Validation Notes: The method must be validated for each strain to ensure accuracy, precision, specificity, and robustness. For multi-strain products, cross-growth interference on selective media must be quantified and acceptance criteria set accordingly [74].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development and regulatory approval of microbiome-based products rely on a suite of specialized reagents and tools.
Table 3: Essential Research Reagent Solutions for Microbiome Product Development [73] [75] [74]
| Category | Specific Examples | Function & Application |
|---|---|---|
| Cell Banking & Culture | Master and Working Cell Banks, Cryopreservatives (e.g., glycerol) | Ensures long-term genetic stability and provides a consistent source of microbial strains for manufacturing. |
| Genomic Analysis | 16S rRNA PCR Primers, Whole Genome Sequencing Kits, Strain-specific qPCR Assays | For microbial identification, purity assessment, and genetic stability monitoring. |
| Selective Media | Strain-specific culture media | Enables selective growth and enumeration of individual strains within a multi-strain consortium for potency testing. |
| Advanced Analytics | MALDI-TOF MS, Metagenomic Sequencing Kits, "Spike-in" Controls | Provides high-throughput identification and characterization. Controls monitor technical variability in complex assays. |
| GMP Manufacturing | Raw Materials (e.g., GMP-grade growth substrates), Single-Use Bioreactors | Ensures product is manufactured under controlled, reproducible, and contaminant-free conditions. |
Strategic Roadmap for Market Approval
Navigating the path to market requires a proactive, strategic, and integrated approach from the earliest stages of development. The following workflow outlines the critical stages and key activities for achieving regulatory success.
Key Strategic Pillars:
- Engage Regulators Early and Often: Request pre-submission meetings with agencies like the FDA to discuss your development strategy, proposed analytical methods, and clinical trial design. This early alignment de-risks later development stages [74].
- Invest in Robust Analytical Development: Prioritize the development, optimization, and validation of methods for identity, purity, potency, and stability. For multi-strain LBPs, focus on resolving strain-to-strain interference in quantification assays [74].
- Prioritize Quality and Consistency from the Outset: Implement Good Manufacturing Practice (GMP) principles early. Establish rigorous cell banking practices and genetic monitoring to ensure product consistency and safety throughout the product lifecycle [75].
- Design Clinically Relevant and Mechanistically Informed Trials: Clinical trials must be meticulously designed with robust safety and risk management protocols. As the field matures, potency assays should ideally be linked to a understood mechanism of action (MoA) rather than relying solely on viability [75] [74].
- Plan for Post-Marketing Surveillance: Develop a comprehensive pharmacovigilance plan to monitor the long-term safety and real-world effectiveness of the product after approval, a key expectation of regulators [75].
By adhering to this structured approach—grounded in rigorous science, proactive regulatory dialogue, and strategic planning—developers can successfully navigate the complex path to market for innovative microbiome-based therapies.
The landscape of clinical microbiome research has dramatically evolved over the past decade, moving from descriptive associations to mechanism-based understanding of how microbial communities influence human health and disease [17]. By leveraging in vivo and in vitro experimentation, multiomic approaches, and computational biology, researchers have uncovered specific mechanisms of action, microbial metrics of association, and effective methods for modifying the microbiome across numerous diseases and treatment modalities [17]. This progress has spearheaded Food and Drug Administration (FDA)-approved microbiome therapies for recurrent Clostridioides difficile infections and emerging microbiome-based diagnostics and therapeutics for other conditions [17]. However, the translation of these advances into routine clinical practice faces significant barriers, including interindividual variability, incomplete functional annotation of microbial "dark matter," and the absence of validated biomarkers [53]. Addressing these challenges requires a concerted effort in clinician education and interdisciplinary collaboration to bridge the knowledge gap between fundamental research and clinical application.
The complexity of host-microbiome interactions necessitates moving beyond siloed approaches toward integrated research frameworks. As the field progresses, it becomes increasingly evident that leveraging existing connections between microbiome researchers can inform and guide the future of microbiome science, catalyze collaborative investigations, and aid in developing proposals to attract funding [77]. This article outlines the current state of microbiome-based diagnostics and therapeutics, presents standardized experimental protocols, and proposes frameworks for interdisciplinary collaboration to accelerate clinical translation.
Current Landscape of Microbiome-Based Diagnostics and Therapeutics
Diagnostic Capabilities and Methodologies
Microbiome-based diagnostics leverage various technologies to characterize microbial ecosystems for disease detection, risk stratification, and therapeutic monitoring. The gut microbiome, one of the most complex and functionally diverse microbial ecosystems in the human body, has demonstrated particular diagnostic potential across gastrointestinal, metabolic, and immune-mediated conditions [53]. Several methodological approaches have emerged, each with distinct capabilities and limitations for clinical application.
Table 1: Comparison of Major Microbiome Diagnostic Methodologies
| Method | Detectable Microbes | Relative Abundance | Absolute Abundance | Species Richness | Resistome | Clinical Applications |
|---|---|---|---|---|---|---|
| Culture-Based | Culturable organisms only | Semiquantitative for culturable organisms | Semiquantitative for culturable organisms | Culturable organisms | In vitro phenotypic susceptibility | Infection control surveillance [78] |
| qPCR | Known targets only | Limited | Limited | Limited | If known resistance sequences exist | Targeted pathogen detection [78] |
| 16S rRNA Sequencing | All bacterial targets | Yes | No | Yes | Possibly inferred from taxonomy | Community profiling, dysbiosis assessment [78] |
| Shotgun Metagenomic Sequencing (MGS) | All domains (bacteria, fungi, viruses) | Yes | No | Yes | Identifies known resistance sequences | Comprehensive community and functional profiling [78] |
| Quantitative Microbiome Profiling (QMP) | Depends on sequencing technique | Yes | Yes | Yes | Depends on sequencing technique | Biomarker identification with absolute abundance [79] |
| Metabolomics | Reflects impact of microbiome composition | No | No | No | Undefined | Functional activity assessment [78] |
The transition from relative to quantitative microbiome profiling represents a critical advancement for clinical translation. Traditional relative microbiome profiling (RMP), where taxon abundances are expressed as percentages, remains dominant but suffers from compositionality issues that can lead to spurious associations [79]. Quantitative microbiome profiling (QMP) addresses these limitations by providing absolute abundance measurements, reducing both false-positive and false-negative rates in downstream analyses, thereby focusing clinical programs on biologically relevant targets [79]. The importance of this approach was highlighted in a recent colorectal cancer (CRC) study, where well-established microbiome CRC targets, such as Fusobacterium nucleatum, did not significantly associate with CRC diagnostic groups when controlling for covariates like transit time, fecal calprotectin, and body mass index [79].
Established and Emerging Therapeutic Applications
Microbiome-based therapeutics have expanded beyond fecal microbiota transplantation (FMT) for recurrent C. difficile infection to include targeted interventions such as phage therapy, live biotherapeutic products, precision nutrition, and microbiota transplantation [53]. These approaches aim to restore healthy microbial communities or target specific pathogenic functions while preserving commensal microbes.
Table 2: Microbiome-Based Therapeutic Approaches in Development
| Therapeutic Approach | Composition | Mechanism of Action | Development Stage | Target Conditions |
|---|---|---|---|---|
| Fecal Microbiota Transplantation (FMT) | Complex, undefined microbial community | Restore diverse gut microbiota | FDA-approved for rCDI; investigational for other indications [17] | Recurrent C. difficile infection (rCDI) [17] |
| Defined Microbial Consortia | Specific bacterial strains in defined ratios | Introduce missing functions or compete with pathogens | Clinical trials | IBD, metabolic syndrome [4] |
| Phage Therapy | Bacteriophage cocktails targeting specific pathobionts | Precisely eliminate disease-contributing strains | Phase 1 clinical trials [4] | IBD (Klebsiella pneumoniae suppression) [4] |
| Live Biotherapeutic Products | Single strain or simple mixtures of beneficial bacteria | Deliver specific health-promoting functions | Clinical development | Metabolic syndrome (Akkermansia muciniphila) [4] |
| Precision Nutrition | Dietary interventions personalized to microbiome | Modulate microbial community structure and function | Research and commercial development | Metabolic health, weight management [4] |
Innovative therapeutic strategies are increasingly moving from human-derived to synthetic communities. While FMT has demonstrated efficacy for recurrent C. difficile infection, its effectiveness remains variable depending on delivery method and donor characteristics, and it carries risks of pathogen transfer [4]. Defined microbial consortia offer several advantages, including reduced risk of pathogen transmission, improved product consistency, and enhanced engineerability [4]. Research indicates that complex defined consortia of bacteria (more than 100 strains) harbor highly diverse metabolic pathways that can engraft reliably and consistently compared to simpler consortia [4].
Experimental Protocols for Microbiome Research
Quantitative Microbiome Profiling with Confounder Control
Robust microbiome research requires meticulous experimental design that incorporates quantitative assessment and comprehensive confounder control. The following protocol outlines an approach for biomarker identification that addresses these considerations, based on methodologies successfully applied in colorectal cancer studies [79].
Sample Collection and Storage
- Collection Material: Use sterile, DNA-free containers with stabilizers if immediate freezing is not possible
- Temperature Control: Flash-freeze samples in liquid nitrogen or place on dry ice immediately after collection
- Storage: Maintain consistent storage at -80°C; avoid freeze-thaw cycles
- Documentation: Record collection time, date, and processing intervals precisely
- Quality Assessment: Note sample color, consistency, and any irregularities
DNA Extraction and Quantification
- Extraction Method: Use mechanical lysis with bead beating for comprehensive cell disruption across bacterial taxa
- Inhibition Control: Include internal standards or spike-in controls to detect PCR inhibitors
- Quality Assessment: Measure DNA concentration using fluorometric methods (e.g., Qubit) rather than spectrophotometry for accuracy
- Normalization: Implement quantitative microbiome profiling (QMP) using flow cytometry or digital PCR for absolute abundance determination [79]
Library Preparation and Sequencing
- 16S rRNA Gene Sequencing:
- Target the V4 region using primers 515F/806R with Illumina overhang adapters
- Include negative controls (extraction blanks) and positive controls (mock communities) in each batch
- Perform amplification in triplicate to reduce PCR bias
- Use low-cycle PCR (≤25 cycles) to minimize amplification artifacts
- Shotgun Metagenomic Sequencing:
- Fragment DNA to 300-500 bp using ultrasonication
- Use library preparation kits with minimal bias
- Sequence to sufficient depth (≥10 million reads per sample for complex communities)
Bioinformatic Processing
- 16S rRNA Data:
- Process using DADA2 for amplicon sequence variant (ASV) inference
- Trim primers and filter reads based on quality scores
- Remove chimeras using consensus method
- Assign taxonomy using SILVA or Greengenes database
- Shotgun Metagenomic Data:
- Perform quality control with FastQC and Trimmomatic
- Remove host reads using alignment to human reference genome
- Perform taxonomic profiling with MetaPhlAn or Kraken2
- Conduct functional analysis with HUMAnN2 for pathway abundance
Covariate Assessment and Statistical Analysis
- Essential Covariates: Measure and control for transit time (via moisture content), intestinal inflammation (fecal calprotectin), and BMI [79]
- Additional Variables: Document age, medication use (especially antibiotics and PPIs), dietary patterns, and dental health
- Statistical Methods:
- Apply appropriate multiple testing correction (e.g., Benjamini-Hochberg FDR)
- Use multivariate models (PERMANOVA) to partition variance among covariates
- Employ cross-validation to assess model robustness
- Implement machine learning approaches with strict train-test separation
Reagent Solutions for Microbiome Research
Table 3: Essential Research Reagents for Microbiome Studies
| Reagent Category | Specific Products/Methods | Function | Considerations |
|---|---|---|---|
| Sample Preservation | RNAlater, DNA/RNA Shield, -80°C freezing | Preserve microbial composition at time of collection | Storage at -80°C appears most appropriate; different methods produce unique taxonomic profiles [4] |
| DNA Extraction Kits | MoBio PowerSoil, QIAamp Fast DNA Stool Kit | Comprehensive cell lysis and DNA purification | Mechanical lysis with bead beating essential for gram-positive bacteria |
| Quantification Standards | Flow cytometry, digital PCR, synthetic spike-ins | Absolute abundance quantification | Enables quantitative microbiome profiling [79] |
| PCR Amplification | 16S primers (515F/806R), high-fidelity polymerases | Target amplification for sequencing | Low-cycle PCR reduces bias; include mock communities |
| Sequencing Kits | Illumina MiSeq, NovaSeq, PacBio | High-throughput DNA sequencing | Choice affects read length, depth, and error rates |
| Reference Materials | Human Fecal Reference Material | Method standardization and cross-study comparison | Enables harmonization across laboratories [4] |
Interdisciplinary Collaboration Framework
Effective translation of microbiome research requires integration of diverse expertise across scientific disciplines, clinical specialties, and regulatory domains. The complexity of host-microbiome interactions necessitates collaborative approaches that bridge traditional academic and clinical silos.
Model for Integrated Microbiome Research
Successful interdisciplinary programs share common structural elements that facilitate collaboration and accelerate translation. The University of North Carolina's Interdisciplinary Microbiome Research Program (IMeRP) provides a framework that can be adapted across institutions [77]. This model aims to:
- Leverage existing connections between microbiome researchers to inform and guide the future of microbiome science
- Catalyze collaborative science through structured interactions and shared resources
- Aid in attracting high-profile microbiome researchers through critical mass and infrastructure
- Enable the development of proposals to attract substantial funding
- Increase visibility for microbiome research through unified institutional identity [77]
Regulatory Considerations for Translation
Navigating the regulatory landscape represents a critical component of successful clinical translation. Regulatory agencies including the FDA (United States) and EMA (Europe) have established pathways for microbiome-based products, with important distinctions based on product composition and intended use [4]:
- Investigational New Drug (IND) Requirements: An IND is required prior to initiating a clinical trial for any product intended to treat, prevent, or cure a human disease or condition, including live biotherapeutic products [4].
- Chemistry, Manufacturing, and Controls (CMC): Critical safety considerations include bioburden testing and assessment of antimicrobial sensitivities of the product organism(s) [4].
- Probiotics Regulation: Probiotics regulated as foods and dietary supplements are not subject to IND requirements unless the intended use is to treat, prevent, or cure a human disease or condition [4].
- European Framework: In Europe, microbiome-based medicinal products intended to treat or prevent disease are regulated by pharmaceutical legislation (Directive 2001/83/EC) and considered biological medicinal products [4].
Bridging the knowledge gap in microbiome science requires sustained commitment to clinician education and interdisciplinary collaboration. As research continues to unravel the complex relationships between microbial communities and human health, translating these insights into clinical practice demands robust methodologies, standardized protocols, and frameworks that facilitate cooperation across traditional disciplinary boundaries. The integration of quantitative approaches, comprehensive confounder control, and structured collaborative models will accelerate the development of microbiome-based diagnostics and therapeutics, ultimately advancing precision medicine and improving patient outcomes.
Evidence and Efficacy: Validating Microbiome Applications Across Diseases
Within the clinical translation of microbiome research, Fecal Microbiota Transplantation (FMT) and Live Biotherapeutic Products (LBPs) have emerged as transformative therapeutic modalities for gastrointestinal indications. FMT involves transplanting functional microbiota from healthy donors to patients to restore microbial balance, while LBPs represent standardized, pharmaceutical-grade formulations of beneficial live microorganisms [80] [81]. The gut microbiome plays a fundamental role in human health, and its disruption (dysbiosis) is implicated in various gastrointestinal disorders [80]. This Application Note provides a structured analysis of the efficacy data, detailed experimental protocols, and mechanistic insights for FMT and LBP applications, serving researchers and drug development professionals engaged in microbiome therapeutic development.
Quantitative Efficacy Analysis
Comparative Clinical Success Rates Across GI Indications
Table 1: Efficacy of FMT and LBPs for Gastrointestinal Conditions
| Indication | Therapy | Efficacy Rate/Outcome | Evidence Quality | Key Findings |
|---|---|---|---|---|
| Recurrent C. difficile Infection (rCDI) | FMT | 80-90% resolution [81] | High (Moderate to High GRADE) [82] | Superior to standard antibiotic therapy (81% vs 31%) [81] |
| LBP (SER-109) | 12% recurrence vs 40% for placebo [81] | High (Phase III RCT) [81] | Firmicutes-spore based formulation | |
| LBP (RBX2660) | 70.4% success vs 58.1% for placebo [81] | High (Phase III RCT) [81] | Microbial consortium derived from human stool | |
| Ulcerative Colitis (UC) | FMT | 30.43% remission vs 9.82% for placebo (OR 4.11) [81] | Moderate (Meta-analysis) [82] | Lower efficacy than for rCDI but statistically significant |
| Irritable Bowel Syndrome (IBS) | FMT | OR = 0.46 (95% CI: 0.33-0.64) [83] | Low to Moderate [82] | Significant improvement in symptoms |
| Probiotics (specific strains) | OR = 0.53 (95% CI: 0.48-0.59) [83] | Moderate (Network Meta-analysis) [83] | Particularly Bifidobacterium and Lactobacillus | |
| Functional Constipation | FMT | Positive association [82] | Low-quality evidence [82] | Statistically significant but low-grade evidence |
| Metabolic Syndrome | FMT | Does not appear to be associated with positive outcomes [82] | Low-quality evidence [82] | Limited evidence for efficacy |
Efficacy Determinants and Modifiers
The therapeutic success of microbiome-based interventions is influenced by several critical factors. Administration route significantly impacts safety and patient tolerance, with capsule-based delivery emerging as a strategy to reduce procedural risks [81]. Donor microbiota composition and recipient microbial engraftment are crucial, as the antagonistic nature of a recipient's native bacteria can limit the colonization of transplanted beneficial strains [84]. Recent advances include probiotic preconditioning of donor microbiota, exemplified by L. plantarum GR-4 pretreatment, which enhances stress resistance and butyrate production, achieving an 83% remission rate in colitis models compared to 50% with conventional FMT [85].
Experimental Protocols
Protocol: FMT for Ulcerative Colitis Treatment
Objective: To evaluate the efficacy of FMT in inducing clinical and endoscopic remission in active ulcerative colitis patients.
Materials and Reagents:
- Donor stool screening kits (multidrug-resistant organisms, SARS-CoV-2, enteric pathogens)
- Sterile normal saline or glycerin
- Stool processing equipment (anaerobic chamber, blender, filtration system)
- Administration supplies (colonoscopy equipment or nasoenteric tubes/capsules)
Procedure:
- Donor Screening: Comprehensively screen donors for transmissible pathogens, multidrug-resistant organisms, and health history [81].
- Stool Processing: Process stool within 6 hours of donation under aerobic or preferred anaerobic conditions. Dilute with saline or glycerin (typically 50-100g stool in 200-500ml liquid), homogenize, and filter through sequential filters (0.5-2.0mm) to remove particulate matter [81].
- Recipient Preparation: Perform colonoscopy bowel preparation or administer proton pump inhibitors for upper GI delivery to enhance engraftment.
- Administration:
- Lower GI: Deliver via colonoscopy (≥30g microbiota) or enema (10-30g microbiota).
- Upper GI: Administer via nasoenteric tube or acid-resistant capsules (typically 12-12g microbiota over multiple days) [81].
- Follow-up: Assess clinical symptoms, endoscopic remission, and adverse events at 4-8 weeks post-treatment. Monitor microbial engraftment via serial stool sampling [82] [81].
Quality Control:
- Standardize microbiota quantification (16S rRNA sequencing)
- Test final product for pathogens and aerobicity
- Utilize central donors or rigorously screened individual donors
Protocol: Probiotic-Enhanced FMT (MFMT)
Objective: To enhance donor microbiota stability, functionality, and therapeutic efficacy through probiotic preconditioning [85].
Materials and Reagents:
- Lactobacillus plantarum GR-4 (or comparable strain)
- Anaerobic culture media (MRS broth)
- Sterile phosphate-buffered saline (PBS)
- pH measurement equipment
- Metabolomic analysis kits (for indoles, SCFAs, bile acids)
Procedure:
- Donor Preconditioning: Administer L. plantarum GR-4 to donor mice for 3 weeks (human equivalent: 1×10^9 CFU/day) [85].
- Modified FMT (MFMT) Preparation: Collect stool from preconditioned donors and process as standard FMT with maintenance of anaerobic conditions.
- Characterization: Assess MFMT for:
- Acidification: Measure pH (target ~3.97)
- Metabolite Profile: Quantify butyrate increase (target ~73% elevation) and immunomodulatory indoles (ILA, IAA)
- Stress Resistance: Evaluate bile acid and gastric condition survival (target 1.25× survival vs conventional FMT) [85]
- Administration: Administer MFMT to recipients using standard FMT protocols.
- Assessment: Monitor engraftment efficiency (target 1.25× improvement), remission rates, and metabolic parameters.
Protocol: LBP Efficacy Testing for IBS
Objective: To evaluate the efficacy of LBPs containing Bifidobacterium and Lactobacillus strains in improving IBS symptoms [83].
Materials and Reagents:
- LBP formulation (lyophilized or encapsulated)
- Placebo control (matched formulation without active strains)
- IBS-SSS (Symptom Severity Score) questionnaire
- Quality of Life measurement tools (IBS-QOL)
- Stool collection kits for microbiome analysis
Procedure:
- Study Design: Randomized, double-blind, placebo-controlled trial with 8-12 week intervention period.
- Participant Recruitment: Enroll adults meeting Rome IV criteria for IBS, excluding other GI pathologies.
- Randomization: Assign participants to LBP (typically 1×10^9-1×10^10 CFU/day) or matched placebo groups.
- Outcome Assessment:
- Primary Outcome: Global IBS symptom improvement (≥30-point reduction in IBS-SSS)
- Secondary Outcomes: Abdominal pain severity, bloating, stool frequency/consistency (Bristol Stool Form Scale), quality of life measures
- Microbiome Analysis: Collect serial stool samples for 16S rRNA sequencing to assess microbial changes and engraftment.
- Safety Monitoring: Record adverse events (particularly GI symptoms) throughout study period.
Statistical Analysis:
- Calculate odds ratios for treatment response with 95% confidence intervals
- Perform network meta-analysis if comparing multiple probiotic regimens
Signaling Pathways and Mechanisms
Mechanistic Pathways of FMT and LBPs in GI Disease
The therapeutic mechanisms of FMT and LBPs operate through multiple interconnected pathways. Microbial ecosystem restoration involves increasing beneficial taxa (Sporobacter, Butyricimonas) while suppressing pathogens (Clostridium papyrosolvens), enhancing colonization resistance against C. difficile [85]. Metabolic reprogramming includes elevated butyrate production (73% increase), which enhances gut barrier function, and generation of immunomodulatory indoles (ILA, IAA) from tryptophan metabolism, activating the aryl hydrocarbon receptor (AHR) pathway [85]. Immunomodulation occurs through AHR-mediated upregulation of anti-inflammatory cytokines (IL-10, IL-22), reducing intestinal inflammation [85]. Bile acid remodeling restores physiological ratios of sulfolithocholic acid (SLCA) and β-muricholic acid (β-MCA), resolving metabolic dysregulation associated with colitis [85].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Specification Notes |
|---|---|---|
| Anaerobic Chamber | Maintain oxygen-free environment for stool processing and microbial culture | Ensure <1 ppm O₂ for strict anaerobe viability |
| MedDRA Coding Dictionary | Standardize adverse event terminology for pharmacovigilance | Use latest version (e.g., 25.1) for FAERS reporting [86] |
| 16S rRNA Sequencing Kits | Profiling microbial community composition and diversity | Include standards for quantification and contamination control |
| SCFA Analysis Standards | Quantify microbially-derived metabolites (butyrate, acetate, propionate) | Utilize GC-MS or LC-MS protocols with internal standards |
| Bile Acid Panels | Assess bile acid remodeling in response to therapy | Measure primary/secondary ratios and specific species (β-MCA, SLCA) |
| AHR Activation Assay | Evaluate immunomodulatory pathway engagement | Reporter gene assays in appropriate cell lines |
| Strain-Specific Probes | Track engraftment of donor or LBP strains | Design for FISH, qPCR, or genome-based detection |
| Cytokine ELISA Panels | Quantify inflammatory and anti-inflammatory mediators | Focus on IL-10, IL-22, TNF-α for IBD applications |
| Colonoid/Organoid Systems | Test host-microbe interactions in human-derived models | Establish from patient biopsies for personalized medicine approaches |
FMT and LBPs represent promising therapeutic approaches with proven efficacy for specific gastrointestinal indications, particularly rCDI, ulcerative colitis, and IBS. The success of these interventions depends on multiple factors, including administration route, donor-recipient matching, and the ability to overcome colonization resistance in the recipient's gut [84]. Future development should focus on standardizing protocols, enhancing bacterial engraftment through approaches like probiotic preconditioning [85], and identifying patient subgroups most likely to respond to these innovative therapies. As the field advances, the transition from complex fecal preparations to defined LBPs offers a pathway to more reproducible, scalable, and regulatable microbiome-based therapeutics.
The human microbiome, particularly the gut microbiota, has transitioned from a subject of basic science to a central pillar in understanding and treating a broad spectrum of diseases. This expansion is driven by the recognition that these complex microbial communities are not passive inhabitants but active participants in host physiology, influencing immunity, metabolism, and inflammation. Clinical translation of microbiome research is now a vibrant frontier, moving beyond association to causation and therapeutic intervention [87]. The core premise is that microbiome modulation—through dietary strategies, live biotherapeutics, fecal microbiota transplantation (FMT), or engineered microbes—can restore ecological balance and exert therapeutic effects across diverse disease states [88] [89].
The mechanisms underlying these effects are increasingly elucidated. Gut bacteria produce a vast repertoire of metabolites, such as short-chain fatty acids (SCFAs), that serve as critical signaling molecules, regulating immune cell function, reinforcing intestinal barrier integrity, and modulating systemic inflammation [90] [91]. Dysbiosis, a state of microbial imbalance, disrupts these processes and is a hallmark of many chronic conditions [89]. This document provides a synthesized overview of the current state and future directions of microbiome-based interventions, framed as Application Notes and Protocols for researchers and drug development professionals working at the intersection of microbiology, immunology, and clinical medicine.
Microbiome in Disease Pathogenesis and Therapeutic Response
Key Mechanistic Pathways
The therapeutic potential of microbiome modulation is grounded in well-defined host-microbe interactions. The following pathways are central to its role in oncology, metabolic, and autoimmune diseases.
Quantitative Microbial Signatures Across Diseases
Dysbiosis manifests as quantifiable alterations in microbial abundance and diversity. The following table synthesizes key taxonomic shifts associated with disease states and therapeutic responses.
Table 1: Key Microbial Taxa and Metabolites in Disease and Therapeutic Response
| Disease Area | Associated Microbial Taxa/Metabolites | Direction of Change | Clinical Correlation |
|---|---|---|---|
| Oncology (Immunotherapy Response) | Bifidobacterium, Faecalibacterium, Akkermansia muciniphila | Increased | Enhanced response to Immune Checkpoint Inhibitors (ICIs) in melanoma, NSCLC [92] [93] |
| Ruminococcaceae, Lachnospiraceae | Increased | Favorable anti-PD-1 response in melanoma [92] | |
| Microbial Gene Richness | Increased | Predictive of weight loss response to GLP-1 analogues in obesity [72] | |
| Metabolic Disorders | Firmicutes/Bacteroidetes (F/B) Ratio | Increased | Marker for obesity and metabolic syndrome [89] |
| Akkermansia muciniphila, Bifidobacterium spp. | Decreased | Associated with insulin resistance and obesity [91] [89] | |
| Faecalibacterium prausnitzii (butyrate producer) | Decreased | Characteristic of Type 2 Diabetes [89] | |
| Short-Chain Fatty Acids (SCFAs) | Decreased | Linked to impaired gut barrier and inflammation [91] | |
| Autoimmune Diseases | Overall Microbial Diversity | Decreased | Consistent feature across rheumatoid arthritis, multiple sclerosis, and type 1 diabetes [90] |
| T-helper 17 (Th17) cells | Increased | Positively correlated with disease severity [90] |
Application Notes & Experimental Protocols
Application Note: Modulating Microbiome to Enhance Cancer Immunotherapy
Background: The efficacy of Immune Checkpoint Inhibitors (ICIs) is not universal, and the gut microbiome is a key determinant of response. Objective: To outline strategies for overcoming ICI resistance via microbiome modulation.
Key Findings:
- Fecal Microbiota Transplantation (FMT) from ICI responders can re-sensitize refractory melanoma to anti-PD-1 therapy [92].
- Dietary interventions, such as a high-fiber diet (30-50 g/day), are associated with a favorable ICI response in metastatic melanoma [72].
- Specific microbial metabolites, like SCFAs, are crucial for modulating host immune reactivity and enhancing dendritic cell function, which is critical for ICI efficacy [92] [93].
Considerations: The microbial signatures of response can vary by ICI type (anti-PD-1 vs. anti-CTLA-4) and cancer type, necessitating stratified approaches [92].
Protocol: Fecal Microbiota Transplantation (FMT) in Clinical Trials
Purpose: To standardize the procedure for FMT preparation and administration in clinical research settings, such as for improving ICI response or treating metabolic syndrome.
Materials:
- Donor Screening Kit: Comprehensive questionnaire and blood/stool tests for pathogens.
- Anaerobic Workstation: For processing samples under oxygen-free conditions.
- Cryoprotectant: Glycerol for preserving microbial viability.
- Delivery Capsules/Endoscope: For oral or lower GI tract administration.
Procedure:
- Donor Selection & Screening: Select healthy donors based on strict criteria (absence of metabolic, autoimmune, or infectious diseases). Screen stool for pathogens (C. difficile, ESBL, VRE, etc.), viruses, and parasites.
- Stool Processing:
- Weigh and homogenize fresh donor stool in sterile saline with cryoprotectant (e.g., 10% glycerol) under anaerobic conditions.
- Filter the slurry through coarse filters to remove particulate matter.
- Aliquot the filtrate for immediate use or freeze at -80°C.
- Recipient Preparation: For ICI trials, patients should have confirmed progressive disease on prior ICI. Administer a bowel preparation regimen if using lower GI delivery.
- FMT Administration:
- Route: Deliver via colonoscopy for maximal colonic engraftment or via oral, acid-resistant capsules.
- Dosage: A typical dose is 30-50 grams of stool per infusion.
- Post-Procedure Monitoring: Monitor for engraftment (via sequential stool metagenomics), adverse events, and clinical outcome (e.g., tumor response per RECIST criteria).
Application Note: Microbiome-Targeted Therapies for Metabolic Health
Background: Dysbiosis is a core feature of metabolic disorders, influencing energy harvest, insulin signaling, and chronic inflammation. Objective: To evaluate the efficacy of microbiome-targeted interventions.
Key Findings:
- Probiotics: Strains like Lactobacillus and Bifidobacterium can improve glycemic control and lipid profiles, partly by reducing inflammation in mesenteric adipose tissue [91] [89].
- Prebiotics & Diet: Fibers and Mediterranean diets promote microbial diversity and SCFA production. A low-emulsifier diet reduced symptoms and inflammation (fecal calprotectin) in active Crohn's disease [72].
- Postbiotics: These inanimate microbial products offer a stable, safe alternative to live probiotics, with demonstrated benefits for metabolic health [89].
Protocol: Designing a Synbiotic Intervention Study
Purpose: To provide a methodology for evaluating the combined effect of a probiotic and prebiotic (synbiotic) on a metabolic endpoint.
Materials:
- Probiotic Strains: e.g., Lactobacillus plantarum, Bifidobacterium longum (≥10⁹ CFU/dose).
- Prebiotic Substrate: e.g., Inulin, Fructooligosaccharides (FOS), Galactooligosaccharides (GOS).
- Placebo: Maltodextrin or microcrystalline cellulose.
- Blood Collection Tubes: Including EDTA tubes for plasma and serum separator tubes.
- Stool Collection Kits: With DNA/RNA stabilizer.
Procedure:
- Study Design: Randomized, double-blind, placebo-controlled trial. Arm 1: Synbiotic. Arm 2: Prebiotic only. Arm 3: Placebo.
- Intervention:
- Dosage: Typically 1-10 billion CFU of probiotic combined with 5-15g of prebiotic daily.
- Duration: Minimum 8-12 weeks.
- Baseline & Endpoint Assessment:
- Clinical: Body weight, BMI, blood pressure.
- Metabolic Biomarkers: Fasting glucose, HbA1c, lipid profile, inflammatory markers (CRP, IL-6).
- Microbiome Analysis: Collect stool samples for 16S rRNA or shotgun metagenomic sequencing and SCFA quantification via GC-MS.
- Statistical Analysis: Compare changes from baseline to endpoint between groups using appropriate tests (e.g., paired t-test, ANOVA for within- and between-group comparisons).
Application Note: Resetting Immune Tolerance in Autoimmunity
Background: Autoimmune diseases like rheumatoid arthritis and multiple sclerosis involve a loss of immune tolerance, which is heavily influenced by the microbiome. Objective: To explore microbiome modulation for abrogating autoimmune inflammation.
Key Findings:
- Dysbiosis can trigger systemic autoimmunity via mechanisms like mucosal immune modulation and antigenic mimicry [90].
- Microbiome composition affects the balance between pro-inflammatory T-helper 17 (Th17) cells and regulatory T-cells (Tregs) [90].
- Microbiome-based interventions, including probiotics and FMT, are emerging as a novel class of immunotherapy for autoimmune diseases, aiming to restore immune homeostasis [94].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful microbiome research requires a specialized set of tools for manipulation, analysis, and delivery.
Table 2: Key Research Reagent Solutions for Microbiome Studies
| Category | Item | Function/Application |
|---|---|---|
| Microbiome Modulators | Probiotics (e.g., Lactobacillus, Bifidobacterium strains) | Live biotherapeutics for direct microbial supplementation [88]. |
| Prebiotics (e.g., Inulin, FOS, GOS) | Selective substrates to nourish beneficial gut bacteria [88] [89]. | |
| Rationally Designed Consortia (e.g., SER-155) | Investigational, multi-strain therapeutics engineered to reduce specific risks like antibiotic-induced dysbiosis [72]. | |
| Analytical Tools | Metagenomic Sequencing Kits (16S rRNA, Shotgun) | Comprehensive profiling of microbial community structure and function [92] [87]. |
| Metabolomics Kits (e.g., for SCFA analysis via GC-MS/LC-MS) | Quantification of key microbiome-derived metabolites [91] [93]. | |
| ELISA Kits for Inflammatory Markers (CRP, IL-6, TNF-α) | Measuring host immune and inflammatory responses to intervention [91]. | |
| Delivery & Engineering | Anaerobic Culture Systems | For cultivating oxygen-sensitive gut microbes. |
| Cryopreservation Media (with Glycerol) | Long-term storage and viability maintenance of microbial strains or FMT material. | |
| Encapsulation Materials (Acid-Resistant Capsules) | Oral delivery platform to protect probiotics from gastric acidity. |
The horizon of microbiome modulation is expanding rapidly, moving from correlation to causation and therapeutic application. Future progress hinges on overcoming key challenges: the strain-specificity of effects, inter-individual variability in microbiome composition, and the need for standardized protocols and larger clinical trials [88] [87]. The field is moving towards personalized microbiota therapies, where multi-omics data will guide the selection of bespoke interventions [87]. Furthermore, the development of engineered microbial consortia and the refined use of postbiotics represent the next wave of precision microbiome-based therapeutics [89]. As research continues to unravel the complex dialogue between the microbiome and the host, its integration into standard care for oncology, metabolic, and autoimmune diseases promises to revolutionize patient outcomes.
The clinical translation of microbiome research has catalyzed the development of three distinct therapeutic classes: Fecal Microbiota Transplantation (FMT), Defined Microbial Consortia, and Engineered Live Biotherapeutic Products (eLBPs). These modalities represent a spectrum from ecological restoration to precision engineering, each with unique mechanisms, advantages, and challenges [95] [96]. FMT involves the transfer of entire microbial communities from a healthy donor to a recipient, representing the most holistic but least characterized approach [95]. Defined consortia are synthetic mixtures of specific, well-characterized bacterial strains designed to perform targeted functions with improved safety and reproducibility over FMT [97]. Engineered biotherapeutics represent the most precise approach, utilizing synthetic biology to genetically modify microbes for enhanced therapeutic functions, such as the production of therapeutic compounds or sensing of disease biomarkers [98] [52]. Understanding the comparative strengths, limitations, and appropriate applications of each modality is crucial for advancing microbiome-based treatments for gastrointestinal, metabolic, immune, and neurological disorders.
Comparative Analysis of Therapeutic Modalities
Table 1: Comparative Analysis of Key Microbiome Therapeutic Modalities
| Feature | Fecal Microbiota Transplantation (FMT) | Defined Microbial Consortia | Engineered Biotherapeutics |
|---|---|---|---|
| Definition | Transfer of entire microbial community from healthy donor stool [95] | Synthetic mixture of specific, characterized bacterial strains [97] | Genetically modified microbes with enhanced functions [98] [52] |
| Composition | Complex, undefined (thousands of taxa) [95] | Defined number of strains (typically 5-100+) [97] | Single or few engineered strains [96] [52] |
| Standardization | Low (donor-dependent) [95] | High (controlled manufacturing) [97] | Very High (clonal populations) [98] |
| Mechanism of Action | Ecological restoration, multi-factorial [95] | Targeted restoration of specific functions [97] | Precise, programmable action (e.g., metabolite production, pathogen sensing) [98] |
| Safety Profile | Risk of pathogen transmission, limited donor screening [95] [97] | Improved safety (strains from curated biobanks) [97] | Requires careful evaluation of GMO safety and genetic stability [52] |
| Regulatory Status | FDA enforcement discretion for rCDI; EU SoHO regulation [95] | Regulated as biologics/Live Biotherapeutic Products (LBPs) [97] [96] | Evolving regulatory pathway for genetically modified organisms [98] |
| Key Advantages | High efficacy in rCDI (>85-90%), holistic community approach [95] [96] | Reproducibility, safety, rational design [97] | Unlimited precision, novel functions beyond natural microbiology [98] |
| Major Limitations | Donor variability, pathogen risk, limited scalability [95] | Potential reduced efficacy vs. FMT, complex manufacturing [97] [96] | Host immune response to engineered components, public acceptance of GMOs [52] |
| Representative Products | Rebyota (RBX2660) [96] | VE303 (8 strains), VE202 [97] [96] | SYNB1934 (engineered E. coli Nissle for phenylketonuria) [39] |
Table 2: Clinical and Market Landscape Comparison (Data sourced from 2024-2025 reports)
| Parameter | Fecal Microbiota Transplantation (FMT) | Defined Microbial Consortia | Engineered Biotherapeutics |
|---|---|---|---|
| Market Size (2024) | $158.3 Million [99] | Part of LBP segment ($425M) [39] | Part of LBP segment [39] |
| Projected Market (2034) | $2.3 Billion [99] | $2.39 Billion (Full LBP segment) [39] | Growing segment of LBP market [39] |
| Approved Indications | rCDI (Rebyota) [96] | rCDI (Vowst) [96] | None approved; multiple in trials [39] |
| Clinical Efficacy (rCDI) | 85-95% (general FMT); 70.6% (Rebyota) [96] [99] | Relative risk reduction 0.32 vs. placebo (Vowst) [96] | N/A (Not yet approved for rCDI) |
| Pipeline Candidates | Limited, primarily for non-CDI indications [39] | >15 in Phase II/III for UC, hyperoxaluria, CKD [39] | Multiple in early phases for PKU, oncology, infections [39] |
| Manufacturing Cost | Moderate (donor screening and processing) [95] | High (fermentation, purification, blending) [97] | Very High (strain engineering, characterization) [98] |
Experimental Protocols for Development and Analysis
Protocol 1: FMT Donor Screening and Material Preparation
Objective: To standardize the screening of FMT donors and preparation of fecal material for clinical use or research, minimizing the risk of pathogen transmission [95] [97].
Materials:
- Healthy donor candidates
- Stool collection kit (anaerobic container, gloves, sealable bag)
- Cryopreservation solution (e.g., 10% glycerol in saline)
- Anaerobic chamber or workstation
- Laboratory blender
- Sterile filtration system (e.g., 0.22-500 µm sequential filters)
- Cryogenic vials
- -80°C freezer
Procedure:
- Donor Recruitment and Screening: Recruit healthy volunteers with no recent antibiotic use (≥2 months). Conduct extensive screening via questionnaire for medical history, travel, and lifestyle risks. Perform laboratory testing on blood and stool for pathogens including Clostridioides difficile, ESBL-producing organisms, SARS-CoV-2, and enteric pathogens [95] [97].
- Stool Collection and Processing: Collect fresh stool sample in an anaerobic container. Process within 6 hours of passage. Weigh stool and dilute 1:5 with cryopreservation solution in a laboratory blender under anaerobic conditions. Homogenize thoroughly until a consistent suspension is achieved [95].
- Filtration and Purification: Sequentially filter the homogenate through 500 µm and 0.22 µm filters to remove particulate matter and most viruses. Alternatively, for spore-rich products like SER-109, subject the homogenate to ethanol treatment to purify spores [96].
- Dosage Formulation and Storage: Aliquot the final filtrate into single-dose cryogenic vials. Store immediately at -80°C for long-term preservation. For use, thaw rapidly at room temperature or 37°C and administer within a short timeframe [95].
Protocol 2: Design and Validation of a Defined Microbial Consortium
Objective: To rationally design, construct, and validate a defined microbial consortium for a specific clinical indication, such as recurrent C. difficile infection (rCDI) or Inflammatory Bowel Disease (IBD) [97].
Materials:
- Bacterial strains from culture biobanks (e.g., ATCC, DSMZ)
- Anaerobic growth media (e.g., YCFA, GAM, M2GSC)
- Anaerobic chamber
- 96-well plates and spectrophotometer
- Gnotobiotic mouse models
- Metagenomic sequencing tools
- Mass spectrometer for metabolite analysis
Procedure:
- Strain Selection ("Bottom-Up" Design): Identify candidate strains via metagenomic analysis of healthy vs. diseased cohorts. Select strains based on: a) abundance in healthy donors, b) known beneficial functions (e.g., bile acid metabolism, SCFA production, immunomodulation), and c) compatibility (no antagonism). A typical starting point may include 8-20 strains from genera such as Clostridium clusters IV and XIVa, Bacteroides, and Bifidobacterium [97] [96].
- In Vitro Community Assembly and Testing: Cultivate individual strains in anaerobic media. Test for strain-strain interactions via cross-streaking and co-culture assays. Assemble the final consortium by combining strains at specific ratios based on their relative abundance in healthy human stool or functional optimization. Validate community stability in continuous culture bioreactors over 5-10 days [97].
- In Vivo Validation in Gnotobiotic Mice: Use germ-free or antibiotic-treated mice. Divide into groups: 1) Consortium monocolonization, 2) FMT control, 3) Untreated control. Orally administer the consortium and challenge with C. difficile spores or a chemical colitis inducer (e.g., DSS). Monitor for: a) colonization levels (qPCR, 16S sequencing), b) protection from disease (survival, weight loss, pathology), and c) mechanism of action (SCFA levels, host transcriptomics) [97].
- Manufacturing for Clinical Use: Scale up individual strain fermentation under cGMP conditions. Harvest, concentrate, and blend strains to the target ratio. Formulate into capsules with cryoprotectants or as lyophilized powder. Confirm viability, identity, and purity of each batch [97].
Protocol 3: Engineering a Probiotic for Targeted Therapeutic Delivery
Objective: To engineer a probiotic chassis (e.g., E. coli Nissle) to produce a therapeutic metabolite in response to a disease-specific signal [98] [52].
Materials:
- Probiotic chassis strain (e.g., E. coli Nissle 1917)
- Plasmids with inducible promoters/parts (e.g., tetR, lacI)
- CRISPR-Cas9 gene editing system
- Synthetic DNA fragments
- Microfluidic culturing devices
- HPLC/MS for metabolite quantification
- In vitro gut-on-a-chip model
- Animal disease models
Procedure:
- Circuit Design and Construction: Identify a disease-relevant trigger (e.g., inflammation marker tetrathionate, AHL for quorum sensing). Design a genetic circuit where a promoter sensing this trigger drives the expression of a therapeutic gene (e.g., IL-10, antioxidant enzymes, phenylalanine ammonia-lyase). Assemble the construct using Gibson assembly or Golden Gate cloning into a plasmid or the chromosome via CRISPR-Cas9 [98].
- In Vitro Characterization: Transform the engineered construct into the chassis strain. Characterize the dose-response of the circuit to the trigger molecule in microfluidic cultures. Quantify the dynamic range and sensitivity. Measure the production level of the therapeutic compound using ELISA or HPLC/MS. Test strain survival in simulated gut conditions [98].
- Functional Validation in Gut Models: Introduce the engineered probiotic into a gut-on-a-chip model containing human intestinal epithelial cells. Apply the disease trigger and measure: a) circuit activation, b) therapeutic output, and c) improvement in barrier integrity (TEER) or reduction in inflammatory cytokines (e.g., TNF-α, IL-6) [98].
- In Vivo Efficacy and Safety Testing: Administer the engineered probiotic to a rodent disease model (e.g., DSS colitis, PKU model). Monitor disease progression and therapeutic effect. At endpoint, analyze gut microbiota (to assess ecological impact), host tissues for toxicity, and blood for systemic metabolite levels. Confirm genetic stability of the engineered circuit by sequencing plasmids/chromosome from bacteria recovered from feces [98] [52].
Visualization of Signaling Pathways and Workflows
Microbiome-Host Signaling Pathways in Therapeutics
Therapeutic Modality Mechanisms: This diagram illustrates the primary mechanisms of action through which Fecal Microbiota Transplantation (FMT), Defined Consortia, and Engineered Biotherapeutics exert their effects on host physiology.
Defined Consortium Development Workflow
Consortium Development Pipeline: This workflow outlines the key stages in the rational design and development of a defined microbial consortium, from initial discovery to clinical application.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Microbiome Therapeutics
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Gnotobiotic Mouse Models | Provides sterile host for mono- or defined colonization to study causality and mechanism [97] | Validating colonization and efficacy of a defined consortium without background microbiota interference. |
| Anaerobic Growth Chambers | Maintains oxygen-free environment for cultivating obligate anaerobic gut bacteria [97] | Cultivating fastidious anaerobes like Faecalibacterium prausnitzii for inclusion in a consortium. |
| Genome-Scale Metabolic Models (GEMs) | Computational models predicting metabolic interactions and outputs of microbial communities [98] | In silico design of a consortium to optimize SCFA production and avoid cross-feeding conflicts. |
| CRISPR-Cas9 Systems | Precision genome editing for engineering bacterial chassis [98] [52] | Knocking in a therapeutic gene cassette into the chromosome of E. coli Nissle for stable expression. |
| Microfluidic Gut-on-a-Chip | In vitro model simulating human gut physiology, microbiome, and flow [98] | Testing the response of an engineered probiotic to inflammatory signals in a human-relevant system. |
| Metagenomic Sequencing | Comprehensive profiling of all genetic material in a sample for community analysis [95] [1] | Assessing engraftment of donor microbes post-FMT or tracking strain dynamics in a consortium. |
| Mass Spectrometry Metabolomics | Quantitative profiling of small molecule metabolites (e.g., SCFAs, bile acids) [1] | Measuring functional output of a therapeutic (e.g., butyrate levels) in response to treatment. |
The future of microbiome clinical translation lies in strategically applying the most appropriate therapeutic modality based on the clinical indication, mechanism of action, and required level of precision. While FMT remains a powerful ecological intervention for conditions like rCDI, its future role may be limited due to inherent variability and safety concerns [95]. Defined consortia offer a balanced approach, providing reproducible, multi-strain communities with rational design for a broadening range of indications from IBD to metabolic diseases [97] [96]. Engineered biotherapeutics represent the cutting edge, offering the potential for bespoke solutions for complex diseases and even personalized medicine, though they face the highest regulatory and technical hurdles [98] [52]. The successful integration of these therapies into clinical practice will depend on continued advances in synthetic biology, a deeper functional understanding of host-microbiome interactions, and the development of evolved regulatory frameworks that can accommodate these novel therapeutic paradigms.
The therapeutic and diagnostic potential of the human microbiome represents a frontier in clinical medicine, with implications for managing a broad range of gastrointestinal, metabolic, immune, and neurological diseases [1]. However, the rapid proliferation of commercial microbiome tests, often marketed directly to consumers, has outpaced the development of robust scientific evidence and regulatory frameworks [100] [101]. This gap between commercial availability and clinical validation poses risks, including misinterpretation of results, inappropriate clinical management, and erosion of public trust [102]. In response, an international multidisciplinary panel of 69 experts from 18 countries convened to establish the first comprehensive consensus on microbiome testing in clinical practice [100] [103]. This application note distills this consensus and complementary research to provide structured protocols and frameworks for researchers and drug development professionals working to translate microbiome science into validated clinical applications.
Table 1: Core Principles of the International Consensus on Microbiome Testing
| Principle Area | Key Recommendation | Clinical/Research Implication |
|---|---|---|
| General Principles | Tests must communicate limited evidence transparently [100]. | Manages patient and clinician expectations; frames testing as investigational. |
| Requires a multidisciplinary team for interpretation [100] [103]. | Involves clinicians, microbiologists, and bioinformaticians at all stages. | |
| Pre-Testing Protocols | Testing must be initiated by a licensed healthcare professional [101] [104]. | Discourages direct-to-consumer self-referral; ensures clinical rationale. |
| Comprehensive clinical metadata is mandatory [101]. | Essential for contextualizing results and controlling for confounders. | |
| Analysis Methods | Amplicon or whole-genome sequencing are required [101]. | Multiplex PCR and bacterial cultures are not sufficient for microbiome profiling. |
| Reporting Standards | Reports must include alpha and beta diversity and detailed taxonomy [101]. | Provides an ecological overview of the microbial community. |
| The Firmicutes/Bacteroidetes ratio should be excluded [103]. | This oversimplified metric lacks evidence for a causal relationship with health. | |
| Clinical Application | Post-testing therapeutic advice from the testing provider is discouraged [103]. | Clinical management is the responsibility of the referring healthcare provider. |
Consensus Framework: From Sample to Report
Pre-Analytical Standards and Metadata Collection
The consensus emphasizes that rigorous pre-analytical protocols are the foundation of reliable microbiome data. A licensed healthcare provider should prescribe testing based on a clear clinical indication, not patient self-referral [103] [104]. Prior to sample collection, extensive clinical metadata must be compiled to control for variables known to significantly influence microbiome composition [101].
Table 2: Essential Pre-Analytical Clinical Metadata
| Metadata Category | Specific Variables | Rationale |
|---|---|---|
| Patient Demographics | Age, Gender, Body Mass Index (BMI) [103] | Core determinants of baseline microbiome composition. |
| Health Status | Current and past diseases/conditions, Gastrointestinal symptoms [101] | Provides clinical context for interpreting dysbiosis. |
| Medication History | Current and past medications (especially antibiotics, PPIs) [101] | Drugs are major confounders of microbiome structure and function. |
| Dietary Information | Dietary patterns, Gut transit time [101] [103] | Diet is a primary driver of microbiome variation and function. |
| Lifestyle Factors | Smoking status, Alcohol consumption, Exercise frequency [101] | Lifestyle choices can modulate microbiome ecology. |
Stool collection should utilize a kit containing a DNA stabilizer or preservative to prevent microbial growth and genetic material degradation [103]. The consensus recommends that samples be frozen at -80°C in the laboratory and testing should be performed within a validated time frame to ensure analytical integrity [103].
Analytical Methods and Sequencing Protocols
The expert panel specifies that gut microbiome community profiling must use either amplicon sequencing (e.g., of the 16S rRNA gene) or shotgun whole-genome sequencing [101] [103]. While techniques like multiplex PCR or bacterial culture can identify specific pathogens, they cannot be used as a proxy for comprehensive microbiome analysis [101].
Protocol 1: 16S rRNA Gene Amplicon Sequencing
- DNA Extraction: Use a standardized, validated kit from a known manufacturer. The extraction method must be documented in the final report [101].
- PCR Amplification: Target hypervariable regions (e.g., V3-V4) of the 16S rRNA gene. Include positive and negative controls in every run to monitor for contamination and PCR efficacy.
- Sequencing: Perform on an Illumina MiSeq or similar platform to generate paired-end reads (e.g., 2x300 bp).
- Bioinformatic Analysis:
- Processing: Use QIIME 2 or mothur for demultiplexing, quality filtering (based on Phred score), and merging of paired-end reads.
- Clustering: Cluster high-quality sequences into Amplicon Sequence Variants (ASVs) using DADA2 or Deblur to achieve high resolution.
- Taxonomy Assignment: Assign taxonomy against a reference database (e.g., SILVA, Greengenes) using a trained classifier.
Protocol 2: Shotgun Metagenomic Sequencing
- DNA Extraction & Library Preparation: Extract high-quality, high-molecular-weight DNA. Prepare sequencing libraries using a kit compatible with your platform (e.g., Illumina Nextera). The input DNA quantity and quality should be verified.
- Sequencing: Perform on an Illumina NovaSeq or similar platform to achieve sufficient depth (e.g., 10-20 million reads per sample).
- Bioinformatic Analysis:
- Quality Control: Use FastQC for initial quality assessment and Trimmomatic to remove adapters and low-quality reads.
- Host Read Depletion: Align reads to a human reference genome (e.g., hg38) using Bowtie2 and remove matching sequences.
- Microbial Profiling:
- Taxonomic: Use MetaPhlAn for precise species-level profiling.
- Functional: Use HUMAnN 3.0 to quantify gene families and metabolic pathways from the UniRef and MetaCyc databases.
Reporting and Interpretation Guidelines
The consensus provides strict guidance on the content of microbiome test reports to ensure clarity and utility while preventing misinterpretation [101] [103].
Report Content Checklist:
- Patient medical history and relevant clinical metadata.
- Detailed test protocol (sample collection, storage, DNA extraction, sequencing method, bioinformatic tools).
- Ecological measures: Alpha diversity (e.g., Shannon, Chao1 indices) and Beta diversity (e.g., PCoA plots with UniFrac distance).
- Complete taxonomic profiling at the deepest possible resolution (species level for shotgun metagenomics).
- Comparison to a matched healthy control group to contextualize findings.
Content to Exclude:
- The Firmicutes/Bacteroidetes ratio and other oversimplified "dysbiosis indices" due to a lack of validation and clinical utility [103] [104].
- Direct post-testing therapeutic advice from the testing provider. Clinical decision-making is the sole responsibility of the referring healthcare professional [103].
Diagram 1: Microbiome testing workflow.
Advanced Translational Applications and Protocols
Integrating Multi-Omics for Mechanistic Insights
While sequencing is foundational, the consensus and contemporary reviews highlight that clinical translation requires moving beyond correlation to causation through multi-omics integration [1] [105]. This approach provides a systems-level understanding of host-microbe interactions.
Protocol 3: A Multi-Omics Integration Workflow
- Objective: To identify functional mechanistic links between the microbiome and host physiology.
- Experimental Steps:
- Metagenomics: As described in Protocol 2, define the genetic potential of the microbiome.
- Metatranscriptomics:
- RNA Extraction: Extract total RNA from stool samples, ensuring removal of DNA.
- Library Prep: Deplete ribosomal RNA, then prepare strand-specific RNA-seq libraries.
- Analysis: Map sequences to a gene catalog to quantify expression levels of microbial genes, revealing active pathways.
- Metaproteomics:
- Protein Extraction & Prep: Lyse microbial cells, digest proteins with trypsin, and label with TMT or iTRAQ reagents for multiplexing.
- LC-MS/MS: Analyze peptides using liquid chromatography coupled with tandem mass spectrometry.
- Analysis: Identify and quantify proteins by searching spectra against a protein database derived from metagenomic data.
- Metabolomics:
- Sample Prep: Extract metabolites from stool or blood plasma using methanol/water or chloroform/methanol.
- Analysis: Use NMR or LC-MS to profile the metabolome.
- Integration: Correlate metabolite abundances with microbial gene and protein abundances to connect microbial activity to host-relevant molecules (e.g., SCFAs, bile acids).
Diagram 2: Multi-omics to mechanism pipeline.
Microbiome-Based Therapeutic Monitoring
Microbiome testing shows promise for monitoring the efficacy of interventions like fecal microbiota transplantation (FMT), probiotics, and phage therapy [100] [72]. The key is longitudinal sampling and focused analysis.
Protocol 4: Monitoring FMT Engraftment
- Objective: To assess the engraftment of donor microbiota in a recipient post-FMT.
- Pre-FMT Baseline: Collect stool from both donor and recipient for metagenomic sequencing.
- Post-FMT Sampling: Collect recipient stool samples at regular intervals (e.g., days 1, 7, 30, 90).
- Analysis:
- Strain-Level Tracking: Use tools like StrainPhlAn or metaSNV to track the transmission of specific donor bacterial strains in the recipient.
- Ecological Shift: Calculate beta-diversity distances (e.g., Bray-Curtis) between all recipient time points and the donor baseline. Successful engraftment is indicated by a sustained shift in the recipient's microbiome profile toward the donor's profile.
- Functional Engraftment: Use HUMAnN 3.0 to compare metabolic pathway abundances pre- and post-FMT, assessing functional convergence with the donor.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Microbiome Testing
| Item | Function/Description | Example Kits/Tools |
|---|---|---|
| Stool DNA Preservation Kit | Stabilizes microbial DNA/RNA at room temperature for transport, preventing shifts in composition. | OMNIgene•GUT, Zymo Research DNA/RNA Shield |
| High-Yield DNA Extraction Kit | Efficiently lyses diverse microbial cell walls (Gram+, Gram-, spores) for representative DNA extraction. | QIAamp PowerFecal Pro DNA Kit, MagMAX Microbiome Ultra Kit |
| 16S rRNA PCR Primers | Amplify hypervariable regions for amplicon sequencing (e.g., V4: 515F/806R). | Illumina 16S Metagenomic Sequencing Library Prep reference |
| Shotgun Metagenomic Library Prep Kit | Prepares sequencing libraries from fragmented metagenomic DNA for whole-genome sequencing. | Illumina DNA Prep, Nextera XT DNA Library Prep Kit |
| Bioinformatic Pipelines | Software for processing raw sequencing data into taxonomic and functional profiles. | QIIME 2 (16S), HUMAnN 3.0 (shotgun), MetaPhlAn (shotgun) |
| Healthy Reference Database | Curated collection of metagenomes from healthy individuals for comparative analysis. | The Human Microbiome Project (HMP) database, curated in-house cohorts |
The international consensus provides an indispensable framework for standardizing microbiome testing, emphasizing rigorous methodology, clinical context, and transparent reporting [100] [103]. For researchers and drug developers, this framework is a roadmap for building a robust evidence base. The future of microbiome-based diagnostics and therapeutics lies in embracing these standards, advancing multi-omics integration to establish causality, and conducting well-designed clinical trials that address specific clinical needs [1] [22] [105]. By adhering to this consensus, the field can move beyond descriptive associations and reliably translate the promise of the microbiome into effective clinical applications.
The human microbiome has undergone a profound paradigm shift, from being considered a passive passenger to being recognized as a dynamic organ that actively shapes human physiology, immunity, metabolism, and therapeutic responses [1]. This recognition positions microbiome science at the forefront of a fundamental transformation in medicine, driving the development of novel diagnostics, therapeutics, and preventive strategies. The clinical translation of microbiome research is now redefining early-life programming, cardiometabolic regulation, immune homeostasis, neuropsychiatric resilience, and cancer therapy response [1]. The convergence of multi-omic technologies, advanced computational approaches, and mechanistic insights has created a fertile ground for innovation, propelling the field toward an anticipated $5.1 billion market valuation by 2030 [106]. This growth trajectory reflects the expanding scope of microbiome-based applications across diverse clinical domains, from gastroenterology to oncology, psychiatry, and reproductive health. This document provides application notes and experimental protocols to support researchers and drug development professionals in navigating this rapidly evolving landscape, with a specific focus on validating microbial biomarkers and developing targeted therapeutic interventions.
Quantitative Market Landscape
The cellular Internet of Things (IoT) market, which encompasses connected devices for health monitoring and data collection, is projected to reach 5.1 billion connections by 2030, with a significant portion of this growth driven by healthcare and medical research applications [106]. This infrastructure expansion will facilitate large-scale microbiome studies and personalized medicine approaches. The table below summarizes key regional and technological drivers of this growth.
Table 1: Key Market Drivers and Regional Analysis
| Factor | Impact & Relevance | Geographic Concentration |
|---|---|---|
| 5G RedCap Technology | Ideal mid-tier connectivity for medical devices not requiring premium specs; provides essential futureproofing [106] | Global, with accelerating adoption from 2025 onward [106] |
| Regional Market Leadership | Contributes over 67% of global IoT module shipments and 80% of total IoT connections [106] | Asia & Oceania region [106] |
| Automotive Industry Catalyst | Rising consumer demand for intelligent vehicles with integrated 5G connectivity features [106] | Global, with strong influence in Asia & Oceania [106] |
The Asia & Oceania region's dominance, contributing approximately 80% of total IoT connections in 2024, underscores a significant shift in global technology leadership that will shape IoT deployment strategies for years to come [106]. This connectivity backbone is essential for the data-intensive nature of modern microbiome research and its clinical applications.
Application Notes: Key Research Themes and Findings
Microbiome-Targeting Therapies in Neonatology
The administration of probiotics to preterm, low-birth-weight infants represents one of the most successful examples of microbiome clinical translation. Network meta-analyses of randomized controlled trials (RCTs) demonstrate that specific probiotic formulations significantly reduce the risk of severe necrotizing enterocolitis (NEC) and all-cause mortality [46].
- Most Effective Interventions: Combinations of one or more Lactobacillus spp. and one or more Bifidobacterium spp. show the most consistent benefits, reducing the incidence of severe NEC (Odds Ratio, 0.35; 95% CI, 0.20–0.59) and all-cause mortality (OR, 0.56; 95% CI, 0.39–0.80) based on moderate- to high-quality evidence [46].
- Population Considerations: The risk-benefit ratio is less favorable for extremely low-birth-weight (<1,000 g) neonates, where probiotics may have little or no effect on NEC or mortality [46].
- Clinical Guideline Status: Despite strong evidence, routine probiotic administration in US neonatal intensive care units (NICUs) has decreased to 29–39% due to concerns regarding product quality, heterogeneity of clinical data, and potential risks in vulnerable populations [46].
Diet and Nutritional Interventions
Diet is a primary driver of gut microbiome composition and function, offering a powerful lever for clinical intervention.
- Emulsifiers: A clinical trial (the ADDapt trial) demonstrated that a low-emulsifier diet is a safe and effective intervention for mild-to-moderately active Crohn's disease, reducing clinical symptoms and fecal calprotectin [72].
- Fermented Foods: Human studies, primarily on fermented dairy, indicate that fermented foods can improve digestive health. Research on fermented cabbage shows it can affect intestinal barrier function, with effects varying based on fermentation time, probiotic inoculants, and production methodology [72].
- Prebiotic Fibers: Not all fibers impact the host similarly. Mouse studies reveal that the benefits of fiber-rich foods are not fully recapitulated by supplemental fiber. Diets enriched with inulin induced hepatocellular carcinoma in 10% of mice, whereas psyllium and wheat bran showed beneficial effects on the microbiota and obesity [72].
- Personalized Nutrition: An individual's gut microbiome can determine the efficacy of nutritional interventions. For example, women whose gut microbiota can convert soy isoflavones to equol experience a 75% greater reduction in menopausal symptoms when supplemented with isoflavones compared to those who lack these microbial species [60].
Gut-Brain Axis and Neuropsychiatry
State-of-the-art bioinformatics applied to large population cohorts have strengthened the link between microbial disturbances and conditions like depression and quality of life. Researchers have identified and clustered biochemical pathways into 56 different Gut-Brain Modules (GBMs), each corresponding to a process for producing or degrading a single neuroactive compound [60]. This systems-level approach provides a mechanistic framework for developing microbiome-based diagnostics and therapeutics for neuropsychiatric conditions.
Microbiome in Cancer Therapy
The gut microbiome significantly influences cancer treatment outcomes, particularly immunotherapy.
- Dietary Modulation: The Be GONE Trial found that adding navy beans to the usual diet of patients with obesity and a history of colorectal cancer favorably modulated the gut microbiome [72].
- Fiber Intake and Immunotherapy: Unpublished data from the Prebiotic Food Enriched Diet (PreFED) trial showed that a high-fiber diet (30-50 g/d) was associated with a favorable immune checkpoint blockade response in patients with metastatic melanoma [72].
- Mitigating Antibiotic Dysbiosis: In patients undergoing allogeneic hematopoietic cell transplantation, low fecal microbiome diversity was strongly associated with intake of foods rich in simple sugars. Dietary sucrose exacerbated antibiotic-induced Enterococcus expansion, suggesting that avoiding sugar during antibiotic courses can help mitigate dysbiosis [72].
Experimental Protocols
Protocol: Multi-Strain Probiotic Efficacy Testing in Preterm Infants
Objective: To evaluate the efficacy of a specific multi-strain probiotic formulation in reducing the incidence of severe Necrotizing Enterocolitis (NEC) (Bell's stage II or III) and all-cause mortality in preterm infants (birth weight < 1500 g) [46].
Materials:
- Research Reagent Solutions:
- Probiotic Formulation: Lyophilized powder containing Lactobacillus acidophilus (1 x 10^9 CFU), Bifidobacterium infantis (1 x 10^9 CFU), and Streptococcus thermophilus (1 x 10^9 CFU) [46].
- Placebo: Maltodextrin powder identical in appearance and packaging.
- Sterile Diluent: Phosphate-buffered saline (PBS) for reconstitution.
Procedure:
- Randomization & Blinding: Randomize eligible infants to receive either probiotic or placebo within 72 hours of birth. Ensure allocation concealment and double-blinding of investigators, clinicians, and outcome assessors.
- Intervention Administration:
- Reconstitute the assigned powder (probiotic or placebo) in 2 mL of sterile PBS.
- Administer the suspension via orogastric tube once daily until the infant reaches 34 weeks postmenstrual age or is discharged.
- Outcome Monitoring:
- Monitor daily for clinical signs of NEC (feeding intolerance, abdominal distension, bloody stools).
- If NEC is suspected, obtain abdominal radiographs to identify pneumatosis intestinalis or portal venous gas.
- Record all-cause mortality until discharge.
- Data Analysis:
- Analyze data on an intention-to-treat basis.
- Calculate Odds Ratios (OR) with 95% Confidence Intervals (CI) for the outcomes of severe NEC and all-cause mortality.
Protocol: Assessing Low-Emulsifier Diet in Crohn's Disease
Objective: To determine the clinical and inflammatory response to a low-emulsifier dietary intervention in adults with mild-to-moderately active Crohn's disease [72].
Materials:
- Research Reagent Solutions:
- Food Frequency Questionnaire (FFQ): Customized to quantify intake of common emulsifiers (carboxymethylcellulose, polysorbate-80, carrageenan, lecithins, mono-/diglycerides).
- Dietary Counseling Materials: Structured educational resources and meal plans for a low-emulsifier diet.
- Inflammation Biomarker Kit: Fecal calprotectin ELISA kit.
Procedure:
- Baseline Assessment:
- Record patient demographics, disease activity (using Crohn's Disease Activity Index, CDAI), and current medication.
- Collect stool sample for baseline fecal calprotectin measurement.
- Administer FFQ to establish baseline emulsifier intake.
- Dietary Intervention:
- Provide individualized dietary counseling to eliminate major dietary sources of synthetic emulsifiers.
- Schedule bi-weekly follow-up calls for 8 weeks to support dietary adherence and troubleshoot challenges.
- Outcome Measurement:
- At week 8, reassess CDAI and collect a second stool sample for fecal calprotectin.
- Re-administer the FFQ to quantify changes in emulsifier intake.
- Data Analysis:
- Use paired t-tests (or Wilcoxon signed-rank tests for non-parametric data) to compare changes in CDAI and fecal calprotectin from baseline to week 8.
Protocol: Phage Therapy for Targeted Bacterial Reduction
Objective: To assess the efficacy of a bacteriophage cocktail in reducing the load of a specific bacterial pathobiont (e.g., Escherichia coli) in a clinical setting [72].
Materials:
- Research Reagent Solutions:
- Bacteriophage Cocktail: Purified, sterile-filtered lytic phage preparation (≥10^9 PFU/mL) targeting the specific bacterial strain.
- Placebo: Phage storage buffer (SM Buffer).
- qPCR Kit: For quantitative detection of the target bacterial species in stool samples.
Procedure:
- Screening & Enrollment: Identify patients colonized with the target bacterial strain via baseline stool qPCR.
- Randomization & Dosing: Randomize eligible patients to receive either the phage cocktail or an identical-looking placebo, administered orally twice daily for 7-14 days.
- Sample Collection: Collect stool samples at baseline, end-of-treatment, and at follow-up time points (e.g., 4 weeks post-treatment).
- Microbial Analysis:
- Extract total DNA from all stool samples.
- Perform qPCR with primers specific to the target bacterial species to quantify the bacterial load.
- Outcome & Safety:
- The primary outcome is the change in target bacterial load from baseline to end-of-treatment.
- Monitor and record all adverse events throughout the study period.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Microbiome Clinical Translation Research
| Reagent / Material | Function & Application | Example Use Case |
|---|---|---|
| Multi-Strain Probiotics | Live microbial supplements to restore a healthy microbial community and confer specific health benefits. | Prevention of necrotizing enterocolitis in preterm infants [46]. |
| Defined Synbiotics | Combinations of probiotics and prebiotics designed to improve survival and engraftment of beneficial microbes. | Sepsis and mortality reduction in full-term and late-preterm newborns in resource-constrained settings [46]. |
| Bacteriophage Cocktails | Lytic viruses that specifically target and lyse bacterial pathogens with high precision. | Reduction of multidrug-resistant E. coli load in hematological cancer patients; treatment of alcoholic hepatitis [72]. |
| Fecal Calprotectin ELISA Kit | Quantifies a protein biomarker in stool that correlates with neutrophil infiltration in the gut, a sign of intestinal inflammation. | Objective measurement of inflammatory response to a low-emulsifier diet in Crohn's disease patients [72]. |
| qPCR Assays for Specific Bacteria | Enables precise, quantitative tracking of specific bacterial taxa of interest in complex microbial communities. | Monitoring the reduction of a target pathobiont during and after phage therapy [72]. |
| SER-155 (Investigational) | A rationally designed, orally administered consortium of 16 bacterial Firmicutes strains. | Prevention of antibiotic-induced dysbiosis and bloodstream infections in adults undergoing allo-HCT [72]. |
The trajectory toward a $5.1 billion industry by 2030 is underpinned by tangible scientific advances and a growing pipeline of microbiome-based diagnostic and therapeutic applications. The protocols and application notes detailed herein provide a framework for validating microbial biomarkers and interventions with rigor and reproducibility. Future progress hinges on overcoming key challenges, including high interindividual variability, incomplete functional annotation of microbial "dark matter," and the establishment of standardized, validated biomarkers [1]. As the field moves from descriptive association to mechanistic understanding and interventional design, the integration of microbiome science into clinical practice promises to redefine the future of personalized and predictive medicine.
Conclusion
The clinical translation of microbiome research represents a paradigm shift in medicine, moving from associative observations to mechanism-based interventions with significant therapeutic potential. The approval of the first microbiome-based drugs and a robust pipeline of over 180 candidates underscore this progress. However, the full integration of microbiome science into routine clinical care hinges on overcoming key challenges: standardizing methodologies, validating biomarkers across diverse populations, designing conclusive clinical trials, and educating clinicians. Future success will depend on sustained collaboration between academia and industry to transform the promise of the microbiome into a reality for precision medicine, ultimately enabling more personalized and effective diagnostics and therapeutics for a wide range of diseases.
References
- 1. The human microbiome in clinical translation: from bench to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479421/]
- 2. Microbiome–metabolome dynamics associated with ... [https://www.nature.com/articles/s41591-025-03642-6]
- 3. Decoding the diagnostic and therapeutic potential of ... [https://www.nature.com/articles/s41467-024-52598-7]
- 4. Diagnostic and therapeutic potential roles of gut microbiome [https://www.gutmicrobiotaforhealth.com/unlocking-the-diagnostic-and-therapeutic-potential-roles-of-gut-microbiome-takeaways-from-the-2024-gmfh-summit/]
- 5. Deep learning in microbiome analysis: a comprehensive ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1516667/full]
- 6. iNAP: An integrated network analysis pipeline for microbiome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10989900/]
- 7. Reporting guidelines for Human Microbiome Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC9105086/]
- 8. Interaction between microbiota and immunity in health and ... [https://www.nature.com/articles/s41422-020-0332-7]
- 9. Metabolism at the centre of the host–microbe relationship - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6642865/]
- 10. Drug-microbiota interactions: an emerging priority for ... [https://www.nature.com/articles/s41392-023-01619-w]
- 11. Microbiota–gut–brain axis and its therapeutic applications ... [https://www.nature.com/articles/s41392-024-01743-1]
- 12. Microbiome therapeutics: exploring the present scenario and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8972995/]
- 13. Understanding the host-microbe interactions using metabolic ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-020-00955-1]
- 14. Microbiome at the Frontier of Personalized Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5730337/]
- 15. The Microbiota‐Gut‐Brain Connection: A New Horizon in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411739/]
- 16. Gut Microbial Dysbiosis in the Pathogenesis ... [https://www.jnmjournal.org/journal/view.html?doi=10.5056/jnm20149]
- 17. Clinical translation of microbiome research [https://pubmed.ncbi.nlm.nih.gov/40217076/]
- 18. Perturbations in gut microbiota composition in patients with ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1513599/full]
- 19. The role of gut microbiota dysbiosis in drug-induced brain injury [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395749/]
- 20. A comprehensive review on immunological mechanisms ... [https://link.springer.com/article/10.1007/s44337-025-00495-3]
- 21. decoding the gut–immune–brain axis in health and disease [https://www.nature.com/articles/s41423-025-01333-3]
- 22. Experts chart path to bring microbiome science into routine ... [https://www.news-medical.net/news/20250602/Experts-chart-path-to-bring-microbiome-science-into-routine-clinical-care.aspx]
- 23. Early-life gut microbiome development and its potential long ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12367470/]
- 24. Maternal–to–neonatal microbial transmission and impact of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07293-6]
- 25. Early life microbial succession in the gut follows common ... [https://www.nature.com/articles/s41467-025-56072-w]
- 26. A model of early-life interactions between the gut microbiome ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003263]
- 27. Gut Microbiota and Neurodevelopment in Preterm Infants [https://www.mdpi.com/2076-2607/13/9/2213]
- 28. Early-life gut microbiome and stress-axis perturbations ... [https://www.sciencedirect.com/science/article/pii/S3051172025000027]
- 29. Fecal microbiota transplantation: Current evidence and ... [https://www.ccjm.org/content/92/7/421]
- 30. What are the approved indications for Rebyota? [https://synapse.patsnap.com/article/what-are-the-approved-indications-for-rebyota]
- 31. Ferring Presents New Data Analyses for REBYOTA® (fecal ... [https://ferringusa.com/?press=ferring-presents-new-data-analyses-for-rebyota-fecal-microbiota-live-jslm-at-acg-2025]
- 32. REBYOTA® (fecal microbiota, live-jslm) for Recurrent C. diff ... [https://www.rebyotahcp.com/]
- 33. FDA Approves First Orally Administered Fecal Microbiota ... [https://www.fda.gov/news-events/press-announcements/fda-approves-first-orally-administered-fecal-microbiota-product-prevention-recurrence-clostridioides]
- 34. Mechanism of Action, Engraftment Data & Manufacturing [https://www.vowsthcp.com/moa]
- 35. What are the approved indications for VOWST? [https://synapse.patsnap.com/article/what-are-the-approved-indications-for-vowst]
- 36. New treatment for recurrence of C. difficile infection ... [https://health.ucdavis.edu/news/headlines/new-treatment-for-recurrence-of-c-difficile-infection-approved-by-fda/2023/05]
- 37. Ferring Presents New Real-World REBYOTA® (fecal ... [https://ferringusa.com/?press=ferring-presents-new-real-world-rebyota-fecal-microbiota-live-jslm-data-underscoring-effectiveness-and-significant-improvements-in-patient-quality-of-life]
- 38. Safety and Efficacy of Fecal Microbiota, Live-jslm ... [https://pubmed.ncbi.nlm.nih.gov/39862395/]
- 39. Human Microbiome Market & Therapeutic Pipeline 2025 [https://www.strategicmarketresearch.com/blogs/human-microbiome-market-clinical-trials-pipeline]
- 40. Genome-scale metabolic model-guided systematic framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12234829/]
- 41. Microbiome highlights from Digestive Disease Week 2025 [https://www.gutmicrobiotaforhealth.com/microbiome-highlights-from-digestive-disease-week-2025/]
- 42. Live Biotherapeutic Products: Development, Investment, and ... [https://www.alacrita.com/whitepapers/live-biotherapeutic-products-landscape-analysis?hs_amp=true]
- 43. Microbiome CDMO & Live Biotherapeutic Manufacturing ... [https://listlabs.com/microbiome-lbp/]
- 44. Personalized inhaled bacteriophage therapy for treatment ... [https://www.nature.com/articles/s41591-025-03678-8]
- 45. Therapeutic engineering of the gut microbiome using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12328466/]
- 46. Present and future of microbiome-targeting therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12126222/]
- 47. 11 microbiome biotech companies to watch in 2025 [https://www.labiotech.eu/best-biotech/microbiome-biotech-companies/]
- 48. Phage therapy as a revitalized weapon for treating clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540056/]
- 49. Phage Therapy Analysis 2025 and Forecasts 2033 [https://www.datainsightsmarket.com/reports/phage-therapy-1473695]
- 50. Recent insights on challenges encountered with phage ... [https://gutpathogens.biomedcentral.com/articles/10.1186/s13099-025-00735-y]
- 51. Microbiome engineering: unlocking therapeutic potential in ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1610029/full]
- 52. Gut microbiome engineering with probiotics: current trends ... [https://link.springer.com/article/10.1007/s42452-025-07622-w]
- 53. The human microbiome in clinical translation: from bench ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1632435/full]
- 54. Tools for Analysis of the Microbiome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7598837/]
- 55. A quantitative sequencing framework for absolute ... [https://www.nature.com/articles/s41467-020-16224-6]
- 56. Precision nutrition and nutrients: making the promise a reality [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1553149/full]
- 57. Targeting the Gut Microbiota's Role in Host Energy Absorption ... [https://pubmed.ncbi.nlm.nih.gov/40233201/]
- 58. The Role of the Gut Microbiome in Predicting Response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6855943/]
- 59. Precision nutrition for obesity management: A gut ... [https://www.sciencedirect.com/science/article/abs/pii/S0899900725002102]
- 60. Nutrition & microbiome research highlights NeuroGASTRO ... [https://www.gutmicrobiotaforhealth.com/nutrition-and-microbiome-research-highlights-from-neurogastro-2025/]
- 61. The Roles of Diet, Gut Microbiome and Microbial ... [https://www.mdpi.com/journal/metabolites/special_issues/7QAFQCH85S]
- 62. Precision Nutrition Forum and PREDIMED Omics Symposium ... [https://hsph.harvard.edu/nutrition/events/precision-nutrition-forum-and-predimed-omics-symposium/]
- 63. challenges in translating microbiome research to clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550608/]
- 64. Connecting precision nutrition with the Food is Medicine ... [https://www.sciencedirect.com/science/article/abs/pii/S1043276024002510]
- 65. Systems biology and microbiome innovations for ... [https://www.nature.com/articles/s41540-025-00607-w]
- 66. Study Designs and Statistical Analyses for Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3444086/]
- 67. A systematic framework for understanding the microbiome ... [https://www.nature.com/articles/s41392-024-01946-6]
- 68. Designing Effective Clinical Trials for Microbiome-Based ... [https://www.sgs.com/en-ge/news/2025/01/designing-effective-clinical-trials-for-microbiome-based-products]
- 69. Not quite a cure yet: unlocking the unfulfilled promise of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626851/]
- 70. Gut microbiome metagenomics in clinical practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562794/]
- 71. Human Microbiome Research Report 2025: Market ... [https://finance.yahoo.com/news/human-microbiome-research-report-2025-093500315.html]
- 72. takeaways from the 2025 GMFH Summit [https://www.gutmicrobiotaforhealth.com/clinical-translation-of-microbiome-research-takeaways-from-the-2025-gmfh-summit/]
- 73. The regulatory framework for microbiome-based therapies: insights into European regulatory developments | npj Biofilms and Microbiomes [https://www.nature.com/articles/s41522-025-00683-0]
- 74. Frontiers | Navigating regulatory and analytical challenges in live biotherapeutic product development and manufacturing [https://www.frontiersin.org/journals/microbiomes/articles/10.3389/frmbi.2024.1441290/full]
- 75. New Article:2025 Guidelines for Developing Live ... [https://microbiome.org.au/new-article2025-guidelines-for-developing-live-biotherapeutic-products/]
- 76. Microbiome Therapeutic Market Size, Share and Forecast 2035 [https://www.factmr.com/report/microbiome-therapeutics-market]
- 77. UNC researchers launch Interdisciplinary Microbiome ... [https://tracs.unc.edu/index.php/news-articles/2109-unc-researchers-launch-interdisciplinary-microbiome-research-program]
- 78. Current Capabilities of Gut Microbiome–Based Diagnostics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8206793/]
- 79. Microbiome confounders and quantitative profiling ... [https://www.nature.com/articles/s41591-024-02963-2]
- 80. Gut microbiome therapy: fecal microbiota transplantation vs ... [https://pubmed.ncbi.nlm.nih.gov/39377231/]
- 81. Fecal microbiota transplantation across the lifespan [https://pmc.ncbi.nlm.nih.gov/articles/PMC9992015/]
- 82. Fecal Microbiota Transplantation and Health Outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC9271871/]
- 83. The Efficacy of Probiotics, Prebiotics, Synbiotics, and Fecal ... [https://pubmed.ncbi.nlm.nih.gov/38999862/]
- 84. Review Fecal microbiota transplantation in clinical practice [https://www.sciencedirect.com/science/article/pii/S2949928324000087]
- 85. The probiotic enhances donor microbiota stability and ... [https://www.sciencedirect.com/science/article/pii/S2090123225001778]
- 86. A pharmacovigilance study on probiotic preparations based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106448/]
- 87. Clinical translation of microbiome research [https://www.nature.com/articles/s41591-025-03615-9]
- 88. Microbial Therapeutics in Cancer: Translating Probiotics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551701/]
- 89. Microbiome-based therapeutics for metabolic disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613280/]
- 90. The role of gut microbiota in autoimmune disease ... [https://www.frontiersin.org/journals/microbiomes/articles/10.3389/frmbi.2025.1553243/full]
- 91. Therapeutic Potential Targeting Gut Microbiota Modulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602043/]
- 92. Gut microbiota shapes cancer immunotherapy responses [https://www.nature.com/articles/s41522-025-00786-8]
- 93. Gut microbiota and metabolites: emerging prospects in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627001/]
- 94. Innovations in immunotherapy for autoimmune diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485509/]
- 95. The challenges and opportunities in the expanding horizons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584655/]
- 96. The Future of Microbiome Therapeutics - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11802617/]
- 97. Design and application of synthetic human gut microbial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12622336/]
- 98. Synthetic biology approaches for restoring gut microbial ... [https://www.sciencedirect.com/science/article/abs/pii/S0882401025006564]
- 99. Microbiome Therapeutics Market Size [https://www.gminsights.com/industry-analysis/microbiome-therapeutics-market]
- 100. International consensus statement on microbiome testing in ... [https://pubmed.ncbi.nlm.nih.gov/39647502/]
- 101. International consensus statement on microbiome testing ... [https://www.sciencedirect.com/science/article/abs/pii/S246812532400311X]
- 102. International Researchers Draft Consensus Document That ... [https://www.darkdaily.com/?p=51012]
- 103. International consensus on microbiome testing in clinical ... [https://www.gutmicrobiotaforhealth.com/new-international-consensus-on-microbiome-testing-in-clinical-practice/]
- 104. Clinical context over quick fix: the fresh consensus on ... [https://www.biocodexmicrobiotainstitute.com/en/pro/clinical-context-over-quick-fix-fresh-consensus-microbiome-testing]
- 105. From big data and experimental models to clinical trials [https://www.sciencedirect.com/science/article/pii/S0092867425001072]
- 106. Omdia forecasts cellular IoT connections to reach 5.1 billion ... [https://omdia.tech.informa.com/pr/2025/jul/omdia-forecasts-cellular-iot-connections-to-reach-5point1-billion-by-2030]