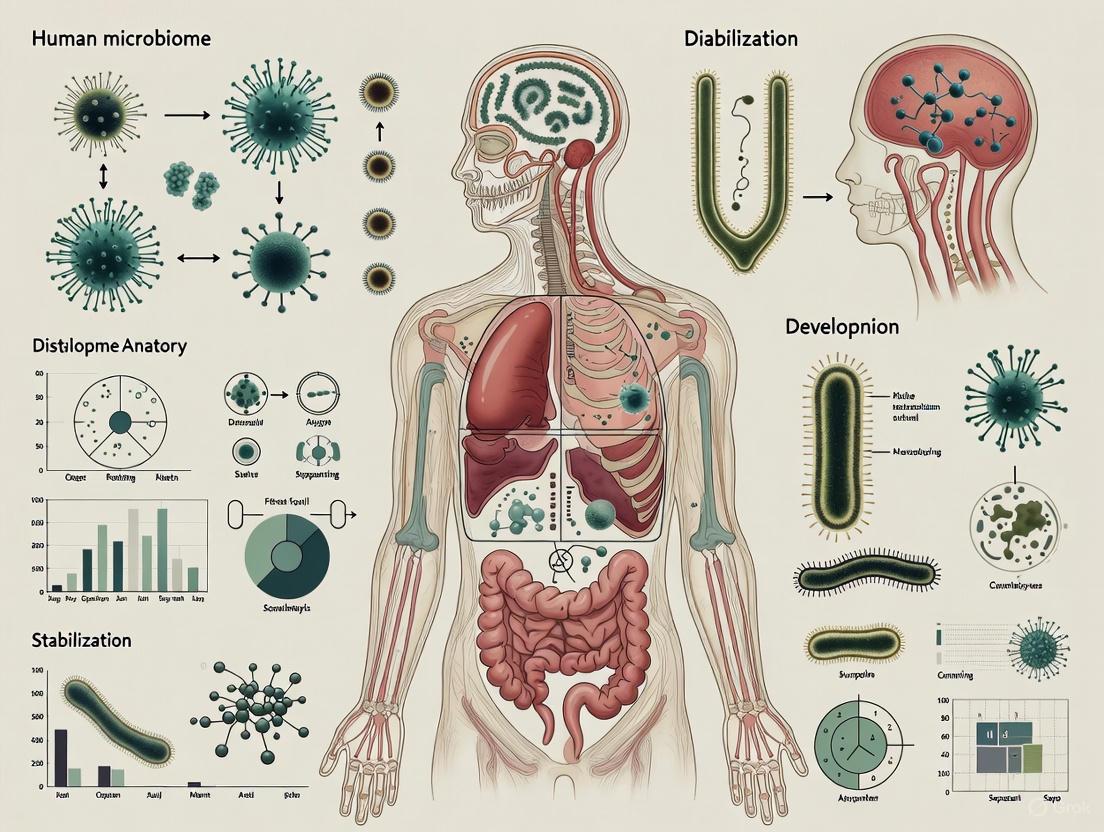
Human Microbiome Anatomy and Development: From Foundational Distribution to Therapeutic Stabilization
This article provides a comprehensive analysis of the human microbiome for researchers and drug development professionals.
Human Microbiome Anatomy and Development: From Foundational Distribution to Therapeutic Stabilization
Abstract
This article provides a comprehensive analysis of the human microbiome for researchers and drug development professionals. It synthesizes current knowledge on the anatomical distribution and developmental trajectory of microbial communities from birth to adulthood. The scope extends from foundational ecological principles and core microbiome concepts to advanced methodological applications in live biotherapeutic products (LBPs) and fecal microbiota transplantation (FMT). It further addresses challenges in managing dysbiosis, optimizing microbial resilience, and validates approaches through comparative analysis of the clinical pipeline and AI-driven predictive models. This resource is designed to bridge foundational microbiome science with translational clinical applications.
Mapping the Human Microbiome: Anatomical Distribution, Core Concepts, and Developmental Trajectory
The human body functions as a complex, heterogeneous landscape for microbial colonization. Understanding the spatial organization of the microbiome—specifically the variations in microbial density and diversity across different anatomical sites—is fundamental to a broader thesis on human microbiome distribution, anatomy, development, and stabilization research. This spatial patterning is not random; it reflects profound evolutionary adaptations, anatomical constraints, and physiological functions [1]. The precise mapping of these gradients provides a critical baseline for health and a reference for identifying dysbiosis in disease states. For researchers and drug development professionals, this knowledge is pivotal for designing targeted therapies, from site-specific probiotic delivery to novel antibiotics and microbiome-based diagnostics. Advances in spatial omics technologies and large-scale mapping projects are now enabling an unprecedented, high-resolution view of this microbial topography, moving beyond bulk compositional analysis to reveal the intricate, location-specific relationships between microbes and their human host [2].
Quantitative Atlas of Microbial Distribution
The distribution of microorganisms throughout the human body is highly uneven, governed by local environmental conditions such as pH, oxygen levels, moisture, and nutrient availability. The quantitative density of bacterial presence across major anatomical niches has been systematically characterized, providing a foundational metric for spatial organization.
Table 1: Microbial Density Gradients Across Major Anatomical Sites
| Anatomical Site | Relative Bacterial Density (%) | Predominant Microbial Phyla | Key Spatial Characteristics |
|---|---|---|---|
| Gastrointestinal Tract | 29% | Firmicutes, Bacteroidetes | Highest density; gradient from low density in stomach/duodenum to highest in colon [1] |
| Oral Cavity | 26% | Firmicutes, Bacteroidetes, Proteobacteria | High diversity; site-specific niches (tongue, plaque, gums) [1] |
| Skin | 21% | Actinobacteria, Firmicutes, Proteobacteria | Medium density; varies by skin region (sebaceous, moist, dry) [1] |
| Respiratory Tract | 14% | Firmicutes, Bacteroidetes, Proteobacteria | Density gradient: higher in upper tract, lower in lower tract [1] |
| Urogenital Tract | 9% | Firmicutes (e.g., Lactobacillus), Actinobacteria | Low density; composition sensitive to physiological changes [1] |
Beyond density, the concept of diversity gradients is equally critical. For instance, the gastrointestinal tract exhibits not only a density gradient but also a succession of microbial communities from the stomach to the colon, each adapted to the distinct physicochemical conditions of these sub-niches [1]. Similarly, the respiratory tract shows a decreasing gradient in both microbial density and diversity from the nasal passages to the alveoli, a feature essential for maintaining sterile conditions in the deep lungs [1].
Methodological Foundations for Spatial Microbiome Analysis
Elucidating the spatial architecture of the microbiome requires a suite of advanced technologies. The following experimental workflows represent cutting-edge methodologies for mapping microbiome density and diversity with high resolution.
High-Resolution Multimodal Spatial Atlas Construction
The Spatial Atlas of Human Anatomy (SAHA) project exemplifies a robust, multimodal framework for generating a subcellular-resolution reference of human tissues, integrating spatial transcriptomics, proteomics, and histological data [2].
Table 2: Key Experimental Protocols from the SAHA Framework
| Protocol Step | Detailed Methodology | Primary Objective |
|---|---|---|
| Tissue Procurement & Processing | Standardized collection from over 100 donors; rigorous quality control; fixation and embedding to preserve spatial context and biomolecule integrity [2]. | Minimize batch effects and cross-platform variability for robust data integration. |
| Multimodal Spatial Profiling | Sequential or parallel imaging using:• CosMx SMI: 1000-plex RNA, 67-plex protein.• 10x Xenium: High-throughput transcriptomics.• RNAscope: For RNA integrity assessment and validation.• GeoMx DSP: Region-specific protein and RNA profiling [2]. | Generate complementary, high-plex molecular data at subcellular (50 nm) resolution. |
| Cell Detection & Annotation | Automated recognition algorithms followed by manual curation; cell type annotation using canonical marker genes; validation via immunohistochemistry [2]. | Precisely identify and label over 50 distinct cell types (epithelial, immune, stromal, neuronal). |
| Spatial Registration & Data Integration | Registration of individual cells to a standardized brain coordinate framework (e.g., Allen CCFv3); use of UMAP for visualization; cell-cell adjacency mapping and ligand-receptor interaction analysis [2]. | Enable cross-organ and cross-donor comparisons; identify cellular neighborhoods and interaction networks. |
Figure 1: Experimental workflow for constructing a high-resolution spatial atlas, integrating multiple profiling platforms to map cellular and microbial neighborhoods.
Strain-Level Metagenomic Analysis for Global Diversity
To understand global genetic diversity and transmission patterns, large-scale metagenomic sequencing and strain-level phylogenetic analysis are employed. This approach moves beyond taxonomic classification to assess intraspecies genetic variability, which is crucial for linking specific microbial lineages to host phenotypes and geographical stratification [3].
Detailed Protocol Workflow:
- Sample Collection & Metagenomic Sequencing: 32,152 metagenomes from 94 global studies were collected and sequenced using shotgun metagenomics [3].
- Strain-Level Phylogenetic Reconstruction: Species-specific phylogenies were reconstructed for 583 microbial species from the metagenomic data. This allows for the tracking of specific microbial strains [3].
- Phenotype-Genotype Integration: The reconstructed microbial clades are linked to 241 host phenotypes, including anthropometric factors, biochemical measurements, and diseases [3].
- Geographic and Transmission Analysis: Strain geographic stratification is analyzed in relation to the species' horizontal transmissibility, providing insights into microbial dispersal and acquisition [3].
Conceptual Models of Microbiome Organization and Stability
Spatial organization has profound functional implications, influencing ecosystem stability and host-microbe interactions. The "Two Competing Guilds" (TCG) model, identified through systems biology and network analysis, provides a functional framework for understanding this organization.
Figure 2: The Two Competing Guilds (TCG) model depicts the core microbiome as a balance between health-promoting and disease-driving forces.
This model posits that the core gut microbiome is structured around two functionally antagonistic groups: the Foundation Guild (FG), dominated by Short-Chain Fatty Acid (SCFA)-producing bacteria, and the Pathobiont Guild (PG), enriched with opportunistic pathogens and pro-inflammatory microbes [4]. These guilds represent opposing functional forces, and their spatial and ecological balance directly influences host health.
The relational stability between these guilds is more significant than the mere presence of individual taxa. Network analysis of 38 microbiome datasets revealed that TCG members, though constituting less than 10% of total microbial members, form the ecosystem's backbone, accounting for 85% of all ecological interactions [4]. The FG members, such as Faecalibacterium prausnitzii and Roseburia spp., produce SCFAs that inhibit PG microbes, enhance gut barrier integrity, and mitigate inflammation [4]. This stable, competitive relationship is a key spatial-functional determinant of microbiome health.
The Scientist's Toolkit: Essential Research Reagents & Platforms
To replicate and advance the research outlined in this whitepaper, scientists require access to a specific set of high-end reagents, technologies, and computational tools.
Table 3: Research Reagent Solutions for Spatial Microbiome Analysis
| Category / Item | Specific Function / Example | Application in Spatial Analysis |
|---|---|---|
| Spatial Transcriptomics Platforms | CosMx SMI, 10x Xenium, GeoMx DSP [2] | Subcellular mapping of host and microbial RNA in intact tissue sections. |
| Multiplex Proteomics Panels | CosMx protein panel (67-plex) [2] | Simultaneous detection of dozens of proteins to define cell states and immune responses. |
| In Situ Hybridization Reagents | RNAscope assays [2] | Validation of RNA integrity and precise localization of specific microbial or host transcripts. |
| Bioinformatic Analysis Suites | Algorithms for cell detection, spatial registration (e.g., to Allen CCFv3), and network analysis [2] [3] | Automated cell typing, 3D reconstruction, and quantification of cellular neighborhoods. |
| Strain-Tracking Metagenomics Tools | Computational pipelines for strain-level phylogenetic reconstruction from metagenomes [3] | Linking global genetic diversity of microbes to host phenotypes and geographic origins. |
| Gnotobiotic Animal Models | Germ-free mice [1] [5] | Establishing causality by studying host physiology in the absence of microbes and after targeted colonization. |
| o-Cresol-d7 | o-Cresol-d7 Isotopic Standard | High-purity o-Cresol-d7 isotopic standard for MS, NMR, and environmental tracer studies. For Research Use Only. Not for human use. |
| L-Methionine-34S | L-Methionine-34S, MF:C5H11NO2S, MW:151.11 g/mol | Chemical Reagent |
The systematic mapping of density and diversity gradients across major anatomical sites provides an indispensable spatial framework for human microbiome research. The integration of multimodal spatial omics, as demonstrated by the SAHA atlas, with large-scale, strain-resolved metagenomics represents the frontier of this field. This synergy allows researchers to move from correlative observations to mechanistic understandings of how specific microbial communities, positioned in precise anatomical niches, influence human physiology and disease. For drug development, these insights are paving the way for next-generation therapies. This includes the design of precision delivery systems that target specific gut regions [6], the development of rationally defined consortia of microbes (synthetic biotics) [7], and the use of phage therapies targeting pathogens within complex biofilms [7]. As these spatial technologies become more accessible and computational models more sophisticated, the future of microbiome research lies in comprehensively charting this intricate landscape to develop novel, spatially informed diagnostics and therapeutics.
The long-standing doctrine of human sterility at internal sites is undergoing a profound reassessment. Traditional human anatomy has taught that organs such as the brain, vascular system, and placenta exist in sterile isolation from the microbial world. However, emerging evidence from advanced sequencing technologies and carefully controlled studies challenges this paradigm, suggesting that these sites may host resident microbial communities under certain conditions [1]. This whitepaper examines the compelling evidence and methodological considerations surrounding microbiome presence in traditionally sterile human sites, framed within the broader context of human microbiome distribution, anatomy, development, and stabilization research. Understanding these microbial communities requires a systematic framework that considers anatomical distribution, physiological functions, and the complex interplay between microbial and human genomes [1]. The implications for disease pathogenesis, diagnostic approaches, and therapeutic development are substantial, potentially reshaping fundamental concepts in human physiology and pathology.
Evidence for Microbiome Presence in Traditionally Sterile Sites
Vascular System Microbiota
The human vascular system, long presumed to be sterile, now shows evidence of hosting microbial communities in both health and disease states. Atherosclerotic vessels demonstrate a non-sterile environment containing bacteria and viruses, with arterial atherosclerosis sequencing providing compelling evidence [1]. A rigorous study employing strict exclusion criteria, aseptic sampling, repeated measures, and negative controls to eliminate potential contamination analyzed femoral arteries from brain-dead donors, predominantly those with hemorrhagic or ischemic strokes [1]. The research identified Proteobacteria, Firmicutes, and Actinobacteria as the predominant phyla, with Staphylococcus, Pseudomonas, Corynebacterium, Bacillus, Acinetobacter, and Propionibacterium representing prevalent genera [1]. Interestingly, the study also observed a notable correlation between blood type and microbiota diversity, suggesting potential host genetic factors influencing vascular microbial colonization [1]. However, limitations including small sample size (14 participants) and restricted age range (40-60 years) necessitate cautious interpretation and further validation.
Despite these findings, the sterility of blood in healthy individuals remains supported by substantial evidence. An analysis of 9,770 samples from healthy individuals in the Human Microbiome Project revealed the absence of similar microbial communities in the bloodstream, with 82% of the sampled population exhibiting no microbial sequences [1]. This dichotomy suggests that vascular microbiota may represent a disease-associated phenomenon rather than a baseline physiological state, though temporal dynamics and methodological limitations leave this question open for further investigation.
Ocular Surface and Brain Microbiota
The human ocular surface, despite constant exposure to the environment and protective mechanisms, hosts a diverse microbiome that includes Pseudomonas, Bradyrhizobium, Propionibacterium, Acinetobacter, and Corynebacterium as the most abundant genera [1]. This community exists despite the antimicrobial properties of tears and frequent blinking, suggesting sophisticated adaptation mechanisms.
Perhaps most controversially, the brain—long considered the archetypal sterile organ due to the protective blood-brain barrier—has shown potential evidence of microbial presence. Surprising findings from microscopic examination of multiple brain regions in post-mortem healthy individuals, presented at a neuroscience conference, have suggested the existence of microbiota in the brain [1]. However, the scientific community awaits confirmation through rigorous animal models and independent human validation studies [1]. The potential mechanisms for microbial entry into the brain, including transcellular migration, Trojan horse mechanisms, or peripheral nerve pathways, remain speculative without stronger evidence.
Other Potentially Non-Sterile Sites
Other anatomical sites are similarly challenging traditional sterility assumptions:
- Gallbladder: Though sampling difficulties exist, studies have confirmed the presence of microbial communities in the gallbladder, potentially through retrograde entry of gastrointestinal microbiota [1].
- Mammary Tissue: Women aged 18-90 show a diverse range of bacteria, predominantly Proteobacteria, in mammary tissue [1].
- In Utero Environment: The question of whether a normal fetus is colonized by microbes prenatally ("in utero colonization" hypothesis) remains highly controversial, challenging the established "sterile womb" paradigm [1]. A recent comprehensive discussion suggests that detected microbes may represent contamination rather than true colonization, emphasizing the lack of reliable evidence for consistent microbial presence [1].
Table 1: Evidence for Microbiome Presence in Traditionally Sterile Sites
| Anatomical Site | Key Microbial Findings | Strength of Evidence | Controversies/Limitations |
|---|---|---|---|
| Vascular System | Proteobacteria, Firmicutes, Actinobacteria; Staphylococcus, Pseudomonas, Corynebacterium | Moderate in disease states; Limited in health | Potential contamination; Small sample sizes; Blood largely sterile in healthy individuals |
| Ocular Surface | Pseudomonas, Bradyrhizobium, Propionibacterium, Acinetobacter, Corynebacterium | Established | Differentiation between resident vs. transient communities |
| Brain | Potential presence based on post-mortem examination | Preliminary | Requires animal model confirmation; Independent validation needed |
| Gallbladder | Microbial communities present | Moderate | Retrograde GI migration suspected; Sampling difficulties |
| Mammary Tissue | Proteobacteria predominant | Established | Age range 18-90 studied |
| In Utero Environment | Potential microbial presence | Highly controversial | Likely contamination; No reliable evidence of consistent colonization |
Methodological Approaches and Technical Considerations
Sequencing Technologies and Their Applications
The investigation of microbiomes in low-biomass environments like traditionally sterile sites requires sophisticated sequencing approaches, each with distinct advantages and limitations:
DNA Metabarcoding (Amplicon Sequencing): This approach characterizes samples using reads obtained through selective amplification of marker genes like the 16S rRNA gene for prokaryotes or ITS regions for fungi [8]. While cost-effective and suitable for detecting rare taxa with approximately 100,000 reads per sample, it faces three main limitations: (1) Restricted taxonomic resolution due to conservation of marker genes, (2) Inherent limitations in functional profiling, and (3) Vulnerability to PCR amplification errors and biases including undersampling, contamination, storage conditions, and polymerase errors [8]. Tools like PICRUSt2 and Tax4Fun2 attempt functional prediction from taxonomic profiles but with limited accuracy and resolution [8].
Shotgun Metagenomic Sequencing: This method involves isolation of DNA from samples followed by deep sequencing without target-specific amplification [8]. Shotgun metagenomics enables high-resolution taxonomic profiling from phylum to strain level and allows study of the functional potential of microbial communities through gene identification and pathway analysis [8]. However, it requires greater sequencing depth, is more costly, and generates data that is typically more sparse than 16S rRNA data [9].
Multi-Omics Integration: Advanced approaches including metatranscriptomics, metaproteomics, and metabolomics provide complementary insights into microbial community function beyond compositional assessment [8]. Metatranscriptomics measures mRNA levels to reveal actively expressed functions, while metaproteomics identifies and quantifies proteins actually produced by the community [10]. Metabolomics profiles the small molecule metabolites produced, offering the most direct readout of microbial functional activities [8].
Special Considerations for Low-Biomass Sites
Research on microbiomes in traditionally sterile sites presents unique methodological challenges:
Contamination Control: The low microbial biomass in these environments makes them exceptionally vulnerable to contamination during sampling, processing, or sequencing. Strategies include implementation of strict exclusion criteria, aseptic sampling techniques, repeated measures, negative controls, and careful documentation of potential confounding factors [1].
Metadata Collection: Comprehensive and standardized metadata is crucial for interpreting results and comparing datasets across studies [8]. This includes detailed information about sample collection, processing, sequencing parameters, and host characteristics. Incomplete metadata hinders the ability to perform robust data stratifications and account for confounding factors [8].
Computational and Statistical Methods: Microbiome data analysis must account for characteristics including zero inflation, overdispersion, high dimensionality, compositionality, and sample heterogeneity [9]. Statistical methods for differential abundance analysis include edgeR, metagenomeSeq, DESeq2, ANCOM, ZIBSeq, ZIGDM, and corncob, each with different normalization approaches and underlying models [9].
Research Workflow for Sterile Site Microbiome Studies
Analytical Framework and Technical Challenges
Statistical Considerations for Microbiome Data Analysis
Microbiome data derived from traditionally sterile sites presents unique statistical challenges that require specialized analytical approaches:
Compositional Data Analysis: microbiome sequencing data is compositional, meaning that counts are relative rather than absolute due to variable sequencing depth across samples [9]. This compositionality necessitates special statistical methods that account for the constrained nature of the data, with false positives potentially arising from analyzing relative abundances as if they were absolute measurements [9].
Zero Inflation and Overdispersion: Microbiome datasets typically contain a high proportion of zeros (up to 90% in some cases), with both true absences and false zeros due to technical limitations [9]. These data also exhibit overdispersion, where variance exceeds the mean, violating assumptions of standard statistical models. Methods like zero-inflated models (ZIBSeq, ZIGDM) specifically address these characteristics [9].
Batch Effects and Normalization: Technical variability arising from different DNA extraction methods, sequencing runs, or laboratory personnel can introduce batch effects that confound biological signals [9]. Normalization approaches including Total Sum Scaling (TSS), Cumulative Sum Scaling (CSS), Relative Log Expression (RLE), and Trimmed Mean of M-values (TMM) help account for variable sequencing depth, while methods like ComBat, removeBatchEffect, and surrogate variable analysis (SVA) address batch effects specifically [9].
Table 2: Key Analytical Methods for Sterile Site Microbiome Data
| Analytical Challenge | Statistical Methods | Key Features | Applicability to Sterile Sites |
|---|---|---|---|
| Differential Abundance Analysis | edgeR, DESeq2, metagenomeSeq, ANCOM, corncob | Accounts for compositionality, zero inflation, overdispersion | High (essential for low-biomass comparisons) |
| Batch Effect Correction | ComBat, removeBatchEffect, SVA, RUV | Removes technical variability from different processing batches | Critical (due to heightened contamination concerns) |
| Normalization | TSS, CSS, TMM, RLE | Adjusts for variable sequencing depth | Essential (particularly for cross-study comparisons) |
| Functional Prediction | PICRUSt2, Tax4Fun2 | Infers functional potential from taxonomic data | Moderate (limited by reference database completeness) |
| Network Analysis | SparCC, SPIEC-EASI, MInt | Infers microbial association networks | Emerging (requires sufficient sample size) |
Contamination Identification and Control
For low-biomass microbiome studies, distinguishing true signal from contamination is paramount:
Negative and Positive Controls: Inclusion of extraction controls, no-template amplification controls, and positive controls with known microbial compositions helps identify contamination sources and assess technical variability [1].
Bioinformatic Decontamination: Computational approaches including frequency-based filtering, prevalence-based methods, and machine learning techniques help identify and remove potential contaminants by leveraging patterns indicative of contamination rather than biological signal [8].
Indicator Molecules: Detection of molecules unlikely to survive in viable microbes (such as certain RNAs or labile metabolites) can help distinguish between living residents and non-viable contaminants or DNA fragments [1].
Research Reagent Solutions and Experimental Tools
Table 3: Essential Research Reagents and Tools for Sterile Site Microbiome Research
| Reagent/Tool Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| DNA Extraction Kits | MoBio PowerSoil, DNeasy Blood & Tissue | DNA isolation from low-biomass samples | Optimization needed for different sample types; includes controls for contamination |
| 16S rRNA Primers | 515F-806R (V4), 27F-338R (V1-V2) | Amplification of bacterial taxonomic markers | Selection affects taxonomic coverage and resolution |
| Shotgun Library Prep | Illumina Nextera, KAPA HyperPrep | Preparation of sequencing libraries | Optimized for low-input DNA crucial for sterile sites |
| Contamination Control | DNase/RNase removal reagents, UV irradiation | Reduction of external DNA contamination | Critical for low-biomass studies |
| Positive Control Standards | ZymoBIOMICS Microbial Community Standards | Assessment of technical variability | Known composition communities for benchmarking |
| Storage/Preservation | RNA/DNA Stabilization Tubes, Freezing at -80°C | Sample integrity maintenance | Critical between collection and processing |
| Bioinformatics Pipelines | QIIME2, Mothur, DADA2, MEGAN | Data processing and analysis | Standardization enables cross-study comparisons |
Conceptual Framework and Theoretical Implications
The emerging evidence challenging traditional sterility concepts necessitates new conceptual frameworks for understanding host-microbe relationships:
Evolving Paradigms in Host-Microbe Relationships
Innate and Adaptive Genomes: This framework proposes viewing the human innate genome (inherited genetic blueprint) in continuous crosstalk with the adaptive genome (dynamic microbiome), with exploration of their interplay potentially explaining a broader spectrum of individual phenotypic variations [1].
Meta-Host Model: This concept broadens the definition of host to include symbiotic microbes as an integrated biological entity, potentially explaining disease heterogeneity or organ transplantation success rates resulting from host-microbiome interactions [1].
Germ-Free Syndrome: The abnormalities observed in germ-free animals challenge the traditional "microbes as pathogens" view, instead advocating for the necessity of microbes for health, with potential implications for understanding the consequences of absent microbiota in traditionally sterile sites [1].
Slave Tissue Concept: This perspective views microbes as exogenous tissues under the control of human master tissues (nerve, connective, epithelial, muscle), highlighting the dynamic health implications of microbial interactions in various anatomical niches [1].
Conceptual Evolution in Sterile Site Microbiome Research
The investigation of microbiomes in traditionally sterile human sites represents a frontier in microbiome research with profound implications for understanding human physiology and disease. While compelling evidence suggests microbial presence in locations like the vascular system, ocular surface, and potentially the brain, methodological challenges including contamination control, appropriate statistical analysis, and result interpretation remain substantial. Future research directions should include:
Standardized Methodologies: Development and implementation of standardized protocols for sample collection, processing, and analysis specifically optimized for low-biomass environments [8].
Longitudinal Studies: Implementation of longitudinal sampling designs to distinguish between transient and resident communities and understand microbial dynamics in health and disease transitions [1].
Multi-Omics Integration: Combined application of metagenomics, metatranscriptomics, metaproteomics, and metabolomics to move beyond compositional assessment to functional understanding [8].
Experimental Validation: Development of sophisticated animal models and in vitro systems to experimentally validate sequencing findings and establish causal mechanisms [1].
Clinical Translation: Exploration of diagnostic and therapeutic applications, including microbial biomarkers for disease detection or microbial-based interventions for conditions originating in traditionally sterile sites [11].
As research methodologies continue to advance and conceptual frameworks evolve, our understanding of microbial presence in traditionally sterile sites will likely transform fundamental concepts in human anatomy, physiology, and pathology, ultimately contributing to more comprehensive approaches to human health and disease.
The core microbiome represents a fundamental concept in microbial ecology, crucial for understanding the intricate relationship between microbial ecosystems and human health. Traditionally defined through taxonomic overlap—identifying microbial species consistently present across multiple individuals—this approach has provided valuable but limited insights [4]. While useful for establishing baseline microbial composition, taxonomic definitions often fail to capture the functional dynamics and ecological interactions that ultimately determine microbiome stability and host health outcomes [4] [1]. This limitation is particularly evident when considering the substantial functional redundancy across microbial communities, where different species can perform similar ecological roles, making taxonomic presence alone an insufficient predictor of ecosystem function [4].
A paradigm shift is emerging toward understanding the core microbiome through the lens of relational stability, which focuses on persistent microbial interactions rather than merely persistent taxa [4]. This systems biology framework recognizes that stable relationships—not just individual components—signify the core structure of complex adaptive systems like the gut microbiome [4]. By identifying microbial relationships that endure across varying conditions such as dietary interventions or disease states, researchers can better elucidate the fundamental architecture that maintains ecosystem integrity and functionality [4]. This transition from taxonomic to relational definitions represents a significant advancement in microbiome science, with profound implications for predictive modeling, therapeutic development, and personalized medicine.
Theoretical Foundations: From Taxonomy to Relational Stability
Limitations of Taxonomic Overlap Approaches
Conventional approaches to defining the core microbiome have primarily relied on cataloging microbial taxa that are commonly shared across populations [4]. This method assumes that shared presence equates to ecological importance, but this assumption often proves inadequate for several reasons. First, taxonomic labels frequently fail to capture the ecological and functional roles of individual strains, risking the exclusion of key microbial interactions that sustain host health [4]. Second, functional redundancy across microbial communities means that different taxa can perform similar metabolic functions, making presence/absence data insufficient for predicting ecosystem performance [4]. Third, taxonomic approaches typically overlook the strain-level diversity that often determines functional capabilities and host interactions [4].
The practical limitations of taxonomic overlap become evident when considering that core microbiome members identified through this method are indeed commonly shared, but not all commonly shared microbes contribute significantly to critical ecosystem functions [4]. This discrepancy explains why taxon-based approaches often struggle to identify consistent microbial signatures associated with health states across diverse populations, and why therapeutic interventions based solely on taxonomic composition have shown limited success [4].
The Relational Stability Framework
The relational stability framework addresses these limitations by applying systems biology principles to microbiome analysis [4]. This approach is grounded in the fundamental tenet that in complex adaptive systems, stable relationships—not individual components—signify core structure [4]. For the gut microbiome, this implies identifying microbial relationships that endure across varying conditions, such as dietary interventions or disease states [4].
The core methodology involves identifying stably connected genome pairs across diverse conditions [4]. This approach involves constructing co-abundance networks from microbiome data and searching for genome pairs that exhibit stable correlations across different perturbations [4]. These stable genome pairs reflect ecological interactions—including cooperation, competition, and niche sharing—that are essential for maintaining ecosystem integrity [4]. Analysis of 38 microbiome datasets spanning dietary interventions and 15 diseases revealed a consistent Two Competing Guilds (TCG) structure as a core signature, comprising a Foundation Guild (FG) dominated by short-chain fatty acid-producing bacteria and a Pathobiont Guild (PG) enriched with opportunistic pathogens and pro-inflammatory microbes [4].
Table 1: Key Concepts in Relational Stability Framework
| Concept | Definition | Significance |
|---|---|---|
| Stably Connected Genome Pairs | Microbial genomes that maintain correlated abundance patterns across diverse conditions | Identifies ecologically significant interactions beyond taxonomic presence |
| Co-abundance Networks | Mathematical representation of microbial abundance correlations | Enables visualization and quantification of microbial relationships |
| Two Competing Guilds (TCG) | Core structure comprising Foundation and Pathobiont Guilds | Represents fundamental functional organization of gut microbiome |
| Foundation Guild (FG) | Microbial consortium specialized in fiber fermentation and SCFA production | Promotes gut barrier integrity, reduces inflammation, maintains metabolic homeostasis |
| Pathobiont Guild (PG) | Microbial consortium with virulence factors and inflammatory potential | Drives inflammation, disrupts metabolic balance, associated with disease states |
Methodological Approaches: Analyzing Microbial Relational Stability
Data Generation and Preprocessing
The analysis of relational stability in microbiome research relies on sophisticated sequencing technologies and careful data processing. The two primary sequencing methods are 16S ribosomal RNA gene sequencing and metagenomic shotgun sequencing (MSS) [9] [12]. While 16S sequencing provides a cost-effective approach for taxonomic classification, MSS offers greater resolution by sequencing entire genomes, enabling species-level identification and functional profiling [12]. For relational stability analyses, MSS is particularly valuable as it provides the genome-level data required for identifying stable genome pairs [4].
Microbiome data present several analytical challenges that must be addressed during preprocessing, including zero inflation (where up to 90% of counts may be zeros), overdispersion, high dimensionality, and compositional effects [9]. Normalization techniques such as Cumulative Sum Scaling (CSS) and Trimmed Mean of M-values (TMM) are essential to account for variable sequencing depth across samples [9]. Additionally, batch effect correction methods like Remove Unwanted Variation (RUV) and ComBat may be necessary to eliminate technical artifacts [9].
Network Construction and Analysis
The construction of co-abundance networks begins with correlation analysis between microbial abundances. The SparCC algorithm and similar approaches are particularly valuable as they account for compositional data constraints [9]. Once correlation matrices are established, network inference techniques identify significant associations, with stability across conditions determined through permutation testing or cross-validation approaches [4].
The relational stability framework specifically searches for network connections that persist across multiple perturbations or population subsets [4]. In practice, this involves analyzing multiple datasets—spanning different diseases, dietary interventions, or population cohorts—and identifying the microbial interactions that remain statistically significant across these diverse conditions [4]. This cross-condition stability distinguishes core ecological relationships from situation-specific associations.
Experimental Validation and Functional Characterization
The relational stability framework extends beyond computational analysis to experimental validation. Key experimental approaches include gnotobiotic mouse models colonized with defined microbial communities, in vitro culture systems that recapitulate microbial interactions, and metabolomic profiling to verify functional outputs [4] [11]. These validation approaches are essential for establishing causal relationships between stable microbial interactions and host phenotypes.
Functional characterization typically involves metatranscriptomics to assess gene expression patterns, metaproteomics to quantify protein abundance, and metabolomics to measure metabolic outputs [12]. For the TCG model, specific functional assays might quantify short-chain fatty acid production by Foundation Guild members or measure inflammatory potential of Pathobiont Guild members [4]. These functional readouts provide mechanistic links between relational stability and host health outcomes.
Table 2: Key Analytical Methods for Relational Stability Analysis
| Method Category | Specific Techniques | Application in Relational Stability |
|---|---|---|
| Sequencing Technologies | 16S rRNA sequencing, Shotgun Metagenomics | Generate raw microbial abundance data for network construction |
| Normalization Methods | CSS, TMM, TSS, RLE | Account for technical variability and compositional nature of data |
| Network Inference | SparCC, Pearson/Spearman Correlation | Identify significant microbial associations in co-abundance networks |
| Stability Assessment | Cross-validation, Permutation Testing | Determine which network connections persist across conditions |
| Functional Validation | Metabolomics, Metatranscriptomics, Gnotobiotic Models | Verify biological significance of stable relationships |
The Two Competing Guilds Model: A Core Structure Revealed Through Relational Stability
Foundation Guild Characteristics
The Foundation Guild (FG) represents a core functional consortium within the gut microbiome, characterized by dominance of short-chain fatty acid (SCFA)-producing bacteria [4]. Key SCFAs produced by this guild include acetic acid, propionic acid, and butyric acid, which serve multiple host-beneficial functions [4]. Butyrate, in particular, serves as the primary energy source for colonocytes, enhances gut barrier function by strengthening tight junctions, and exhibits anti-inflammatory properties through inhibition of histone deacetylases [4].
From an ecological perspective, FG members typically include taxa such as Faecalibacterium prausnitzii, Roseburia species, and other specialized fiber-fermenting bacteria that have co-evolved with human hosts [4]. These taxa often form stable cooperative networks, cross-feeding on metabolic byproducts to maximize energy extraction from dietary fibers [4]. The relational stability analysis revealed that FG members maintain consistent ecological relationships despite dietary variations and other perturbations, underscoring their foundational role in ecosystem integrity [4].
Pathobiont Guild Characteristics
The Pathobiont Guild (PG) comprises microorganisms with potential for virulence factor expression, antibiotic resistance genes, and pro-inflammatory activities [4]. Unlike frank pathogens, pathobionts typically exist as commensals under homeostatic conditions but can promote pathology when their growth goes unchecked or when they translocate across compromised mucosal barriers [4].
PG members produce various metabolites with potential host-detrimental effects, including endotoxins (such as lipopolysaccharide), indole derivatives, and hydrogen sulfide [4]. These compounds can drive systemic inflammation, disrupt gut barrier integrity, interfere with insulin signaling, and promote metabolic dysfunction [4]. The relational stability framework demonstrates that PG members maintain stable associations with each other, forming a coherent functional group that behaves distinctly from the Foundation Guild [4].
Guild Interactions and Ecological Dynamics
The TCG model reveals that Foundation and Pathobiont Guilds typically exist in a dynamic equilibrium, with competitive exclusion and resource competition shaping their ecological relationship [4]. FG members often inhibit PG growth through multiple mechanisms, including SCFA-mediated suppression of virulence gene expression, nutrient competition, and reinforcement of gut barrier function [4]. This competitive relationship explains why these guilds emerge as distinct network modules in relational stability analyses.
The balance between FG and PG has profound implications for host health. Analysis of 38 datasets across 15 diseases revealed that 85% of ecological interactions in the gut microbiome center around TCG members, despite these guilds constituting less than 10% of total microbial membership [4]. This disproportionate influence on network structure positions the TCG as a primary determinant of microbiome stability and function. Removal of FG or PG members significantly disrupts network integrity, confirming their foundational role as the backbone of the gut microbial ecosystem [4].
Research Toolkit: Essential Methods and Reagents
Table 3: Essential Research Tools for Relational Stability Analysis
| Tool Category | Specific Tools/Reagents | Function/Application |
|---|---|---|
| Sequencing Platforms | Illumina MiSeq/HiSeq, PacBio, Oxford Nanopore | Generate raw sequence data for microbial community analysis |
| Bioinformatics Pipelines | QIIME2, DADA2, Mothur, MetaPhlAn2 | Process raw sequencing data, perform taxonomic assignment |
| Network Analysis Software | SparCC, CoNet, SPIEC-EADI | Construct co-abundance networks from microbial abundance data |
| Statistical Programming | R (phyloseq, vegan, igraph packages), Python | Perform statistical analysis, visualization, and stability testing |
| Reference Databases | GREENGENES, SILVA, KEGG, eggNOG | Taxonomic and functional annotation of microbial sequences |
| Culture Media | Modified YCFA, Gifu Anaerobic Medium | In vitro cultivation of Foundation and Pathobiont Guild members |
| Analytical Standards | SCFA standards (acetate, propionate, butyrate), LPS standards | Quantification of microbial metabolites in validation experiments |
| GN25 | GN25|SNAIL-p53 Inhibitor|For Research | GN25 is a novel SNAIL-p53 interaction inhibitor used in cancer research to reverse EMT and inhibit angiogenesis. This product is For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| Leukotriene E4-d5 | Leukotriene E4-d5 Stable Isotope | Leukotriene E4-d5 is a deuterium-labeled internal standard for precise LC/MS or GC/MS quantification of LTE4 in asthma and inflammation research. For Research Use Only. |
Applications and Implications: From Basic Research to Clinical Translation
Predictive Modeling and Diagnostics
The relational stability framework significantly enhances predictive modeling in microbiome research. Using stably connected genomes in TCGs as features substantially improves classification of disease versus control samples and enhances prediction of treatment outcomes compared to models relying solely on taxonomic composition [4]. This approach has demonstrated particular value in predicting responses to immunotherapy, where TCG-based models outperformed conventional taxonomic markers [4] [13].
The Stably Connected Agent Network (SCAN) AI modeling framework capitalizes on relational stability by using stably connected agents as key features for prediction and analysis [4]. In medical applications, SCAN improves the precision of models for diagnosing diseases or predicting treatment outcomes by leveraging stable microbial relationships as indicators of health or disease states [4]. This approach underscores the translational potential of moving beyond taxonomic composition to relational signatures.
Therapeutic Development and Microbiome Engineering
Relational stability opens new avenues for therapeutic development by identifying key ecological relationships that can be targeted for intervention. Rather than attempting to introduce or eliminate specific taxa, microbiome engineering can focus on manipulating the stable relationships that determine ecosystem outcomes [4]. This might involve developing prebiotics that selectively enhance Foundation Guild function, or designing bacteriophage cocktails that specifically target Pathobiont Guild members without disrupting beneficial microbes [11].
Clinical trials building on the relational stability framework are exploring interventions that specifically target the balance between Foundation and Pathobiont Guilds [4] [11]. These include high-fiber dietary interventions to support SCFA production, precision probiotics designed to integrate into existing Foundation Guild networks, and microbiota transplantation protocols that transfer stable microbial relationships rather than just microbial taxa [11]. The TCG model provides a rational framework for designing and evaluating these interventions based on their impact on core ecological dynamics rather than simply taxonomic composition.
The transition from taxonomic overlap to relational stability represents a paradigm shift in how we define and understand the core microbiome. This framework recognizes that stable relationships—not just stable taxa—form the fundamental architecture of microbial ecosystems, with the Two Competing Guilds model providing a concrete example of how this architecture shapes host health [4]. By focusing on persistent microbial interactions that withstand environmental perturbations, relational stability offers a more robust, functional, and clinically relevant definition of what constitutes a "core" microbiome.
The implications of this shift extend beyond basic science to therapeutic development, diagnostic innovation, and personalized medicine [4] [11]. As microbiome research continues to evolve, the relational stability framework provides a powerful approach for identifying intervention targets, predicting health outcomes, and ultimately harnessing the microbiome to improve human health. Future research should further refine our understanding of how these stable relationships establish during early development, how they vary across populations, and how they can be therapeutically manipulated to prevent and treat disease.
The human microbiome, particularly within the gastrointestinal tract, is now recognized as a fundamental regulator of health, influencing processes from digestion and immunity to neurological function [14] [15]. A significant challenge in microbiome research has been defining a "core microbiome"—a set of microbial entities consistently associated with health across diverse populations [16] [4]. Traditional approaches focusing on taxonomic abundance have proven inadequate, as they often conflate beneficial and harmful strains within the same species and fail to account for functional redundancy across taxa [17] [16].
The Two Competing Guilds (TCG) Model represents a paradigm shift from taxonomy to ecology and function. This model identifies two distinct bacterial groups—the Foundation Guild (FG) and the Pathobiont Guild (PG)—that engage in dynamic competition to determine gut ecosystem stability and host health outcomes [18] [4] [19]. A "guild" is defined as a group of bacteria that show consistent co-abundance behavior and likely work together to contribute to the same ecological function, irrespective of their taxonomic classification [17] [20]. This framework provides a universal strategy for identifying core microbiome structures based on stable relational dynamics rather than mere taxonomic presence [4].
Theoretical Framework and Ecological Principles
From Taxonomy to Functional Guilds
Conventional microbiome analysis has relied heavily on collapsing bacterial strains based on nearest-neighbor taxonomy, often leading to controversial and inconsistent results across studies [17] [20]. A prominent example is the decade-long debate over the Firmicutes/Bacteroidetes (F/B) ratio in obesity, where meta-analyses ultimately found no consistent relationship [17]. These limitations stem from several critical factors:
- Strain-Level Diversity: Bacterial strains within the same species can exhibit up to 30% difference in their genomic makeup, leading to contrasting phenotypes and host interactions [17] [20].
- Functional Redundancy: Similar ecological functions can be performed by taxonomically distinct organisms [4].
- Database Limitations: Taxonomic approaches often exclude novel bacteria that cannot be classified against existing reference databases [17] [20].
The guild-based approach addresses these limitations by focusing on co-abundance behavior and functional coherence rather than phylogenetic relationships [17]. Members of the same guild cooperate, thrive, or decline together, showing synchronized ecological behavior across different environmental conditions and host states [20].
The Relational Stability Principle
The TCG model is grounded in the principle of relational stability—the concept that core microbiome members maintain consistent functional relationships within the gut ecosystem across diverse conditions [4]. From an evolutionary perspective, these stable relationships represent millennia of co-evolution between humans and their microbiota, forming a foundational structure that withstands various environmental pressures [4].
This principle shifts the focus from cataloging individual taxa to identifying persistent ecological interactions that form the backbone of the microbial ecosystem. Research analyzing 38 microbiome datasets spanning dietary interventions and 15 diseases revealed that TCG members constitute less than 10% of total microbial members yet form the center of 85% of ecological interactions within the gut network [4]. This disproportionate influence confirms their foundational role in maintaining ecosystem integrity.
Defining the Competing Guilds: Characteristics and Functions
Foundation Guild: The Cornerstone of Health
The Foundation Guild represents a consortium of bacteria that serve as structural and functional pillars of the gut ecosystem. These taxa exhibit several defining characteristics:
Table 1: Key Characteristics of the Foundation Guild
| Characteristic | Description | Functional Significance |
|---|---|---|
| Primary Metabolic Function | Dietary fiber degradation and fermentation | Produces short-chain fatty acids (SCFAs) including butyrate, acetate, and propionate [18] [4] [19] |
| Ecological Role | Structures and stabilizes the gut microbial network | Forms the backbone of ecological interactions; removal disrupts network integrity [4] [19] |
| Host Benefits | Enhances gut barrier function, reduces inflammation, promotes satiety hormone production | Butyrate serves as energy source for colonocytes; strengthens tight junctions; regulates immune responses [18] [4] [19] |
| Representative Taxa | Faecalibacterium prausnitzii, Roseburia spp., and other SCFA-producing bacteria | These species have co-evolved with humans as cooperative partners [4] |
The Foundation Guild's dominance creates an environment that suppresses pathogenic species through multiple mechanisms: competitive exclusion for nutrients and adhesion sites, creation of unfavorable metabolic conditions (e.g., lower pH from SCFA production), and direct enhancement of host defense mechanisms [4] [19].
Pathobiont Guild: Necessary but Potentially Harmful
The Pathobiont Guild comprises bacteria that exist in a symbiotic relationship with the host under normal conditions but can proliferate and become detrimental under certain circumstances:
Table 2: Key Characteristics of the Pathobiont Guild
| Characteristic | Description | Functional Impact |
|---|---|---|
| Metabolic Output | Production of endotoxins, indole, hydrogen sulfide, and other inflammatory mediators | Promotes systemic inflammation, disrupts gut barrier integrity, contributes to insulin resistance [18] [4] |
| Ecological Role | Necessary in small amounts for immune education and vigilance | Provides tonic stimulation to host immune system; required for proper immune development [18] [19] |
| Disease Association | Ecological dominance linked to chronic inflammatory states | Associated with inflammatory bowel disease, metabolic disorders, neurological conditions, and certain cancers [18] [4] [19] |
| Regulation | Suppressed by Foundation Guild metabolites (SCFAs) and host immune factors | SCFAs inhibit PG growth; gut barrier integrity prevents systemic translocation of PG components [4] |
The Pathobiont Guild's necessary but precarious position in the ecosystem illustrates the complexity of host-microbe relationships. At low abundance, these microbes contribute to immune system education and maintain ecological diversity, but when their population expands beyond a critical threshold, they can drive disease processes [18] [19].
The Seesaw Dynamics of Guild Competition
The TCG model conceptualizes gut health as a dynamic balance between the Foundation and Pathobiont Guilds, often described as a "seesaw" relationship [19]. When the Foundation Guild dominates, gut health is maintained through the mechanisms described above. Conversely, when the balance tips in favor of the Pathobiont Guild, dysbiosis occurs, potentially leading to inflammation that can exacerbate various chronic conditions [18] [19].
This competitive dynamic is primarily mediated through metabolic interference, where Foundation Guild members utilize dietary fibers to produce SCFAs that simultaneously benefit the host and inhibit Pathobiont Guild expansion [4]. The diagram below illustrates these core competitive dynamics:
Methodological Framework: Analytical Approaches and Protocols
Genome-Centric Analysis for Strain-Level Resolution
The TCG model employs a genome-centric analytical approach that overcomes the limitations of traditional taxonomy-dependent methods [20] [19]. This methodology is built on three key pillars:
Genome-Specific Analysis: Utilizes high-quality metagenome-assembled genomes (MAGs) or amplicon sequence variants (ASVs) as fundamental analytical units, providing near strain-level resolution [20]. Each genome receives a universal unique identifier (UUID) to track its ecological behavior across studies without relying on taxonomic classification [19].
Database-Independent Inclusivity: By assigning UUIDs based on sequence identity rather than taxonomic affiliation, this approach ensures that novel and unclassifiable bacteria are included in analyses, significantly reducing information loss [20].
Interaction-Focused Aggregation: Microbial sequences are grouped into guilds based on co-abundance patterns across samples and conditions, rather than phylogenetic relationships [17] [20].
The experimental workflow below outlines the key steps in guild-based analysis:
Research Reagent Solutions and Essential Materials
Implementation of the TCG analytical framework requires specific reagents and computational tools:
Table 3: Essential Research Reagents and Tools for TCG Analysis
| Category | Specific Tools/Reagents | Function | Considerations |
|---|---|---|---|
| Sequencing Technology | Shotgun metagenomic sequencing platforms | Comprehensive genomic characterization of microbial communities | Prefer long-read technologies for improved assembly; depth >10M reads/sample [20] |
| Genome Assembly | MEGAHIT, metaSPAdes | Assembly of short reads into contigs and metagenome-assembled genomes (MAGs) | Use multiple assemblers; quality assessment with CheckM [17] |
| Bin Refinement | DAS Tool, MetaBAT2, MaxBin2 | Grouping contigs into MAGs based on sequence composition and abundance | Apply refinement pipelines; aim for >90% completeness, <5% contamination [16] |
| UUID System | Custom UUID generation scripts | Tracking genomes across studies without taxonomic assignment | Enables database-independent analysis [20] [19] |
| Co-abundance Analysis | SparCC, CoNet, FlashWeave | Quantifying coordinated abundance patterns to identify guilds | Network inference with multiple methods; statistical validation [4] |
| Functional Annotation | KEGG, MetaCyc, eggNOG | Predicting functional potential of identified guilds | 40-60% of genes may lack annotation; consider pathway completeness [17] |
Validation Through Cross-Study Analysis
A critical strength of the TCG model is its validation across diverse populations and conditions. Researchers have applied this framework to 38 microbiome datasets spanning dietary interventions and 15 different diseases, consistently identifying the same core guild structure [4]. This cross-study validation confirms that the Foundation and Pathobiont Guilds represent universal ecological units in the human gut, transcending variations in ethnicity, geography, and disease states.
The robustness of guild identification is evaluated using β-diversity matrices of all ASVs or MAGs as a benchmark for the entire information content of the original datasets [20]. Procrustes analysis and Mantel tests are then employed to compare β-diversity matrices before and after data reduction to guild-level variables, ensuring minimal information loss or distortion during the analytical process [20].
Clinical and Therapeutic Implications
Diagnostic and Predictive Applications
The TCG framework provides a powerful approach for classifying health states and predicting treatment outcomes:
- Disease Classification: Artificial intelligence models using stably connected genomes in TCGs as features significantly improve classification of disease versus control samples compared to models based on taxonomic composition alone [4].
- Treatment Response Prediction: The TCG model enhances prediction of personalized responses to immunotherapy across four different diseases, demonstrating its clinical utility beyond gastrointestinal disorders [4] [19].
- Microbiome Health Assessment: The balance between Foundation and Pathobiont Guilds serves as a functional biomarker for gut ecosystem health, transcending the limitations of diversity metrics or taxonomic ratios [16] [4].
Therapeutic Interventions
The TCG model informs targeted therapeutic strategies aimed at restoring Foundation Guild dominance:
Table 4: TCG-Informed Therapeutic Approaches
| Intervention | Mechanism | Application |
|---|---|---|
| Personalized Nutrition | Targeted supplementation with fibers matching Foundation Guild degradation capabilities | Precision diets to support SCFA production and Pathobiont suppression [4] [19] |
| Fecal Microbiota Transplantation (FMT) | Direct restoration of Foundation Guild communities | Severe dysbiosis states; requires rigorous donor screening for safety [21] [16] |
| Prebiotic Formulations | Selective stimulation of Foundation Guild growth | Fiber blends targeting SCFA-producing bacteria; inulin, oligosaccharides [21] |
| Probiotic Consortia | Introduction of defined Foundation Guild members | Next-generation probiotics containing keystone SCFA producers [21] |
| Phage Therapy | Selective targeting of dominant Pathobiont species | Precision depletion of pathobionts without broad-spectrum antibiotics [21] |
Safety and Ethical Considerations
Clinical translation of TCG-based therapies requires careful attention to safety and ethical implications. Fecal microbiota transplantation, while effective, has resulted in infections when proper screening protocols were not followed [16]. Rigorous donor screening, standardized preparation methods, and long-term safety monitoring are essential for microbiome-based interventions [21] [16].
Future Directions and Research Agenda
The TCG model opens several promising avenues for future research:
Strain-Resolved Dynamics: Further refinement to strain-level resolution will elucidate functional differences within guilds and enhance personalization [16].
Multi-Omics Integration: Combining metagenomics with metabolomics, proteomics, and host profiling will provide systems-level understanding of guild-host interactions [16] [1].
Longitudinal Studies: Dense temporal sampling will reveal how guild dynamics fluctuate in response to interventions, disease progression, and normal physiological variation [16].
Extrabiblical Guilds: Investigating whether similar competing guild structures exist in other body sites (oral, skin, respiratory) [14] [1].
AI-Driven Causal Inference: Developing machine learning approaches that can establish causal relationships between guild imbalances and specific health outcomes [16].
The Two Competing Guilds model represents a transformative framework for understanding gut microbiome structure and function. By shifting focus from taxonomic classification to ecological roles and relational stability, it provides a universal strategy for identifying core microbiome components essential for human health. The dynamic balance between Foundation and Pathobiont Guilds serves as both a biomarker for health assessment and a target for therapeutic intervention.
As research progresses, the TCG model has the potential to redefine precision medicine approaches for numerous chronic conditions linked to gut dysbiosis. Its validation across diverse populations and conditions underscores its robustness as a foundational framework for future microbiome research and clinical translation.
From Bench to Bedside: Methodologies and Therapeutic Applications for Microbiome Manipulation
The human microbiome, a complex ecosystem of trillions of microorganisms inhabiting various anatomical sites, has co-evolved with humans to play essential roles in metabolism, immunity, and disease prevention [22] [23]. Technological advancements have transformed our understanding of this "hidden organ," which contains over 150 times the genetic material of the human genome [22]. Traditional microbiome studies, primarily focused on microbial composition through 16S ribosomal RNA (rRNA) gene sequencing, provided limited insights into functional and mechanistic host-microbiome interactions [22] [23]. The advent of multi-omics technologies—integrating genomics, proteomics, metabolomics—coupled with artificial intelligence (AI) has revolutionized microbiome research, enabling a systems-level understanding of microbial ecology and function [22] [23].
This technological evolution represents a paradigm shift from purely taxonomic descriptions to functional microbiome characterization [23]. Where earlier methods could identify which bacteria were present, integrated multi-omics approaches can now reveal what functions these microbes are performing, how they interact with each other and the host, and what metabolic products they generate [22]. AI and machine learning further enhance this approach by deciphering complex patterns within massive datasets that would be impossible for humans to analyze manually [24] [25]. This comprehensive analytical framework is particularly valuable for understanding microbiome development, distribution, and stabilization across different anatomical sites throughout the human lifespan [1] [11].
The clinical translation of these technological advances is already underway, with applications in precision medicine, drug development, and therapeutic interventions [11] [26]. Microbiome-based diagnostics and therapeutics are increasingly recognized as integral to preventing and treating complex diseases, with the global human microbiome market expected to reach $1.52 billion by 2030 [26]. This growth reflects the expanding recognition that harnessing microbial functions offers unprecedented opportunities for personalized healthcare solutions tailored to an individual's unique microbial composition [22] [11].
Genomic Approaches in Microbiome Research
Metagenomic Sequencing and Analysis
Metagenomics represents a foundational genomic approach in microbiome research, enabling the direct sequencing and analysis of genetic material from entire microbial communities without the need for cultivation [23]. This approach has overcome significant limitations associated with studying unculturable microbial species, which constitute a substantial portion of the human microbiome [23]. Two primary strategies dominate metagenomic sequencing: 16S rRNA sequencing and shotgun metagenomics.
16S rRNA sequencing targets the hypervariable regions of the bacterial 16S ribosomal RNA gene, which contains both conserved and variable regions that serve as fingerprints for taxonomic classification [22]. This method provides a cost-effective approach for profiling microbial community composition and estimating relative abundances of different bacterial taxa [22]. However, it has several limitations, including PCR amplification biases, primer specificity issues, and limited resolution at the species or strain level [23]. Additionally, 16S rRNA sequencing identifies which bacteria are present but provides little information about their functional capabilities [22].
Shotgun metagenomics (shotgunMG) represents a more comprehensive approach by sequencing all DNA fragments in a sample randomly, enabling reconstruction of complete microbial genomes and functional profiles [22] [23]. This method facilitates strain-level identification and can detect microbial genes, pathways, and functional potential [22]. In personalized medicine, shotgunMG offers valuable insights for tailoring interventions based on an individual's unique gut microbiome profile, potentially predicting treatment responses and disease susceptibility [22].
Table 1: Comparison of Genomic Sequencing Approaches in Microbiome Research
| Feature | 16S rRNA Sequencing | Shotgun Metagenomics |
|---|---|---|
| Target Region | 16S rRNA gene hypervariable regions | All genomic DNA in sample |
| Resolution | Genus to species level | Species to strain level |
| Functional Insights | Limited inference from taxonomy | Direct assessment of functional genes |
| Quantification | Relative abundance | Relative abundance with potential for absolute quantification |
| Cost | Lower | Higher |
| Reference Database Dependence | High for taxonomy assignment | High for functional annotation |
| Primary Applications | Microbial community profiling, diversity analysis | Functional potential assessment, pathogen detection |
Metagenomic Workflows and Experimental Protocols
A standardized metagenomic workflow begins with sample collection from the target anatomical site (e.g., gut, skin, oral cavity), followed by DNA extraction using optimized kits that ensure comprehensive lysis of diverse microbial cell types [23]. For 16S rRNA sequencing, PCR amplification of specific hypervariable regions (V1-V9) is performed using primer sets tailored to the research question, followed by library preparation and high-throughput sequencing [23]. For shotgun metagenomics, DNA undergoes fragmentation, size selection, adapter ligation, and library preparation without target-specific amplification [22].
Bioinformatic analysis pipelines process the resulting sequencing data. For 16S rRNA data, this typically involves quality filtering, denoising, amplicon sequence variant (ASV) or operational taxonomic unit (OTU) clustering, taxonomic assignment against reference databases (e.g., SILVA, Greengenes), and diversity analyses [23]. Shotgun metagenomic analysis employs quality control, host DNA removal, de novo assembly or reference-based mapping, gene prediction and annotation, taxonomic profiling, and functional pathway analysis using tools like HUMAnN or MetaPhlAn [22] [27].
The National Microbiome Data Collaborative (NMDC) has developed standardized workflows and data processing tools to enhance reproducibility and interoperability across studies [28] [29]. Their bioinformatics pipeline, NMDC EDGE, provides standardized workflows for processing multi-omics microbiome data, supporting best practices in data stewardship throughout the research lifecycle [28].
Proteomic and Metabolomic Technologies
Metabolomic Profiling in Microbiome Research
Metabolomics provides a direct readout of microbial functional activity by characterizing the complete set of small molecule metabolites (<1,500 Da) produced by microbial communities and their host interactions [22]. These metabolites act as chemical messengers, circulating through the body and influencing metabolism, immunity, and even brain function [24]. Gut microbes produce and modify thousands of metabolites, including short-chain fatty acids (SCFAs), bile acids, neurotransmitters, and vitamins, which play crucial roles in host physiology [22] [24].
Two primary analytical platforms dominate metabolomic studies: mass spectrometry (MS) and nuclear magnetic resonance (NMR) spectroscopy [22]. MS-based approaches, particularly liquid chromatography-mass spectrometry (LC-MS) and gas chromatography-mass spectrometry (GC-MS), offer high sensitivity, broad dynamic range, and the ability to characterize thousands of metabolites simultaneously [22]. NMR spectroscopy provides advantages in quantitative accuracy, minimal sample preparation, and structural elucidation capabilities, though with generally lower sensitivity than MS [22].
Metabolomic workflows begin with careful sample collection (feces, blood, urine) and immediate quenching of metabolic activity to preserve the in vivo metabolic state [27]. Sample extraction employs methods like methanol precipitation or methyl-tert-butyl ether liquid-liquid extraction to recover diverse metabolite classes [22]. Following instrumental analysis, raw data processing includes feature detection, alignment, normalization, and metabolite identification using databases such as HMDB, METLIN, and MassBank [22]. Statistical analysis then identifies differentially abundant metabolites associated with specific microbial communities or host phenotypes.
In athletic performance research, metabolomic profiling has revealed distinct metabolic adaptations between different types of athletes. A study of Colombian elite athletes found that weightlifters showed elevated carnitine, amino acid, and glycerolipid levels compared to cyclists, suggesting energy system-specific metabolic adaptations tailored to their athletic disciplines [27]. These findings underscore how microbiome-influenced metabolomic profiles can reflect specialized physiological demands.
Proteomic Analysis of Microbial Communities
Proteomic approaches characterize the complete set of proteins expressed by microbial communities and host cells in response to microbial interactions, providing direct insight into functional activities and signaling pathways [22]. Microbial proteins include enzymes catalyzing metabolic reactions, structural proteins, and secreted proteins that mediate host-microbe interactions [22].
Mass spectrometry-based proteomics, particularly liquid chromatography-tandem mass spectrometry (LC-MS/MS), is the primary technology for large-scale protein identification and quantification [22]. Two main strategies are employed: bottom-up proteomics, which involves protein extraction, enzymatic digestion (typically with trypsin), and LC-MS/MS analysis of resulting peptides; and top-down proteomics, which analyzes intact proteins without digestion [22]. Bottom-up approaches currently dominate due to their higher sensitivity and compatibility with complex mixtures.
Experimental protocols for microbiome proteomics (metaproteomics) begin with protein extraction from fecal or tissue samples using detergent-based lysis buffers [22]. Proteins are digested into peptides, which are then separated by liquid chromatography and analyzed by tandem mass spectrometry [22]. Bioinformatics analysis involves database searching against matched metagenomic sequences or reference databases, protein inference, quantification, and functional annotation [22].
Metaproteomics faces unique challenges, including the complexity of protein mixtures from multiple organisms, dynamic range issues, and the need for matched metagenomic data for accurate protein identification [22]. Despite these challenges, metaproteomics provides crucial functional information that complements other omics approaches by revealing which genetic potentials are actually being expressed and how microbial functions change in response to environmental stimuli [23].
Table 2: Multi-omics Technologies in Microbiome Research
| Technology | Analytical Target | Key Platforms | Information Gained | Limitations |
|---|---|---|---|---|
| Metagenomics | DNA | 16S rRNA sequencing, Shotgun sequencing | Microbial composition, genetic potential, phylogenetic relationships | Does not measure functional activity |
| Metatranscriptomics | RNA | RNA-Seq | Gene expression patterns, active metabolic pathways | RNA instability, difficult extraction |
| Metaproteomics | Proteins | LC-MS/MS | Protein expression, enzymatic activities, host-microbe interactions | Complex sample preparation, database dependencies |
| Metabolomics | Metabolites | LC-MS, GC-MS, NMR | Metabolic activities, end products of microbial processes | High variability, complex identification |
Artificial Intelligence and Machine Learning Applications
AI-Driven Pattern Recognition in Microbiome Data
Artificial intelligence, particularly machine learning (ML) and deep learning (DL), has become indispensable for analyzing the immense complexity of multi-omics microbiome data [24] [25]. These approaches can identify subtle, non-linear patterns and interactions within high-dimensional datasets that traditional statistical methods often miss [24]. ML algorithms learn from training data to recognize complex relationships between microbial features and host phenotypes, enabling predictions about disease states, treatment responses, and ecological dynamics [25].
Various ML approaches are applied to microbiome research, including supervised learning for classification and regression tasks (e.g., predicting disease status from microbial features), unsupervised learning for clustering and dimensionality reduction (e.g., identifying microbial enterotypes), and semi-supervised learning that leverages both labeled and unlabeled data [25]. Deep learning models, such as convolutional neural networks (CNNs) and recurrent neural networks (RNNs), can automatically learn hierarchical feature representations from raw sequencing data or spectral profiles [25].
A notable advancement is the development of specialized AI tools like VBayesMM, a Bayesian neural network that identifies genuine biological relationships between bacterial groups and metabolites while quantifying uncertainty in its predictions [24]. This system has outperformed traditional models in studies of obesity, sleep disorders, and cancer, demonstrating how AI can extract meaningful biological insights from complex microbiome datasets [24]. The Bayesian approach is particularly valuable for microbiome data because it explicitly models uncertainty, helping prevent overconfident but incorrect conclusions that can arise from noisy or incomplete data [24].
AI Applications in Microbial Communication and Ecology
AI approaches are revolutionizing our understanding of microbial communication and ecology by decoding how gut microbes interact with each other and with their human host through chemical signals [24] [25]. Researchers at the University of Tokyo applied AI to map relationships between specific bacterial groups and metabolites, moving closer to understanding how to manipulate these interactions for therapeutic benefits [24]. Their system analyzes which bacterial families significantly influence particular metabolites, providing clues about how to grow specific bacteria to produce beneficial metabolites or design targeted therapies that modify these metabolites to treat diseases [24].
Beyond human health, AI is being applied to environmental microbiome ecosystems. Researchers at Oregon State University are using deep learning to analyze oceanic microbial ecosystems, particularly focusing on methane seeps off the coast of Oregon and Washington [25]. This research aims to identify the role of unknown genes in global biogeochemical cycles by developing AI models that categorize genes into pathways and predict functions of unknown genes based on protein sequences and text-based data [25]. This demonstrates how AI approaches developed for human microbiome research can be adapted to diverse ecological contexts.
The integration of AI with multi-omics data creates powerful predictive models for personalized medicine. Machine learning algorithms can integrate genomic, proteomic, and metabolomic data to predict individual responses to diets, drugs, or probiotics [22] [25]. For example, AI models have been developed to classify conditions such as inflammatory bowel disease or colorectal cancer with greater accuracy by recognizing complex microbial patterns that elude traditional analysis [25]. These models "remember relationships that humans might not," identifying complex patterns across multiple data types that can inform clinical decision-making [25].
Integrated Multi-Omics Workflows
Data Integration and Network Analysis
The true power of modern microbiome research lies in integrating multiple omics technologies to obtain a comprehensive picture of microbiome structure and function [22] [23]. Multi-omics integration involves combining data from genomics, transcriptomics, proteomics, and metabolomics to achieve a systems-level understanding that transcends the limitations of any single approach [22]. This holistic perspective enables researchers to connect microbial genetic potential with actual functional activities and their effects on host physiology [23].
Network analysis provides a powerful framework for integrating multi-omics data by representing relationships between microbial taxa, genes, proteins, and metabolites as interconnected nodes in a graph [22]. These networks can reveal microbial community structure, keystone species, and functional modules that correlate with host phenotypes [22]. Statistical and computational frameworks range from global concordance and latent factor models to feature-wise association networks that detect cross-modal correlations and mechanistic links [22]. By jointly analyzing metabolomics with metagenomics, studies can attribute specific metabolites to particular microbial species or pathways, uncovering mechanistic relationships between microbiome composition and host health [22].
Large-scale initiatives like the Integrative Human Microbiome Project (iHMP) have applied multi-omics strategies to investigate the epidemiology, evolution, and diversity of gut microbial communities [23]. These initiatives extend beyond taxonomic and functional profiling, laying the groundwork for microbiome-based disease prevention, therapeutic interventions, and precision medicine [23]. The iHMP has demonstrated how longitudinal multi-omics profiling can reveal dynamic relationships between host physiology, microbiome ecology, and disease states, providing insights into the temporal progression of microbiome-associated conditions [11].
Standards and Data Stewardship in Multi-Omics Research
The growing complexity and volume of multi-omics data have highlighted the critical importance of data standards and stewardship for ensuring reproducibility, interoperability, and reusability [28] [29]. Many microbiome datasets are currently produced using non-standardized methods across researchers and organizations, creating challenges for data comparison, integration, and meta-analysis [28]. To address these challenges, initiatives like the National Microbiome Data Collaborative (NMDC) have developed standardized workflows, metadata templates, and data management best practices [28].
The FAIR data principles (Findable, Accessible, Interoperable, and Reusable) provide a framework for microbiome data stewardship [28] [29]. Implementation involves using persistent identifiers (PIDs) for studies, samples, and datasets; rich metadata using controlled vocabularies and ontologies; and standardized data formats that enable machine-actionability [29]. The Genomic Standards Consortium's Minimum Information about any (x) Sequence (MIxS) standard provides a community-developed framework for reporting microbiome metadata across diverse environments [28].
The NMDC Ambassador Program utilizes a community-learning model to train early-career researchers in microbiome data stewardship best practices [28]. This program has demonstrated effectiveness in promoting awareness and implementation of data standards, with 98% of workshop participants reporting gained knowledge about metadata standards, principles for microbiome data management, and the importance of standardization in microbiome data processing [28]. Such initiatives are essential for building a culture of data sharing and collaboration that accelerates microbiome research translation.
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Platforms for Microbiome Multi-Omics
| Category | Specific Products/Platforms | Key Applications | Considerations |
|---|---|---|---|
| DNA Extraction Kits | QIAamp PowerFecal Pro, DNeasy PowerLyzer, MoBio PowerSoil | Metagenomic DNA isolation from diverse sample types | Efficiency for gram-positive bacteria, inhibitor removal, yield consistency |
| Library Prep Kits | Illumina Nextera XT, NEBNext Ultra II, Swift Accel | Sequencing library preparation for metagenomics | Insert size selection, amplification bias, compatibility with sequencing platform |
| Sequencing Platforms | Illumina NovaSeq, PacBio Sequel, Oxford Nanopore | High-throughput sequencing for metagenomics | Read length, error rates, throughput requirements, cost considerations |
| Chromatography Systems | Agilent HPLC, Thermo Vanquish, Waters UPLC | Metabolite and protein separation prior to MS analysis | Resolution, sensitivity, throughput, compatibility with MS systems |
| Mass Spectrometers | Thermo Orbitrap, Bruker timsTOF, Sciex TripleTOF | Metabolite and protein identification and quantification | Mass accuracy, resolution, dynamic range, fragmentation capabilities |
| Bioinformatics Tools | QIIME 2, HUMAnN, MetaPhlAn, Motif | Microbiome data processing and analysis | Database dependencies, computational requirements, user expertise needed |
| AI/ML Platforms | TensorFlow, PyTorch, scikit-learn, VBayesMM | Pattern recognition and predictive modeling | Computational demands, interpretability, validation requirements |
The technological arsenal for microbiome analysis has evolved dramatically, transitioning from basic taxonomic profiling to comprehensive multi-omics approaches that reveal the functional dynamics of microbial communities [23]. The integration of genomics, proteomics, metabolomics, and artificial intelligence provides unprecedented insights into how microbiomes influence human health and disease across different anatomical sites and life stages [1] [11]. These advances are driving a paradigm shift in medicine, with microbiome-based diagnostics and therapeutics becoming increasingly integrated into clinical practice [11] [26].
Future developments in microbiome research will likely focus on several key areas. First, the continued refinement of multi-omics technologies will enhance our ability to characterize low-biomass niches and resolve strain-level variation [11]. Second, standardization of methodologies and data stewardship practices will improve reproducibility and enable larger-scale meta-analyses [28] [23]. Third, AI and machine learning will become increasingly sophisticated in predicting microbiome dynamics and host responses, facilitating truly personalized microbiome interventions [24] [25]. Finally, the translation of microbiome research into clinical applications will expand, with microbiome-based therapies playing larger roles in oncology, gastroenterology, neurology, and metabolic disorders [11] [26].
As these technologies continue to advance, they will deepen our understanding of the intricate relationships between human microbiomes and health, ultimately enabling more precise, effective, and personalized approaches to medicine [22] [23]. The integration of technological innovation with biological insight will continue to unravel the complexity of our microbial inhabitants and their profound influence on human physiology [1] [11].
The human microbiome, a complex ecosystem of microorganisms, plays a pivotal role in regulating physiological processes including digestion, immune responses, and metabolic functions [30]. Therapeutic modulation of this ecosystem has evolved from a niche clinical procedure to a sophisticated drug development frontier. This evolution spans a spectrum from whole-community restoration to precisely targeted biological interventions, framed within the broader context of human microbiome distribution, anatomy, development, and stabilization research [31]. The proven success of fecal microbiota transplantation (FMT) for recurrent Clostridioides difficile infection (rCDI) validated the fundamental premise that restoring microbial communities can treat disease, thereby catalyzing the development of standardized, regulated therapeutic modalities [32] [33]. This whitepaper examines the core technical and developmental characteristics of three principal therapeutic classes: FMT, defined microbial consortia, and Live Biotherapeutic Products (LBPs), providing researchers and drug development professionals with a comparative analysis and methodological framework.
Comparative Analysis of Core Therapeutic Modalities
The landscape of microbiome therapeutics is characterized by a progression from complex, undefined communities toward precisely engineered products, balancing ecological restoration with mechanistic specificity.
Table 1: Comparative Analysis of Core Microbiome Therapeutic Modalities
| Feature | Fecal Microbiota Transplantation (FMT) | Defined Microbial Consortia | Live Biotherapeutic Products (LBPs) |
|---|---|---|---|
| Definition | Transfer of entire microbial community from healthy donor stool [33] | Laboratory-grown consortium of defined bacterial strains [34] | Regulated biological products containing live organisms for disease treatment/prevention [33] [35] |
| Composition | Complex, undefined; thousands of microbial taxa, viruses, fungi [31] | 2 to ~50 defined, characterized bacterial strains (e.g., VE303: 8 Clostridia strains) [34] [33] | Single strain or defined consortium; can be native or genetically engineered [31] |
| Mechanism of Action | Ecosystem restoration & colonization resistance [32] [31] | Targeted restoration of specific functional groups [34] | Specific molecular mechanisms (e.g., bile acid metabolism, immunomodulation) [33] [31] |
| Key Examples | Traditional FMT; OpenBiome supplies [32] | VE303 (rCDI), VE202 (Ulcerative Colitis) [36] [34] | Rebyota (rCDI), Vowst (rCDI), Akkermansia muciniphila (metabolic) [32] [33] [35] |
| Manufacturing | Donor screening, stool processing, suspension in saline/PEG [32] [31] | Individual strain fermentation, blending to defined ratios [34] [31] | Controlled fermentation under GMP; lyophilization [31] |
| Regulatory Status | FDA enforcement discretion for rCDI; varies globally [32] [31] | Developed under IND/EMA pathways as biological drugs [34] | Regulated as drugs by FDA/EMA; specific LBP guidelines [33] [31] |
Table 2: Clinical Efficacy and Commercial Positioning of Major Modalities
| Modality / Product | Indication | Efficacy Results | Administration | Commercial/Development Stage |
|---|---|---|---|---|
| FMT (Traditional) | rCDI | >80-90% success rate with single/repeated doses [33] [35] | Colonoscopy, enema, capsules [31] | Clinical standard for rCDI; use expected to decline with approved products [31] |
| Rebyota (RBX2660) | rCDI | ~70.6% success vs. 57.5% placebo at 8 weeks [32] [33] | Rectal enema [32] | FDA-approved 2022 [32] [36] |
| Vowst (SER-109) | rCDI | Significant superiority vs. placebo (RR 0.32) [33] [35] | Oral capsules [33] | FDA-approved; oral purified Firmicutes spores [36] [33] |
| VE303 | rCDI | 13.8% recurrence (high-dose) vs. 45.5% placebo [33] [35] | Oral capsules [36] | Phase 3 [36] [34] |
| MaaT013 | aGvHD | Improved clinical responses; satisfactory safety in immunocompromised [33] [31] | Enema (Oral also in development) [36] [31] | MAA submitted to EMA (2025); Phase 3 for aGvHD [31] |
Experimental and Methodological Frameworks
Protocol for Defined Consortium Assembly and Validation
The development of a defined microbial consortium requires a methodical, multi-stage process to ensure therapeutic viability.
Step 1: Strain Selection and Rational Design: Candidate strains are selected from bacterial biorepositories or isolated from healthy donor stools based on functional attributes (e.g., SCFA production, bile acid metabolism, immunomodulatory properties) [34] [31]. Selection occurs at the strain level, not species level, as critical phenotypes like virulence factor expression, antibiotic resistance, and manufacturability are strain-specific [31]. For example, Vedanta Biosciences' VE303 was rationally designed from eight distinct strains of Clostridia that promote colonization resistance [34] [33].
Step 2: Individual Strain Cultivation and Banking: Each selected strain undergoes optimized anaerobic fermentation in controlled bioreactors. A key development challenge is reforming growth media for GMP scale-up, which involves eliminating undefined or animal-derived components [31]. Master and working cell banks are created for each strain to ensure consistent starting material for all production runs.
Step 3: Co-Fermentation or Blending: Two primary manufacturing paths exist: 1) Co-fermentation, where strains are grown together for efficiency, requiring holistic purity testing, or 2) Monoculture-then-blend, where strains are fermented separately and then combined, which maintains superior strain-level control and ratio precision [31].
Step 4: Formulation and Lyophilization: The blended consortium is formulated into its final delivery format (e.g., suspension, powder for capsules). Lyophilization parameters must be optimized for each strain, as survival rates vary significantly by strain and bacterial growth phase [31]. This represents a critical development milestone to ensure adequate viability through manufacturing, storage, and administration.
Step 5: Potency and Engraftment Validation: Finished product testing includes potency assays to confirm viability and metabolic function, alongside in vitro colonization models (e.g., gut simulators) and in vivo gnotobiotic mouse models to validate community stability and host engraftment potential [34]. These models are crucial for determining the minimal effective dose and predicting clinical performance.
Signaling Pathways in Microbiome Therapeutics
Microbiome therapeutics mediate their effects through complex host-microbe interactions. The following diagram illustrates key molecular pathways involved.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful development of microbiome therapeutics relies on specialized research tools and platforms for strain characterization, functional analysis, and product validation.
Table 3: Essential Research Reagent Solutions for Microbiome Therapeutic Development
| Reagent / Platform | Function/Description | Application in Development |
|---|---|---|
| Gnotobiotic Mouse Models | Germ-free animals colonized with defined microbial communities [34] | Mechanistic studies of consortium engraftment, host interaction, and therapeutic efficacy [34] |
| Anaerobic Cultivation Media | Specialized formulations for growing oxygen-sensitive commensal bacteria | Strain isolation, expansion, and manufacturing process development [31] |
| Multi-Omics Analysis Tools | Integrated genomics, metabolomics, and proteomics platforms | Comprehensive characterization of consortium composition, function, and host response [30] [37] |
| CRISPR-Based Editing Systems | Precision gene editing tools for microbial engineering | Creation of engineered LBPs with enhanced functions or tracking capabilities [36] [30] |
| In Vitro Gut Simulators | Bioreactor systems mimicking human gastrointestinal conditions | Pre-clinical testing of consortium stability and metabolic activity [34] |
| Cell-Based Immunoassays | Systems for measuring immune responses to microbial components | Screening strain immunomodulatory properties (e.g., Treg induction, cytokine profiling) [31] |
| L-ANAP | L-ANAP, CAS:1313516-26-5, MF:C15H16N2O3, MW:272.304 | Chemical Reagent |
| 3-Bromopyridine-D4 | 3-Bromopyridine-d4 Isotope - 66148-14-9 - For Research Use |
Development Workflow for Microbiome Therapeutics
The transition from concept to commercial microbiome therapeutic requires careful planning across distinct development phases. The following workflow outlines the key stages from research to market entry.
The therapeutic modality spectrum from FMT to defined LBPs represents a maturation of microbiome science from ecological restoration toward precision medicine. While FMT established the fundamental principle that microbial community transfer can effectively treat disease, its future application will likely be limited to exceptional circumstances due to regulatory, manufacturing, and patient acceptance challenges [31]. Defined microbial consortia offer a balanced approach, maintaining multi-strain complexity while enabling standardized manufacturing and improved safety profiles [34] [33]. The ongoing clinical development of consortia for indications beyond rCDI, including inflammatory bowel disease and oncology, will be a critical test of this modality's broader applicability [36] [34].
The most significant frontier lies in the advancement of Live Biotherapeutic Products, both single-strain and defined consortia, which promise targeted mechanisms of action, superior manufacturability, and clear regulatory pathways [33] [31]. Future success depends on solving key technical challenges: optimizing lyophilization for fastidious anaerobes, elucidating molecular mechanisms beyond "colonization resistance," and establishing robust potency assays and engraftment metrics [31]. Furthermore, the field is expanding toward engineered microbes with enhanced functions and the integration of AI and multi-omics data for patient stratification and personalized consortium design [30] [37]. As research continues to unravel the complexities of human microbiome anatomy and stabilization, therapeutic modalities will increasingly reflect this sophistication, moving from broad ecological restoration to precise manipulation of host-microbe interactions for targeted therapeutic outcomes.
The human microbiome, a complex ecosystem of bacteria, fungi, archaea, and viruses, has emerged from a scientific curiosity to a frontier of therapeutic innovation. Historically regarded as passive passengers, microbial communities are now recognized as active determinants of human physiology, shaping immunity, metabolism, and therapeutic responses across organ systems [11]. The completion of the Human Microbiome Project and related initiatives has catalysed a paradigm shift, enabling researchers to decode the mechanistic basis of host-microbe interactions and exploit this knowledge for drug development [1]. This transition from descriptive ecology to interventional medicine is evidenced by the first regulatory approvals for microbiome-based therapies and a pipeline that has expanded to encompass over 230 candidates targeting conditions from recurrent Clostridioides difficile infection (rCDI) to oncology and metabolic disorders [36].
Anatomically, the microbiome is distributed as a dynamic network across host tissues, with the gastrointestinal tract representing the most densely populated site (29%), followed by the oral cavity (26%) and skin (21%) [1]. Its development begins at birth, evolving through a primary succession phase that stabilizes into a "climax community" by adolescence, remaining relatively stable yet adaptable throughout adulthood [1]. The conceptual framework of the "meta-host" – which redefines the human host as an integrated unit comprising human cells and their microbial counterparts – provides the essential context for understanding how microbiome-targeted therapies exert their effects across such diverse disease areas [1]. This whitepaper provides a comprehensive technical overview of the clinical pipeline, experimental methodologies, and translational frameworks driving this rapidly advancing field.
Analytical Frameworks for Microbiome-Host Dynamics
Conceptual Models Informing Therapeutic Development
The development of effective microbiome therapeutics requires a robust theoretical understanding of host-microbe relationships. Several key models and hypotheses provide this foundation:
- The "Innate and Adaptive Genomes": This concept reframes the human genetic landscape by distinguishing the static, inherited "innate genome" from the dynamic, environmentally acquired "adaptive genome" represented by the microbiome. This framework is crucial for understanding individual variations in disease susceptibility and therapeutic response that cannot be explained by human genetics alone [1].
- The "Slave Tissue" Hypothesis: This model posits that the microbiome functions as an exogenous tissue under the control of human master tissues (nerve, connective, epithelial, and muscle). This perspective elucidates the symbiotic intricacies between human tissues and their microbial counterparts, explaining how microbial communities can be harnessed for therapeutic purposes [1].
- The "Health-Illness Conversion Model": This systematic framework outlines common patterns of dysbiosis, describing how interactions between the innate and adaptive genomes can transition from homeostasis to disease states. It provides a roadmap for designing interventions that reverse specific dysbiotic patterns [1].
- Acquired Microbial Immunity: This concept positions the microbiome as an adjunct to the human immune system, providing colonization resistance against pathogens and modulating immune responses. This rationale underpins probiotic therapies and justifies prudent antibiotic use to preserve these protective functions [1].
Technological and Analytical Foundations
Advances in core technologies have been instrumental in translating these conceptual models into therapeutic candidates:
- Multi-OMICS Integration: The combined application of metagenomics, metatranscriptomics, metabolomics, and proteomics provides a comprehensive view of microbial community structure, function, and metabolic output. This integration is essential for identifying therapeutic targets and biomarkers [11].
- High-Throughput Culturing Techniques: Improved methods for cultivating previously "unculturable" microbes have expanded the library of strains available for defined consortia development, moving the field beyond donor-derived fecal microbiota transplantation [36].
- Artificial Intelligence and Machine Learning: AI platforms analyze complex multi-OMICS datasets to identify predictive signatures of disease, stratify patients, and personalize therapeutic interventions [36].
- Gnotobiotic Animal Models: Germ-free animals provide a controlled system for establishing causal relationships between microbial communities and host phenotypes, enabling rigorous testing of therapeutic candidates [1].
Table 1: Core Conceptual Frameworks in Microbiome Therapeutics
| Conceptual Model | Key Principle | Therapeutic Implication |
|---|---|---|
| Innate and Adaptive Genomes | The microbiome constitutes an acquired "adaptive genome" | Explains interindividual variability in drug response; enables personalized microbiome medicine |
| Slave Tissue Hypothesis | Microbial communities function as exogenous tissues under host control | Provides rationale for manipulating microbiome as a tissue-like therapeutic target |
| Health-Illness Conversion Model | Disease results from specific dysbiosis patterns | Enables targeted reversal of defined dysbiotic states rather than broad microbial manipulation |
| Acquired Microbial Immunity | Microbiome provides colonization resistance and immune education | Supports development of probiotics for pathogen protection and immunomodulation |
The Clinical Pipeline: From rCDI to Novel Indications
Market Landscape and Growth Dynamics
The microbiome therapeutics market has demonstrated explosive growth potential, with the global market size estimated at approximately $990 million in 2024 and projected to exceed $5.1 billion by 2030, representing a compound annual growth rate (CAGR) of 31% [36]. This growth is underpinned by the first regulatory approvals of microbiome-based products, which have de-risked the regulatory pathway for subsequent candidates. The market bifurcates into prescription therapeutics (including Live Biotherapeutic Products [LBPs] and Fecal Microbiota Transplantation [FMT]) and non-prescription products (including diagnostics, nutrition-based interventions, and personal care) [36]. LBPs are anticipated to become the dominant category, expanding from $425 million in 2024 to $2.39 billion in 2030, overtaking FMT as the leading therapeutic modality [36].
Geographically, North America remains the largest market, but the Asia Pacific region shows the most rapid growth (34.7% CAGR), increasing from $213 million in 2024 to $1.27 billion in 2030, driven by regulatory pilots in China, innovation in Japan, and India's emergence as a clinical trial hub [36]. The pipeline's scope is substantial, with approximately 243 candidates in development across more than 100 companies, spanning all phases of clinical testing and a broadening spectrum of therapeutic areas [36]. The distribution of candidates by development stage reflects a sector still in early translation, with an estimated 60% of programs in preclinical stages, 20% in Phase I, 15% in Phase II, and less than 5% in Phase III trials [36].
Pipeline Composition by Therapeutic Area
Gastrointestinal Disorders
Gastrointestinal conditions, particularly rCDI, remain the most established indication for microbiome therapeutics, with two FDA-approved products already on the market:
- REBYOTA (RBX2660): A rectally administered fecal microbiota suspension that restores broad microbial diversity; approved for rCDI [36].
- VOWST (SER-109): An oral live biotherapeutic containing purified Firmicutes spores that recolonize the gut, restore bile acid metabolism, and outcompete C. difficile; approved for rCDI [36].
The pipeline continues to expand with late-stage candidates featuring novel mechanisms:
- VE303 (Vedanta Biosciences): A defined eight-strain bacterial consortium that promotes colonization resistance and bile acid metabolism to suppress C. difficile; currently in Phase III development for rCDI prevention [38] [36].
- Ibezapolstat (Acurx Pharmaceuticals): A novel oral antibiotic from a new class of DNA polymerase IIIC inhibitors that specifically targets C. difficile while preserving beneficial gut bacteria; Phase 3-ready with international trials planned [39] [38] [40].
- MBK-01 (Mikrobiomik): An investigational therapy derived from fecal microbiota transplantation, formulated as Full-spectrum Purified Intestinal Microbiota (FSPIM) in lyophilized oral capsules; expected to become Europe's "first intestinal microbiota-based biologic" with commercial launch projected for 2027 [38].
Beyond rCDI, the pipeline includes candidates for other gastrointestinal conditions:
- VE202 (Vedanta Biosciences): An eight-strain consortium designed to induce regulatory T-cell responses and produce anti-inflammatory metabolites; in Phase II for ulcerative colitis [36].
- MaaT013 (MaaT Pharma): A pooled FMT product designed to deliver diverse gut communities to restore immune homeostasis; in Phase III for graft-versus-host disease [39] [36].
Oncology Applications
The microbiome pipeline has expanded significantly into oncology, with candidates designed to modulate response to cancer immunotherapy, directly exert anti-tumor activity, or manage treatment side effects:
- MRx0518 (4D Pharma): A single-strain Bifidobacterium longum engineered to activate innate and adaptive immunity and augment checkpoint inhibitors; in Phase I/II trials for solid tumors [36].
- EO2401 (Enterome): An "onco-mimic" therapy comprising peptides from the gut microbiome that mimic tumor antigens to train immunity; in Phase I/II for glioblastoma and adrenal tumors [36].
- MB097 (Microbiotica): A live biotherapeutic product being developed to complement immuno-oncology treatments, including MSD's anti-PD-1 therapy KEYTRUDA (pembrolizumab) [39].
Metabolic and Other Disorders
The pipeline further diversifies into metabolic, neurologic, and rare genetic disorders:
- Akkermansia Therapeutics (Ak02): Pasteurized Akkermansia muciniphila developed to improve insulin sensitivity and weight control; in Phase I/II for metabolic disorders [36].
- SYNB1934 (Synlogic): Engineered E. coli Nissle expressing phenylalanine ammonia lyase to convert phenylalanine into trans-cinnamic acid; in Phase II for phenylketonuria (PKU) [36].
- Oxabact (OXA1, OxThera): Live Oxalobacter formigenes that degrades intestinal oxalate to lower systemic oxalate levels; in Phase III for primary hyperoxaluria and chronic kidney disease [36].
- ST-598 (Siolta Therapeutics): A rationally designed infant-microbiota supplement to prevent atopic disease; in Phase II [36].
Table 2: Selected Microbiome Therapeutics in Clinical Development
| Company / Product | Indication(s) | Modality & Mechanism | Development Stage |
|---|---|---|---|
| Seres Therapeutics - Vowst (SER-109) | rCDI; exploring ulcerative colitis | Oral LBP; purified Firmicutes spores | Approved |
| Vedanta Biosciences - VE303 | rCDI | Defined 8-strain bacterial consortium | Phase III |
| Acurx Pharmaceuticals - Ibezapolstat | CDI | DNA pol IIIC inhibitor antibiotic | Phase 3-ready |
| Mikrobiomik - MBK-01 | rCDI | Oral FMT capsules | Phase III |
| 4D Pharma - MRx0518 | Solid tumors | Single-strain B. longum for immune activation | Phase I/II |
| Synlogic - SYNB1934 | Phenylketonuria (PKU) | Engineered E. coli Nissle | Phase II |
| Akkermansia Therapeutics - Ak02 | Metabolic disorders | Pasteurized A. muciniphila | Phase I/II |
| Siolta Therapeutics - ST-598 | Allergy prevention | Infant microbiota supplement | Phase II |
| Eligo Bioscience - Eligobiotics | Carbapenem-resistant infections | CRISPR-guided bacteriophages | Phase I |
| Finch Therapeutics - CP101 | rCDI; exploring IBD | Full-spectrum microbiota consortium | Phase II/III |
Experimental Models and Methodologies
Standardized Workflows for Microbiome Analysis
Robust experimental protocols are essential for generating reproducible data in microbiome research. The following workflow represents a standardized approach for assessing therapeutic efficacy in preclinical models:
- Sample Collection and Preservation: Biological samples (stool, mucosal biopsies, etc.) are collected using standardized kits that stabilize microbial DNA/RNA at the point of collection, typically using solutions that inhibit nuclease activity and prevent microbial growth.
- Nucleic Acid Extraction: Automated extraction methods employing bead-beating mechanical lysis ensure comprehensive disruption of diverse microbial cell walls, followed by purification columns to remove PCR inhibitors.
- Library Preparation and Sequencing: Amplification of the 16S rRNA gene (for taxonomic profiling) or shotgun metagenomic sequencing (for functional potential) using platform-specific adapters and barcodes to enable multiplexing.
- Bioinformatic Analysis: Processing of raw sequences through quality filtering, removal of human reads, clustering into operational taxonomic units (OTUs) or amplicon sequence variants (ASVs), and taxonomic assignment using reference databases.
- Statistical and Functional Analysis: Multivariate statistical methods (PCoA, PERMANOVA) to identify community differences, followed by phylogenetic investigation of communities by reconstruction of unobserved states (PICRUSt2) for metagenome prediction or HUMAnN2 for pathway analysis of shotgun data.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Microbiome Therapeutic Development
| Research Reagent | Function and Application | Technical Considerations |
|---|---|---|
| DNA Stabilization Buffers | Preserve microbial community structure at collection | Critical for accurate representation of low-abundance taxa; eliminates room temperature shipping bias |
| Mock Community Standards | Quality control for sequencing and bioinformatic workflows | Contain defined mixtures of microbial genomes; enable assessment of technical variability and detection limits |
| Gnotobiotic Mice | Causality testing of microbial communities | Germ-free animals allow colonization with defined communities; essential for establishing mechanism of action |
| Anaerobic Culturing Systems | Isolation and expansion of obligate anaerobic species | Required for working with oxygen-sensitive gut commensals; essential for producing defined consortia |
| Mass Spectrometry Standards | Quantification of microbial metabolites | Enable absolute quantification of SCFAs, bile acids, neurotransmitters in host tissues and biofluids |
| Cell Culture Media | In vitro models of host-microbe interactions | Simulate gut environment (oxygen tension, pH, nutrients) to maintain microbial viability during co-culture with host cells |
| Fmoc-Gly-Pro-Hyp-OH | Fmoc-Gly-Pro-Hyp-OH Collagen Mimetic Tripeptide | |
| Epanorin | Epanorin|Lichen Metabolite for Cancer Research | Epanorin is a lichen secondary metabolite that inhibits MCF-7 breast cancer cell proliferation. For Research Use Only. Not for human use. |
Visualizing Therapeutic Development Pathways
The development pathway for microbiome therapeutics involves distinct stages from candidate selection to clinical application, with key decision points determining progression. The schematic below illustrates this workflow, highlighting critical validation checkpoints.
Emerging Modalities and Technical Innovations
Next-Generation Therapeutic Platforms
The microbiome therapeutic landscape is evolving beyond first-generation FMT products toward precisely engineered solutions:
- Defined Bacterial Consortia: These products comprise specific combinations of bacterial strains selected for complementary functions. Unlike donor-derived FMT, they offer batch-to-batch consistency and eliminat donor variability. VE303 exemplifies this approach with its eight precisely selected strains manufactured from pure clonal bacterial cell banks [38].
- Engineered Microbial Therapeutics: Synthetic biology approaches are being used to design microorganisms with enhanced therapeutic functions. SYNB1934 represents this category – an engineered E. coli Nissle strain modified to express phenylalanine ammonia lyase for treating phenylketonuria [36].
- CRISPR-Based Phage Therapies: These precision antimicrobials use bacteriophages equipped with CRISPR-Cas systems to selectively eliminate pathogenic bacteria while sparing commensals. Eligobiotics (Eligo Bioscience) and SNIPR001 (SNIPR Biome) represent this novel approach for targeting antibiotic-resistant bacteria [36].
- Microbiome-Derived Biologics: Rather than live microbes, this modality isolates beneficial microbial metabolites, proteins, or polysaccharides for therapeutic use. Second Genome's SG-3, a microbiome-derived peptide targeting immune pathways, exemplifies this approach [36].
Mechanism of Action: Pathways and Targets
Microbiome therapeutics exert their effects through several key mechanistic pathways that can be visualized as interconnected networks:
The primary mechanisms through which microbiome therapies achieve clinical benefits include:
- Microbiome-Mediated Bile Acid Metabolism: Interventions like ibezapolstat and VE303 modify the bile acid pool by sparing or introducing bacteria that transform primary bile acids into secondary bile acids, creating an environment hostile to C. difficile while supporting commensals [40].
- Short-Chain Fatty Acid (SCFA) Production: Therapeutic microbes produce SCFAs like butyrate, propionate, and acetate through fermentation of dietary fiber. These metabolites strengthen epithelial barrier function, modulate immune responses, and regulate host metabolism [11].
- Colonization Resistance: Defined bacterial consortia occupy ecological niches and consume resources that would otherwise support pathogens, while producing bacteriocins that directly inhibit competing microbes [1].
- Immune System Priming: Certain microbiome therapeutics train the immune system by modulating regulatory T-cell populations, dendritic cell function, and cytokine profiles, resulting in systemic anti-inflammatory effects or enhanced anti-tumor immunity [11] [36].
Regulatory and Manufacturing Considerations
Evolving Regulatory Frameworks
The regulatory landscape for microbiome-based therapies has matured significantly with the first FDA approvals of FMT-based products and LBPs. Key developments include:
- Establishment of LBP Category: Regulatory agencies now recognize Live Biotherapeutic Products as a distinct class, simplifying clinical trial design and manufacturing guidelines. This categorization has de-risked investment in the sector [36].
- Standardized Efficacy Endpoints: For rCDI trials, sustained clinical cure has emerged as the standard endpoint, typically defined as resolution of diarrhea without recurrence at 8 weeks post-treatment [38].
- Pediatric Development Plans: Regulatory agencies are requiring pediatric investigation plans (PIPs) for microbiome therapeutics, as evidenced by the EMA's approval of Mikrobiomik's PIP for MBK-01 in children with CDI [38].
Advanced Manufacturing Platforms
Manufacturing consistency represents a critical challenge for microbiome therapeutics, with distinct approaches emerging:
- Donor-Derived FMT Platforms: Products like REBYOTA utilize standardized donor screening, stool processing, and purification protocols to minimize variability while retaining microbial diversity [36].
- Defined Consortia Production: Companies like Vedanta Biosciences manufacture products like VE303 from pure clonal bacterial cell banks, resulting in a consistent powdered formulation that eliminates donor variability [38].
- Proprietary Production Systems: Lumen Bioscience's spirulina-based GMP manufacturing platform enables cost-effective production of biologic combinations like LMN-201, an oral capsule therapy for CDI [39].
The clinical pipeline of microbiome therapeutics has evolved from a narrow focus on rCDI to a diverse landscape addressing oncology, metabolic disorders, and rare diseases. With over 230 candidates in development and the market projected to exceed $5 billion by 2030, the field has transitioned from proof-of-concept to established therapeutic modality [36]. The continued expansion of this pipeline will be fueled by several converging trends: the elucidation of mechanism of action for increasingly sophisticated candidates, the development of standardized regulatory pathways, and advances in manufacturing that ensure product consistency [11].
Future development will likely focus on personalized microbiome therapeutics tailored to an individual's microbial baseline, combination approaches that pair microbiome therapies with conventional drugs to enhance efficacy, and expansion into new indications where host-microbe interactions play a defining role in disease pathogenesis. The ongoing translation of microbiome science into clinical practice represents a paradigm shift in therapeutic development, moving beyond the traditional "one drug, one target" model toward ecological restoration of the human microbial organ system. As the field matures, microbiome-based interventions are poised to become integral components of precision medicine across a broadening spectrum of human diseases.
The human microbiome, once regarded as a passive passenger, is now recognized as a dynamic and essential determinant of human physiology, shaping immunity, metabolism, neurodevelopment, and therapeutic responsiveness across the lifespan [11]. Microbiome-guided precision medicine represents a paradigm shift in clinical science, offering a targetable axis in the landscape of individualized therapeutics [41]. This approach moves beyond descriptive associations to intervention-ready, mechanistically grounded models that position the human microbiome at the center of precision medicine [11]. The clinical translation of this knowledge has begun to redefine early-life programming, cardiometabolic regulation, immune homeostasis, neuropsychiatric resilience, and cancer therapy response [11]. This technical guide examines the diagnostic frameworks, stratification methodologies, and tailored intervention strategies enabling the transition of microbiome science from bench to bedside, framed within the broader context of human microbiome distribution, anatomy, development, and stabilization research.
Scientific Foundations and Mechanistic Insights
Core Mechanistic Pathways in Host-Microbiome Interactions
The microbiome influences host physiology through three primary mechanistic pathways: immune modulation, metabolic transformation, and gene regulation [41]. Microbial metabolites and structural components serve as central conduits for these interactions, influencing immune homeostasis across both mucosal and systemic compartments [11].
Table 1: Core Mechanistic Pathways of Microbiome-Host Interaction
| Mechanistic Pathway | Key Microbial Components | Host Systems Affected | Clinical Implications |
|---|---|---|---|
| Immune Modulation | Microbial-associated molecular patterns (MAMPs), Short-chain fatty acids (SCFAs) | Mucosal immunity, Systemic inflammation, T-cell differentiation | Inflammatory bowel disease, Autoimmune disorders, Cancer immunotherapy response |
| Metabolic Transformation | Bile acid derivatives, Tryptophan metabolites, Neurotransmitters | Energy harvest, Insulin signaling, Blood-brain barrier function | Obesity, Type 2 diabetes, Neuropsychiatric conditions |
| Gene Regulation | Histone deacetylase inhibitors, Methyl donors | Epigenetic modifications, Transcriptional networks | Cellular differentiation, Carcinogenesis, Transgenerational effects |
Early Life Microbiome Development and Stabilization
Early life represents a critical period for microbiome assembly with long-lasting effects on host physiology [42]. The developmental trajectory of the gut microbiome from infancy through adulthood provides a foundational framework for targeted therapeutic strategies [11]. Colonization begins at birth and is largely dictated by maternal microbial transmission and environmental exposures [11]. Vaginal delivery facilitates maternal transfer of Lactobacillus, Prevotella, and Sneathia, while cesarean delivery is associated with enrichment of skin-derived taxa such as Staphylococcus and Corynebacterium [11]. This early divergence has been linked to increased risk of immune dysregulation and metabolic disorders later in life [11].
The gut microbiome generally reaches a stable, adult-like configuration by approximately 2–3 years of age, establishing a core microbiome that provides functional resilience but remains modifiable throughout life [11]. Postnatal nutrition plays a critical role in this developmental process, with breastfeeding delivering maternal microbes and bioactive compounds, notably human milk oligosaccharides (HMOs), which are pivotal in guiding microbial colonization, particularly of Bifidobacterium infantis [11].
Diagnostic Approaches and Multi-Omics Technologies
Multi-Omics Integration for Microbiome Profiling
Advanced multi-omics technologies provide integrative tools that generate a systems-level understanding of host–microbe interactions [41]. The convergence of metagenomics, metatranscriptomics, metaproteomics, and metabolomics enables comprehensive functional profiling beyond taxonomic classification.
Table 2: Multi-Omics Technologies for Microbiome Analysis
| Technology | Analytical Focus | Resolution | Clinical Applications | Limitations |
|---|---|---|---|---|
| Metagenomics | Microbial gene content | Species to strain level | Pathogen detection, Functional potential | Does not measure active transcription |
| Metatranscriptomics | Gene expression patterns | Community transcriptome | Active metabolic pathways, Response to interventions | RNA stability, Technical variation |
| Metaproteomics | Protein expression | Functional proteome | Enzyme activity, Host response proteins | Analytical complexity, Database dependence |
| Metabolomics | Metabolic outputs | Metabolic phenotype | Functional readout of microbial activity | Host vs. microbial source attribution |
Computational Frameworks and Data Integration
Computational frameworks for data integration and interpretation are essential for translating multi-omics data into clinically actionable insights [41]. Constraint-based metabolic modeling has emerged as a powerful approach to overcome the complexity of microbiota-host interactions. This method builds on in silico representations of metabolic networks of individual species—genome-scale metabolic networks—and allows prediction of metabolic fluxes in individual species or entire communities [43].
Recent research combining metagenomics, transcriptomics, and metabolomics from aging mice with metabolic modeling demonstrated a pronounced reduction in metabolic activity within the aging microbiome accompanied by reduced beneficial interactions between bacterial species [43]. These changes coincided with increased systemic inflammation and the downregulation of essential host pathways, particularly in nucleotide metabolism, predicted to rely on the microbiota and critical for preserving intestinal barrier function, cellular replication, and homeostasis [43].
Patient Stratification Strategies
Microbiome-Based Biomarkers for Disease Subtyping
Patient stratification in microbiome medicine utilizes microbial signatures to categorize individuals into subgroups with distinct disease risks, therapeutic responses, or clinical outcomes. Research has revealed that the proportions of microbes such as Bacteroides, Bifidobacterium and Prevotella have well-studied roles in conditions such as obesity and inflammatory bowel disease, but these organisms have very different patterns of abundance in world regions outside of Europe and North America, calling into question the applicability of findings from Western-centric studies to global populations [44].
Large-scale initiatives are addressing these disparities. The Human Microbiome Compendium represents one such effort, uniformly processing more than 160,000 gut microbiome samples from 68 nations—the largest publicly available dataset of its kind [44]. This resource enables identification of patterns that would not be detectable in smaller, geographically restricted studies and highlights the discovery rate phenomenon, where adding samples from underrepresented regions uncovers substantially more information about microbial identity and abundance [44].
Global Representation in Microbiome Research
A significant challenge in microbiome-based patient stratification is the substantial geographic bias in existing research. Most published studies focus on populations from high-income regions such as North America and Europe, limiting the generalizability of microbiome-health associations [45]. Underrepresentation of populations from low- and middle-income countries in the microbiome literature is compounded by computational barriers, including biases in reference databases, nonrepresentative metadata, and infrastructure limitations [45].
Table 3: Global Representation in Gut Microbiome Studies
| World Region | Representation in Studies | Distinct Microbial Features | Health Implications |
|---|---|---|---|
| North America | Heavily overrepresented | High Bacteroides prevalence | Baseline for most current references |
| Europe | Heavily overrepresented | Moderate Bifidobacterium levels | Well-characterized in disease associations |
| Asia | Moderately represented | Variable Prevotella levels | Distinct metabolic phenotypes |
| South America | Underrepresented | Unique fermented food adaptations | Potential novel probiotic candidates |
| Africa | Severely underrepresented | High microbial diversity | Protective effects against inflammatory diseases |
Therapeutic Interventions and Tailored Approaches
Microbiome-Targeted Therapeutic Modalities
Therapeutic manipulation of the microbiome encompasses multiple intervention strategies ranging from wholesale community transplantation to precisely engineered microbial therapeutics.
Fecal Microbiota Transplantation (FMT): FMT represents the most direct approach to microbiome modification, transferring an entire microbial community from a healthy donor to a recipient. While most established for recurrent Clostridioides difficile infection, FMT is being investigated for other conditions including inflammatory bowel disease, metabolic syndrome, and neurological disorders [11].
Engineered Probiotics and Live Biotherapeutics: Synthetic biology approaches are being used to design engineered probiotics with enhanced therapeutic functions. These include microorganisms engineered to produce anti-inflammatory molecules, deliver therapeutic enzymes, or compete with pathogens for ecological niches [41]. For example, strains of Bifidobacterium infantis are being developed to restore the protective functions disrupted by antibiotic exposure or cesarean birth [11].
Precision Nutrition and Microbiome-Directed Foods: Targeted nutritional interventions based on individual microbiome composition represent a non-invasive approach to microbiome modulation. Precision nutrition strategies use microbiome profiling to recommend personalized dietary patterns that support beneficial microbial functions, such as the production of short-chain fatty acids or the metabolism of specific bile acids [11].
Bacteriophage Therapy: Phage consortia targeting specific bacterial pathogens offer a precise approach to microbiome editing without broad-spectrum disruption. For example, phage cocktails targeting Klebsiella pneumoniae have shown promise in attenuating inflammation in inflammatory bowel disease contexts [11].
Experimental Protocols for Microbiome Therapeutic Development
Protocol 1: Fecal Microbiota Transplantation for Clinical Research
Materials:
- Sterile collection containers with anaerobic gas generators
- Normal saline or glycerol-based cryopreservation solution
- Laboratory blender or stomacher for homogenization
- Filtration system (stainless steel or mesh filters)
- Administration equipment (colonoscopy supplies, nasojejunal tubes, or encapsulation materials)
Methodology:
- Donor screening: Comprehensive medical history and laboratory testing for enteric pathogens
- Sample processing: Fresh stool processed within 6 hours of collection under anaerobic conditions
- Homogenization: Stool mixed with cryopreservation solution at 1:1 to 1:5 ratio (w/v)
- Filtration: Sequential filtration through mesh filters (500μm to 106μm) to remove particulate matter
- Quality control: Aliquots taken for microbial viability testing and pathogen screening
- Administration: Delivery via colonoscopy, enema, oral capsules, or nasoduodenal tube
- Efficacy assessment: Pre- and post-treatment microbiome profiling using shotgun metagenomics
Protocol 2: Metabolic Modeling for Therapeutic Target Identification
Materials:
- High-performance computing infrastructure
- Genome-scale metabolic reconstructions (e.g., AGORA, VMH databases)
- Constraint-based modeling software (e.g., COBRA Toolbox, MICOM)
- Metagenomic sequencing data from patient cohorts
- Metabolomic profiling data (LC-MS, GC-MS)
Methodology:
- Data acquisition: Collection of multi-omics datasets (metagenomics, metabolomics, host transcriptomics)
- Model reconstruction: Construction of personalized microbiome metabolic models using template-based approaches
- Integration: Building integrated host-microbiome models representing metabolic interactions
- Simulation: Performing flux balance analysis under different nutritional and therapeutic conditions
- Identification: Pinpointing critical microbial functions and metabolites influencing host pathways
- Validation: Experimental verification of predicted targets using in vitro or animal models
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Microbiome Medicine
| Research Reagent | Function/Application | Technical Considerations |
|---|---|---|
| 16S rRNA Gene Primers | Amplification of hypervariable regions for taxonomic profiling | Primer selection impacts taxonomic resolution and bias |
| Shotgun Metagenomic Kits | Library preparation for whole-genome sequencing | Enable strain-level resolution and functional gene analysis |
| Anaerobic Chamber | Maintenance of oxygen-sensitive microorganisms during processing | Essential for cultivating obligate anaerobes without viability loss |
| Metabolomic Standards | Quantitative analysis of microbial metabolites (SCFAs, bile acids) | Isotope-labeled internal standards required for absolute quantification |
| Genome-Scale Metabolic Models | In silico prediction of microbial community metabolic fluxes | AGORA and VMH databases provide curated reconstructions |
| Gnotobiotic Animal Models | Investigation of host-microbe interactions in controlled systems | Germ-free animals enable defined microbial community studies |
| Cell Culture Systems | Modeling host-microbe interactions at cellular level | Enteroid and organoid cultures replicate gut physiology |
| VU 0360223 | VU 0360223, MF:C15H9FN2S, MW:268.31 g/mol | Chemical Reagent |
| Berninamycin A | Berninamycin A, CAS:58798-97-3, MF:C51H51N15O15S, MW:1146.1 g/mol | Chemical Reagent |
Implementation Challenges and Future Directions
Addressing Technical and Ethical Complexities
The translation of microbiome science into clinical practice faces several persistent challenges. Inter-individual variability represents a fundamental barrier, as microbiome composition and function are influenced by diet, geography, host genetics, antibiotic exposure, and age [11]. This variability complicates the development of universally applicable diagnostic and therapeutic tools [11]. Additional challenges include data standardization across studies, incomplete functional annotation of microbial "dark matter," and the absence of validated biomarkers [11].
Ethical and regulatory complexities surrounding microbiome-based therapies also present significant hurdles. Fecal microbiota transplantation exists in a regulatory gray area in many jurisdictions, while engineered probiotics and other novel microbiome therapeutics face evolving regulatory pathways [41]. Equitable access to microbiome-based therapies represents another ethical consideration, particularly given the geographic disparities in microbiome research and the potential for high costs associated with personalized microbiome interventions.
Emerging Solutions and Innovative Approaches
Several emerging solutions address these challenges:
- Decision-Support Algorithms: Computational frameworks that integrate multi-omics data with clinical metadata to guide therapeutic decisions [41]
- Standardized Methodologies: Efforts to harmonize sampling, sequencing, and analytical protocols across research centers [11]
- Longitudinal Study Designs: Research capturing microbiome dynamics over time and in response to interventions [11]
- Enhanced Visualization Tools: Innovative approaches like MicroLabVR, which provides interactive 3D visualization of simulated spatiotemporal microbiome data in virtual reality, helping researchers explore complex datasets in an immersive environment [46]
The future of personalized microbiome medicine lies in collaborative, mechanistically anchored, and longitudinal approaches that fully translate microbiome science into actionable precision health strategies [41]. As research continues to unravel the complex relationships between microbial communities and human health, microbiome-guided diagnostics and therapeutics are poised to become integral components of personalized medicine, transforming concepts of disease etiology, therapeutic design, and the future of individualized healthcare [11].
The human microbiome has evolved from a scientific curiosity to a frontier of biotherapeutic innovation, with the global market projected to grow from approximately $990 million in 2024 to $5.1 billion by 2030, representing a compound annual growth rate of 31% [36]. This growth is catalyzed by the first regulatory approvals of microbiome-based therapies which have validated the entire field. These pioneering therapies address a critical medical challenge: recurrent Clostridioides difficile infection (rCDI), a condition emblematic of microbiome dysbiosis where standard antibiotic treatments perpetuate a cycle of recurrence by further disrupting gut microbial ecology [47] [48]. This whitepaper provides a technical analysis of the two approved microbiome therapies—Rebyota and Vowst—and the most advanced clinical candidates in late-stage development, framing their development within the broader context of human microbiome anatomy, distribution, and stabilization research. The analysis integrates detailed product profiles, quantitative clinical data, experimental methodologies, and the essential research tools driving this rapidly advancing field.
Approved Microbiome Therapies
The U.S. Food and Drug Administration (FDA) has approved two microbiota-based products for preventing rCDI, establishing a regulatory pathway for live biotherapeutic products (LBPs). Both target the same indication but employ distinct technological approaches.
REBYOTA (fecal microbiota, live – jslm)
- Technology Profile: REBYOTA is a fecal microbiota transplant (FMT) product, derived from standardized, pre-screened donor stool. It is a broad-consortium, rectally administered suspension containing up to trillions of live microbes, including Bacteroides species [47] [49].
- Mechanism of Action: It aims to restore a healthy gut microbiome by directly introducing a diverse microbial community, thereby outcompeting C. difficile and re-establishing colonization resistance [48].
- Clinical Evidence and Protocol: The Phase 3b CDI-SCOPE trial (NCT05831189) was a single-arm study evaluating a single 150 mL dose administered via colonoscopy to the right colon after a 24- to 72-hour antibiotic washout period [48].
- Efficacy: The 8-week analysis showed a 95.1% treatment success rate (no CDI recurrence). Through 6 months, 92.7% of participants remained recurrence-free [48].
- Microbiome Analysis: Metagenomic sequencing in a subset of patients (n=20) showed a significant, sustained shift in microbiome composition toward the REBYOTA profile. Beneficial bacteria (Bacteroidia and Clostridia) increased, while pathogenic classes (Gammaproteobacteria and Bacilli) decreased. The Microbiome Health Index (MHI-A) showed a sustained increase through 6 months, indicating a shift away from a dysbiotic state [47] [49].
- Safety: The 6-month data showed a favorable safety profile. Only 9.8% of participants experienced related treatment-emergent adverse events (TEAEs), all mild and gastrointestinal. No related serious adverse events were reported [48].
VOWST (SER-109)
- Technology Profile: VOWST is an oral, purified, spore-based live biotherapeutic. It is manufactured from firmicutes spores sourced from qualified donors and undergoes ethanol inactivation and purification to remove vegetative bacteria and pathogens [50].
- Mechanism of Action: While its exact mechanism is not fully established, VOWST is hypothesized to facilitate microbiome restoration and inhibit C. difficile spore germination following antibiotic treatment. The purified Firmicutes spores are designed to recolonize the gut, restore bile acid metabolism, and outcompete C. difficile [36] [50].
- Clinical Evidence and Protocol: The ECOSPOR III trial was a randomized, placebo-controlled, double-blind study.
- Engraftment Data: An exploratory endpoint used metagenomic sequencing to track bacterial engraftment. The data showed that the number of VOWST dose species was greater in the treatment group compared to placebo at week 1 and remained higher through week 8, demonstrating colonization [50].
- Efficacy: The trial demonstrated a high rate of efficacy in preventing rCDI, leading to its FDA approval [36].
- Safety: The therapy was well-tolerated, with a safety profile supporting its use in a vulnerable patient population [50].
Table 1: Comparison of Approved Microbiome Therapies for rCDI
| Feature | REBYOTA (fecal microbiota, live – jslm) | VOWST (SER-109) |
|---|---|---|
| Manufacturer | Ferring Pharmaceuticals (Rebiotix) | Seres Therapeutics/Nestlé Health Science |
| Product Type | Fecal Microbiota Transplant (FMT) | Purified Live Biotherapeutic Product (LBP) |
| Mechanism | Restores broad microbial diversity | Purified Firmicutes spores reconstitute microbiome & bile acid metabolism |
| Administration | Rectal (single dose via colonoscopy/enema) | Oral (capsules, multi-dose over 3 days) |
| Key Trial | Phase 3b CDI-SCOPE | Phase 3 ECOSPOR III |
| Efficacy (Prevention) | 95.1% at 8 weeks; 92.7% at 6 months | Statistically significant reduction vs. placebo |
| Microbiome Analysis | Increased MHI-A, diversity; beneficial taxa engraftment | Dose species engraftment confirmed via metagenomics |
| Common AEs | Mild GI events (abdominal pain, diarrhea, bloating) | Well-tolerated, detailed profile in prescribing information |
Late-Stage Clinical Pipeline
The microbiome therapeutic pipeline has expanded significantly beyond rCDI, with over 240 candidates in development [36]. The following table summarizes promising late-stage clinical candidates.
Table 2: Select Late-Stage Clinical Microbiome Candidates (as of September 2025)
| Company / Product | Indication(s) | Modality & Mechanism | Development Stage |
|---|---|---|---|
| Vedanta Biosciences - VE303 | rCDI | Defined, rationally designed 8-strain bacterial consortium; promotes colonization resistance | Phase 3 (RESTORATiVE303) |
| Vedanta Biosciences - VE202 | Ulcerative Colitis (UC) | 8-strain consortium designed to induce regulatory T-cells & anti-inflammatory metabolites | Phase 2 (Did not meet primary endpoint) [51] |
| MaaT Pharma - MaaT013 | Graft-versus-host disease (GvHD) | Pooled, full-ecosystem FMT product; restores gut diversity for immune homeostasis | Phase 3 |
| 4D Pharma - MRx0518 | Oncology (solid tumors) | Single-strain Bifidobacterium longum; activates innate/adaptive immunity with checkpoint inhibitors | Phase I/II |
| OxThera - Oxabact (OXA1) | Primary Hyperoxaluria & Chronic Kidney Disease | Live Oxalobacter formigenes that degrades intestinal oxalate to lower systemic levels | Phase III |
| Finch Therapeutics - CP101 | rCDI; exploring IBD | Full-spectrum microbiota consortium (FSM) delivering complete communities via oral capsules | Phase II/III |
| Synlogic - SYNB1934 | Phenylketonuria (PKU) | Engineered E. coli Nissle expressing phenylalanine ammonia lyase to metabolize phenylalanine | Phase II |
| Eligo Bioscience - Eligobiotics | Carbapenem-resistant infections | CRISPR-guided bacteriophages to selectively eliminate antibiotic-resistant bacteria | Phase I |
Key Pipeline Insights:
- Therapeutic Diversification: While gastrointestinal disorders (rCDI, IBD) remain a core focus, the pipeline shows rapid expansion into oncology, metabolic, autoimmune, and rare genetic diseases [36].
- Modality Evolution: The pipeline showcases a shift from undefined FMTs to defined bacterial consortia (e.g., Vedanta), and further to engineered microbes (e.g., Synlogic) and synthetic biology solutions like CRISPR-phages (e.g., Eligo) [36].
- Clinical Attrition: The field is not without challenges. The recent failure of Vedanta's VE202 in a Phase 2 ulcerative colitis study highlights the hurdles in translating microbiome science to efficacy in complex immune-mediated diseases [51].
Experimental Protocols & Methodologies
The development of microbiome therapies relies on sophisticated experimental workflows to establish safety, efficacy, and mechanism of action.
Clinical Trial Protocol: FMT Administration & Long-Term Follow-up
The CDI-SCOPE trial for REBYOTA provides a template for evaluating microbiota therapies [48].
- Participant Selection: Adults (≥18 years) with recurrent CDI (≥1 recurrence or ≥2 episodes) and a positive stool test for C. difficile toxin, following completion of standard-of-care antibiotics.
- Intervention Protocol:
- Antibiotic Washout: A 24- to 72-hour washout period after the last antibiotic dose.
- Bowel Preparation: Standard bowel preparation as per investigator discretion for colonoscopy.
- Product Administration: A single 150 mL dose of the microbiota suspension is delivered via colonoscopy to the right colon (between ileocecal valve and hepatic flexure).
- Endpoints:
- Primary Safety: Incidence of treatment-related TEAEs through 8 weeks.
- Primary Efficacy: Treatment success, defined as the absence of CDI recurrence (no CDI-associated diarrhea and a positive toxin test) for 8 weeks.
- Exploratory/Long-term: Safety and further CDI episodes assessed at 3 and 6 months. Microbiome composition analyzed via stool metagenomics at baseline, 1, 2, 4, 8 weeks, and 6 months.
- Statistical Analysis: Descriptive statistics are used for safety and efficacy analyses in this single-arm trial. Categorical data are summarized with counts and percentages.
Microbiome Engraftment Analysis Protocol
The engraftment analysis for VOWST exemplifies how to track microbial colonization [50].
- Sample Collection: Stool specimens are collected from trial participants at predefined timepoints (e.g., baseline, weeks 1, 2, and 8).
- Sequencing & Bioinformatic Processing:
- DNA Extraction: Microbial DNA is extracted from all stool samples.
- Whole Metagenomic Sequencing: Shotgun sequencing is performed on the extracted DNA to achieve strain-level resolution.
- Strain Tracking: Bioinformatics pipelines are used to align sequencing reads to a reference database containing the strains present in the therapeutic dose. This allows for the identification and quantification of "engrafting" dose species in the recipient's microbiome over time.
- Data Interpretation: The number and abundance of engrafted dose species are compared between treatment and placebo groups to confirm colonization and persistence.
The following diagram illustrates the core mechanism of action shared by these therapies in breaking the cycle of rCDI.
The Scientist's Toolkit: Key Research Reagents & Materials
The advancement of microbiome therapies depends on a suite of specialized tools and reagents.
Table 3: Essential Research Reagents and Solutions for Microbiome Therapeutic Development
| Tool / Reagent | Function & Application |
|---|---|
| Whole Metagenomic Sequencing | Provides strain-level resolution and functional gene profiling of microbial communities; used for engraftment analysis, biomarker discovery, and quality control [36] [50]. |
| Culturomics & Bacterial Libraries | Enables the isolation, cultivation, and banking of individual bacterial strains from human samples for defined consortium design [51]. |
| Gnotobiotic Mouse Models | Germ-free or defined-flora animal models are essential for establishing causal relationships between microbial consortia and host phenotypes, and for testing mechanistic hypotheses [11]. |
| Anaerobic Chambers & Growth Media | Critical for maintaining the viability of obligate anaerobic bacteria during all stages of research, development, and manufacturing. |
| CGMP Manufacturing Systems | Specialized bioreactors and purification systems for producing consistent, well-characterized, and safe live biotherapeutic products at commercial scale [51]. |
| Multi-omics Integration Platforms | Computational tools that combine metagenomic, metatranscriptomic, metabolomic, and proteomic data to build a holistic view of microbiome function and host interaction [11]. |
| Coronene-d12 | Coronene-d12 Isotope|Research Chemical |
| ML 190 | ML 190, MF:C27H32N6O3, MW:488.6 g/mol |
Anatomical & Developmental Context of the Human Microbiome
The development of effective microbiome therapies is grounded in a deep understanding of how microbial communities assemble and stabilize in the human host.
Early-Life Microbiome Development as a Blueprint
Early life is a critical period for microbiome assembly, with long-lasting effects on host physiology [11] [42].
- Initial Colonization: The neonatal gut microbiome is seeded at birth, with mode of delivery (vaginal vs. cesarean section) being a major determinant. Vaginal delivery facilitates transfer of Lactobacillus and Prevotella, while C-section leads to enrichment of skin-associated Staphylococcus and Corynebacterium [11].
- Nutritional Drivers: Postnatal nutrition, particularly breastfeeding, provides human milk oligosaccharides (HMOs) that selectively nourish key early colonizers like Bifidobacterium infantis, which promotes immune homeostasis [11].
- Developmental Windows: The gut microbiome generally stabilizes to an adult-like state by 2-3 years of age. Disruptions during this critical developmental window (e.g., by antibiotics) are linked to an increased risk of immune and metabolic disorders later in life [11].
A Framework for Microbial Transmission
A reconceptualized framework for understanding microbiome acquisition, based on the "4 Ws"—What, Where, Who, and When—provides a structure for designing therapeutic interventions [42].
- What: The unit of transmission (e.g., microbial cells, spores, metabolites).
- Where: The anatomical source and destination (e.g., maternal gut to infant gut).
- Who: The donor source of the microbes (e.g., maternal, environmental, or defined consortia).
- When: The timing of transmission (e.g., prenatal, perinatal, postnatal, or adult therapeutic intervention).
This framework underscores that therapies like Rebyota and Vowst are, in essence, a controlled, therapeutic re-enactment of the natural processes of microbial transmission and community assembly that occur optimally in early life.
The approval of Rebyota and Vowst marks a pivotal transition for microbiome science from descriptive research to clinical application. These first-generation therapies validate the concept that manipulating the gut microbiome can effectively treat a specific disease, rCDI. The field is now rapidly evolving, with a diverse pipeline of next-generation candidates exploring defined consortia, engineered microbes, and synthetic biology approaches for a wider range of indications. Future success will depend on overcoming significant challenges, including high interindividual variability, the complexity of host-microbe interactions in non-infectious diseases, and the development of standardized biomarkers and manufacturing processes. As research continues to unravel the intricate anatomy and developmental biology of the human microbiome, it will pave the way for more precise, predictive, and personalized microbiome-based medicines.
Addressing Dysbiosis and Optimizing for a Resilient Microbial Ecosystem
The human body is host to complex ecosystems of microorganisms, including bacteria, fungi, viruses, and archaea, collectively known as the microbiome [52] [1]. These communities reside in various anatomical sites, with the highest densities in the gastrointestinal tract (29%), oral cavity (26%), and skin (21%) [1]. A balanced, symbiotic relationship between the host and these microorganisms is crucial for maintaining health, supporting functions including immune modulation, metabolic regulation, and protection against pathogens [53] [54]. Dysbiosis refers to a disruption of this balanced state, characterized by a loss of microbial diversity, a shift in community composition, and altered functional capacity [53] [55]. This whitepaper examines the causes and consequences of dysbiosis within the framework of human microbiome anatomy, development, and stabilization research, focusing specifically on antibiotic-induced disruptions and disease-related imbalances for a scientific audience.
Gut Microbiota Development and Stabilization
The establishment of the human microbiome is a sequential process that begins at birth and evolves throughout the lifespan. The initial microbial colonization is predominantly influenced by delivery mode. Vaginally delivered infants acquire microbes from the maternal vaginal and intestinal tract (e.g., Lactobacillus, Prevotella), while cesarean-delivered infants are initially colonized by maternal skin-associated taxa (e.g., Staphylococcus, Corynebacterium) [11]. This early divergence has been linked to long-term health outcomes, including altered immune development [11].
Postnatal nutrition further shapes the nascent microbiome. Breastfeeding provides human milk oligosaccharides (HMOs) that selectively promote the growth of beneficial bacteria, particularly Bifidobacterium infantis, which plays a key role in immune homeostasis [11]. The gut microbiome undergoes rapid succession during infancy, generally stabilizing to an adult-like configuration between 2-3 years of age [11]. This "climax community" remains relatively stable throughout adulthood but can be disrupted by factors such as diet, antibiotics, and disease [1]. In later life, the microbiota undergoes a final succession, typically marked by reduced diversity [1].
Table 1: Factors Influencing Early-Life Microbiome Development
| Factor | Impact on Microbiome | Potential Long-Term Health Consequences |
|---|---|---|
| Vaginal Delivery | Colonization with maternal vaginal and intestinal microbiota (e.g., Lactobacillus, Prevotella) | Established immune homeostasis; lower risk of immune dysregulation [11] |
| Cesarean Delivery | Colonization with maternal skin microbiota (e.g., Staphylococcus); delayed Bifidobacterium acquisition | Increased risk of obesity, asthma, and allergies [11] |
| Breastfeeding | Enrichment of Bifidobacterium infantis via Human Milk Oligosaccharides (HMOs) | Promotes immune tolerance and metabolic health [11] |
| Formula Feeding | Lower abundance of Bifidobacterium; higher abundance of Clostridium and Enterobacteriaceae | Altered SCFA production; increased gut permeability; higher risk of immune-mediated disorders [11] |
| Antibiotic Exposure | Decreased microbial diversity and delayed developmental trajectory | Increased risk of obesity, allergies, asthma, and weakened vaccine response [53] [11] |
Causes and Mechanisms of Dysbiosis
Dysbiosis can be triggered by a multitude of environmental, iatrogenic, and host-related factors that disrupt the ecological balance of the microbiome.
Antibiotic-Induced Dysbiosis
Antibiotics are among the most significant disruptors of microbial communities [56]. Their impact is determined by factors including the antibiotic's spectrum, route of administration, dosage, and treatment duration [53]. Broad-spectrum antibiotics cause the most profound damage, leading to:
- Reduced Diversity: A marked decrease in the variety of microbial species [53] [57].
- Taxonomic Shifts: Depletion of beneficial genera (e.g., Bifidobacterium, Faecalibacterium) and expansion of potentially harmful ones (e.g., Proteobacteria) [57] [58].
- Functional Alteration: Changes in the microbiome's metabolic output, such as reduced short-chain fatty acid (SCFA) production [57].
- Emergence of Resistance: Selection for antibiotic-resistant strains and horizontal gene transfer of antibiotic resistance genes (ARGs) [53] [57].
The diagram below illustrates the multifaceted impact of antibiotic therapy on gut homeostasis.
Non-Antibiotic Causes
Multiple other factors contribute to dysbiosis:
- Diet: Diets high in sugar, saturated fats, food additives (e.g., emulsifiers), and low in fiber reduce microbial diversity and promote inflammation [55] [59].
- Medications: Non-antibiotic drugs, including proton pump inhibitors, can alter microbial composition [53].
- Lifestyle Factors: Smoking, excessive alcohol consumption, and psychological stress disrupt microbial balance [52] [59].
- Host Conditions: Underlying chronic diseases, infections (e.g., SARS-CoV-2), and genetic predispositions can trigger dysbiosis [55] [59].
Functional Consequences and Systemic Disease Links
Dysbiosis impacts host physiology through several key mechanisms, leading to a wide range of gastrointestinal and systemic diseases.
Mechanisms of Pathogenesis
- Impaired Barrier Function: Dysbiosis can compromise the intestinal epithelial barrier, a condition often referred to as "leaky gut." This allows bacterial products and toxins to translocate into the bloodstream, triggering systemic inflammation [55] [57].
- Immune Dysregulation: The microbiome is essential for proper immune education and function. Dysbiosis disrupts the balance between pro-inflammatory and anti-inflammatory pathways, leading to inappropriate immune responses [55] [57]. This is mediated through pattern recognition receptors (e.g., TLRs, NLRs) and altered metabolite production [57].
- Metabolic Disruption: A dysbiotic microbiome exhibits altered production of microbial metabolites. This includes reduced levels of beneficial SCFAs like butyrate, acetate, and propionate, which are crucial for energy homeostasis and anti-inflammatory signaling, and increased production of harmful metabolites like trimethylamine (TMA) and succinate [55] [57] [58].
Disease Associations
Dysbiosis is implicated in a vast spectrum of conditions, as summarized in the table below.
Table 2: Select Disease Associations with Dysbiosis and Key Microbial Shifts
| Disease Category | Specific Conditions | Documented Microbial Shifts |
|---|---|---|
| Gastrointestinal | Inflammatory Bowel Disease (IBD), Irritable Bowel Syndrome (IBS), Clostridioides difficile infection [53] [55] | ↓ Diversity; ↓ Firmicutes (e.g., Faecalibacterium prausnitzii); ↑ Proteobacteria; ↑ mucolytic bacteria (e.g., Ruminococcus gnavus) [55] |
| Metabolic | Obesity, Type 2 Diabetes, NAFLD/NASH [53] [55] [54] | ↓ Diversity; ↓ Akkermansia muciniphila; ↓ Faecalibacterium; ↑ succinate-producing bacteria; altered SCFA profiles [53] [55] |
| Immunological / Allergic | Allergic rhinitis, Asthma, Atopic dermatitis [53] [59] | Early-life antibiotic use linked to higher risk; ↓ protective taxa; altered immune maturation [53] |
| Neuropsychiatric | Anxiety, Depression, Parkinson's Disease [59] [57] [56] | Communication via gut-brain axis; altered microbial neurotransmitter production; systemic inflammation [57] [56] |
| Cardiovascular | Atherosclerosis, Hypertension [57] [56] | ↑ Microbes converting choline to TMA (precursor of pro-atherogenic TMAO) [55] |
The following diagram synthesizes the primary signaling pathways through which a dysbiotic microbiome influences systemic health.
Experimental Models and Methodologies
Research into dysbiosis relies on a combination of in vivo models, in vitro systems, and advanced omics technologies to elucidate causal mechanisms and functional impacts.
In Vivo Antibiotic Intervention Model
A standard protocol for inducing and studying dysbiosis in mice is detailed below [58].
Objective: To investigate the causal role of antibiotic-induced dysbiosis in purine metabolism and hyperuricemia.
- Subjects: C57BL/6J mice.
- Intervention: Administration of an antibiotic cocktail (e.g., ampicillin, neomycin, metronidazole, vancomycin) in drinking water for 2 weeks.
- Control Group: Vehicle-only treatment.
- Sample Collection: Fecal samples collected pre- and post-intervention for 16S rRNA sequencing. Blood serum collected for uric acid (UA) quantification and liver/kidney function tests (ALT, AST, creatinine, urea).
- Functional Analysis: PICRUSt2 (Phylogenetic Investigation of Communities by Reconstruction of Unobserved States) algorithm applied to 16S data to predict metagenomic functional content, focusing on purine metabolism pathways.
- Tissue Analysis: Histological examination (H&E staining) of liver, kidney, small intestine, and colon to assess structural integrity.
Key Findings from this Model: Antibiotic treatment significantly altered microbiota composition, reducing diversity and increasing the abundance of Proteobacteria and Actinobacteria. This was paralleled by a 1.5-fold increase in serum uric acid without evidence of liver or kidney toxicity, indicating a direct functional impact of dysbiosis on host purine metabolism [58].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents and Models for Dysbiosis Research
| Category / Item | Specific Examples | Function / Application in Research |
|---|---|---|
| Animal Models | C57BL/6J mice, Germ-Free (GF) mice | In vivo study of host-microbe interactions; GF mice provide a blank slate for microbial colonization [54] [58]. |
| Antibiotic Cocktails | Ampicillin, Neomycin, Metronidazole, Vancomycin | Experimental induction of controlled, reproducible dysbiosis in animal models [58]. |
| Sequencing Technologies | 16S rRNA Gene Sequencing, Shotgun Metagenomics | Taxonomic profiling of microbial communities; shotgun sequencing allows for strain-level resolution and functional gene assessment [1] [58]. |
| Bioinformatics Tools | PICRUSt2, QIIME 2, UNOISE3 | Prediction of metagenome functions from 16S data; analysis of sequencing data; identifying exact amplicon sequence variants (ASVs) [58]. |
| Gnotobiotic Models | Ex-Germ-Free mice colonized with defined human microbiota | To establish causal relationships between specific microbial consortia and host phenotypes in a controlled environment [54]. |
Therapeutic Strategies and Interventions
Restoring a balanced microbiome is a key goal in managing dysbiosis-associated diseases. Interventions range from whole-community restoration to targeted approaches.
- Fecal Microbiota Transplantation (FMT): This procedure involves transferring processed fecal matter from a healthy, screened donor into a patient's gastrointestinal tract. FMT is highly effective (>90% cure rate) for recurrent Clostridioides difficile infection and is under investigation for IBD, IBS, and hepatic encephalopathy [55] [57]. The main mechanism is thought to be the restoration of a diverse and functional microbial community.
- Probiotics and Synbiotics: Probiotics are live microorganisms that confer a health benefit when administered in adequate amounts. Strains of Lactobacillus, Bifidobacterium, and Saccharomyces boulardii have demonstrated efficacy in preventing antibiotic-associated diarrhea and reducing necrotizing enterocolitis in preterm infants [53] [55] [11]. Synbiotics combine probiotics with prebiotics (non-digestible food ingredients that stimulate the growth of beneficial bacteria) to improve probiotic survival and persistence.
- Prebiotics and Dietary Modulation: A diet rich in diverse plant fibers and fermented foods supports a healthy microbiome by providing necessary substrates for beneficial bacteria, leading to increased SCFA production [52] [59]. This is a foundational approach for maintaining and restoring microbial balance.
- Precision Microbiome Therapeutics: Emerging strategies include engineered live biotherapeutic products (LBPs), defined consortia of beneficial bacteria, and phage therapies that target specific pathogenic bacteria without disrupting the commensal community [11] [57].
Dysbiosis represents a critical breakdown in the symbiotic relationship between the host and its microbiome, with far-reaching consequences for human health. Driven strongly by antibiotic exposure and other environmental factors, dysbiosis is not merely a taxonomic shift but a functional disturbance that compromises barrier integrity, immune homeostasis, and metabolic signaling. The translation of microbiome research into clinical practice is advancing, with FMT and probiotics already establishing efficacy for specific conditions. Future research must focus on defining causal mechanisms, standardizing diagnostic biomarkers, and developing personalized, microbiome-based therapeutics to effectively prevent and treat the myriad diseases associated with microbial imbalance.
The human gastrointestinal tract is home to trillions of microorganisms, collectively known as the gut microbiome, which maintains a continuous crosstalk with the human body and plays integral roles in health and disease [1]. Among its critical attributes, microbial resilience—the ability of the gut microbial community to resist perturbation and recover its original composition and function after disturbance—is increasingly recognized as a fundamental characteristic of a healthy gut ecosystem [60]. This resilience ensures the stability of core microbial functions despite numerous stressors, from dietary changes to antibiotic treatments [10] [60].
Understanding resilience requires viewing the human body as a "meta-organism" where host tissues and microbial communities engage in complex symbiosis [1]. The microbiome's collective genetic potential, far exceeding that of the human genome, provides functional capabilities essential for host physiology [61] [1]. When this symbiotic relationship is disrupted, a state of dysbiosis occurs, characterized by reduced microbial diversity, loss of beneficial microorganisms, and potential proliferation of pathogens [60]. This review examines the biomarkers, mechanisms, and assessment methodologies for gut microbiome resilience within the broader context of human microbiome anatomy, development, and stabilization.
Anatomical and Physiological Context of the Gut Microbiome
The human microbiome is distributed across various anatomical sites, with the gastrointestinal tract representing the most densely populated organ, hosting approximately 29% of the body's microbial communities [1]. This distribution follows distinct gradients, with microbial density increasing substantially from the stomach and small intestine to the colon [1].
The development of the gut microbiome begins at birth, undergoing ecological succession through defined life stages [10] [1]. The initial colonization is influenced by delivery mode, feeding practices, and early environmental exposures [10]. This development progresses through a phase of rapid changes before stabilizing into a relatively stable "climax community" during adolescence [1]. This mature community is typically dominated by bacteria from the Bacillota (formerly Firmicutes) and Bacteroidota (formerly Bacteroidetes) phyla, which constitute the majority of the gut microbes [60].
Despite interpersonal variation in species composition, healthy gut microbiomes share a functional core of metabolic capabilities, demonstrating functional redundancy despite taxonomic differences [10]. This functional stability, maintained through various resilience mechanisms, supports critical host functions including immune modulation, nutrient metabolism, and protection against pathogens [60] [1].
Defining Microbial Resilience and Stability
In ecological terms, resilience describes the capacity of an ecosystem to return to its original state after disturbance, while stability reflects its ability to resist compositional and functional changes [60]. Within gut microbiome science, these concepts translate to specific measurable properties:
- Resistance: The ability to maintain original composition and function when faced with stressors
- Recovery: The capacity to return to pre-disturbance state following perturbation
- Functional Flexibility: Maintenance of core metabolic functions despite taxonomic shifts
The "slave tissue" concept provides a useful framework for understanding host-microbe relationships, viewing the microbiome as an exogenous tissue under the control of human master tissues (nerve, connective, epithelial, and muscle) [1]. This perspective highlights the intricate regulatory mechanisms maintaining microbial homeostasis and the health implications when this balance is disrupted.
Biomarkers and Assessment of a Resilient Microbiome
Identifying a resilient microbiome requires monitoring specific biomarkers before, during, and after controlled disturbances. The following table summarizes key resilience biomarkers and assessment methodologies:
Table 1: Biomarkers and Assessment Methods for Microbial Resilience
| Biomarker Category | Specific Indicators | Assessment Methods | Interpretation |
|---|---|---|---|
| Diversity Indices | Shannon Diversity Index, Chao1 Richness, Phylogenetic Diversity | 16S rRNA sequencing, shotgun metagenomics | Higher baseline diversity correlates with greater resilience [61] [60] |
| Taxonomic Composition | Firmicutes/Bacteroidetes ratio, abundance of SCFA-producing bacteria (e.g., Faecalibacterium prausnitzii, Roseburia intestinalis) | Relative abundance analysis, qPCR, fluorescence in situ hybridization | Stable ratios indicate resistance; recovery patterns indicate resilience [60] |
| Functional Markers | SCFA concentrations (acetate, propionate, butyrate), bile acid metabolism, vitamin synthesis | Metabolomics (GC-MS, LC-MS), metatranscriptomics | Maintenance of metabolic functions despite disturbance indicates functional resilience [60] |
| Recovery-Associated Bacteria | Specific bacterial taxa with rapid regrowth patterns following disturbance | Time-series sampling, growth rate calculations | Early reappearance predicts overall recovery trajectory [60] |
Experimental Protocols for Assessing Resilience
Protocol 1: Antibiotic Perturbation and Recovery Assessment
Objective: Quantify resilience following controlled antibiotic intervention.
Materials:
- Sterile stool collection kits
- DNA/RNA stabilization buffer
- DNA extraction kit (e.g., QIAamp PowerFecal Pro DNA Kit)
- 16S rRNA gene sequencing primers (e.g., 515F/806R for V4 region)
- Antibiotic cocktail (e.g., vancomycin, neomycin, metronidazole)
- Short-chain fatty acid analysis kit (GC-MS based)
Methodology:
- Baseline sampling: Collect three baseline stool samples over one week prior to intervention
- Antibiotic administration: Administer broad-spectrum antibiotics for 5-7 days
- Perturbation sampling: Collect daily samples during antibiotic administration
- Recovery phase sampling: Collect samples at days 1, 3, 7, 14, 21, and 28 post-antibiotic cessation
- Sample processing:
- Preserve aliquots in DNA/RNA stabilization buffer
- Extract genomic DNA following manufacturer protocols
- Perform 16S rRNA gene sequencing with appropriate controls
- Conduct SCFA analysis using GC-MS
- Data analysis:
- Calculate alpha diversity indices (Shannon, Chao1)
- Assess beta diversity using PCoA with Bray-Curtis dissimilarity
- Track relative abundance of key taxonomic groups
- Measure SCFA concentration changes over time
Resilience quantification: Calculate recovery quotient (RQ) as: RQ = (Xrecovery - Xmin)/(Xbaseline - Xmin), where X represents diversity metrics or taxon abundance [60].
Protocol 2: Dietary Perturbation and Functional Resilience
Objective: Assess functional stability during dietary intervention.
Materials:
- Controlled diet materials (high-fiber vs. high-fat)
- Metabolomic profiling kits
- Metatranscriptomic sequencing reagents
- pH and microbial culture media
Methodology:
- Baseline period: Standard diet for 2 weeks with daily sampling
- Intervention period: Administer test diet for 3 weeks
- Reversion period: Return to standard diet for 4 weeks
- Multi-omics profiling:
- Metatranscriptomics: RNA extraction, library preparation, sequencing
- Metabolomics: LC-MS for polar metabolites, GC-MS for volatile compounds
- Functional assessment:
- Enzyme activity assays for key metabolic pathways
- SCFA production rates
- Bile acid transformation efficiency
Analysis: Identify preserved core functions despite taxonomic shifts, indicating functional resilience [10].
Research Reagent Solutions for Resilience Studies
Table 2: Essential Research Reagents for Microbial Resilience Investigations
| Reagent Category | Specific Product Examples | Primary Function | Application Notes |
|---|---|---|---|
| DNA/RNA Stabilization Buffers | RNAlater, DNA/RNA Shield | Preserves nucleic acid integrity during storage and transport | Critical for time-series experiments requiring batch processing [60] |
| DNA Extraction Kits | QIAamp PowerFecal Pro DNA Kit, DNeasy PowerLyzer PowerSoil Kit | Efficient lysis of diverse microbial cells and purification of inhibitor-free DNA | Ensures representative community analysis without bias toward easily-lysed taxa [60] |
| Sequencing Reagents | 16S rRNA PCR primers (515F/806R), Illumina sequencing chemistry, shotgun library prep kits | Amplification and sequencing of microbial genomic content | 16S for taxonomic profiling; shotgun for functional potential [61] [10] |
| Metabolomic Analysis Kits | GC-MS SCFA analysis kits, LC-MS bile acid panels | Quantification of microbial-derived metabolites | Provides functional readout of microbial activities [60] |
| Bacterial Culture Media | Gifu Anaerobic Medium (GAM), YCFA, specific selective media | Cultivation of fastidious anaerobic gut bacteria | Essential for isolating and characterizing recovery-associated bacteria [60] |
| Antibiotic Cocktails | Vancomycin, neomycin, metronidazole combinations | Controlled perturbation of gut microbiota | Standardized disturbance for resilience quantification [60] |
Visualization of Microbial Resilience Concepts
Microbial Resilience Pathways: This diagram illustrates the dynamic pathways of microbial community response to disturbance, highlighting the critical decision points between recovery and chronic dysbiosis, along with key biomarkers that predict trajectory outcomes.
Factors Influencing Microbial Resilience
Numerous intrinsic and extrinsic factors modulate the resilience capacity of the gut microbiome, creating substantial inter-individual variation in response patterns to similar disturbances.
Intrinsic Factors
- Host Genetics: Genetic variants related to immune function (e.g., LINGO2, VANGL1) influence microbial composition and potentially resilience capacity [60]
- Age: The gut microbiome demonstrates distinct life stage patterns, with aging associated with reduced diversity and decreased abundance of SCFA-producing bacteria, potentially diminishing resilience [60]
- Baseline Microbiome State: Pre-existing microbial diversity, composition, and functional capacity significantly influence resilience [61] [60]
Extrinsic Factors
- Dietary Patterns: Long-term dietary patterns profoundly shape microbial community structure [10]. High-fiber diets typically support greater microbial diversity and SCFA production, enhancing resilience [10] [60]
- Antibiotic Exposure: As major disruptors of microbial ecosystems, antibiotics can cause long-term alterations to community composition, with repeated exposures potentially causing incremental loss of resilience [60]
- Lifestyle and Environment: Environmental exposures, physical activity, and circadian rhythms contribute to microbial stability [60]
Intervention Strategies to Enhance Resilience
Targeted interventions can potentially strengthen microbial resilience, offering promising approaches for maintaining microbiome health and preventing dysbiosis-related conditions.
Table 3: Intervention Strategies for Enhancing Microbial Resilience
| Intervention Type | Specific Approaches | Mechanism of Action | Evidence Status |
|---|---|---|---|
| Nutritional Interventions | High-fiber diets, prebiotics (e.g., inulin, GOS), polyphenol-rich foods | Increases SCFA production, supports beneficial taxa, provides colonization resistance | Clinical evidence supported [10] [60] |
| Probiotics | Specific strains (e.g., Lactobacillus, Bifidobacterium), multi-strain formulations | Direct introduction of beneficial taxa, competitive exclusion of pathogens | Mixed evidence; strain-specific effects [60] |
| Postbiotics | SCFA supplements, microbial metabolites | Direct provision of beneficial metabolites, modulation of host signaling | Emerging evidence [60] |
| Fecal Microbiota Transplantation | Transfer of processed stool from healthy donors | Complete microbial community restoration, introduction of keystone species | Established for C. difficile; experimental for other conditions [60] |
| Phage Therapy | Targeted bacteriophage cocktails | Precision elimination of specific pathogens, preservation of commensals | Preclinical development [60] |
Challenges and Future Directions
Despite significant advances, the study of microbial resilience faces several methodological and conceptual challenges that require attention in future research:
- Standardization of Metrics: Lack of consensus on standardized metrics and protocols for quantifying resilience limits comparability across studies [60]
- Temporal Resolution: Most human studies lack sufficient sampling frequency to capture rapid microbial dynamics during disturbance and recovery [60]
- Multi-omics Integration: Effectively integrating data from genomics, transcriptomics, metabolomics, and proteomics to create comprehensive resilience profiles remains technically challenging [60] [62]
- Personalized Approaches: Developing individualized resilience biomarkers that account for unique host genetics, microbiome composition, and environmental contexts represents a frontier in precision medicine [60]
Future research directions should include longitudinal studies with dense sampling, development of computational models predicting individual resilience thresholds, and clinical trials testing resilience-enhancing interventions in at-risk populations. The integration of microbiome resilience assessment into clinical practice could transform approaches to antibiotic stewardship, chronic disease prevention, and personalized nutrition.
Within the broader context of human microbiome research—encompassing its distribution, anatomy, development, and stabilization—the concept of microbial resilience has emerged as a critical characteristic of a healthy ecosystem. The human gut microbiome is a complex community that interacts with the host via multiple gut-organ axes (e.g., gut-brain, gut-liver, gut-immune) to maintain health [60] [63]. A resilient microbiome can resist perturbations and restore its composition and function after disturbances, such as antibiotic treatments, infections, or dietary changes [60] [63]. This in-depth technical guide synthesizes current research on the principal biomarkers used to identify and quantify this resilience, focusing on diversity indices, short-chain fatty acid (SCFA) producers, and functional flexibility. These biomarkers are vital for advancing predictive diagnostics and developing targeted therapeutic interventions in precision medicine [60].
Core Biomarkers of a Resilient Microbiome
Diversity Indices
Microbial diversity is a foundational metric for assessing ecosystem health and resilience. It provides a measure of the community's ability to buffer against disturbances and maintain functional stability.
Table 1: Key Diversity Indices as Biomarkers of Resilience
| Index Name | Description | Measurement Approach | Association with Resilience |
|---|---|---|---|
| Alpha-diversity | Within-sample richness and evenness of microbial species [60] | 16S rRNA amplicon or shotgun metagenomic sequencing [42] | Higher diversity is correlated with greater stability and resistance to dysbiosis [60] [63] |
| Richness | The total number of distinct species or taxa present in a sample [60] | 16S rRNA amplicon or shotgun metagenomic sequencing | A core feature of a healthy gut microbiome [60] [63] |
| Phyla Ratio (F/B) | The ratio of Bacillota (Firmicutes) to Bacteroidota (Bacteroidetes) [60] [63] | Taxonomic profiling from sequencing data | An altered ratio is a common sign of dysbiosis linked with aging and disease [60] [63] |
A decline in these diversity indices is a hallmark of dysbiosis, an imbalance linked to numerous gastrointestinal and extra-intestinal diseases [60] [63]. The restoration of a diverse community is a key indicator of recovery and resilience.
SCFA-Producing Bacteria
Short-chain fatty acids (SCFAs), such as acetate, propionate, and butyrate, are crucial microbial metabolites that maintain host health. Butyrate serves as the primary energy source for colonocytes, propionate regulates gluconeogenesis and satiety, and acetate influences cholesterol metabolism and systemic immunity [60] [63]. The abundance of SCFA-producing bacteria is a critical functional biomarker for a resilient microbiome.
Table 2: Key SCFA-Producing Bacterial Taxa and Their Functions
| Bacterial Taxa | Primary SCFA | Function & Significance | Response to Perturbation |
|---|---|---|---|
| Faecalibacterium prausnitzii | Butyrate | Anti-inflammatory properties; key health-associated species [60] [63] | Depleted in inflammatory bowel disease (IBD) and other dysbiotic states [60] [63] |
| Roseburia intestinalis | Butyrate | Maintains gut barrier integrity [60] [63] | Reduced in IBD and irritable bowel syndrome (IBS) [60] [63] |
| Eubacterium rectale | Butyrate | Important for gut homeostasis [60] [63] | Decreased in dysbiosis [60] [63] |
| Anaerostipes | Butyrate | Contributes to butyrate production | Increases in response to prebiotic inulin supplementation [64] |
| Bifidobacterium | Acetate/Lactate | Promotes immune homeostasis; consumes HMOs in infants [11] | Depleted by neonatal antibiotic exposure [11]; increases with inulin [64] |
| Fusicatenibacter | SCFAs | Associated with metabolic health | Increases in B-type microbiota after arabinoxylan supplementation [64] |
The functional output of these taxa, namely SCFA levels, can be directly measured. For instance, a study stratified by the Prevotella-to-Bacteroides (P/B) ratio demonstrated that arabinoxylan fiber supplementation significantly increased fasting and postprandial plasma propionate and acetate levels, particularly in individuals with a Bacteroides-dominated (B-type) microbiota [64].
Figure 1: SCFA Signaling Pathway in Health and Resilience. SCFAs produced by gut bacteria from dietary fiber are key mediators of microbial influence on host health.
Functional Flexibility
Functional flexibility refers to the microbiome's capacity to maintain metabolic output and stability despite fluctuations in taxonomic composition. This concept is central to resilience, as it emphasizes preserved function over rigid structural membership.
- Functional Redundancy: A diverse microbiome contains multiple different bacteria that can perform the same metabolic function (e.g., SCFA production). If one species is diminished, others can compensate, ensuring functional stability [60].
- Functional Biomarkers: Beyond taxonomy, direct measures of function are key. These include the abundance of microbial genes involved in SCFA synthesis, resistance genes, antimicrobial peptides, and the production of metabolites like SCFAs [60].
- The Prevotella-to-Bacteroides Ratio: This ratio has been investigated as a potential biomarker for predicting functional responses, particularly to dietary fiber. Individuals with a high Prevotella-to-Bacteroides (P-type) ratio may respond differently to fiber interventions like arabinoxylan and inulin compared to those with a B-type ratio, highlighting the link between community structure and functional output [64].
Methodologies for Biomarker Assessment
Sequencing and Metagenomic Analysis
Tracking microbial strains and their genes over time via high-throughput sequencing is the primary method for assessing resilience biomarkers.
Table 3: Key Experimental Protocols for Biomarker Analysis
| Method | Protocol Summary | Key Applications | Considerations |
|---|---|---|---|
| 16S rRNA Gene Sequencing | - Amplify hypervariable regions (V4-V5) [64].- Sequence on Illumina MiSeq or similar.- Cluster sequences into OTUs/ASVs using QIIME 2 or DADA2. | Taxonomy-based diversity analysis (alpha/beta diversity) [64]. | Cost-effective; limited to taxonomic and low-resolution functional inference. |
| Shotgun Metagenomic Sequencing | - Fragment genomic DNA from samples.- Sequence without target-specific primers (Illumina).- Analyze with tools like HUMAnN2, MetaPhlAn, and strain-level trackers [42]. | High-resolution taxonomic profiling; functional gene analysis (e.g., SCFA pathways); strain tracking [60] [42]. | Enables comprehensive functional insight and strain-level transmission studies [42]. |
| Strain-Level Tracking | - Use reference-based or de novo assembly from shotgun data.- Identify single-nucleotide variants (SNVs) to link strains across samples (e.g., mother-infant pairs) [42]. | Defining "transmitted strains" to map microbiome acquisition and resilience [42]. | Requires high sequencing depth and sophisticated bioinformatics. |
Figure 2: Workflow for Metagenomic Analysis. Standard pipeline from sample collection to data output for assessing taxonomic and functional biomarkers.
Measuring Functional Output
To complement genetic potential, direct measurement of metabolites and gases provides a readout of microbial activity.
- SCFA Measurement: Protocol: Collect fecal samples or plasma. For fecal SCFAs, homogenize samples in acidified water or phosphate buffer, centrifuge, and analyze the supernatant using gas chromatography (GC). For plasma SCFAs, derivatization may be required prior to GC analysis [64].
- Breath Hydrogen Test: Protocol: After an overnight fast, subjects consume a test substrate (e.g., 15g of inulin). Breath samples are collected at baseline and at regular intervals (e.g., every 30-60 minutes) for up to 8 hours. Hydrogen concentration is measured using a gas chromatograph or a dedicated breath hydrogen analyzer [64]. A significant rise in breath hydrogen indicates microbial fermentation of the substrate.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| 16S rRNA Primers (e.g., 515F/806R) | Amplify conserved bacterial gene regions for taxonomic profiling [64] | Initial characterization of community diversity and composition. |
| Shotgun Metagenomic Library Prep Kits (e.g., Illumina DNA Prep) | Prepare sequencing libraries from total community DNA for functional analysis. | Comprehensive profiling of microbial genes and pathways. |
| GC-MS Systems | Quantify SCFA concentrations (acetate, propionate, butyrate) in fecal or plasma samples [64]. | Validating functional output of the microbiome in intervention studies. |
| Breath Hydrogen Analyzers | Measure hydrogen gas in breath samples as a direct indicator of microbial carbohydrate fermentation [64]. | Assessing real-time microbial metabolic activity in response to prebiotics. |
| Gnotobiotic Mouse Models | Provide a controlled, germ-free environment to study host-microbe interactions and test causality. | Mechanistic studies to determine if specific bacteria confer resilience traits. |
The biomarkers of resilience—diversity indices, SCFA-producing bacteria, and functional flexibility—provide a multi-faceted framework for assessing the health and stability of the human gut microbiome. The integration of high-throughput sequencing with metabolomic techniques allows researchers to move beyond correlation toward a mechanistic understanding of how resilient microbiomes protect host health. This knowledge is foundational for developing novel diagnostics and targeted interventions, such as personalized nutrition and next-generation probiotics, aimed at restoring and maintaining microbial resilience to prevent and treat disease.
The human microbiome, particularly the gut microbiota, represents a complex ecosystem that plays a pivotal role in host physiology, immune function, and metabolic homeostasis [65] [66]. This community of trillions of microorganisms, dominated by the phyla Firmicutes, Bacteroidetes, Actinobacteria, Proteobacteria, and Verrucomicrobia, expresses a diverse genetic repertoire that significantly expands the host's metabolic capabilities [65] [66]. Dysbiosis, an imbalance in this microbial community, has been implicated in a wide range of metabolic, immunological, and neurological conditions [65]. Against this backdrop, targeted nutritional interventions using prebiotics, probiotics, and synbiotics have emerged as promising strategies to modulate the gut microbiota and restore microbial balance [65] [67] [68]. This whitepaper provides an in-depth technical examination of these interventions within the broader context of human microbiome research, focusing on their mechanisms, efficacy, and applications in both foundational and clinical science.
Definitions and Core Concepts
Probiotics
The Food and Agriculture Organization (FAO) and World Health Organization (WHO) define probiotics as "live microorganisms which when administered in adequate amounts confer a health benefit on the host" [66] [69]. To be classified as a probiotic, a strain must be non-pathogenic, non-toxic, adequately characterized, and maintain viability throughout its shelf life [65]. Core functional criteria include resistance to gastrointestinal stresses (low pH, bile salts), adherence to intestinal epithelial cells, and production of beneficial metabolites [65]. The most extensively studied probiotic genera include Lactobacillus and Bifidobacterium, with other notable strains belonging to Pediococcus, Lactococcus, Enterococcus, Streptococcus, and the yeast Saccharomyces boulardii [65] [68] [69].
Prebiotics
Prebiotics are "non-digestible food ingredients that beneficially affect the host by selectively stimulating the growth and/or activity of beneficial microorganisms" in the gastrointestinal tract [67] [68]. They are dietary substrates that resist host digestion and reach the colon intact, where they serve as fermentation substrates for beneficial gut bacteria [67]. Common prebiotics include fructans (inulin, fructo-oligosaccharides), galacto-oligosaccharides (GOS), xylo-oligosaccharides (XOS), chitooligosaccharides, lactulose, resistant starch, and polyphenols [67] [70].
Synbiotics
Synbiotics refer to combinations of probiotics and prebiotics that act synergistically [65] [68] [71]. In these formulations, the prebiotic component selectively supports the survival and metabolic activity of the co-administered probiotic strains, enhancing their persistence and functionality within the gut ecosystem [68] [72]. Synbiotics can be designed as either complementary (independent actions of probiotic and prebiotic) or synergistic (prebiotic selectively supports the administered probiotic) [68].
Mechanisms of Action
Probiotic Mechanisms
Probiotics exert their beneficial effects through multiple interconnected mechanisms [68] [69]:
Competitive Exclusion of Pathogens: Probiotics compete with pathogens for nutrients and adhesion sites on the intestinal mucosa, limiting pathogenic colonization [68] [69]. They also produce antimicrobial substances including short-chain fatty acids (SCFAs), organic acids, hydrogen peroxide, and bacteriocins that inhibit pathogen growth [69].
Enhancement of Intestinal Barrier Function: Probiotics strengthen the gut barrier by stimulating mucin production from goblet cells and regulating the expression of tight junction proteins (e.g., occludin, claudin-1), thereby reducing intestinal permeability [68] [69].
Immunomodulation: Probiotics interact with intestinal epithelial cells and immune cells (dendritic cells, macrophages, B and T lymphocytes) to modulate both innate and adaptive immune responses [68] [69]. This includes increasing anti-inflammatory cytokines (e.g., IL-10) while reducing pro-inflammatory cytokines (e.g., TNF-α, IL-8) [71] [69].
Neurotransmitter Production: Specific probiotic strains can produce or influence the production of neurotransmitters including serotonin, gamma-aminobutyric acid (GABA), and dopamine via the gut-brain axis, potentially affecting mood, behavior, and gut motility [69].
Prebiotic Mechanisms
Prebiotics primarily function through selective stimulation of beneficial gut bacteria [67]:
Selective Microbial Stimulation: Prebiotics serve as growth substrates for beneficial bacteria such as Bifidobacterium and Lactobacillus, enhancing their abundance and metabolic activity [67].
SCFA Production: Fermentation of prebiotics by gut microbiota produces SCFAs, primarily acetate, propionate, and butyrate, which have numerous health benefits [67]. Butyrate serves as the primary energy source for colonocytes, propionate influences gluconeogenesis and satiety, and acetate contributes to lipid metabolism [67] [72].
Microbiota Modulation: By promoting the growth of beneficial bacteria, prebiotics help shift the overall gut microbiota composition toward a more health-promoting profile, characterized by increased diversity and stability [67].
Synbiotic Mechanisms
Synbiotics leverage combined mechanisms from both probiotics and prebiotics [68] [72]:
Enhanced Probiotic Survival: The prebiotic component provides a selective substrate that improves the survival, persistence, and colonization of the co-administered probiotic strains during gastrointestinal transit [68].
Metabolic Cross-Feeding: Prebiotics support not only the administered probiotics but also indigenous beneficial bacteria, creating synergistic metabolic networks that enhance the production of health-promoting metabolites like SCFAs [72].
Bile Acid Metabolism: Certain synbiotics enhance bile acid deconjugation and modulate bile acid composition, potentially improving lipid metabolism and offering weight management benefits [72].
The following diagram illustrates the core mechanisms of action for probiotics, prebiotics, and synbiotics:
Figure 1: Core mechanisms of action of probiotics, prebiotics, and synbiotics. Probiotics (yellow) act directly on host physiology, prebiotics (green) work indirectly via microbial metabolism, and synbiotics (blue) combine these approaches for synergistic effects, ultimately leading to health benefits (red).
Quantitative Efficacy Data
Health Benefits Across Conditions
Table 1: Efficacy of probiotic, prebiotic, and synbiotic interventions across health conditions
| Health Condition | Intervention Type | Specific Strains/Substances | Dosage | Key Outcomes | Reference |
|---|---|---|---|---|---|
| Ulcerative Colitis | Probiotic | Bifidobacterium longum 536 | 2–3 × 10¹¹ CFU, three times daily for 8 weeks | ↓ Mayo subscore, ↓ Rachmilewitz endoscopic index | [69] |
| Ulcerative Colitis | Probiotic | Lactococcus lactis NCDO 2118 | 2.5 × 10ⶠCFU/g (mouse model) | ↓ Disease activity index, ↑ tight junction protein expression | [69] |
| Crohn's Disease | Synbiotic | B. longum + inulin/oligofructose | 2 × 10¹¹ CFU twice daily for 6 months | ↓ Crohn's disease activity indices, ↓ TNF-α expression | [69] |
| Irritable Bowel Syndrome | Probiotic | L. delbruekii + L. fermentum | 10¹ⰠCFU twice daily for 4 weeks | ↓ Abdominal pain, ↓ IL-8, restored normal intestinal flora | [69] |
| Antibiotic-Associated Diarrhea | Probiotic | Lactobacillus + Bifidobacterium strains | 1 × 10⹠CFU once daily | Delayed recurrence of diarrhea (5.39 days), ↓ stool frequency | [69] |
| Radiation-Induced Diarrhea | Probiotic | L. acidophilus + B. animalis | 1.75 × 10⹠CFU three times daily | ↓ Moderate and severe diarrhea, ↓ Grade II abdominal pain | [69] |
| Lactose Intolerance | Probiotic | L. acidophilus | 1 × 10¹ⰠCFU once daily for 4 weeks | ↓ Abdominal pain, ↓ cramping, ↓ vomiting | [69] |
| Hypercholesterolemia | Probiotic | L. casei pWQH01 + L. plantarum AR113 | 1 × 10⹠CFU for 5 weeks (mouse model) | ↓ Hepatic TC and LDL-C, ↑ CYP7A1 gene expression | [69] |
| Obesity-Related Metabolism | Synbiotic | L. reuteri KUB-AC5 + Wolffia globosa | 10⸠CFU + 6 g/day (in vitro model) | ↑ Butyrate, ↓ p-cresol, modulated bile acid composition | [72] |
Key: CFU = Colony Forming Units; ↓ = decrease/reduction; ↑ = increase/elevation; TC = Total Cholesterol; LDL-C = Low-Density Lipoprotein Cholesterol
Gut Microbiota Response Metrics
Table 2: Microbiota and metabolic response to interventions
| Intervention Parameter | Metric | Model System | Key Changes | Reference |
|---|---|---|---|---|
| Synbiotic Efficacy | Bacterial Counts | In vitro gastrointestinal model (obese donor) | ↑ Anaerobic bacteria (+2.6 log CFU/mL in AC, +2.2 log in DC) | [72] |
| Synbiotic Efficacy | Microbial Composition | In vitro gastrointestinal model (obese donor) | ↑ Lactic acid bacteria, ↓ Enterobacteriaceae | [72] |
| Synbiotic Efficacy | Metabolic Output | In vitro gastrointestinal model (obese donor) | ↑ Butyrate, ↓ p-cresol, ↑ bile acid deconjugation | [72] |
| Dietary Intervention Response | Community Stability | Human dietary interventions (n=641) | Response variability linked to baseline functional redundancy | [73] |
| Intervention Response | Predictive Features | Multiple human studies | Higher functional redundancy → lower responsiveness to intervention | [73] |
Key: AC = Ascending Colon; DC = Descending Colon
Experimental Models and Methodologies
In Vitro Gastrointestinal Simulation Model
Advanced in vitro systems provide physiologically relevant models for investigating intervention effects on human gut microbiota. The following workflow illustrates a comprehensive experimental approach using a continuous gastrointestinal simulator:
Figure 2: Experimental workflow for evaluating synbiotic efficacy using a continuous in vitro gastrointestinal model. This system mimics the human gut environment to assess microbial and metabolic changes following intervention [72].
Detailed Methodology:
Fecal Inoculum Preparation: Fecal samples from rigorously screened donors (e.g., obese adults with BMI >40 kg/m², no recent antibiotic/probiotic use) are homogenized in phosphate-buffered saline (PBS) with cryoprotectants (0.1% trehalose, 50% glycerol), filtered, aliquoted, and stored at -80°C until use [72].
Continuous Gastrointestinal Simulator: A three-stage bioreactor system (Biostat B-DCU) replicates the small intestine (SI), ascending colon (AC), and descending colon (DC) compartments. The system maintains anaerobic conditions (N₂ flushing), physiological temperatures (37°C), pH gradients (AC: 5.8, DC: 6.8), and continuous agitation (200 rpm) [72].
System Stabilization: The system is fed daily with carbohydrate-based GI medium (containing peptone, yeast extract, soluble starch, pectin, mucin, xylan, and reduction agents) to stabilize microbial communities before intervention [72].
Intervention Phase: Synbiotic/probiotic/prebiotic interventions are introduced while maintaining continuous medium flow. For example, a synbiotic combination of Limosilactobacillus reuteri KUB-AC5 (10⸠CFU) and Wolffia globosa powder (6 g/day) [72].
Monitoring and Analysis: Regular samples from AC and DC compartments are analyzed using:
- Culture-dependent methods: Viable counts on selective media to quantify specific bacterial groups [72].
- Culture-independent methods: 16S rRNA gene sequencing to assess microbial diversity and community structure [72].
- Metabolite analysis: Gas chromatography/mass spectrometry (GC/MS) for SCFAs, bile acids, and other microbial metabolites [72].
Assessing Microbiome Response to Interventions
Measuring gut microbiome stability and response to interventions requires specialized metrics:
Beta Diversity Analysis: Commonly measured using Bray-Curtis or Aitchison dissimilarities between pre- and post-intervention samples [73].
Raup-Crick Metric (RCbray): A null model-based approach that corrects for the computational dependence of beta diversity on alpha diversity, providing a more robust measure of community change [73]. Values range from -1 (identical communities) to 1 (maximally distinct communities).
Response Determinants: Baseline microbiome features influencing intervention response include:
- Functional redundancy (average number of genes per microorganism in community) - negatively correlated with responsiveness [73].
- Enterotype-specific drivers - abundance of dominant taxa in specific enterotypes (Bact1, Rum) affects response magnitude [73].
- Microbial diversity and composition - specific metabolic capacities influence intervention efficacy [73].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential research reagents and materials for microbiome intervention studies
| Reagent/Material | Application/Function | Example Specifications | Reference |
|---|---|---|---|
| MRS Agar with Supplements | Cultivation and maintenance of lactic acid bacteria and probiotics | + 0.5% CaCO₃ + 0.05% L-cysteine-HCl; anaerobic conditions at 37°C | [72] |
| Anaerobic Culture Systems | Creating oxygen-free environment for obligate anaerobes | Anaerobic jars with gas packs; continuous Nâ‚‚ flushing in bioreactors | [72] |
| Phosphate-Buffered Saline (PBS) with Cryoprotectants | Fecal sample homogenization and preservation for microbial viability | PBS pH 6.8 + 0.1% trehalose + 50% glycerol; storage at -80°C | [72] |
| Reducing Agents | Maintaining anaerobic conditions in liquid media | 0.025-0.3% L-cysteine HCl + 0.025-0.3% sodium thioglycolate | [72] |
| Carbohydrate-Based GI Medium | In vitro simulation of gut nutrient environment | Peptone, yeast extract, starch, pectin, mucin, xylan, hemin, vitamins | [72] |
| Selective Media | Enumeration of specific bacterial groups | Media for LAB, Enterobacteriaceae, total anaerobes | [72] |
| DNA Extraction Kits | Microbial DNA isolation for sequencing | Protocols optimized for complex fecal samples | [73] |
| 16S rRNA Gene Primers | Amplicon sequencing of bacterial communities | Targeting V3-V4 hypervariable regions; Illumina compatible | [73] |
| GC/MS Systems | Quantification of microbial metabolites | SCFA analysis (acetate, propionate, butyrate); bile acid profiling | [72] |
Emerging Research and Future Directions
Advanced Molecular Approaches
CRISPR-Based Genetic Engineering: CRISPR-Cas systems enable precise genetic modifications in probiotic strains, allowing for targeted gene insertions, deletions, or alterations to enhance therapeutic efficacy [68]. For instance, engineered Escherichia coli Nissle 1917 has been modified with a type I-E CRISPR-Cas system to target and degrade antibiotic resistance genes in the gut microbiome, reducing horizontal gene transfer [68].
Multi-Omics Integration: Combining metagenomics, metatranscriptomics, metaproteomics, and metabolomics provides comprehensive insights into host-microbiome interactions [68] [71]. The Integrative Human Microbiome Project has demonstrated how longitudinal multi-omics data can reveal associations between specific microbes (e.g., Faecalibacterium prausnitzii, Escherichia coli) and functional outputs in inflammatory bowel disease [68].
Microbiome Acquisition and Early Life Programming
A reconceptualized framework for microbiome transmission emphasizes four key components: What (transmitted cells or microbial components), Where (body sites involved), Who (transmission sources), and When (developmental timing) [42]. Understanding these parameters is crucial for developing early-life interventions that appropriately program the developing microbiome, with potential long-term health implications [42].
Personalized Nutrition
Interindividual variability in microbiome response to dietary interventions presents both a challenge and opportunity for personalized approaches [73]. Baseline microbiome features, including functional redundancy, enterotype, and specific taxonomic composition, can predict intervention responsiveness [73]. Future strategies will likely involve microbiome profiling to tailor prebiotic, probiotic, and synbiotic interventions for maximal individual benefit.
Targeted nutritional interventions using prebiotics, probiotics, and synbiotics represent powerful tools for modulating the human gut microbiome and restoring microbial balance. Through well-characterized mechanisms including competitive exclusion, barrier enhancement, immunomodulation, and selective microbial stimulation, these interventions demonstrate efficacy across various gastrointestinal and metabolic conditions. Advanced experimental models, from continuous in vitro gastrointestinal simulators to gnotobiotic animal systems, provide robust methodologies for investigating intervention effects. Future research directions emphasizing CRISPR-based engineering, multi-omics integration, and personalized approaches will further advance this field, offering promising strategies for microbiome-based therapeutics in human health and disease.
Manufacturing and Standardization Hurdles in Scaling Microbiome Therapeutics
The human microbiome, comprising trillions of microorganisms inhabiting various body sites, plays a fundamental role in regulating immunity, metabolism, and therapeutic responsiveness across the lifespan [74]. The global microbiome therapeutics market is projected to grow from $212.1 million in 2024 to $3.2 billion by 2034, reflecting a compound annual growth rate (CAGR) of 31.1% [75]. Similarly, the broader human microbiome market is expected to reach $1.52 billion by 2030, rising at a CAGR of 16.28% [76] [26]. Despite this rapid market expansion and promising clinical applications, significant manufacturing and standardization hurdles impede the widespread commercialization and clinical translation of microbiome-based therapies.
The transition from laboratory-scale research to industrial-scale production presents unique challenges for live biotherapeutic products (LBPs). These challenges stem from the inherent biological complexity of microbial communities, the technical difficulties in maintaining viability and function during manufacturing, and the absence of universally accepted standards for quality control and efficacy assessment [77] [78]. This whitepaper examines these critical hurdles within the context of human microbiome research and details the methodological advances necessary to overcome them.
Key Manufacturing Hurdles in Industrial Scaling
Biological Complexity and Process Control
Manufacturing live microbial therapeutics introduces complexities absent from conventional pharmaceutical production. Unlike small-molecule drugs, live biotherapeutic products (LBPs) consist of single or multiple bacterial strains that require precise, controlled growth conditions to maintain viability, stability, and therapeutic function [77].
- Anaerobic Cultivation Requirements: Many gut-derived therapeutic species are obligate anaerobes, requiring oxygen-free environments throughout manufacturing. Industrial-scale anaerobic fermentation demands specialized equipment and monitoring systems to maintain strict anaerobiosis [77].
- Batch-to-Batch Variability: Minor discrepancies in fermentation conditions (pH, temperature, nutrient availability) can significantly alter the composition and function of microbial consortia, leading to inconsistent final products [75].
- Viability and Stability Preservation: Ensuring microbial viability through fermentation, harvesting, formulation, and storage presents substantial challenges. Stabilization techniques like lyophilization must be optimized for each strain to maintain therapeutic potency [77].
Analytical and Quality Control Challenges
The complexity of microbiome therapeutics complicates the establishment of critical quality attributes (CQAs) essential for quality control.
- Potency and Functionality Assessment: For many microbiome therapeutics, the mechanisms of action are not fully characterized, making it difficult to establish relevant potency assays beyond simple viability counts [78].
- Characterization of Complex Consortia: Multi-strain products require analytical methods to quantify the relative abundance of each strain and verify community structure throughout shelf life [78].
- Contamination Control: Maintaining purity in multi-strain fermentation requires rigorous monitoring to prevent cross-contamination or overgrowth of production strains [77].
Table 1: Key Manufacturing Challenges and Technical Implications
| Manufacturing Challenge | Technical Implication | Impact on Scalability |
|---|---|---|
| Anaerobic cultivation | Requires specialized bioreactors and monitoring systems | Increases capital investment and operational complexity |
| Batch-to-batch variability | Necessitates extensive process validation and in-process controls | Limits production consistency and increases rejection rates |
| Viability preservation | Demands optimized cryopreservation or lyophilization protocols | Affects shelf-life stability and therapeutic efficacy |
| Complex consortia characterization | Requires advanced analytics for community structure verification | Complicates quality control and release testing |
Standardization Barriers Across the Development Pipeline
Pre-analytical Variability
Inconsistent sample collection, processing, and storage methods introduce significant variability that compromises data comparability across studies and institutions [79]. The Clinical-Based Human Microbiome Research and Development Project (cHMP) in the Republic of Korea has documented extensive protocols to address these challenges, highlighting the meticulous attention required for reliable microbiome research [79].
- Specimen Collection Heterogeneity: Collection methods vary by body site, requiring specific protocols for gastrointestinal, urogenital, respiratory, oral, and skin specimens. For example, gut microbiome analysis typically utilizes fecal specimens, with a minimum of 1g of solid stool or 5mL of liquid stool required, with condition recorded according to the Bristol stool chart [79].
- Storage and Transportation Conditions: Time-to-freezing, temperature stability during transport, and freeze-thaw cycles can dramatically alter microbial composition. Standardized protocols specifying immediate freezing at -80°C or use of stabilization buffers are critical but not universally implemented [79].
- DNA Extraction Method Bias: Different DNA extraction methods vary significantly in extraction efficiency, shearing, and representation of Gram-positive versus Gram-negative bacteria, dramatically impacting downstream sequencing results [78].
Analytical Standardization Gaps
The absence of standardized analytical protocols and reference materials hampers reproducibility and comparability across studies and manufacturing facilities.
- Bioinformatics Pipeline Variability: Different bioinformatics tools for taxonomic profiling demonstrate significant variability in sensitivity, false positive rates, and diversity estimates. One study evaluating five common bioinformatics tools (MetaPhlAn2, Kraken, Bracken, Kaiju, and Centrifuge) found a notable trade-off between sensitivity and the relative abundance of false positives in final datasets [78].
- Missing Reference Materials: Until recently, no accredited or certified reference materials existed for microbiome analysis. The National Institute for Biological Standards and Control (NIBSC) has developed DNA reference reagents (Gut-Mix-RR and Gut-HiLo-RR) consisting of 20 common gut microbiome strains in both even and staggered compositions to address this gap [78].
- Diversity Metric Calculation: Different algorithms for calculating alpha and beta diversity can lead to conflicting interpretations of the same underlying data, complicating cross-study comparisons and clinical application [61].
Table 2: Standardization Initiatives and Frameworks
| Standardization Area | Current Initiative | Development Stage |
|---|---|---|
| Reference reagents | NIBSC Gut-Mix-RR and Gut-HiLo-RR | Candidate WHO International Reference Reagents [78] |
| Clinical metadata collection | cHMP case report forms | Implemented in Korean national project [79] |
| Bioinformatics reporting | Four-measure framework (sensitivity, FPRA, diversity, similarity) | Proposed evaluation system [78] |
| Regulatory pathways | FDA approvals of Vowst (2023) and Rebyota (2022) | Established precedent for LBPs [75] |
| Manufacturing quality control | Anaerobic fermentation platforms with real-time monitoring | Commercial implementation [77] |
Emerging Solutions and Methodological Advances
Manufacturing Innovation
Advanced manufacturing platforms are emerging to address the unique challenges of microbiome therapeutic production.
- Anaerobic Fermentation Platforms: Closed-system bioreactors with integrated oxygen monitoring and control enable scalable cultivation of oxygen-sensitive species. These systems incorporate real-time adjustment of nutrient feeds based on metabolic activity monitoring [77].
- Formulation and Stabilization Technologies: Advanced lyophilization protocols using proprietary cryoprotectant formulations improve viability retention and shelf-life stability. Microencapsulation technologies protect strains during gastrointestinal transit [77].
- Process Analytical Technologies (PAT): Integration of inline sensors and automated sampling systems enables real-time monitoring of critical process parameters, facilitating better control and earlier intervention [77].
Standardization Frameworks
Several initiatives are developing comprehensive standardization frameworks to improve reproducibility and reliability.
- Reference Reagents and Reporting Standards: The NIBSC has developed a four-measure framework for evaluating bioinformatics tool performance: (1) sensitivity (true positive rate), (2) false positive relative abundance (FPRA), (3) diversity (observed species), and (4) similarity (Bray-Curtis index) [78].
- Clinical Metadata Standards: The cHMP protocol mandates comprehensive clinical metadata collection, including demographic information, medication history (especially antibiotic exposure within 6 months), dietary habits, and disease-specific clinical parameters, with a target missing data rate of less than 10% [79].
- Integrated Databases: National-level databases, such as the cHMP repository at the Korea National Institute of Health, enable data sharing and comparative analysis using standardized data formats and metadata structures [79].
Experimental Protocols for Manufacturing and Standardization
Standardized DNA Extraction and Sequencing Protocol
The cHMP has established rigorous protocols for DNA extraction and sequencing to ensure data consistency [79].
Sample Collection and Storage
- Collect specimens according to body-site specific protocols (e.g., fecal samples: ≥1g solid or 5mL liquid)
- Record specimen condition using standardized metrics (e.g., Bristol stool chart for feces)
- Immediately freeze at -80°C or place in specified stabilization buffers
- Document time-to-freezing and storage conditions in metadata
- Transport on dry ice with temperature monitoring
DNA Extraction and Quality Control
- Use validated extraction kits with mechanical lysis for Gram-positive bacteria
- Include extraction controls to monitor contamination
- Assess DNA concentration using fluorometric methods (e.g., Qubit)
- Verify DNA quality via spectrophotometry (A260/280 ratio) and fragment analysis
- Minimum quality thresholds: DNA concentration ≥5ng/μL, A260/280 ≥1.8, fragment size >10kb
Library Preparation and Sequencing
- For shotgun metagenomics: use dual-indexed library preparation with PCR amplification minimization
- For 16S rRNA sequencing: target the V3-V4 hypervariable region with primers 341F/806R
- Include negative controls (extraction and PCR blanks) and positive controls (mock communities)
- Sequence on Illumina platforms with minimum depth of 10 million reads per sample for shotgun, 50,000 reads per sample for 16S rRNA
Manufacturing Process Validation Protocol
A structured approach to process validation ensures consistent production of microbiome therapeutics [77].
Fermentation Process Optimization
- Inoculum preparation: Maintain master and working cell banks with comprehensive characterization
- Media optimization: Screen multiple carbon sources, nitrogen sources, and growth factors
- Parameter optimization: Systematically evaluate temperature, pH, agitation, and feeding strategies
- Scale-up studies: Execute 10L → 100L → 1000L scale transitions with comparative metabolomics
Harvesting and Stabilization
- Biomass recovery: Evaluate centrifugation versus tangential flow filtration for yield and viability
- Cryoprotectant screening: Test multiple excipient combinations for lyophilization survival
- Lyophilization cycle development: Optimize freezing rate, primary drying temperature, and secondary drying parameters
- Stability testing: Monitor viability at 4°C, 25°C, and 40°C with 0%, 60% relative humidity
Quality Control Analytics
- Potency assays: Develop strain-specific functional assays (e.g., short-chain fatty acid production)
- Purity testing: Sterility testing per USP <71>, endotoxin testing per USP <85>
- Identity confirmation: Strain-specific PCR or whole-genome sequencing on final product
- Community composition: 16S rRNA sequencing for multi-strain products
Diagram 1: Microbiome Therapeutic Manufacturing and Quality Control Workflow. This diagram illustrates the integrated manufacturing process with critical quality control checkpoints necessary for consistent production of live biotherapeutic products.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Microbiome Therapeutic Development
| Reagent/Material | Function | Application in Microbiome Research |
|---|---|---|
| NIBSC Gut-Mix-RR & Gut-HiLo-RR | DNA reference reagents with known composition | Benchmarking bioinformatics pipelines, validating sequencing methods [78] |
| Anaerobic fermentation systems | Specialized bioreactors maintaining oxygen-free conditions | Cultivation of obligate anaerobic strains for therapeutic development [77] |
| Stabilization buffers (e.g., RNA later, glycerol solutions) | Preserve microbial composition during storage | Pre-analytical sample stabilization for DNA/RNA analysis [79] |
| Mock microbial communities | Defined mixtures of microbial strains with known proportions | Process validation, analytical method development, inter-laboratory comparisons [78] |
| Standardized DNA extraction kits | Consistent nucleic acid isolation across samples | Minimizing technical variability in DNA extraction [79] |
| Biorepository and cell banking systems | Long-term preservation of microbial strains | Maintenance of master and working cell banks for manufacturing [77] |
The transformation of microbiome research into reliable therapeutics hinges on overcoming significant manufacturing and standardization challenges. While promising solutions are emerging—including advanced anaerobic fermentation platforms, reference reagents, and standardized protocols—collaborative effort across academia, industry, and regulatory bodies remains essential. Initiatives like the ASM's Microbiome to Medicine are working to develop consensus standards, accelerate clinical validation, and align regulatory pathways [80]. The continued development and widespread adoption of standardized materials, such as the NIBSC reference reagents, and rigorous experimental protocols, as exemplified by the cHMP guidelines, will be crucial for advancing microbiome therapeutics from bench to bedside [79] [78]. Through coordinated efforts to address these manufacturing and standardization hurdles, the field can realize the immense therapeutic potential of the human microbiome for treating chronic diseases, optimizing cancer therapy, and advancing personalized medicine.
Diagram 2: Challenges, Solutions, and Outcomes in Microbiome Therapeutic Development. This framework illustrates the interconnected nature of manufacturing and standardization hurdles and the integrated solutions required to advance the field.
Validating Microbiome Science: Clinical Evidence, Market Growth, and Comparative Analysis
The human microbiome, a complex and dynamic ecosystem of microorganisms, is now recognized as a fundamental determinant of human physiology, playing critical roles in immunity, metabolism, and neurodevelopment [11]. This collective of microbes maintains continuous crosstalk with the human genome, influencing a broader spectrum of individual phenotypic variations than previously appreciated [1]. Conceptual frameworks such as the "innate and adaptive genomes" have enhanced our genetic and evolutionary understanding of the human genome, where the "adaptive genome" refers to the external and dynamic microbiome, while the "innate genome" denotes the inherent genetic blueprint [1]. The "germ-free syndrome" concept challenges the traditional 'microbes as pathogens' view, demonstrating the necessity of microbes for health through abnormalities observed in germ-free animals [1].
Within this paradigm, recurrent Clostridioides difficile infection (rCDI) represents a clear manifestation of microbiome disruption, where standard antibiotic therapy further perpetuates dysbiosis, creating a vicious cycle of recurrence [48] [81]. This review examines the clinical validation of microbiome-based interventions—specifically fecal microbiota transplantation (FMT) and live biotherapeutic products (LBPs)—for rCDI, while exploring their expanding therapeutic indications, all framed within the broader context of human microbiome anatomy, development, and stabilization research.
Microbial Distribution and Stability: Foundations for Therapeutic Intervention
Anatomical Distribution and Developmental Trajectory
The human microbiome is not uniformly distributed throughout the body. The gastrointestinal tract harbors the most complex and dense microbial community (approximately 29% of the body's total), followed by the oral cavity (26%), skin (21%), respiratory tract (14%), and urogenital tract (9%) [1]. These communities exhibit density gradients within specific organs and undergo predictable successional development throughout the human lifespan [1].
The neonatal period represents a critical window for microbial colonization, primarily dictated by maternal microbial transmission and environmental exposures. Vaginal delivery facilitates transfer of Lactobacillus, Prevotella, and Sneathia, while cesarean delivery is associated with enrichment of skin-derived taxa like Staphylococcus and Corynebacterium, and delayed acquisition of commensals such as Bifidobacterium [11]. This early divergence has been linked to long-term health consequences, including increased risk of immune dysregulation and metabolic disorders [11]. The gut microbiome generally reaches a stable, adult-like configuration by approximately 2-3 years of age, establishing a core microbiome that provides functional resilience while remaining modifiable by diet, antibiotics, and other environmental factors throughout life [11].
Conceptual Framework for Microbiome Therapeutics
Understanding microbiome therapeutics requires several key conceptual frameworks:
- "Acquired microbial immunity": This concept positions the microbiome as an adjunct to the human immune system, providing colonization resistance against pathogens and immune modulation, forming the rationale for probiotic therapies and prudent antibiotic use [1].
- "Homeostatic reprogramming hypothesis": This integrates the microbiome into the internal environment theory, potentially explaining changes in homeostatic indicators post-industrialization and providing a basis for therapeutic microbiome manipulation [1].
- "Cell-microbe co-ecology model": This elucidates the symbiotic regulation affecting cellular balance, providing mechanistic insights into how microbial interventions can restore ecological balance in dysbiotic conditions [1].
These frameworks establish the theoretical foundation for microbiome-based interventions, particularly for conditions like rCDI where dysbiosis is a central feature of the disease pathogenesis.
Clinical Trial Methodologies for FMT and LBPs
Distinguishing Efficacy from Effectiveness in Microbiome Trials
In evaluating microbiome-based interventions, it is crucial to distinguish between efficacy trials (explanatory trials) that determine whether an intervention produces expected results under ideal circumstances, and effectiveness trials (pragmatic trials) that measure beneficial effects in "real-world" clinical settings [82]. These exist on a continuum, with trade-offs between internal validity (control over variables) and external validity (generalizability to broader populations) [82].
For microbiome interventions, key design considerations include:
- Patient characteristics: Age, microbiome baseline status, prior treatments, comorbidities
- Intervention protocols: Donor screening, preparation methods, administration routes, dosage
- Outcome measures: Clinical resolution, microbiome engraftment, safety parameters
- Follow-up duration: Short-term resolution vs. long-term sustainability
Experimental Protocols for FMT and LBP Trials
Sample Preparation and Administration: FMT products like REBYOTA (fecal microbiota, live-jslm) consist of a liquid mix of up to trillions of live microbes, including Bacteroides, derived from prescreened healthy donors [48] [81]. In the CDI-SCOPE trial, participants received a single 150-mL dose administered to the right colon between the ileocecal valve and hepatic flexure via colonoscopy, following a 24- to 72-hour antibiotic washout period and bowel preparation [48]. Bowel preparation methods and colonoscopy procedures were determined at the investigator's discretion to reflect real-world practice [48].
Study Design and Endpoints: The CDI-SCOPE trial employed a single-arm exploratory Phase IIIb design conducted at 12 sites in the United States [48]. The primary endpoint was RBL-related treatment-emergent adverse events (TEAEs) through 8 weeks after administration or confirmed treatment failure. Treatment failure was defined as the presence of CDI-associated diarrhea and a positive test for C. difficile toxin within 8 weeks, while treatment success was defined as the absence of CDI-associated diarrhea for 8 weeks [48]. Follow-up visits occurred at 1, 2, 4, and 8 weeks, and 3 and 6 months after administration to assess both immediate and sustained outcomes [48].
Microbiome Analysis: While not detailed in the cited trials, comprehensive microbiome assessment typically includes:
- Sequential stool sample collection pre- and post-intervention
- 16S rRNA gene sequencing for taxonomic profiling
- Shotgun metagenomics for functional gene analysis
- Metabolomic profiling of short-chain fatty acids and other relevant metabolites
- Engraftment analysis to determine donor microbe persistence
Table 1: Key Methodological Elements in FMT/LBP Clinical Trials for rCDI
| Trial Component | Key Considerations | Examples from Cited Studies |
|---|---|---|
| Study Population | Adults with recurrent CDI (≥1 recurrence); completion of antibiotic course for current episode | CDI-SCOPE: 41 participants with mean age 61.2 years; 43.9% with 1 recurrence, 31.7% with 2, 24.4% with ≥3 [48] |
| Intervention Protocol | Single administration via colonoscopy, enema, or capsules; standardized donor screening | REBYOTA: 150mL single dose via colonoscopy to right colon; 24-72 hour antibiotic washout [48] |
| Comparison Group | Standard antibiotic therapy (vancomycin, fidaxomicin) | Meta-analysis: FMT vs. standard antibiotic therapy [83] |
| Primary Outcomes | Treatment success (no recurrence) at 8 weeks; safety and adverse events | CDI-SCOPE: Primary endpoint - RBL-related TEAEs through 8 weeks [48] |
| Follow-up Period | Short-term (8 weeks) and long-term (6 months) assessment of efficacy and safety | CDI-SCOPE: Assessments at 1, 2, 4, 8 weeks, 3 and 6 months [48] |
Efficacy and Effectiveness Data for rCDI
Clinical Trial Results
Recent clinical trials demonstrate compelling efficacy for microbiota-based interventions in rCDI. A comprehensive systematic review and meta-analysis of 15 studies with 1,452 patients found FMT significantly more effective than antibiotics for rCDI (relative risk = 1.85, 95% CI: 1.62-2.11, p < 0.001), with recurrence rates of 16% for FMT versus 42% for antibiotics [83]. Subgroup analyses demonstrated consistent efficacy regardless of administration method (colonoscopy, nasogastric tube, or capsules) [83].
The CDI-SCOPE trial of fecal microbiota, live-jslm (RBL) administered via colonoscopy reported 95.1% treatment success (no CDI recurrence) at 8 weeks [48]. Through 6 months of follow-up, 92.7% of participants (38/41) did not experience further CDI episodes, with only one patient (2.4%) experiencing recurrence between 8 weeks and 6 months [48]. This demonstrates sustained clinical effectiveness beyond the initial post-treatment period.
Real-World Evidence and Quality of Life Impact
Real-world evidence complements clinical trial data and demonstrates effectiveness in routine practice. Two real-world analyses of REBYOTA presented at IDWeek 2025 showed consistent results [81]. In one study of 128 patients with rCDI treated in physician offices, 75% achieved treatment success at 8 weeks, while among 40 patients who completed health-related quality of life (HR-QOL) surveys using the validated Cdiff32 instrument, scores significantly improved from 41.4 ± 17.3 at baseline to 57.5 ± 17.8 at week 8 [81]. This 16-point gain exceeds the minimal clinically important difference for the instrument, indicating clinically meaningful benefit across physical, mental, and social functioning domains [81].
A second ongoing prospective registry reported interim results showing 82.9% treatment success (63/76 patients; 95% CI, 72.5%-90.6%) at 8 weeks [81]. In the subgroup that received REBYOTA after an antibiotic washout period >72 hours, treatment success was 87.8% (36/41) [81]. These real-world outcomes, while slightly lower than rigorous clinical trial results, demonstrate substantial effectiveness in routine clinical practice.
Table 2: Comparative Efficacy and Safety of Microbiome Therapies vs. Standard Care for rCDI
| Parameter | FMT/LBP | Standard Antibiotics | Data Source |
|---|---|---|---|
| Clinical Efficacy | 75-95.1% treatment success at 8 weeks | 42% recurrence rate | [83] [48] [81] |
| Long-term Durability | 92.7% no recurrence at 6 months | High recurrence rates (up to 65% after first recurrence) | [48] [81] |
| Common Adverse Events | Abdominal pain (8.9%), diarrhea (7.2%), bloating (3.9%), gas (3.3%), nausea (3.3%) | GI disturbances, potential for further dysbiosis | [48] [81] |
| Serious Adverse Events | 7.3% in clinical trials (none related to RBL); 7.9% in real-world | C. diff recurrence, complications like toxic megacolon | [48] [81] |
| Quality of Life Impact | Significant improvement in HR-QOL scores (+16 points on Cdiff32) | Limited data, typically impaired QOL due to recurrence | [81] |
Safety Considerations and Adverse Event Profiles
Safety data from clinical trials and real-world studies provide reassurance for microbiota-based therapies. In the CDI-SCOPE trial through 6 months, 23 participants (56.1%) experienced 69 TEAEs, with 94.2% being mild or moderate in severity [48]. Serious TEAEs occurred in three participants (7.3%), none of which were related to RBL or its administration, and no TEAEs led to discontinuation or death [48]. Between 8 weeks and 6 months post-administration, only one TEAE (irritable bowel syndrome) was considered RBL-related and was mild in severity [48].
Real-world safety data align with clinical trial findings. In the registry study of 76 patients receiving REBYOTA, 18 (23.7%) experienced an adverse event, 6 (7.9%) experienced a serious AE, and only 3 (3.9%) had AEs assessed as related to REBYOTA [81]. There was one fatal AE during the study, considered unrelated to REBYOTA [81]. This collective safety profile supports the favorable risk-benefit ratio of microbiota-based therapies for rCDI.
Expanding Therapeutic Indications Beyond rCDI
The success of FMT and LBPs in rCDI has catalyzed exploration of microbiome-based interventions for other conditions characterized by dysbiosis. Research is underway investigating applications in:
- Inflammatory Bowel Disease (IBD): Both Crohn's disease and ulcerative colitis involve significant microbiome alterations, and early trials show potential for microbiota modulation to induce and maintain remission [11].
- Metabolic Disorders: Obesity, type 2 diabetes, and non-alcoholic fatty liver disease have distinct microbiome signatures, with interventions targeting microbial composition and metabolite production [11].
- Neurological and Psychiatric Conditions: The gut-brain axis provides a mechanistic pathway for microbiome influences on neurodevelopment, mood disorders, and potentially neurodegenerative diseases [11].
- Oncology: Microbiome composition affects responses to cancer immunotherapy, particularly immune checkpoint inhibitors, suggesting potential for microbiome modulation to enhance treatment efficacy [11].
- Autoimmune Conditions: Conditions like multiple sclerosis, rheumatoid arthritis, and systemic lupus erythematosus show associations with specific microbiome patterns [11].
The conceptual framework of "slave tissue" underscores the symbiotic intricacies between human tissues and their microbial counterparts, highlighting the dynamic health implications of microbial interactions across multiple disease states [1].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Tools for Microbiome Therapeutic Development
| Tool/Category | Specific Examples | Research Application |
|---|---|---|
| Microbiome Assessment | 16S rRNA sequencing, Shotgun metagenomics, Metatranscriptomics, Metabolomics | Comprehensive characterization of microbial community structure and function pre- and post-intervention |
| Donor Screening | Serological testing, Stool pathogen testing, Health history assessment | Ensure safety of donor material for FMT and source material for LBPs |
| Product Formulation | Cryopreservation solutions, Stabilization buffers, Capsule technology | Maintain microbial viability and function during storage and administration |
| Administration Methods | Colonoscopy equipment, Nasogastric tubes, Enteric-coated capsules | Deliver microbial consortia to appropriate gastrointestinal sites |
| Animal Models | Germ-free mice, Humanized microbiota mice, CDI mouse models | Investigate mechanisms and efficacy in controlled systems before human trials |
| Cell Culture Systems | Gut-on-a-chip, Organoids, Co-culture with human cells | Study host-microbe interactions at cellular and molecular levels |
Mechanisms and Workflows: Visualizing Microbiome Therapeutics
Diagram 1: Mechanism of Action of FMT/LBPs in rCDI. This diagram illustrates the sequential process by which FMT and LBPs restore microbial balance and facilitate clinical recovery in recurrent Clostridioides difficile infection through multiple complementary mechanisms.
Diagram 2: Clinical Trial Workflow for FMT/LBP Evaluation. This diagram outlines the key methodological steps in clinical trials of fecal microbiota transplantation and live biotherapeutic products, from donor screening through long-term outcome assessment.
The clinical validation of FMT and LBPs for rCDI represents a landmark achievement in microbiome therapeutics, demonstrating the profound clinical impact of restoring a healthy microbial ecosystem. Framed within the broader understanding of human microbiome anatomy, development, and stabilization, these interventions operationalize concepts like "acquired microbial immunity" and "homeostatic reprogramming" [1]. The consistent demonstration of superior efficacy compared to standard antibiotics, coupled with acceptable safety profiles and significant quality of life improvements, positions microbiota-based therapies as transformative approaches for rCDI [83] [48] [81].
Future directions include optimizing donor selection, standardizing production protocols, refining administration methods, identifying predictive biomarkers of response, and expanding to novel therapeutic indications. As our understanding of the "meta-host" model evolves—viewing the human host and its microbiome as an integrated unit—the potential for microbiome-based interventions across diverse disease states continues to expand [1]. The successful translation of FMT and LBPs for rCDI provides both a proof-of-concept and a methodological roadmap for this new therapeutic paradigm.
The projected expansion of the global human microbiome market from USD 791 million in 2025 to USD 6.09 billion by 2035, at a compound annual growth rate (CAGR) of 20.4%, represents more than a financial forecast [84] [85]. This growth trajectory validates the intensifying research into the anatomy, development, and stabilization of human microbial communities and their profound implications for therapeutic and diagnostic innovation. The market's momentum is directly fueled by scientific advancements in understanding the human as a holobiont—a complex superorganism comprised of human and microbial cells that co-evolve and function as a single biological unit [86]. This whitepaper provides an in-depth technical analysis for researchers, scientists, and drug development professionals, framing commercial validation within the core biological principles of human-microbe symbiosis.
Quantitative Market Projections
The table below summarizes key quantitative projections from recent market analyses, illustrating a consistent and robust growth outlook across multiple segments.
Table 1: Global Human Microbiome Market Size and Growth Projections
| Metric | 2024/2025 Baseline | 2035 Projection | CAGR (%) | Source |
|---|---|---|---|---|
| Overall Market | USD 791 million (2025) [84] | USD 6.09 billion [84] | 20.4% [84] | ResearchAndMarkets.com |
| Alternative Projection | USD 1.37 billion (2025) [87] | USD 11.31 billion [87] | 23.5% [87] | Research Nester |
| Therapeutics Segment Growth | - | - | 32.0% (2025-2035) [88] | Roots Analysis |
| Diagnostics Segment Growth | - | - | ~53.0% (Annualized) [84] | ResearchAndMarkets.com |
Market Segmentation and Dominant Trends
The market's composition reveals the therapeutic areas and product categories attracting the most significant research and investment interest.
Table 2: Market Segmentation and Key Dominant Trends (2025)
| Segmentation Axis | Dominant Segment | 2025 Market Share/Comment | Key Driver |
|---|---|---|---|
| By Product Type | Diagnostics [88] | ~45% share [88] | Early screening for metabolic & oncological disorders [88] |
| By Therapeutic Area | Infectious Diseases [88] | 100% of therapeutics market [88] | Success of FMT for recurrent C. difficile [88] |
| By Biologic Type | Live Biotherapeutics [88] | Entire therapeutics share [88] | Efficacy in GI, metabolic & oncological disorders [88] |
| By Route of Administration | Oral [88] | 55% share [88] | Safety, convenience, and direct therapeutic intervention [88] |
| By Drug Formulation | Capsule [88] | 55% share [88] | Robust clinical trial pipeline in this formulation [88] |
| By Geography | North America [88] | 95% of therapeutics market [88] | Advanced infrastructure and high number of clinical trials [88] |
Scientific Framework: From Microbial Anatomy to Clinical Translation
The market growth is predicated on an evolving scientific framework that moves beyond correlation to establish causation and mechanism.
Conceptual Models of the Human-Microbe Relationship
Advanced theoretical models are reshaping our fundamental understanding of human biology:
- The Innate and Adaptive Genomes: The "innate genome" is the inherent human genetic blueprint, while the "adaptive genome" comprises the dynamic microbiome, offering a genetic flexibility far exceeding the human genome [1] [89].
- The Meta-Host Model: This model broadens the definition of the host to include its symbiotic microbial communities, which are essential for understanding disease heterogeneity and treatment outcomes [1].
- Germ-Free Syndrome: Observations from germ-free animals demonstrate that the absence of microbes leads to a wide range of physiological abnormalities, challenging the "microbes as pathogens" paradigm and confirming their necessity for health [1].
- The Slave Tissue Concept: This hypothesis posits that the microbiome acts as an exogenous, controlled tissue under the master regulation of human nervous, connective, epithelial, and muscle tissues, highlighting a complex, symbiotic relationship [1].
Anatomical Distribution and Biogeography
The human microbiome is not uniformly distributed but occupies specific anatomical niches with distinct community structures [1] [89]. Metagenomic studies reveal that the gastrointestinal tract is the most densely populated site (29%), followed by the oral cavity (26%) and skin (21%), with the respiratory tract (14%) and urogenital tract (9%) having lower densities [1]. Each body site develops a specific biogeography, and even within organs, density gradients exist, such as the higher microbial density in the lower gastrointestinal tract compared to the upper GI tract [1]. Sites traditionally considered sterile, including the brain, vasculature, and placenta, are now being re-evaluated, though evidence for resident microbiomes in these areas remains controversial and requires further validation with stringent contamination controls [1].
Experimental Methodologies for Microbiome Research
Protocol 1: Longitudinal Metagenomic Analysis of Gut Microbiome Maturation
This protocol is designed to trace the development and stabilization of the infant gut microbiome in response to dietary changes [90].
1. Sample Collection:
- Cohort: Recruit a cohort of 98 mother-infant dyads.
- Sample Type: Serial fecal samples from infants and mothers.
- Frequency: Collect infant samples at birth (meconium), and then at regular intervals (e.g., weekly, monthly) throughout the first year of life and beyond.
- Metadata: Meticulously record metadata including mode of delivery (vaginal vs. C-section), feeding type (breastfeeding vs. formula), introduction of solid foods, antibiotic use, and health status.
2. DNA Extraction and Metagenomic Sequencing:
- Extraction: Use a standardized, bead-beating-enhanced DNA extraction kit from all fecal samples to ensure mechanical lysis of robust bacterial cell walls.
- Sequencing: Perform whole-genome shotgun (WGS) sequencing on the extracted DNA. WGS, as opposed to 16S rRNA amplicon sequencing, allows for strain-level identification and functional profiling of the microbial community.
3. Bioinformatic and Statistical Analysis:
- Quality Control: Process raw sequencing reads through a pipeline (e.g., KneadData) to remove low-quality sequences and contaminating host DNA.
- Taxonomic Profiling: Align reads to a curated microbial genome database (e.g., GRCh38, NCBI RefSeq) using a tool like MetaPhlAn for taxonomic assignment and abundance estimation.
- Functional Profiling: Assemble reads into contigs and predict open reading frames (ORFs) to create a gene catalog. Annotate genes against functional databases (e.g., KEGG, eggNOG) using tools like HUMAnN to determine metabolic pathway abundance.
- Maturation Assessment: Analyze longitudinal data to identify the key inflection point for microbiome maturation. Statistical models (e.g., PERMANOVA) will show that the cessation of breastfeeding, not the introduction of solid food, is the primary driver for the transition to an adult-like microbiota structure [90]. Network analysis can be used to observe the development of more complex and stable ecological interactions as the microbiome matures.
Protocol 2: Investigating Host-Microbe Immune Interactions
This protocol outlines a method to dissect the mechanistic links between the microbiome and the host immune system [89].
1. In Vivo Model Setup:
- Animals: Utilize germ-free (GF) mouse models.
- Colonization: Divide GF mice into two groups: one colonized with a defined microbial consortium from a healthy human donor (HC) and another with a consortium from a patient with a specific immune disorder (e.g., IBD). A control group remains germ-free.
- Monitoring: Monitor the mice for a set period post-colonization.
2. Sample Processing and Multi-Omics Data Generation:
- Sample Types: Collect blood, intestinal tissue (for transcriptomics), and fecal samples (for microbiota and metabolome) at sacrifice.
- Immune Phenotyping: By flow cytometry, characterize immune cell populations (e.g., T-regs, Th17, dendritic cells) in the mesenteric lymph nodes and lamina propria of the colon.
- Host Transcriptomics: Perform RNA sequencing (RNA-Seq) on intestinal tissue to assess host gene expression responses.
- Metabolomics: Analyze fecal and serum samples using LC-MS to quantify microbial-derived metabolites (e.g., short-chain fatty acids - SCFAs like butyrate, propionate; bile acids; tryptophan metabolites).
3. Data Integration and Causal Inference:
- Correlation Analysis: Perform integrative analysis (e.g., using MixOmics, MOFA) to correlate specific microbial taxa, their metabolic outputs, and host immune/transcriptomic markers.
- Mechanistic Validation: Isolate specific bacterial strains identified in the analysis. Introduce these strains into GF mice or use them to stimulate immune cell cultures in vitro to validate their causal role in the observed immune phenotype. For example, the introduction of Christensenella strains, which are heritable and negatively correlated with BMI, can be tested for its ability to induce weight loss in mice [89].
Essential Research Reagent Solutions
Successful execution of the aforementioned protocols relies on a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for Microbiome Research
| Reagent / Tool Category | Specific Examples | Function in Research |
|---|---|---|
| DNA Extraction Kits | Kits with bead-beating (e.g., QIAamp PowerFecal Pro) | Ensures mechanical disruption of diverse microbial cell walls for unbiased DNA recovery from complex samples [84]. |
| Standardized Reagent Kits | CosmosID Metagenomic Services Pipeline [91] | Provides an end-to-end, standardized workflow from sample to bioinformatic report, ensuring reproducibility across studies and labs. |
| Organoid/Stem Cell Tech | Intestinal or colonic epithelial organoids [91] | Creates advanced in vitro models that mimic human tissue for studying host-microbe interactions at the mucosal interface without animal models. |
| Microfluidic Devices | GALT's Prospector System [91] | Enables high-throughput isolation, cultivation, and phenotypic screening of previously unculturable microbial species from samples. |
| AI & Bioinformatics Platforms | Proprietary algorithms (e.g., CosmosID, various AI tools) [92] [91] | Analyzes complex multi-omics datasets, identifies disease biomarkers, and predicts therapeutic targets from metagenomic sequencing data. |
| Live Biotherapeutic Products | Defined microbial consortia (e.g., SER-109, MaaT013) [88] [85] | Serve as both investigational products and tools for mechanistic research into microbiome-based therapeutic interventions. |
Visualizing the Conceptual Framework and Research Workflow
Conceptual Framework of Host-Microbiome Interaction
This diagram illustrates the systematic framework for understanding the microbiome's role in human health and disease, integrating concepts like the innate/adaptive genome and the health-illness conversion model [1].
Diagram Title: Host-Microbiome Interaction Framework
Microbiome Maturation Research Workflow
This flowchart outlines the key stages and decision points in the longitudinal study of infant gut microbiome development [90].
Diagram Title: Microbiome Maturation Study Workflow
The robust projected growth of the human microbiome market to USD 6.09 billion by 2035 is intrinsically linked to the maturation of its scientific foundation. Market segments are being shaped by breakthroughs in understanding the anatomical distribution, developmental trajectory, and ecological stabilization of our microbial counterparts. The transition from descriptive, correlative studies to mechanistic, causal understanding—facilitated by advanced DNA sequencing, multi-omics integration, gnotobiotic models, and sophisticated bioinformatics—is de-risking investment and accelerating clinical translation [1] [89]. For researchers and drug developers, this represents a validated and expanding frontier. The ongoing conceptual revolution, framing humans as meta-organisms, ensures that the scientific questions being answered today will continue to fuel the therapeutic and diagnostic innovations of tomorrow.
The human body exists in a state of profound symbiosis with complex microbial communities, collectively known as the microbiome. These ecosystems, particularly within the gastrointestinal tract, demonstrate specific anatomical distribution patterns and successional development throughout the human lifespan, ultimately stabilizing into a mature state that maintains health through colonization resistance, immunomodulation, and metabolic signaling [1] [93]. Disruptions to this delicate equilibrium, termed dysbiosis, are implicated in numerous disease states, driving the development of therapeutic strategies aimed at restoring microbial balance [94].
Three primary therapeutic modalities have emerged: fecal microbiota transplantation (FMT), defined bacterial consortia, and single-strain live biotherapeutic products (LBPs). These approaches represent a spectrum of complexity from entire community replacement to precisely targeted microbial intervention. This review provides a comparative analysis of these strategies, examining their underlying principles, technical requirements, clinical applications, and relative advantages within the context of human microbiome anatomy, development, and stabilization research.
Anatomical and Developmental Foundations of Microbiome Therapeutics
Microbial Distribution and Successional Development
The human microbiome is not uniformly distributed but rather organizes into distinct niches with specific community structures. The gastrointestinal tract exhibits a dramatic density gradient, hosting approximately 29% of the body's microbial residents, followed by the oral cavity (26%), skin (21%), respiratory tract (14%), and urogenital tract (9%) [1]. This spatial organization is established through a successional process beginning at birth, with primary succession characterized by rapid microbial changes that decelerate into a stable "climax community" by adolescence [1].
Early life represents a critical period for microbiome assembly, with vertical transmission from mother to infant during vaginal birth providing initial colonization with foundational taxa such as Bacteroides and Bifidobacterium [93]. This developmental trajectory is influenced by multiple factors, including diet (with human milk oligosaccharides driving Bifidobacterium dominance in breastfed infants), environmental exposures, and antibiotic use [93]. The concept of "germ-free syndrome" observed in animal models underscores the microbiome's necessity for proper immune system development and overall health, highlighting the therapeutic potential of microbiome modulation [1].
Conceptual Framework for Microbial Acquisition
A modern framework for understanding microbiome acquisition considers four key parameters: "what" (microbial cells, structural elements, or metabolites), "where" (source and destination anatomical sites), "who" (transmission sources), and "when" (developmental timing) [95]. This conceptual model provides a systematic approach for designing therapeutic interventions that account for the multidimensional nature of microbial transmission and colonization.
The "slave tissue" hypothesis offers a valuable perspective for therapeutic development, viewing microbial communities as exogenous tissues under the control of human master tissues (nerve, connective, epithelial, and muscle) [1]. This framework emphasizes the intricate symbiotic relationship between host and microbes, with profound implications for understanding the dynamic health implications of microbial interactions.
Therapeutic Modalities: Mechanisms and Methodologies
Fecal Microbiota Transplantation (FMT)
FMT represents the most complex intervention, involving the transfer of an entire microbial community from screened healthy donor stool to a recipient. This approach aims to restore ecological balance through complete ecosystem replacement or augmentation [31]. The therapeutic mechanism extends beyond simple microbial supplementation, transferring not only fecal-associated microbial communities but also microbe-derived metabolites (e.g., short-chain fatty acids, bile acids), phages, archaea, and fungi [94].
Experimental Protocol for FMT Preparation:
- Donor Screening: Rigorous selection based on inclusion criteria (age 18-50 years; no history of symptomatic medical conditions; no antimicrobial treatment within 6 months) [94]
- Fecal Processing: Suspension of donor stool in saline or polyethylene glycol solution (typically 150 mL) with filtration to remove particulate matter [32]
- Quality Assessment: Broad taxonomic analysis at phylum or family level to ensure community representation [31]
- Administration: Typically via colonoscopy, enema, or nasoduodenal tube following antibiotic cessation 12-48 hours pre-procedure [94]
FMT has demonstrated exceptional efficacy for recurrent Clostridioides difficile infection (rCDI), with cure rates of 67-94% in randomized trials and sustained response rates surpassing 80% in select populations [32] [96]. This robust clinical validation led to FDA approval of standardized microbiota-based therapeutics (Rebyota and Vowst) for rCDI prevention [32].
Defined Bacterial Consortia
Defined bacterial consortia represent an intermediate approach between whole-community FMT and single-strain products. These formulations consist of specific, well-characterized bacterial strains selected for complementary functions and synergistic interactions [31]. The underlying premise is that therapeutic effects can be achieved without replicating an entire microbial community by targeting key functional pathways [31].
Experimental Protocol for Consortium Design:
- Strain Identification: Computational analysis of metagenomic datasets to identify taxa depleted in disease states and correlated with positive outcomes [97]
- Functional Validation: In vitro assays assessing bile acid metabolism, short-chain fatty acid production, and pathogen inhibition [97]
- Compatibility Testing: Co-culture experiments to ensure strain coexistence and functional synergy
- Formulation Development: Optimization of growth conditions, fermentation parameters, and lyophilization protocols to maintain viability and functionality [31]
Promising examples include VE303 (an 8-strain consortium by Vedanta Biosciences), which has demonstrated efficacy in preventing rCDI by promoting colonization resistance and bile acid metabolism [36] [97]. Similarly, VE202, another 8-strain consortium, is designed to induce regulatory T-cell responses and anti-inflammatory metabolites for ulcerative colitis [36].
Single-Strain Live Biotherapeutic Products
Single-strain LBPs represent the most targeted approach, utilizing individual microbial strains with specific, well-defined mechanisms of action. These products typically derive from species with documented probiotic capabilities or specific therapeutic functions [98] [31].
Experimental Protocol for Single-Strain LBP Development:
- Strain Selection: Isolation and identification of strains with desired functional attributes (e.g., immunomodulation, metabolite production, pathogen exclusion) [31]
- Genomic Characterization: Comprehensive sequencing to identify virulence factors, antibiotic resistance genes, and metabolic capabilities [31]
- Mechanistic Studies: In vitro and in vivo validation of proposed mechanisms of action (e.g., activation of specific immune pathways, production of therapeutic metabolites) [31]
- Manufacturing Optimization: Development of scaled fermentation and preservation methods maintaining strain viability and functionality [31]
Notable examples include MRx0518 (a single-strain Bifidobacterium longum by 4D Pharma) for oncology, which activates innate and adaptive immunity to augment checkpoint inhibitors [36]. Similarly, Akkermansia muciniphila strains are being developed for metabolic disorders, demonstrating ability to improve insulin sensitivity and weight control [36].
Table 1: Comparative Analysis of Microbiome Therapeutic Approaches
| Parameter | FMT | Defined Consortia | Single-Strain LBPs |
|---|---|---|---|
| Composition | Whole microbial community (bacteria, viruses, fungi, metabolites) | 4-20 defined bacterial strains | Single bacterial strain |
| Regulatory Status | FDA-approved products (Rebyota, Vowst); traditional FMT under enforcement discretion | Investigational (Phase 1-3 clinical trials) | Investigational (Phase 1-3 clinical trials) |
| Mechanism of Action | Ecosystem restoration via community replacement | Targeted restoration of specific functional groups | Precise mechanistic intervention (immunomodulation, metabolite production) |
| Efficacy in rCDI | 70-90% sustained response [32] [96] | Similar to FMT in trials (VE303) [36] | Variable; generally lower than FMT for rCDI |
| Manufacturing Complexity | High (donor variability, screening logistics) | Medium (multi-strain fermentation, compatibility) | Low (single-strain fermentation) |
| Batch-to-Batch Variability | High (donor-dependent composition) | Low (defined composition) | Very low (clonal populations) |
| Safety Profile | Risk of pathogen transmission; generally favorable [96] | Excellent (defined strains with virulence screening) | Excellent (comprehensive characterization) |
| Therapeutic Scope | Broad (multiple indications via ecosystem reset) | Moderate (targeted multi-functional approach) | Narrow (specific mechanistic interventions) |
Comparative Analysis: Advantages and Limitations
Ecological and Therapeutic Considerations
Each therapeutic approach offers distinct ecological advantages based on the nature of the dysbiosis being treated. FMT provides the most comprehensive ecosystem restoration, making it particularly effective for conditions like rCDI where antibiotic exposure has dramatically reduced microbial diversity [32] [96]. The success of FMT in this context stems from its ability to reestablish colonization resistance through diverse microbial interactions that cannot be replicated by simplified communities [93].
Defined consortia balance ecological complexity with manufacturing control, potentially offering more reproducible outcomes than FMT while retaining functional redundancy and metabolic cross-feeding capabilities [31]. This approach enables targeting of specific functional deficiencies without the unpredictability of entire community transfer.
Single-strain LBPs provide the most precise intervention, ideal when a specific mechanistic pathway has been identified as therapeutic [31]. Their reduced complexity facilitates rigorous characterization, manufacturing control, and clear regulatory pathways, though their narrow focus may limit efficacy in complex dysbiosis states.
Manufacturing and Regulatory Challenges
Manufacturing considerations differ significantly across these modalities. Traditional FMT faces substantial challenges in scale-up due to donor availability, screening requirements, and inherent biological variability [31]. While whole-community LBPs like Rebyota simplify administration, they retain many of the manufacturing complexities of traditional FMT.
Defined consortia require sophisticated fermentation capabilities for multiple fastidious anaerobic strains, with careful attention to strain ratios, co-culture versus blended approaches, and lyophilization parameters that vary by strain [31]. Maintaining viability through fermentation, preservation, and storage represents a critical challenge, with survival rates varying significantly by strain and growth phase [31].
Single-strain products offer the most straightforward manufacturing pathway, though fastidious anaerobes still present technical challenges. The reduced complexity facilitates quality control, potency assays, and stability testing [31].
Regulatory pathways have been established through FDA approvals of FMT-based products, providing precedent for microbiome therapeutics [32] [31]. However, regulatory expectations for defined products increasingly require demonstration of strain-level characterization, mechanism of action elucidation, and manufacturing control [31].
Research Tools and Methodologies
Essential Research Reagents and Platforms
Table 2: Essential Research Reagents for Microbiome Therapeutic Development
| Reagent/Platform | Function | Application Examples |
|---|---|---|
| metaWRAP | Metagenomic assembly, binning, and analysis | Strain-level analysis of microbial communities; identification of therapeutic candidates [97] |
| dRep | Dereplication of metagenome-assembled genomes (MAGs) | Identification of non-redundant bacterial strains from metagenomic data [97] |
| GTDB-Tk | Taxonomic classification of bacterial genomes | Standardized taxonomic labeling based on Genome Taxonomy Database [97] |
| GMPT Analysis | Generalized microbe-phenotype triangulation | Identification of protective or permissive strains correlated with clinical outcomes [97] |
| Anaerobic Chamber | Oxygen-free environment for culturing | Propagation of fastidious anaerobic bacteria for consortia development [31] |
| Robust Aitchison Distance | Compositional data analysis metric | Statistical comparison of microbiome profiles between treatment groups [97] |
| Shotgun Metagenomic Sequencing | Comprehensive community profiling | Strain-level tracking of engraftment and community dynamics [97] |
Computational Workflow for Strain Identification
The rational design of defined consortia increasingly relies on computational approaches for identifying therapeutic strains. The following diagram illustrates a representative workflow for strain identification and validation:
Diagram 1: Computational workflow for therapeutic strain identification
Donor Screening and FMT Preparation Protocol
For FMT-based approaches, rigorous donor screening and standardized preparation protocols are essential for safety and efficacy:
Diagram 2: Donor screening and FMT preparation workflow
Clinical Translation and Future Directions
Emerging Applications Beyond CDI
While rCDI remains the most validated indication for microbiome-based therapies, research is rapidly expanding into other clinical areas. Inflammatory bowel disease (IBD) represents a major focus, with FMT demonstrating induction of steroid-free clinical remission with endoscopic improvement in approximately 27% of ulcerative colitis patients versus 8% with placebo [96]. Defined consortia like VE202 are specifically engineered for IBD through induction of regulatory T-cell responses and anti-inflammatory metabolites [36].
Oncology represents another promising frontier, with microbiome therapies being investigated both for mitigating treatment complications and enhancing anti-tumor immunity. MaaT013, an enriched whole-community LBP, has shown promise for acute graft-versus-host disease following stem cell transplantation [36] [31]. Similarly, MRx0518 is being developed to augment checkpoint inhibitor therapy in solid tumors [36].
Metabolic, neurological, and autoimmune conditions are also active areas of investigation, reflecting the broad influence of the microbiome on host physiology. The Akkermansia muciniphila-based product Ak02, for instance, has demonstrated potential for improving insulin sensitivity and weight control in metabolic disorders [36].
Technical Innovations and Field Evolution
The microbiome therapeutics field is evolving toward greater precision and engineering capability. CRISPR-guided phage therapies (e.g., Eligo Bioscience's Eligobiotics) enable selective elimination of antibiotic-resistant bacteria while preserving commensal communities [36]. Engineered microbial strains, such as Synlogic's SYNB1934 for phenylketonuria, incorporate synthetic biology approaches to enhance therapeutic functionality [36].
The concept of "next-generation probiotics" is expanding beyond traditional Lactobacillus and Bifidobacterium species to include promising commensals like Akkermansia muciniphila, Faecalibacterium prausnitzii, and specific Bacteroides strains [98]. These organisms often present manufacturing challenges due to fastidious growth requirements but offer unique therapeutic mechanisms.
From a regulatory perspective, the approval of Rebyota and Vowst has established pathways for microbiome-based biologics, providing precedent for future products [32] [31]. However, traditional FMT continues to play a role in clinical practice, particularly outside the United States where regulatory frameworks vary [32].
The therapeutic modulation of the human microbiome represents a paradigm shift in medical intervention, moving beyond simple pathogen eradication to ecological restoration and precision manipulation. FMT, defined consortia, and single-strain LBPs each occupy distinct therapeutic niches along a spectrum of complexity, from entire community replacement to targeted mechanistic intervention.
FMT provides the most comprehensive ecosystem restoration and remains the gold standard for rCDI, but faces challenges in standardization, scalability, and safety. Defined consortia offer a balanced approach, maintaining functional complexity while enabling manufacturing control and regulatory characterization. Single-strain LBPs provide the most precise intervention for well-defined mechanisms but may lack the functional redundancy needed for complex dysbiosis states.
The optimal therapeutic approach depends on the specific clinical context, nature of the dysbiosis, and mechanistic understanding of the condition. Future advances will likely involve personalized approaches guided by microbiome profiling, combination strategies leveraging multiple modalities, and continued innovation in strain identification, manufacturing, and delivery. As the field matures, microbiome-based therapies are poised to expand beyond gastroenterology into oncology, metabolic disease, neurology, and immunology, fundamentally expanding our therapeutic arsenal for diverse disease states.
The human microbiome, a complex and dynamic system of microbes residing in various anatomical sites, plays a pivotal role in human health and disease. Recent large-scale sequencing initiatives have generated expansive datasets that reveal significant microbial variations across different body sites and disease states [1] [99]. These datasets offer unprecedented opportunities to investigate the role of microbes in human health but present significant analytical challenges due to their complexity, high dimensionality, and heterogeneity [100]. Traditional computational methods often prove insufficient for extracting meaningful patterns from this data deluge, creating a critical gap between data generation and clinical application [101]. Artificial intelligence (AI), encompassing both classical machine learning and modern deep learning approaches, has emerged as a powerful solution to these challenges, enabling researchers to decode the diagnostic and therapeutic potential hidden within microbiome data [100]. This whitepaper explores how AI and big data are transforming microbiome research, from basic understanding to clinical translation, within the broader context of human microbiome distribution, anatomy, development, and stabilization research.
AI Methodologies for Multiscale Microbiome Analysis
AI-driven methodologies enable the extraction of meaningful biological patterns from complex microbial data from a multiscale perspective, facilitating insights into community dynamics, host-microbe interactions, and functional genomics [100]. The integration of multi-omics approaches—including metagenomics, metatranscriptomics, metaproteomics, and metabolomics—provides a comprehensive understanding of host-microbe interactions and serves as a robust hypothesis generator for downstream research [101].
Machine Learning and Deep Learning Approaches
- Clustering Algorithms: Enable the identification of microbial community types and subtypes across different body sites and disease states, facilitating patient stratification [100].
- Dimensionality Reduction Techniques: Methods such as t-SNE and UMAP help visualize high-dimensional microbiome data in two or three dimensions, revealing inherent structures and patterns [100].
- Convolutional and Recurrent Neural Networks: Process spatial and temporal microbiome data respectively, capturing community dynamics and succession patterns throughout human development and disease progression [100].
- Large Language Models: Emerging applications of transformer-based architectures can process biological sequences and uncover complex relationships in microbiome data that traditional methods might miss [100].
Table 1: AI Approaches in Microbiome Research
| AI Methodology | Primary Application | Data Types | Clinical Utility |
|---|---|---|---|
| Clustering Algorithms | Microbial enterotyping, patient stratification | Species abundance, metabolic profiles | Disease subtyping, personalized treatment |
| Dimensionality Reduction | Data visualization, pattern discovery | Multi-omics datasets | Biomarker discovery, hypothesis generation |
| Convolutional Neural Networks | Spatial structure analysis | Imaging data, spatially-resolved metagenomics | Tissue localization, host-microbe interfaces |
| Recurrent Neural Networks | Temporal dynamics analysis | Longitudinal sampling data | Disease progression monitoring, treatment response |
| Large Language Models | Biological sequence analysis | Genomic sequences, protein data | Functional annotation, novel gene discovery |
Analytical Framework for Microbiome Data
A systematic framework for understanding the microbiome integrates knowledge from anatomy, physiology, immunology, histology, genetics, and evolution [1]. Key conceptual advances include:
- Innate and Adaptive Genomes: The "innate genome" refers to the inherent genetic blueprint humans are born with, while the "adaptive genome" encompasses the dynamic microbiome, enhancing genetic and evolutionary understanding of human physiology [1].
- Cell-Microbe Co-ecology Model: Elucidates the symbiotic regulation affecting cellular balance and homeostasis [1].
- Health-Illness Conversion Model: Encapsulates the innate and adaptive genomes' interplay and dysbiosis patterns, providing a framework for understanding disease development [1].
Diagnostic Applications: From Correlation to Causation
AI-powered analysis of microbiome data has significantly advanced diagnostic capabilities across numerous disease states. Large-scale studies employing standardized protocols have generated sequencing data from diverse specimen types, including saliva, plaque, skin, throat, eye, and stool, revealing significant microbial variations across diseases and specimen types, including unexpected anatomical sites [99].
Pan-Body Pan-Disease Diagnostic Approaches
Comprehensive analysis strategies that include diverse specimen types and various diseases are essential for unlocking the full diagnostic potential of microbiomes [99]. This approach has identified hundreds of unexplored species-level genome bins (SGBs), many of which show significant disease associations [99].
Table 2: Representative Diagnostic Biomarkers from Pan-Body Microbiome Analysis
| Disease Condition | Associated Microbiome Alterations | Detection Sites | AI Analysis Method |
|---|---|---|---|
| Periodontitis | Specific microbial consortia in interdental plaque | Oral cavity, saliva | Metagenomic assembly, clustering |
| Cardiovascular Diseases | Proteobacteria, Firmicutes in vasculature | Arterial samples, stool | Contamination-controlled analysis |
| Inflammatory Bowel Disease | Reduced diversity, pathobiont expansion | Stool, mucosal tissue | Longitudinal pattern recognition |
| Multimorbidity Patterns | Characteristic cross-site dysbiosis | Multiple body sites | Network analysis, graph neural networks |
| Metabolic Disorders | Functional gene enrichment | Stool, saliva | Metabolic pathway reconstruction |
Experimental Protocols for Diagnostic Biomarker Discovery
Robust diagnostic biomarker discovery requires standardized protocols from sample collection through data analysis:
- Sample Collection: Prospective collection of specimens from multiple body sites (saliva, plaque, skin, throat, eye, stool) using standardized protocols to ensure comparability [99].
- DNA Extraction and Quality Control: Implement stringent quality control to avoid bias, with exclusion of samples for insufficient DNA quantity or quality [99].
- Shotgun Metagenomic Sequencing: Average sequencing depth of 5.3 gigabases per specimen after removing ambient human DNA [99].
- Metagenomic Assembly and Binning: Reconstruction of microbial genomes and identification of species-level genome bins (SGBs) [99].
- Statistical Analysis and AI Modeling: Identification of disease-associated SGBs using machine learning models trained on clinical metadata [99].
Therapeutic Development and Precision Microbiome Engineering
AI approaches are accelerating therapeutic development by identifying novel therapeutic targets and enabling precision microbiome engineering. The pharmaceutical landscape has long drawn inspiration from nature, with a significant proportion of drugs derived from natural products (NPs) and their producers [99].
Biosynthetic Gene Cluster Discovery for Novel Therapeutics
Microbiome data mining has revealed an extensive repertoire of biosynthetic gene clusters (BGCs) with therapeutic potential. Comprehensive studies have identified 28,315 potential BGCs in human-associated microbiomes, with 1,050 showing significant correlations to diseases [99]. These BGCs represent a promising source for novel therapeutic compounds that remain hidden in classical culture-based studies.
AI-Driven Workflow for Therapeutic Discovery
The iterative process from data generation to clinical translation involves multiple steps:
- Large-Scale Metagenomic Sequencing: Generation of extensive microbiome datasets from well-phenotyped cohorts [99].
- In silico BGC Identification: Computational identification of biosynthetic gene clusters using tools like antiSMASH [99].
- AI-Powered Prioritization: Machine learning models prioritize BGCs based on disease association, novelty, and predicted bioactivity [99].
- Hypothesis Generation: AI models generate testable hypotheses about microbial functions and host-microbe interactions [101].
- Proof-of-Concept Experiments: Validation of AI-generated hypotheses using in vitro and in vivo models to establish causative effects [101].
- Mechanistic Understanding: Deep investigation into the mechanisms underlying observed effects [101].
- Preclinical Development: Translation of validated findings toward clinical applications [101].
Research Reagent Solutions for Microbiome Studies
Table 3: Essential Research Reagents and Platforms for AI-Driven Microbiome Research
| Reagent/Platform | Function | Application in AI Workflow |
|---|---|---|
| High-throughput Sequencing Platforms | Generate metagenomic data | Provides raw data for AI model training and validation |
| antiSMASH | Biosynthetic gene cluster identification | Annotates BGCs for therapeutic discovery pipelines [99] |
| BiG-FAM Database | Repository of BGCs | Reference database for novel BGC discovery and classification [99] |
| ABC-HuMi Database | Human microbiome BGCs | Specialized resource for human-associated BGCs [99] |
| Multi-omics Integration Platforms | Combine metagenomic, metatranscriptomic, metaproteomic, and metabolomic data | Provides comprehensive data for AI pattern recognition [101] |
| Contamination Control Tools | Identify and remove contaminants in low-biomass samples | Ensures data quality for reliable AI analysis [42] |
| Spike-in Quantitative Standards | Quantify microbial abundance in low-biomass samples | Enables accurate measurement for AI models [42] |
Implementation Framework and Future Directions
Successful implementation of AI in microbiome research requires addressing several practical considerations and anticipating future developments in the field.
Data Quality and Standardization Requirements
The foundation of reliable AI analysis is high-quality, standardized data. Key considerations include:
- Standardized Protocols: Employing standardized protocols for sample collection, processing, and sequencing to ensure comparability across studies [99].
- Contamination Control: Implementing stringent controls for contamination, which is particularly crucial for low microbial biomass samples [42].
- Multi-omics Integration: Combining multiple data types (metagenomics, metatranscriptomics, metaproteomics, metabolomics) for a comprehensive understanding [101].
- Clinical Annotation: Rich phenotypic and clinical data collection to enable meaningful correlation with microbial features [99].
Conceptual Frameworks for Microbiome Acquisition
Understanding microbiome transmission and acquisition is fundamental to therapeutic development. A reconceptualized framework for human microbiome transmission in early life based on four key components (4 W) provides a structured approach: what (transmitted commodity), where (body sites), who (transmission sources), and when (timing) [42]. This framework enables more precise characterization of microbiome assembly and its impact on health and disease.
Mathematical Modeling and Community Dynamics
Spatially structured mathematical models of the gut microbiome reveal factors that increase community stability [102]. These models can be enhanced through AI approaches to predict how therapeutic interventions might affect microbial community structure and function over time.
AI and big data are fundamentally transforming microbiome research, enabling the transition from correlative observations to causative understanding and clinical applications. The integration of multiscale AI methodologies with comprehensive multi-omics data provides unprecedented insights into microbiome community dynamics, host-microbe interactions, and functional potential. As these technologies continue to evolve, they promise to accelerate the development of novel diagnostic biomarkers and therapeutic interventions derived from the human microbiome. The future of microbiome-based medicine lies in the continued refinement of AI approaches, improved data standardization, and the translational framework that iteratively connects computational discoveries with experimental validation and clinical implementation.
The regulatory landscape for microbiome-based biologics is undergoing a significant transformation, moving from a framework designed for traditional drugs toward one that accommodates the unique complexities of living microbial therapies. Driving this evolution are scientific advancements demonstrating the microbiome's critical role in human health and the successful approval of the first microbiome-based products. The U.S. Food and Drug Administration (FDA) is responding with new draft guidance, novel approval pathways, and updated enforcement policies aimed at balancing robust safety and efficacy evaluations with the need to foster innovation in this promising field. This whitepaper details the current regulatory pathways, integrates them with the foundational science of human microbiome anatomy and development, and provides a technical resource for researchers and drug development professionals navigating this dynamic environment.
The Microbiome in Human Health: A Foundation for Therapeutics
To fully grasp the regulatory framework for microbiome-based biologics, one must first understand the biological context from which these therapies are derived. The human microbiome, a complex and dynamic ecosystem of microorganisms, is now recognized as a fundamental determinant of human physiology, shaping immunity, metabolism, and neurodevelopment [11].
Anatomical Distribution and Early Life Development
Microbial communities are distributed across various body sites, with the gastrointestinal tract harboring one of the most complex and functionally diverse ecosystems [11]. The initial colonization of the infant gut is a critical period for immune and metabolic programming. The mode of delivery (vaginal vs. cesarean) and early nutrition (breastfeeding vs. formula) are dominant factors shaping the neonatal microbiome, with long-lasting effects on health trajectories [11]. Breastfeeding, for instance, delivers maternal microbes and bioactive compounds like human milk oligosaccharides (HMOs) that selectively promote the growth of beneficial bacteria such as Bifidobacterium infantis [11].
The Concept of Stability and Dysbiosis
A core property of a healthy microbiome is stability—the ability to maintain compositional and functional integrity despite external perturbations [103]. Research leveraging ecological modeling and statistical analysis has shown that a stable microbiome is more resilient to disturbances. Conversely, dysbiosis, a disruption of this stable state, has been linked to a wide range of disorders, from infectious diseases like recurrent Clostridioides difficile infection (rCDI) to autoimmune, metabolic, and neurological conditions [11] [1]. It is this link between dysbiosis and disease that provides the therapeutic rationale for microbiome-based interventions, which aim to restore a healthy, stable microbial ecosystem.
The Evolving Regulatory Framework for Microbiome-Based Biologics
The FDA regulates microbiome-based therapies as biologics, a category that presents unique challenges due to their living nature and complex composition. The regulatory framework is rapidly adapting to these challenges.
Categorization of Microbiome-Based Therapies
Microbiome-based therapies represent a broad spectrum of products, which can be viewed as a continuum based on their complexity and level of manipulation [104].
Table 1: Categorization of Microbiome-Based Therapies
| Therapy Category | Description | Key Characteristics | Examples |
|---|---|---|---|
| Microbiota Transplantation (MT) | Transfer of a minimally manipulated microbial community from a donor to a recipient [104]. | High complexity; donor-dependent; higher perceived risk of pathogen transmission. | Fecal Microbiota Transplantation (FMT). |
| Donor-Derived Microbiome-Based Medicinal Products | Consist of whole or highly complex ecosystems derived from human microbiome samples but undergo industrial manufacturing [104]. | More controlled than MT but still highly complex; starting material is a human microbiome sample. | REBYOTA (fecal microbiota), vaginal microbiota products in development. |
| Rationally Designed Ecosystem-Based Medicinal Products | Composed of dozens of microbial strains selected to form a controlled ecosystem; produced via co-fermentation [104]. | Produced from clonal cell banks (not directly from a donor); designed for specific functions. | Products containing consortia of dozens of strains. |
| Live Biotherapeutic Products (LBPs) | Contain a single strain or a defined mixture of strains, each fermented separately and then blended [104]. | High level of characterization; well-defined composition; produced from clonal cell banks. | VOWST (oral spores of firmicutes); other single-strain or defined mixture products. |
Recent FDA Actions and Policy Updates
The FDA has implemented several key policy changes and guidance documents specifically impacting microbiome-based biologics.
Streamlining Biosimilar Development: In 2025, the FDA announced new draft guidance to streamline the development of biosimilars—generic versions of complex biological drugs. This guidance proposes allowing companies to scale back on comparative clinical efficacy studies, relying instead on analytical testing to demonstrate similarity to an existing reference product. This change is projected to cut biosimilar development time in half and reduce costs by up to $100 million, thereby increasing market competition and lowering drug costs [105].
The "Plausible Mechanism" Pathway: The FDA has outlined a novel approval pathway for certain personalized therapies, particularly bespoke cell and gene therapies. To qualify, a product must meet several criteria, including targeting a disease with a known biologic cause, having a well-characterized natural history, and providing confirmation that the target was successfully engaged in at least one patient. Evidence of clinical improvement can use patients as their own controls. Post-approval, sponsors are required to collect real-world evidence (RWE) to confirm efficacy and monitor safety [106]. While not yet applied to microbiome therapies, this pathway represents a broader regulatory evolution toward flexibility for novel modalities.
Modernizing Fecal Microbiota Transplant (FMT) Policy: With two FDA-approved microbiome therapeutics now on the market (REBYOTA and VOWST), industry groups are urging the FDA to close the "IND loophole" that permits large-scale distribution of unapproved stool-based products under enforcement discretion. This highlights a shifting regulatory landscape where approved, standardized products are expected to supplant unregulated interventions, prioritizing patient safety and quality control [107].
Experimental and Methodological Considerations for Development
The successful development and regulatory approval of a microbiome-based biologic depend on rigorous and standardized experimental approaches.
Establishing Strain Transmission and Engraftment
A critical aspect of microbiome therapy research is tracking the transmission and engraftment of microbial strains. A conceptual framework termed "4 W" is recommended for designing robust studies [42]:
- What: The transmitted unit (e.g., microbial cells, spores, or metabolites).
- Where: The source and destination body sites.
- Who: The donor and recipient of the microbes.
- When: The timing of the transmission event (e.g., at birth, during intervention).
The most precise unit for tracking transmission is the "transmitted microbial strain" defined by metagenomic sequencing. This requires stringent controls for contamination, especially in low-biomass samples, through sterile sampling and spike-in quantitative approaches [42].
The following diagram illustrates the workflow for establishing strain transmission using the 4W framework.
Assessing Microbiome Stability and Community Dynamics
Evaluating the impact of an intervention on microbiome stability is crucial. A meta-analysis of 9 interventional studies encompassing 3,512 gut microbiome profiles demonstrated the utility of combining two methodological approaches [103]:
- Mathematical Modeling: Using tools like the compositional Lotka-Volterra method to model microbial community dynamics and derive ecological stability measures.
- Observational Statistical Analysis: Measuring observed microbiome changes from interventional studies.
The substantial correlation between these approaches validates their use in assessing a therapy's ability to induce a stable, healthy state in a patient's microbiome.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for Microbiome Therapy Research
| Item | Function/Application | Technical Notes |
|---|---|---|
| Shotgun Metagenomic Sequencing Kits | Provides comprehensive profiling of all genetic material in a sample, enabling strain-level tracking and functional gene analysis [42]. | Superior to 16S rRNA sequencing for tracking specific transmitted strains. |
| Gnotobiotic Mouse Models | Germ-free or defined-flora animals used to establish causal relationships between a microbial therapy and a host phenotype [1]. | Essential for validating mechanism of action (MoA) and safety. |
| Anaerobic Culture Systems | For the cultivation, propagation, and banking of obligate anaerobic bacteria, which dominate the gut microbiome. | Critical for manufacturing Live Biotherapeutic Products (LBPs). |
| Clonal Cell Banks | Master and working cell banks of well-characterized bacterial strains, ensuring batch-to-batch consistency for LBPs [104]. | A regulatory requirement for defined products like VOWST. |
| Spike-in Control Standards | Known quantities of exogenous microbes or DNA added to samples to control for technical variability and quantify absolute abundance [42]. | Mandatory for low-biomass microbiome studies (e.g., tissue, milk) to distinguish signal from contamination. |
| Multi-omics Integration Platforms | Tools for correlating metagenomic, metatranscriptomic, metabolomic, and metaproteomic data to understand functional changes. | Provides a systems-level view of therapy impact on host-microbe interactions. |
The regulatory pathway for microbiome-based biologics is maturing in lockstep with the scientific understanding of the human microbiome. The FDA's recent actions—from streamlining biosimilar development and proposing novel approval pathways to refining policies around FMT—signal a clear commitment to fostering innovation while ensuring patient safety. For researchers and drug developers, success hinges on a deep integration of core microbiome principles, such as anatomical distribution, early-life development, and ecological stability, with robust and methodologically sound R&D practices. By employing strain-tracking frameworks like the "4 W" model, utilizing essential research tools, and designing studies that adequately assess community dynamics and engraftment, the field is poised to unlock the full therapeutic potential of the microbiome for a wide range of human diseases.
Conclusion
The field of human microbiome research has matured from foundational mapping to a robust translational discipline with significant therapeutic potential. The synthesis of insights from anatomical distribution, developmental dynamics, and the core principle of relational stability provides a solid scientific foundation. Methodological advances have yielded a diverse clinical pipeline, moving beyond gastrointestinal diseases to oncology and metabolic disorders. However, challenges in defining and optimizing microbial resilience, standardizing manufacturing, and navigating regulatory pathways remain. The future of microbiome science lies in deepening our functional understanding, leveraging AI for personalized interventions, and validating these approaches through rigorous clinical trials. The convergence of academic research, biotechnological innovation, and strategic investment is poised to fully realize the promise of the microbiome as a target for next-generation therapeutics, ultimately integrating microbiome-based strategies into mainstream precision medicine.
References
- 1. A systematic framework for understanding the microbiome ... [https://www.nature.com/articles/s41392-024-01946-6]
- 2. The Spatial Atlas of Human Anatomy (SAHA): A Multimodal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224548/]
- 3. Global genetic diversity of human gut microbiome species ... [https://www.sciencedirect.com/science/article/pii/S0092867425004167]
- 4. Relational Stability: A New Strategy for Defining the Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12040776/]
- 5. From gut to gamete: how the microbiome influences fertility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465865/]
- 6. The future of gut health: 5 Breakthrough trends from ... [https://www.dsm-firmenich.com/en/businesses/health-nutrition-care/news/talking-nutrition/the-future-of-gut-health-5-breakthrough-trends-from-probiota-2025.html]
- 7. takeaways from the 2025 GMFH Summit [https://www.gutmicrobiotaforhealth.com/clinical-translation-of-microbiome-research-takeaways-from-the-2025-gmfh-summit/]
- 8. A comprehensive overview of microbiome data in the light ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10900530/]
- 9. A Survey of Statistical Methods for Microbiome Data Analysis [https://www.frontiersin.org/journals/applied-mathematics-and-statistics/articles/10.3389/fams.2022.884810/full]
- 10. Diversity, stability and resilience of the human gut microbiota [https://pmc.ncbi.nlm.nih.gov/articles/PMC3577372/]
- 11. The human microbiome in clinical translation: from bench to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479421/]
- 12. Tools for Analysis of the Microbiome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7598837/]
- 13. A core microbiome signature as an indicator of health [https://www.sciencedirect.com/science/article/pii/S0092867424010389]
- 14. The microbiome: composition and locations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8025711/]
- 15. Human microbiome [https://en.wikipedia.org/wiki/Human_microbiome]
- 16. Unlocking the healthy human microbiome: Redefining core ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11959916/]
- 17. Guild-based analysis for understanding gut microbiome in ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-021-00840-y]
- 18. New model defines essential gut microbiome components ... [https://middleeasthealth.com/medical-specialty-features/gut-health/new-model-defines-essential-gut-microbiome-components-for-human-health/]
- 19. Rutgers Researchers Help Redefine Core Microbiome ... [https://research.rutgers.edu/news/rutgers-researchers-help-redefine-core-microbiome-opening-new-chapter-precision-health]
- 20. Guild-based approach for mitigating information loss and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11364377/]
- 21. Mechanisms of microbiota modulation: Implications for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11081615/]
- 22. Microbiome Based Precision Medicine through Integrated ... [https://www.sciencedirect.com/science/article/abs/pii/S094450132500343X]
- 23. Advancing Gut Microbiome Research: The Shift from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12010094/]
- 24. AI unravels the hidden communication of gut microbes [https://www.sciencedaily.com/releases/2025/11/251109013246.htm]
- 25. Microbiome scientist uses AI to redefine the gut-brain axis ... [https://microbiology.oregonstate.edu/impact/2025/03/microbiome-scientist-uses-ai-to-redefine-the-gut-brain-axis-and-deep-sea-ecosystems]
- 26. Human Microbiome Research Report 2025: Market to Reach [https://www.globenewswire.com/news-release/2025/11/19/3190697/0/en/Human-Microbiome-Research-Report-2025-Market-to-Reach-1-52-Billion-by-2030-Rising-at-a-CAGR-of-16-28-Global-Trends-Opportunities-and-Forecast-2020-2030F.html]
- 27. Integrating metagenomics and metabolomics to study the ... [https://www.nature.com/articles/s41598-025-98973-2]
- 28. Quantifying the impact of workshops promoting microbiome ... [https://www.nature.com/articles/s41598-025-89991-1]
- 29. Data Standards [https://microbiomedata.org/data-standards/]
- 30. Microbiome-Driven Therapeutics: From Gut Health to ... [https://www.mdpi.com/2624-5647/7/1/7]
- 31. Live Biotherapeutic Products: Development, Investment, and ... [https://www.alacrita.com/whitepapers/live-biotherapeutic-products-development-challenges]
- 32. What's New and What's Next in Fecal Microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377394/]
- 33. The Future of Microbiome Therapeutics - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11802617/]
- 34. Design and application of synthetic human gut microbial ... [https://pubmed.ncbi.nlm.nih.gov/41239968/]
- 35. The Future of Microbiome Therapeutics | Drugs [https://link.springer.com/article/10.1007/s40265-024-02107-3]
- 36. Human Microbiome Market & Therapeutic Pipeline 2025 [https://www.strategicmarketresearch.com/blogs/human-microbiome-market-clinical-trials-pipeline]
- 37. Microbiome Therapeutics Market Outlook 2025–2034 [https://microbiomecongress.org/report/microbiome-therapeutics-market-outlook-20252034/]
- 38. Clostridioides difficile Infection Market Forecasts by ... [https://www.prnewswire.com/news-releases/clostridioides-difficile-infection-market-forecasts-by-delveinsight-signal-groundbreaking-growth-at-a-cagr-of-13-5-in-the-7mm-during-the-forecast-period-20252034-302543479.html]
- 39. Clostridium Difficile Infections Pipeline 2025 [https://www.barchart.com/story/news/35368139/clostridium-difficile-infections-pipeline-2025-latest-fda-approvals-clinical-trials-and-emerging-therapies-assessment-by-delveinsight-novartis-ag-astellas-pharma-eli-lilly-company-astrazeneca]
- 40. Acurx Announces New Data on its DNA pol IIIC Inhibitor ... [https://www.acurxpharma.com/news-media/press-releases/detail/120/acurx-announces-new-data-on-its-dna-pol-iiic-inhibitor]
- 41. Microbiome-guided precision medicine: Mechanistic ... [https://www.sciencedirect.com/science/article/pii/S3050632825000186]
- 42. A reconceptualized framework for human microbiome ... [https://www.nature.com/articles/s41467-025-61998-2]
- 43. Metabolic modelling reveals the aging-associated decline ... [https://www.nature.com/articles/s41564-025-01959-z]
- 44. Gut microbiome data underscores gaps in global representation [https://biologicalsciences.uchicago.edu/news/gut-microbiome-data-underscores-gaps-global-representation]
- 45. Analyzing human gut microbiome data from global populations [https://pubmed.ncbi.nlm.nih.gov/40483188/]
- 46. MicroLabVR: Interactive 3D Visualization of Simulated ... [https://arxiv.org/html/2508.21736v1]
- 47. Ferring Presents New Data Analyses for REBYOTA® (fecal ... [https://ferringusa.com/?press=ferring-presents-new-data-analyses-for-rebyota-fecal-microbiota-live-jslm-at-acg-2025]
- 48. Prevention of recurrent Clostridioides difficile infection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602906/]
- 49. Ferring Presents New Data Analyses for REBYOTA® [https://www.microbiometimes.com/ferring-presents-new-data-analyses-for-rebyota/]
- 50. Mechanism of Action, Engraftment Data & Manufacturing [https://www.vowsthcp.com/moa]
- 51. Vedanta Biosciences Announces Phase 2 Study of VE202 ... [https://www.vedantabio.com/press-release/vedanta-biosciences-announces-phase-2-study-of-ve202-in-ulcerative-colitis-did-not-meet-primary-endpoint/]
- 52. Dysbiosis: What It Is, Symptoms, Causes, Treatment & Diet [https://my.clevelandclinic.org/health/diseases/dysbiosis]
- 53. Current understanding of antibiotic-associated dysbiosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9969474/]
- 54. Gut Microbial Dysbiosis - One Health Institute [https://onehealth.colostate.edu/2022/02/03/gut-microbial-dysbiosis/]
- 55. Gut Microbiota Dysbiosis: Triggers, Consequences ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8954387/]
- 56. Antibiotic-Therapy-Induced Gut Dysbiosis Affecting Gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9959899/]
- 57. The Impact of Antibiotic Therapy on Intestinal Microbiota [https://pmc.ncbi.nlm.nih.gov/articles/PMC12024230/]
- 58. Antibiotic-induced gut microbiota dysbiosis has a functional ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-023-02932-8]
- 59. Dysbiosis: Your Microbiome Out of Balance [https://www.ummhealth.org/simply-well/dysbiosis-your-microbiome-out-of-balance]
- 60. Understanding dysbiosis and resilience in the human gut ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1559521/full]
- 61. Microbiome and well-being: a meta-analysis [https://www.nature.com/articles/s41522-025-00829-0]
- 62. Exploring the Microbiome Analysis and Visualization Landscape [https://pmc.ncbi.nlm.nih.gov/articles/PMC9580862/]
- 63. Understanding dysbiosis and resilience in the human gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11913848/]
- 64. Microbiota-Dependent Fiber Responses: A Proof-of- ... [https://www.sciencedirect.com/science/article/pii/S0022316625005401]
- 65. A comprehensive overview of the effects of probiotics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575349/]
- 66. Effects of probiotics on gut microbiota - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3539293/]
- 67. The Role of Prebiotics in Modulating Gut Microbiota [https://pubmed.ncbi.nlm.nih.gov/38732060/]
- 68. Probiotics and Synbiotics: Applications, Benefits, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11910042/]
- 69. Probiotics: mechanism of action, health benefits and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10470842/]
- 70. Recent advances in prebiotics: Classification, mechanisms, ... [https://www.sciencedirect.com/science/article/pii/S266683352500142X]
- 71. The role of probiotics, prebiotics, and synbiotics in ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2025.1561047/full]
- 72. Synbiotic-driven modulation of the gut microbiota and ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-03953-1]
- 73. The hallmarks of dietary intervention-resilient gut microbiome [https://www.nature.com/articles/s41522-022-00342-8]
- 74. The human microbiome in clinical translation: from bench ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1632435/full]
- 75. Microbiome Therapeutics Market Size [https://www.gminsights.com/industry-analysis/microbiome-therapeutics-market]
- 76. Human Microbiome Research Report 2025: Market ... [https://sg.finance.yahoo.com/news/human-microbiome-research-report-2025-093500315.html]
- 77. Microbiome Manufacturing Market Size 2025 to 2034 [https://www.precedenceresearch.com/microbiome-manufacturing-market]
- 78. Developing standards for the microbiome field - BioMed Central [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-020-00856-3]
- 79. Standardizing the approach to clinical-based human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245529/]
- 80. Microbiome to Medicine Initiative | ASM.org [https://asm.org/about-asm/asm-strategic-roadmap/asm-health/microbiome-to-medicine-initiative]
- 81. Ferring Presents New Real-World REBYOTA® (fecal ... [https://ferringusa.com/?press=ferring-presents-new-real-world-rebyota-fecal-microbiota-live-jslm-data-underscoring-effectiveness-and-significant-improvements-in-patient-quality-of-life]
- 82. Criteria for Distinguishing Effectiveness From Efficacy Trials in ... [https://www.ncbi.nlm.nih.gov/books/NBK44024/]
- 83. Efficacy of Fecal Microbiota Transplantation (FMT) Versus ... [https://pubmed.ncbi.nlm.nih.gov/40978956/]
- 84. Human Microbiome Market Industry Research 2025-2035 [https://finance.yahoo.com/news/human-microbiome-market-industry-research-081200143.html]
- 85. Human Microbiome Market Outlook 2025–2035 [https://microbiomecongress.org/report/human-microbiome-market-outlook-20252035/]
- 86. A complete guide to human microbiomes: Body niches ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2022.951403/full]
- 87. Human Microbiome Market Size, Share & Growth Report ... [https://www.researchnester.com/reports/human-microbiome-market/4062]
- 88. Global Human Microbiome Market Size & Industry Report ... [https://www.rootsanalysis.com/reports/human-microbiome-market/281.html]
- 89. Current understanding of the human microbiome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7043356/]
- 90. Dynamics and Stabilization of the Human Gut Microbiome ... [https://www.sciencedirect.com/science/article/pii/S1931312815001626]
- 91. Human Microbiome Market Size, Share, and Growth ... [https://www.prophecymarketinsights.com/market_insight/Global-Human-Microbiome-Market-By-3787]
- 92. Human Microbiome Market Size, Growth, Price [https://www.sphericalinsights.com/reports/human-microbiome-market]
- 93. Microbiome-based interventions to modulate gut ecology ... [https://www.nature.com/articles/s41385-022-00564-1]
- 94. Gut microbiome therapy: fecal microbiota transplantation vs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11469438/]
- 95. A reconceptualized framework for human microbiome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12354763/]
- 96. Microbiome-Targeted Therapies in Gastrointestinal Diseases [https://www.mdpi.com/2813-9054/70/3/36]
- 97. Rational Design of Live Biotherapeutic Products for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12247820/]
- 98. Emerging Trends in “Smart Probiotics†- PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5626839/]
- 99. Decoding the diagnostic and therapeutic potential of ... [https://www.nature.com/articles/s41467-024-52598-7]
- 100. AI-empowered human microbiome research [https://pubmed.ncbi.nlm.nih.gov/40983504/]
- 101. From big data and experimental models to clinical trials [https://www.sciencedirect.com/science/article/pii/S0092867425001072]
- 102. Article A spatially structured mathematical model of the gut ... [https://www.sciencedirect.com/science/article/pii/S2589004223015766]
- 103. Stability of human gut microbiome [https://www.sciencedirect.com/science/article/pii/S2001037023003057]
- 104. The regulatory framework for microbiome-based therapies [https://www.nature.com/articles/s41522-025-00683-0]
- 105. FDA to streamline approvals for generic biological drugs in ... [https://www.cnn.com/2025/10/29/health/fda-drug-costs-biosimilars]
- 106. FDA announces “plausible mechanism†approval pathway ... [https://www.hoganlovells.com/en/publications/fda-announces-plausible-mechanism-approval-pathway-for-certain-personalized-therapies-with-few-detai]
- 107. MTIG Statements [https://microbiometig.org/statements/]