The Gut Microbiome in Health and Disease: From Mechanistic Insights to Next-Generation Therapeutics
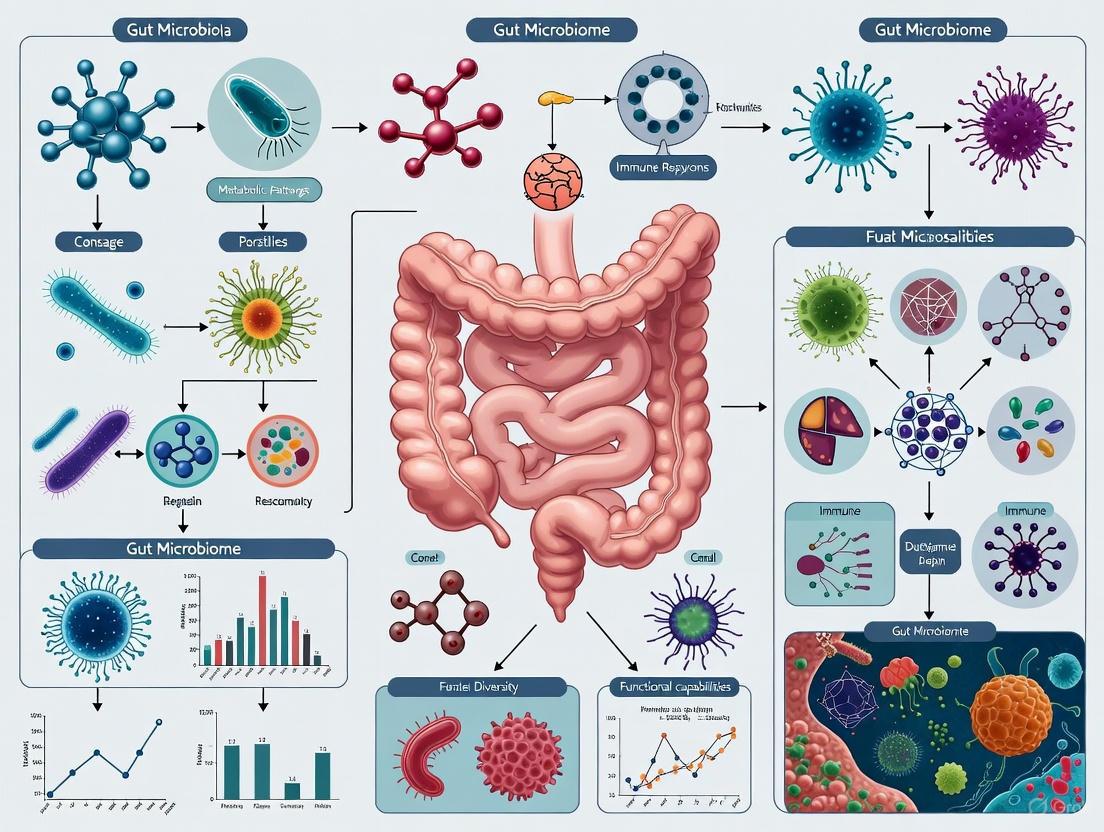
This article synthesizes current research on the gut microbiome's role in human health and disease, tailored for researchers and drug development professionals.
The Gut Microbiome in Health and Disease: From Mechanistic Insights to Next-Generation Therapeutics
Abstract
This article synthesizes current research on the gut microbiome's role in human health and disease, tailored for researchers and drug development professionals. It covers foundational concepts of microbiome composition and host interactions, explores advanced methodologies like multi-omics and gnotobiotic models for target identification, and analyzes challenges in translating research into therapies. The scope includes troubleshooting dysbiosis, optimizing microbial manipulation via FMT, next-generation probiotics, and phages, and validating approaches through comparative analysis of clinical trials and emerging trends in precision microbiome medicine.
Defining the Ecosystem: Core Concepts of the Gut Microbiome and Its Role in Human Physiology
In the rapidly advancing field of microbial research, the terms "microbiota" and "microbiome" are frequently used, yet they represent distinct concepts with critical differences that are essential for precise scientific communication. While both concepts revolve around microbial communities, their definitions encompass different scopes and components. Understanding this distinction is particularly crucial in gut health and disease association research, where the composition and function of microbial communities can significantly influence host physiology, disease states, and therapeutic responses [1] [2].
The confusion between these terms often stems from their historical usage and the overlapping nature of their referents. However, as research methodologies have advanced, particularly with the development of high-throughput sequencing technologies, the scientific community has developed more precise definitions that recognize the functional and genetic dimensions beyond mere taxonomic classification [1]. This semantic precision becomes increasingly important as we seek to understand the complex mechanisms through which microbial communities influence human health and disease.
Table 1: Core Definitions in Microbial Research
| Term | Definition | Key Components | Scope |
|---|---|---|---|
| Microbiota | The community of microorganisms themselves found in a specific environment [1] [2]. | Bacteria, archaea, fungi, viruses, and other microbes [3]. | Limited to the microorganisms themselves and their relative abundances. |
| Microbiome | The entire habitat, including microorganisms, their genetic elements, and environmental conditions [1] [2]. | Microbiota, their structural elements, metabolites, genetic material, and surrounding environmental conditions [1] [2]. | Encompasses the entire ecological system, including functional potential. |
The relationship between microbiota and microbiome is hierarchical and inclusive. The microbiome represents the broader ecological context, while the microbiota constitutes one component within this system. To extend the analogy presented by Allucent et al., if the microbiome is a house, the microbiota represents the people living there, while the furniture and other contents represent the genetic material, metabolites, and environmental factors that complete the system [1]. This distinction becomes methodologically significant when designing studies, as investigating the microbiota primarily involves taxonomic characterization, while studying the microbiome requires additional analysis of functional potential, genetic elements, and environmental interactions.
Key Components and Analytical Framework
Expanding the Vocabulary: Related Terminology
Beyond the core definitions of microbiota and microbiome, several related terms complete the analytical framework used in microbial research. These terms allow researchers to describe specific aspects of microbial communities and their study with greater precision, which is particularly valuable when communicating methodological approaches and findings in scientific literature.
Metagenome refers to the collection of genes and genomes from the microbiota in a given environment [1]. This concept represents the genetic complement of the microbiota and is identified through DNA extraction and metagenomic sequencing. The analysis of the metagenome helps researchers understand the functional capabilities of a microbial community, potentially explaining how specific microbiota function in health and disease states. Unlike the broader microbiome concept, the metagenome specifically focuses on the genetic material present, excluding the immediate environmental conditions and interactions that the microbiome encompasses.
The term microflora represents an older concept that has been largely superseded in rigorous scientific literature. Traditionally, this term referred primarily to microscopic plants, though its definition was later expanded to include various bacteria and microorganisms found in environments such as the human intestinal tract [1]. However, this term lacks the specificity required for modern medical and scientific literature, and its use is now generally confined to popular science rather than technical research communications.
Visualizing the Relationship Between Core Concepts
The following diagram illustrates the hierarchical relationship between the key terms discussed, clarifying how they interrelate within a research context:
The Research Context: Gut Microbiome in Health and Disease
In gut health and disease research, distinguishing between microbiota and microbiome has practical implications for study design and interpretation. Research focused on microbiota typically characterizes which microorganisms are present, their relative abundances, and how these compositions differ between health and disease states [2] [4]. For example, numerous studies have identified reduced microbial diversity in many diseases, with significant alterations in microbial communities detected across most conditions examined [4].
In contrast, research addressing the microbiome investigates not only which microbes are present but also their functional potential, genetic interactions, metabolite production, and relationship with the host environment [2]. This broader approach can reveal mechanisms behind observed associations, such as how microbial-derived metabolites influence host physiology or how environmental factors shape microbial community structure and function.
The gut microbiome functions as a crucial interface between host genetics, environmental exposures, and health outcomes. In healthy states, gut microbiota contribute to numerous physiological processes including nutrient extraction, metabolism, immune modulation, and protection against pathogens through colonization resistance [2]. However, when dysbiosis occurs—an imbalance in the microbial community—this can contribute to disease pathogenesis through multiple mechanisms including immune dysregulation, induction of chronic inflammation, and altered metabolic outputs [2].
Methodological Approaches in Microbiome Research
Experimental Workflow for Gut Microbiome Analysis
Investigating the gut microbiome requires a multi-step process that transforms biological samples into interpretable data. The following diagram outlines a generalized experimental workflow, from sample collection through data analysis:
Essential Research Reagents and Tools
Conducting robust microbiome research requires specific reagents and computational tools that enable precise characterization of microbial communities. The selection of these resources can significantly influence results, particularly due to methodological variations between studies [5]. The following table outlines key solutions used in typical gut microbiome studies:
Table 2: Research Reagent Solutions for Gut Microbiome Analysis
| Item | Function in Research | Technical Considerations |
|---|---|---|
| 16S rRNA Gene Primers | Amplify variable regions for bacterial identification and classification [5]. | Selection of hypervariable region (V1-V9) introduces bias; affects taxonomic resolution and community profile [5]. |
| DNA Extraction Kits | Lyse microbial cells and purify genetic material for downstream analysis [5]. | Lysis efficiency varies for different bacterial taxa; influences observed community structure [5]. |
| Sequencing Platforms (Illumina, Ion Torrent) | Determine nucleotide sequences of amplified genes or entire genomes [5]. | Different technologies (e.g., Illumina vs. Ion Torrent) impact read length, error profiles, and cost [5]. |
| Bioinformatics Pipelines (QIIME 2, mothur, MetaPhlAn4) | Process raw sequence data into taxonomic and functional profiles [5] [4]. | Choice of reference database and algorithm affects taxonomic assignment accuracy and resolution [4]. |
| Reference Databases (Greengenes, SILVA, GTDB) | Provide curated taxonomic frameworks for classifying sequence data [5]. | Database composition and curation influence which taxa can be identified and at what resolution. |
Methodological Considerations in Study Design
The methodological variability in microbiome research presents significant challenges for comparing results across studies. Differences in sample collection, DNA extraction methods, choice of 16S rRNA hypervariable regions, sequencing platforms, and bioinformatic processing can all substantially influence the resulting microbial community profiles [5]. For example, the selection of which hypervariable region to amplify introduces specific biases in the taxonomic composition observed, as different primer sets have varying amplification efficiencies across bacterial taxa [5].
Recognizing these methodological challenges, large-scale initiatives such as the Human Microbiome Project (HMP) by the National Institutes of Health have worked to establish standardized protocols and reference datasets [1]. These resources provide benchmark data that facilitate more consistent approaches across the research community. Furthermore, methods such as shotgun metagenomic sequencing—which sequences all DNA in a sample rather than just specific marker genes—can provide a more comprehensive view of the microbiome, including functional potential through analysis of microbial genes and pathways [4].
Applications in Disease Research and Therapeutic Development
Microbiome Signatures Across Diseases
Large-scale analyses of gut microbiome studies have revealed consistent patterns of alteration in various disease states. A 2024 meta-analysis of 6,314 fecal metagenomes from 36 case-control studies identified significant shifts in microbial diversity and composition across multiple diseases [4]. The research detected 277 disease-associated gut species, including numerous opportunistic pathogens enriched in patients and a concurrent depletion of beneficial microbes [4].
Table 3: Microbial Diversity Changes in Selected Diseases
| Disease Category | Specific Condition | Change in Species Richness | Change in Shannon Diversity | Reference |
|---|---|---|---|---|
| Inflammatory Bowel Disease | Crohn's Disease | Decrease (>10%) | Decrease (>10%) | [4] |
| Infectious Diseases | COVID-19 | Decrease (>10%) | Decrease (>10%) | [4] |
| Cardiometabolic | Hypertension | Decrease (>10%) | Decrease (>10%) | [4] |
| Neurological | Parkinson's Disease | Increase | Increase | [4] |
| Autoimmune | Systemic Lupus Erythematosus | Decrease (>10%) | Decrease (>10%) | [4] |
These disease-associated microbiome signatures have demonstrated potential diagnostic value. A random forest classifier based on these microbial signatures achieved high accuracy in distinguishing diseased individuals from controls (AUC = 0.776) and high-risk patients from controls (AUC = 0.825), maintaining performance in external validation cohorts [4]. This suggests that despite methodological variations between studies, consistent and generalizable microbiome patterns exist across populations and disease states.
Microbiota-Targeted Therapeutic Approaches
Understanding the distinction between microbiota and microbiome directly informs therapeutic development. While microbiota-focused interventions aim to modify the composition of microbial communities themselves, microbiome-targeted approaches consider the broader ecological context, including functional genes and environmental conditions.
Fecal Microbiota Transplantation (FMT) represents a primarily microbiota-focused intervention that transfers entire microbial communities from healthy donors to patients. This approach has demonstrated remarkable efficacy in treating recurrent Clostridioides difficile infections, effectively restoring a healthy microbial community structure [2].
More targeted approaches include:
- Probiotics: Specific live microorganisms that confer health benefits when administered in adequate amounts [6].
- Prebiotics: Substrates selectively utilized by host microorganisms that confer health benefits [6].
- Postbiotics: Preparations of inanimate microorganisms and/or their components that confer health benefits [6].
Recent research has also explored how medications beyond antibiotics affect the gut microbiome. A 2025 Stanford study investigated how 707 different drugs impact gut microbial communities, finding that 141 medications significantly altered microbiome composition [7]. The research revealed that competition for nutrients plays a significant role in determining which bacteria thrive or diminish following medication treatment, providing predictable ecological rules that could inform future drug design to minimize detrimental effects on gut microbial communities [7].
The distinction between microbiota as the community of microorganisms themselves and microbiome as the comprehensive habitat including genetic elements and environmental conditions is fundamental to rigorous research in the field. This precision in terminology becomes increasingly critical as we advance our understanding of how microbial communities influence human health and disease. For researchers investigating gut microbiome health and disease associations, recognizing this distinction informs study design, methodology selection, and data interpretation.
The expanding toolbox for microbiome research—from standardized analytical protocols to advanced computational models—enables increasingly sophisticated investigations into the mechanisms linking microbial communities to health outcomes. Furthermore, the identification of consistent microbial signatures across diverse diseases suggests potential pathways for developing microbiome-based diagnostics and therapeutics. As the field continues to evolve, maintaining clear conceptual distinctions between microbiota and microbiome will facilitate more precise communication and more effective translation of research findings into clinical applications.
The human gut microbiome undergoes a precise sequence of colonization and succession from birth through adulthood, a process fundamentally important to lifelong health. This developmental trajectory is characterized by predictable shifts in microbial diversity, composition, and functional capacity. The establishment of this microbial ecosystem within the first years of life is now understood to be a critical determinant in programming the host's immune, metabolic, and neurological systems [8] [9]. Disruptions during this period, termed the "critical window of development," can induce microbial dysbiosis, which is increasingly implicated in the pathogenesis of a wide array of diseases within the framework of the Developmental Origins of Health and Disease (DOHaD) [8]. This whitepaper delineates the stages of gut microbiome maturation, the factors influencing its assembly, the underlying molecular mechanisms, and the experimental methodologies essential for its investigation, providing a scientific foundation for therapeutic interventions targeting the gut microbiome.
The Phased Succession of the Gut Microbiome
The maturation of the gut microbiome is not a linear process but occurs through distinct, overlapping phases characterized by specific taxonomic and functional profiles. The plasticity of the microbiome is highest during the initial stages, gradually stabilizing into an adult-like state.
Developmental Stages and Taxonomic Shifts
The progression from infancy to early childhood marks a period of rapid microbial evolution. The gut microbiome reaches a mature, stable composition resembling that of an adult around 2.5 to 3 years of age, though some studies suggest the process may extend further [10] [9]. This progression can be categorized into three primary stages:
- Developmental Stage (3–14 months): This phase is dominated by Bifidobacterium [10]. The gut microbiota of infants is initially composed of facultative anaerobes (e.g., Enterobacterales, Enterococci, Staphylococci), which consume oxygen and create an environment conducive for obligate anaerobes [11].
- Transitional Stage (15–30 months): Characterized by an increase in microbial diversity, this stage sees a rise in Proteobacteria and Bacteroidetes, coinciding with the introduction of solid foods [10].
- Stability Stage (≥31 months): The microbiome stabilizes with Firmicutes becoming the predominant phylum, and the community structure begins to resemble that of an adult [10].
The table below summarizes the relative abundance of major bacterial phyla and genera during key developmental periods, synthesized from systematic reviews and cohort studies [12] [10] [9].
Table 1: Taxonomic Shifts in the Developing Gut Microbiome
| Life Stage | Dominant Phyla (Relative Abundance) | Dominant Genera | Key Characteristics |
|---|---|---|---|
| Infancy (0-12 months) | Firmicutes, Bacteroidetes, Actinobacteria, Proteobacteria | Bifidobacterium, Bacteroides, Escherichia, Lactobacillus, Staphylococcus | Low diversity, high volatility; strongly influenced by diet (breastmilk vs. formula) and delivery mode. |
| Preadolescence (2-12 years) | Firmicutes (~51%), Bacteroidetes (~36%), others | Bacteroides (~16%), Prevotella (~9%), Faecalibacterium (~8%), Bifidobacterium (~5%) [12] | Achieves adult-like diversity and composition; influenced by geography and diet. |
| Adulthood | Firmicutes, Bacteroidetes | Faecalibacterium, Bacteroides, Prevotella, Ruminococcus | High diversity and stability; core microbiome established. |
| Old Age / Longevity | Firmicutes, Bacteroidetes | ↑ Akkermansia; ↓ Faecalibacterium, Bacteroidaceae, Lachnospiraceae [13] | Increased alpha diversity; distinct beta diversity from younger adults; potential inflammatory status. |
The Concept of the "Critical Window"
The first 1000 days of life—from conception to approximately two years of age—represent a critical window of development for the gut microbiome [10] [9]. During this period, the microbial ecosystem is highly plastic and susceptible to environmental influences. Once established, a significant portion (60-70%) of an individual's gut microbiome remains relatively constant throughout life [9]. This early-life microbiota is essential for the maturation of the immune system, and disruptions during this period can have long-lasting effects, predisposing individuals to various diseases such as asthma, allergies, obesity, and inflammatory bowel disease later in life [8] [14] [9]. This aligns with the DOHaD hypothesis, which posits that early-life environmental exposures can program an individual's risk for chronic diseases in adulthood [8].
Determinants of Microbial Assembly and Succession
The trajectory of gut microbiome colonization is shaped by a complex interplay of maternal, environmental, and medical factors. Understanding these determinants is crucial for identifying levers to manipulate the microbiome for therapeutic benefit.
Prenatal and Perinatal Factors
Contrary to the long-held belief of a sterile uterus, emerging evidence suggests that microbial exposure may begin in utero, with bacteria detected in the placenta, amniotic fluid, and meconium [11] [10]. However, the most significant microbial inoculation occurs at birth.
- Mode of Delivery: Vaginally delivered infants acquire microbes resembling their mother's vaginal microbiota (e.g., Lactobacillus, Prevotella). In contrast, cesarean-delivered infants are initially colonized by microbes from the maternal skin and hospital environment (e.g., Staphylococcus, Corynebacterium, Propionibacterium), and exhibit lower levels of Bifidobacterium and Bacteroides [10].
- Maternal Factors: The maternal gut, oral, and vaginal microbiota, which undergo changes during pregnancy, serve as primary sources for the infant's microbiome [8] [11]. Maternal diet, BMI, antibiotic use during pregnancy, and overall health status can significantly alter these microbial reservoirs, thereby influencing the infant's microbial inheritance [8] [10].
Postnatal Factors
Following birth, diet becomes the most influential factor driving microbial succession.
- Feeding Type: Breastfed infants have a gut microbiome dominated by Bifidobacterium and Lactobacillus, due to the presence of human milk oligosaccharides (HMOs) that selectively promote their growth. Formula-fed infants, meanwhile, exhibit a more diverse microbiome with higher levels of Bacteroides, Clostridia, Staphylococci, and Enterococci [10].
- Antibiotic Exposure: Antibiotic use, particularly intrapartum antibiotic prophylaxis (IAP), has a profound and sustained impact. A 2025 study found that IAP-exposed infants had a significantly lower relative abundance of Bifidobacterium longum at one month of age, an effect that persisted at one year. This was coupled with a pro-inflammatory T-helper cell profile [15]. Beyond antibiotics, other common medications can also unsettle the gut microbiome by triggering nutrient competition among gut bacteria [7].
- Introduction of Solid Foods: The weaning process catalyzes a major shift in the gut microbiome, driving an increase in diversity and a transition toward an adult-like profile dominated by Firmicutes and Bacteroidetes [10].
Table 2: Impact of Early-Life Factors on Gut Microbiome Composition
| Factor | Impact on Microbial Diversity | Impact on Key Taxa | Associated Long-Term Health Risks |
|---|---|---|---|
| Cesarean Section | Reduced initial diversity | ↑ Staphylococcus, Corynebacterium; ↓ Bifidobacterium, Bacteroides [10] | Increased risk of asthma, allergies, and obesity [8] [9] |
| Formula Feeding | Alters trajectory, often increases diversity early on | ↑ Bacteroides, Clostridia, Staphylococci; ↓ Bifidobacterium [10] | Modulated risk of atopic diseases and obesity |
| Antibiotic Exposure | Can reduce diversity, with effects lasting years | ↓ Bifidobacterium, Bacteroides; ↑ Proteobacteria [15] [8] | Asthma, eczema, allergic diseases, obesity [15] [8] |
| Maternal Obesity | Alters inherited microbiota | ↑ Bacteroides, Staphylococcus; ↓ Bifidobacterium [8] | Predisposition to obesity and metabolic disorders [8] |
Molecular Mechanisms and Host-Microbe Interactions
The developing gut microbiome exerts its long-term effects on host health through complex molecular crosstalk, primarily mediated by microbial metabolites and immune system education.
Key Signaling Pathways and Metabolites
- Short-Chain Fatty Acids (SCFAs): Produced by bacterial fermentation of dietary fiber, SCFAs (acetate, propionate, butyrate) are crucial for gut health. They serve as energy sources for colonocytes, strengthen the gut epithelial barrier, and exert potent immunomodulatory effects. Butyrate, for instance, promotes the differentiation of regulatory T cells (Tregs), which are essential for maintaining immune tolerance and preventing aberrant inflammation [12] [9]. SCFAs signal through G-protein-coupled receptors (GPCRs) like GPR41, GPR43, and GPR109a, which are expressed on various immune and epithelial cells [9].
- Gut-Brain Axis Communication: The gut microbiome bidirectionally communicates with the brain through the vagus nerve, the production of neurotransmitters (e.g., GABA, serotonin), and microbial metabolites like SCFAs [9]. This axis is critical for neurodevelopment, and dysbiosis in early life has been linked to neurodevelopmental disorders [9].
- T-helper Cell Balance: The gut microbiome plays a critical role in educating the immune system and balancing T-helper cell populations. As demonstrated in the IAP study, microbial disruption can lead to a pro-inflammatory state characterized by higher levels of IL-17A, RORγt, and TGF-β, indicative of a Th17-skewed response [15]. This highlights the microbiome's role in regulating the Treg/Th17 balance, which is crucial for immune homeostasis [15].
The following diagram illustrates the primary mechanisms by which the early-life gut microbiome communicates with and influences distant organ systems.
Experimental Models and Methodologies
Research into the developing gut microbiome relies on a suite of sophisticated technologies for profiling microbial communities and modeling their interactions with the host.
Core Profiling Technologies
- 16S rRNA Gene Sequencing: This is the most widely used method for profiling microbial community composition. It involves amplifying and sequencing hypervariable regions of the bacterial 16S rRNA gene. The choice of hypervariable region (e.g., V3-V4, V4) can influence the taxonomic resolution and results, making standardization important for cross-study comparisons [15] [12].
- Shotgun Metagenomics: This technique sequences all the genetic material in a sample, providing not only taxonomic information at a higher resolution than 16S sequencing but also insights into the functional potential of the microbial community [13].
- Metabolomics: Liquid chromatography coupled with mass spectrometry (LC-MS) is used to profile the metabolome, including microbial metabolites like SCFAs, bile acids, and neurotransmitters. This provides a direct readout of microbial functional output [13].
The typical workflow for a microbiome study, from sample collection to data interpretation, is outlined below.
The Scientist's Toolkit: Key Reagents and Technologies
Table 3: Essential Research Reagents and Solutions for Gut Microbiome Studies
| Item | Function / Application | Example Protocols / Kits |
|---|---|---|
| DNA Extraction Kits | Isolation of high-quality microbial DNA from complex stool samples for downstream sequencing. | DNeasy PowerSoil Kit (Qiagen) [15] |
| 16S rRNA Primers | Amplification of specific hypervariable regions for taxonomic profiling. | Primers for V3/V4 regions [15] |
| MiSeq Reagent Kit | Sequencing of amplicon libraries on the Illumina platform. | MiSeq Reagent Kit V3 (600 cycles) [15] |
| Flow Cytometry Antibodies | Immunophenotyping of host immune cells to correlate with microbial changes. | Antibodies for CD3, CD4, CD25, Foxp3, IL-17A, RORγt [15] |
| CapScan Device | A novel, ingestible capsule for sampling the microbiome of the small intestine, a previously difficult-to-access site [16]. | CapScan capsule [16] |
| Live Biotherapeutic Products (LBPs) | Defined bacterial consortia investigated as therapeutics to restore a healthy gut microbiome. | EBX-102-02 (for IBS-C), purified Firmicutes spores (for rCDI) [16] |
| tetranor-PGDM | tetranor-PGDM, CAS:70803-91-7, MF:C16H24O7, MW:328.36 g/mol | Chemical Reagent |
| Toltrazuril-d3 | Toltrazuril-d3, CAS:1353867-75-0, MF:C18H14F3N3O4S, MW:428.4 g/mol | Chemical Reagent |
Experimental Models for Mechanistic Insight
- Gnotobiotic Models: Germ-free mice, colonized with defined human microbial communities, are a gold-standard model for establishing causal relationships between the microbiome and host phenotype. They are indispensable for studying the functional impact of specific microbes or communities.
- In Vitro Culturing Systems: Advanced culturing of complex microbial communities derived from human fecal samples allows for systematic testing of pharmaceutical compounds or dietary interventions. A Stanford study used this approach to test 707 different drugs, finding that 141 altered the microbiome, primarily through nutrient competition [7].
- Longitudinal Cohort Studies: Human studies that track infants and children over time are critical for defining the normal trajectory of microbiome development and understanding how perturbations correlate with health outcomes. These studies require careful collection of metadata, including diet, medication use, and health records [15] [8].
The development of the gut microbiome from infancy to adulthood is a meticulously orchestrated process of colonization and succession, pivotal for setting the trajectory of lifelong health. The "critical window" of early life represents a period of unparalleled plasticity, during which factors like delivery mode, diet, and antibiotic exposure can permanently shape the microbial ecosystem and, consequently, the host's immune and metabolic programming. Disruptions to this process are mechanistically linked to disease via altered microbial metabolites, immune dysregulation, and cross-talk with distant organs. Future research and therapeutic development will rely on sophisticated multi-omics approaches, advanced culturing technologies, and defined live biotherapeutics to precisely diagnose and correct dysbiosis, ultimately harnessing the microbiome to improve human health from its earliest foundations.
The human gastrointestinal (GI) tract hosts one of the most complex microbial ecosystems, with its composition and function critical to host health. A key characteristic of this system is its profound spatial heterogeneity; the microbial communities are not uniform but vary significantly across different segments [17]. Understanding this spatial distribution is fundamental to elucidating the gut microbiome's role in health and disease. While many studies rely on fecal samples as a proxy for the gut microbiota, this approach overlooks the compartmentalized nature of microbial communities along the GI tract [17]. This review synthesizes current knowledge on the spatial variation of the gut microbiota, detailing the distinct microbial compositions in different GI segments, the advanced methodologies used to study them, and the implications of this spatial organization for host physiology and disease pathogenesis.
Spatial Heterogeneity of the Gut Microbiome
The GI tract presents a series of diverse microenvironments, varying in pH, oxygen tension, nutrient availability, and host immune factors, which select for distinct microbial assemblages. A foundational study in wild house mice examining ten segments of the GI tract—oral cavity, esophagus, stomach, duodenum, ileum, proximal cecum, distal cecum, colon, rectum, and feces—clearly demonstrated this spatial stratification [17].
Upper vs. Lower GI Tract Dichotomy
The most pronounced difference in microbial composition exists between the upper and lower GI tract.
- Upper GI Tract: The stomach and small intestine are characterized by lower microbial diversity and a greater relative abundance of facultative anaerobes, which can tolerate the more oxygen-rich and dynamic environment [17].
- Lower GI Tract: The cecum and colon are characterized by a greater relative abundance of strict anaerobic bacteria (e.g., from the phyla Bacteroidetes and Firmicutes) and significantly higher microbial diversity. This is the primary site for fermentation of dietary fibers into short-chain fatty acids (SCFAs) like butyrate, acetate, and propionate [17].
Table 1: Microbial Composition and Function Across Major GI Segments
| GI Segment | Dominant Phyla/Genera | Environmental Conditions | Key Microbial Functions |
|---|---|---|---|
| Stomach & Small Intestine | Lower diversity; Facultative anaerobes (e.g., Lactobacillus, Enterobacteriaceae) | Lower pH (stomach), rapid transit, higher oxygen | Nutrient absorption; initial digestion; immune sampling |
| Cecum & Colon | High diversity; Strict anaerobes (e.g., Bacteroidetes, Firmicutes, Faecalibacterium, Akkermansia) | Neutral pH, slow transit, anaerobic | Fermentation of dietary fiber; production of SCFAs; vitamin synthesis; immune regulation |
Beyond this broad dichotomy, significant variation exists within the lower tract. For instance, the proximal and distal halves of the cecum can harbor different microbial communities [17]. Furthermore, microbial communities derived from fecal samples, while similar to those in the lower GI tract, are not identical to colonic communities, highlighting the need for caution when extrapolating from fecal data alone [17].
Individual Host Factors
While gut segment is a primary driver of microbial composition, variation among individual hosts also plays a significant role. Even when considering the upper and lower GI tracts separately, microbial composition has been shown to associate with individual mice, suggesting that diet, host genotype, and habitat contribute to the spatial structuring of these communities [17].
Advanced Methodologies for Spatial Microbiome Analysis
Traditional 16S rRNA gene amplicon sequencing, as used in the mouse study above, has laid the groundwork for understanding microbial composition [17]. However, emerging "enhanced metagenomic strategies" are providing unprecedented resolution.
Next-Generation Sequencing and Multi-Omics
- Long-Read Sequencing: Technologies like Oxford Nanopore and PacBio resolve repetitive genomic elements and structural variations, enabling complete genome assembly from complex samples and improving the study of mobile genetic elements like plasmids [18].
- Single-Cell Metagenomics: This approach bypasses cultivation biases by isolating individual microbial cells, revealing the genomic blueprints of uncultured taxa and providing insights into functional heterogeneity [18].
- Multi-Omics Integration: Combining metagenomics with metatranscriptomics, metaproteomics, and metabolomics shifts the focus from "who is there" to "what they are doing," mapping niche-specific activities and host-microbe communication [18].
Computational and Modeling Tools
- AI-Guided Annotation: Machine learning and advanced bioinformatics are used to annotate microbial genes and pathways with high accuracy, reducing functional inference biases [18].
- Genome-Scale Models (ME-models): Innovative tools like coralME rapidly create detailed genome-scale computer models that link a microbe's genome to its phenotype. These models can simulate how gut bacteria respond to different nutrients and predict the formation of microbial metabolites, providing a mechanistic basis for understanding behavior in complex environments like the gut of patients with Inflammatory Bowel Disease (IBD) [19].
Table 2: Key Research Reagent Solutions for Gut Microbiome Spatial Analysis
| Research Reagent / Tool | Function and Application |
|---|---|
| 16S rRNA Gene Primers (e.g., 515F/806R) | Amplify the V4 region of the 16S rRNA gene for taxonomic profiling of microbial communities [17]. |
| QIAamp DNA Stool Mini Kit | DNA extraction from complex gut content and mucosal samples, often with mechanical lysis enhancement [17]. |
| Greengenes Database | Reference database for clustering 16S rRNA sequences into Operational Taxonomic Units (OTUs) and assigning taxonomy [17]. |
| PBS Buffer | Used for rinsing and homogenizing gut tissue samples to maintain osmotic balance and preserve microbial integrity during collection. |
| Zirconia/Silica Beads | Used in mechanical lysis via bead-beating to effectively break open hardy microbial cell walls for DNA extraction [17]. |
| coralME Software Tool | Generates Metabolism and Expression models (ME-models) from genomic data to predict microbial metabolic interactions and phenotypes [19]. |
Implications for Host Health and Disease
The spatial distribution of gut microbiota is not merely an ecological curiosity; it has direct consequences for host health through multiple axes of communication.
Signaling Pathways and Host-Microbe Interactions
Spatially specific microbial activities influence host physiology via key signaling pathways. Diagrammatically, the gut-liver axis communication can be summarized as follows:
Diagram 1: Gut-Liver Axis Pathways
Gut-Liver Axis: Altered microbial composition in the colon, such as an enrichment of Clostridium scindens, increases the production of secondary bile acids (e.g., deoxycholic acid). These disrupt the Farnesoid X receptor (FXR) signaling in the liver, impairing lipid/glucose metabolism and promoting steatosis. Concurrently, gut-derived endotoxins (e.g., LPS) can translocate via the portal circulation, activating inflammatory pathways and contributing to liver injury [18].
Gut-Brain Axis: This bidirectional communication network is mediated by microbial metabolites. Dysbiosis in the lower GI tract can reduce the production of SCFAs and serotonin precursors, while increasing pro-inflammatory mediators like TMAO. These shifts can exacerbate neuroinflammation, compromise blood-brain barrier integrity, and are implicated in conditions like anxiety, depression, and Alzheimer's disease [18].
Dysbiosis and Disease
Spatial dysbiosis—the disruption of microbial communities in their specific niches—is linked to disease. For example:
- Inflammatory Bowel Disease (IBD): Blooms of Enterobacteriaceae in the ileal or colonic mucosa are associated with elevated IL-17 production and mucosal damage [18]. Models from coralME reveal that IBD patients exhibit shifts in gut chemistry, including elevated pH and decreased SCFA production [19].
- Colorectal Cancer (CRC): The mucosal-associated pathobiont Bacteroides fragilis can promote oncogenic Wnt/β-catenin signaling through polysaccharide A, driving disease progression [18].
The experimental workflow for establishing these spatial-disease relationships often follows a structured path, from sample collection to therapeutic insight:
Diagram 2: Spatial Dysbiosis Research Workflow
The microbial composition of the gastrointestinal tract is not homogenous but is instead a highly organized and spatially structured ecosystem. The stark contrast between the upper and lower GI tract, coupled with finer-scale variations within segments and the influence of individual host factors, underscores the complexity of this community. Advanced methodologies, from long-read sequencing to mechanistic computational models, are illuminating the functional consequences of this spatial distribution. Understanding how specific microbes in specific locations influence host pathways via axes like the gut-liver and gut-brain axes is crucial for moving from associative observations to causative mechanisms. This refined spatial perspective is paving the way for a new era of personalized microbiome-based diagnostics and therapies, allowing for targeted interventions that consider the ecological nuances of the human gut.
The human gut microbiome functions as a virtual endocrine organ, producing a diverse array of metabolites that profoundly influence host physiology and disease susceptibility. These microbial metabolites represent critical interfaces in host-microbiome crosstalk, mediating effects far beyond the gastrointestinal tract. Within the vast repertoire of microbial chemicals, short-chain fatty acids (SCFAs), bile acids (BAs), and vitamins have emerged as particularly crucial functional mediators in health and disease. This review synthesizes current understanding of these key microbial metabolites, framing their roles within the broader context of gut microbiome-health-disease associations. For researchers and drug development professionals, understanding the mechanistic basis of these metabolites provides unprecedented opportunities for therapeutic intervention. The intricate metabolic interplay between host and microbiota not only maintains homeostasis but, when disrupted, contributes to pathogenesis across multiple organ systems, including cardiovascular, neurological, and hepatic diseases [20] [21]. This whitepaper provides a technical overview of these metabolites, their quantitative profiles, experimental approaches for their study, and their integration into current drug discovery paradigms.
Short-Chain Fatty Acids (SCFAs): Microbial Fermentation Products
Production, Metabolism, and Physiological Concentrations
Short-chain fatty acids (SCFAs), primarily acetate (C2), propionate (C3), and butyrate (C4), are the main metabolites produced from microbial fermentation of dietary fibers and resistant starch in the colon. They are present in an approximate molar ratio of 60:20:20, with approximately 500-600 mmol produced daily in the human gut [22]. Their production is influenced by multiple factors including substrate source, gut microbiota composition, colonic pH, and transit time [23]. Following production, SCFAs are absorbed by colonocytes via monocarboxylate transporters (MCTs and SMCTs). Butyrate serves as a primary energy source for colonocytes, while acetate and propionate that escape hepatic metabolism enter systemic circulation to exert peripheral effects [23] [22].
Table 1: Major SCFAs: Sources, Concentrations, and Primary Functions
| SCFA Type | Primary Producing Bacteria | Typical Fecal Concentration (μM/g) | Major Physiological Functions |
|---|---|---|---|
| Acetate | Numerous commensals | Most abundant | Substrate for cholesterol synthesis; influences appetite regulation |
| Propionate | Bacteroidetes spp. | ~20-80 μM/g | Gluconeogenesis precursor; regulates satiety and immune function |
| Butyrate | Firmicutes (e.g., Faecalibacterium prausnitzii) | ~20-50 μM/g | Primary colonocyte energy source; anti-inflammatory; maintains gut barrier |
Mechanisms of Action and Host Benefits
SCFAs influence host physiology through multiple mechanisms, primarily via G-protein-coupled receptor (GPCR) activation (e.g., GPR41, GPR43, GPR109a) and histone deacetylase (HDAC) inhibition [23] [22]. The health benefits of SCFAs are extensive and well-documented:
- Immunoregulation: SCFAs promote regulatory T-cell (Treg) differentiation and IL-10 production, while inhibiting pro-inflammatory cytokines [23]. Butyrate particularly enhances IL-22 production by CD4+ T cells and innate lymphoid cells, strengthening mucosal immunity [23].
- Anti-inflammatory Effects: SCFAs reduce NF-κB activation and promote Nrf2 nuclear translocation, mitigating oxidative stress and inflammation [23].
- Metabolic Benefits: SCFAs protect against diet-induced obesity and improve insulin sensitivity. Propionate represses triglyceride accumulation via PPARα-responsive genes [23].
- Neuroprotective Activity: Cross-sectional studies show depressed individuals have lower levels of acetate and propionate [23]. SCFAs modulate microglial activation and blood-brain barrier integrity [22] [21].
- Cardiovascular Protection: Butyrate deficiency impairs baroreceptor sensitivity and blood pressure regulation [21]. SCFAs also counteract the atherosclerosis-promoting effects of TMAO [21].
Experimental Approaches for SCFA Research
Table 2: Standard Experimental Models for SCFA Research
| Methodology | Application | Key Parameters Measured | Considerations |
|---|---|---|---|
| In vitro fermentation models (e.g., SIMGI) | Simulating colonic SCFA production | SCFA concentration (GC-MS/LC-MS), bacterial abundance | Controlled pH, sequential vessels mimicking different gut regions [24] |
| In vivo models (germ-free, gnotobiotic mice) | Mechanistic studies of SCFA functions | Tissue SCFA levels, receptor expression, inflammatory markers, metabolic phenotypes | 150-200 mM SCFA supplementation in drinking water; 1-6 mmol/kg intraperitoneal injection [23] |
| Cell culture systems (e.g., 3T3-L1, THP-1, primary colonoids) | Molecular pathway analysis | Gene expression (qPCR/RNA-seq), protein quantification (Western blot), histone acetylation status | SCFA concentrations typically 0.1-10 mM; HDAC inhibition assays [23] |
Figure 1: SCFA Signaling Pathways and Physiological Effects
Bile Acids: Microbial Transformers of Key Signaling Molecules
The Bidirectional Relationship Between Bile Acids and Gut Microbiota
Bile acids represent a paradigm of host-microbiome co-metabolism. The liver synthesizes primary bile acids (cholic acid [CA] and chenodeoxycholic acid [CDCA]), which are conjugated to glycine or taurine before biliary secretion [25]. Upon entry into the intestinal lumen, gut microbiota extensively modify these bile acids through two principal enzymatic activities: bile salt hydrolase (BSH) and bile acid 7α-dehydroxylation [25]. BSH enzymes, widely distributed across gut bacteria, deconjugate bile acids, while the 7α-dehydroxylation pathway, restricted to specific Clostridium species (clusters XVIa and XI), converts primary bile acids into secondary bile acids including deoxycholic acid (DCA) and lithocholic acid (LCA) [25] [26]. The size and composition of the bile acid pool are thus regulated through a dynamic interplay between host synthesis and microbial metabolism.
Bile Acids as Regulatory Molecules and Disease Mediators
Bile acids function beyond their classical roles in lipid digestion, acting as important signaling molecules through activation of specific receptors, particularly the farnesoid X receptor (FXR) and G protein-coupled bile acid receptor 1 (TGR5) [25] [26]. The composition of the bile acid pool significantly influences gut microbial community structure, with more hydrophobic bile acids like DCA exhibiting potent antimicrobial effects [25]. Perturbations in bile acid metabolism have significant pathological consequences:
- Cirrhosis: Progression of cirrhosis is associated with decreased bile acid delivery to the intestine, resulting in dysbiosis characterized by reduced populations of bile acid-transforming bacteria (Blautia, Ruminococcaceae) and expansion of potential pathogens (Enterobacteriaceae) [25].
- Liver Cancer: Secondary bile acids, particularly DCA, promote hepatocellular carcinoma (HCC) through induction of senescence-associated secretory phenotype (SASP) in hepatic stellate cells [25].
- Metabolic Disease: Bile acid signaling through FXR and TGR5 regulates glucose, lipid, and energy metabolism, making these pathways attractive therapeutic targets [26].
Methodologies for Bile Acid Research
Table 3: Experimental Approaches for Bile Acid-Microbiome Studies
| Technique | Application | Key Readouts |
|---|---|---|
| In vitro biotransformation assays | Screening bacterial BA metabolism | BA profile changes (LC-MS/MS), enzyme activity (BSH, 7α-dehydroxylase) |
| Gnotobiotic mouse models | Establishing causal relationships | BA pool size/composition, host gene expression, metabolic phenotypes |
| Targeted bile acidomics | Quantitative BA profiling | >50 individual BA species in feces, serum, liver tissue |
| FXR/TGR5 reporter assays | BA signaling potential | Receptor activation, downstream gene targets (e.g., FGF19, GLPs) |
Figure 2: Bile Acid Metabolism and Host Interactions
Vitamins: Microbial Synthesis and Modification
Gut Microbiota as a Source of Essential Vitamins
The gut microbiota contributes significantly to the host's vitamin status, particularly for fat-soluble vitamins (A, D, E, K) and certain water-soluble vitamins (B group, K) [27]. This relationship is bidirectional: the microbiota synthesizes vitamins and transforms dietary vitamins, while vitamins simultaneously shape the microbial community structure and function. For instance, specific gut bacteria produce vitamin K and multiple B vitamins, while vitamin D receptor (VDR) signaling influences microbial composition [27]. The metabolic interplay between vitamins and gut microbiota affects host physiology through multiple mechanisms, including immune modulation, maintenance of epithelial barrier integrity, and regulation of metabolic homeostasis.
Implications for Host Physiology and Disease
Vitamin-microbiota interactions have profound implications for human health:
- Immune Function: Vitamin A metabolites (retinoic acid) and vitamin D directly modulate immune cell differentiation and function, influencing susceptibility to inflammatory bowel disease (IBD) and other immune-mediated conditions [27].
- Barrier Integrity: Vitamins A, D, and E contribute to maintaining intestinal epithelial barrier function, preventing translocation of bacterial products and subsequent systemic inflammation [27].
- Neurological Health: Gut microbiota-derived B vitamins influence neurological function through their roles as cofactors in neurotransmitter synthesis and myelin formation [27].
Methodological Toolkit for Metabolite Research
Research Reagent Solutions
Table 4: Essential Research Reagents for Microbial Metabolite Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Chemical Inhibitors | GPR41/43 antagonists, FXR antagonists (guggulsterone), TGR5 antagonists | Pathway blockade to establish mechanistic causality |
| Recombinant Enzymes | Purified BSH, 7α-dehydroxylase complexes | In vitro characterization of microbial BA transformations |
| Synthetic Metabolites | Stable isotope-labeled SCFAs (13C-acetate), deuterated bile acids | Metabolic fate tracing, quantitative MS standards |
| Receptor Reporter Systems | FXR-Luc, TGR5-Luc reporter cell lines | High-throughput screening of metabolite receptor activation |
| Specialized Growth Media | Vitamin-free, fiber-defined, BA-defined media | Controlled manipulation of microbial metabolic output |
| Chlorotoluron-d6 | Chlorotoluron-d6, CAS:1219803-48-1, MF:C10H13ClN2O, MW:218.71 g/mol | Chemical Reagent |
| Vitamin D2-d6 | Vitamin D2-d6 Stable Isotope | Vitamin D2-d6 (Ergocalciferol-d6) is a deuterated tracer for metabolic, pharmacokinetic, and nutritional research. For Research Use Only. Not for human use. |
Advanced Computational and Experimental Models
The field is rapidly advancing with innovative tools that enable more predictive modeling of metabolite-host interactions:
- coralME: A recently developed computational tool that rapidly generates genome-scale models of microbial metabolism from multi-omics data, predicting how microbes respond to nutrients and produce metabolites in health and disease [19].
- ME-models: These metabolism and expression models link microbial genomes to phenotypic outcomes, providing unprecedented resolution into microbial community behavior [19].
- Humanized mouse models: Germ-free mice transplanted with human microbiota provide physiologically relevant systems for studying metabolite-host interactions in vivo [24].
- Complex in vitro systems: Advanced gut simulators (e.g., SIMGI, TIM) replicate colonic conditions for studying metabolite production and absorption under controlled conditions [24].
Implications for Drug Discovery and Development
The growing understanding of microbial metabolites has profound implications for pharmaceutical development. First, the microbiome represents a significant source of interindividual variability in drug response, as microbial enzymes can directly metabolize drugs or modulate host metabolism [24]. For instance, microbial β-glucuronidases reactivate the chemotherapeutic irinotecan to its toxic form, causing dose-limiting diarrhea [24]. Second, microbial metabolites and their receptors represent promising novel therapeutic targets. Approaches include:
- Developing FXR and TGR5 agonists/antagonists to modulate metabolic diseases [26].
- Using SCFA receptor agonists to treat inflammatory and neurological conditions [23] [22].
- Engineering BSH inhibitors to manipulate bile acid pool composition for metabolic benefits [25] [26].
- Implementing dietary interventions that selectively modulate microbial metabolite production as adjuvant therapies [19] [21].
The pharmaceutical industry is increasingly integrating microbiome considerations into drug discovery pipelines, employing in silico databases like the Interactome of Microbiome-Derived Metabolites and Drugs (IMMD) to predict drug-microbiome interactions early in development [24]. Standardized tools and reference materials are needed to fully capture these complex interactions and improve the safety and efficacy of new chemical entities.
SCFAs, bile acids, and vitamins represent three fundamental classes of microbial metabolites that mediate host-microbiome communication with far-reaching effects on health and disease. For researchers and drug development professionals, understanding the production, transformation, and signaling mechanisms of these metabolites provides critical insights into pathophysiology and therapeutic opportunities. The continuing development of sophisticated experimental models, computational tools, and analytical technologies will further decipher the complex metabolic interplay between host and microbiota. Integration of this knowledge into drug discovery pipelines holds promise for developing novel therapeutics that target microbial metabolic pathways or harness beneficial metabolites for disease treatment. As our understanding of these functional cores deepens, we move closer to precision interventions that modulate specific microbial functions to restore and maintain human health.
Dysbiosis is defined as a disturbance in the homeostasis of the commensal microbial community, characterized by an imbalance in the composition and function of the microorganisms residing in a particular environment [28] [29]. This imbalance represents a critical transition from a beneficial symbiotic relationship between host and microbiota to a state associated with disease pathogenesis. In the symbiotic state, known as eubiosis, the microbial community maintains a balanced composition that supports numerous host physiological functions, including nutrient metabolism, barrier integrity, and immune regulation [30]. The disruption of this delicate equilibrium manifests through several recognizable patterns: loss of beneficial microorganisms, overgrowth of potentially harmful organisms, and reduction in overall microbial diversity [28] [31] [29]. While these types often coexist, they provide a framework for understanding how dysbiosis contributes to disease processes across multiple body sites, particularly in the gastrointestinal tract.
The human gut represents the most extensively studied microbiome, housing approximately 10¹ⴠbacterial cells encompassing over 1000 different bacterial species, with Firmicutes and Bacteroidetes constituting the dominant phyla in healthy individuals [28] [2]. This complex ecosystem engages in constant cross-talk with the host, creating a homeostatic balance that maintains gastrointestinal health and provides colonization resistance against pathogens [28] [2]. When this balance is disrupted, the protective functions of the microbiota are compromised, potentially leading to or exacerbating a wide range of diseases. Research has established associations between dysbiosis and inflammatory bowel disease (IBD), obesity, allergic disorders, type 1 diabetes mellitus, autism, and colorectal cancer in both human and animal models [28]. The transition from symbiosis to dysbiosis can be triggered by multiple factors, including host genetics, antibiotic use, dietary changes, infections, and environmental exposures [32] [29] [30].
Table 1: Types of Dysbiosis and Their Characteristics
| Type of Dysbiosis | Key Characteristics | Functional Consequences |
|---|---|---|
| Loss of Beneficial Organisms | Decrease in commensal bacteria diversity; Reduction in Faecalibacterium prausnitzii, Bifidobacterium spp., and Bacteroides [28] [29] | Reduced production of anti-inflammatory metabolites like butyrate; Impaired T-regulatory cell induction; Weakened gut barrier function [28] [29] |
| Expansion of Pathobionts | Increase in Enterobacteriaceae family (e.g., AIEC), Ruminococcus gnavus; Rise in sulphate-reducing bacteria [28] | Increased production of toxic metabolites (e.g., hydrogen sulfide); Triggering of pro-inflammatory responses; Epithelial barrier damage [28] |
| Loss of Microbial Diversity | Reduced overall species richness; Loss of obligate anaerobes with expansion of facultative anaerobes [28] [29] | Ecosystem instability; Reduced metabolic capacity; Diminished colonization resistance [28] [2] |
Quantifying Dysbiosis: Microbial Signatures in Disease
The identification of specific microbial signatures associated with disease states has been instrumental in understanding dysbiosis. Advanced sequencing technologies have enabled researchers to move beyond associations toward defining quantitative dysbiosis indices that can potentially serve as diagnostic tools or therapeutic targets.
In inflammatory bowel disease (IBD), dysbiosis demonstrates a characteristic pattern marked by a pronounced decrease in commensal bacteria diversity, particularly affecting the Firmicutes and Bacteroidetes phyla [28]. More specifically, the dysbiosis signature in Crohn's disease is characterized by five key bacterial species: an increase in Ruminococcus gnavus, accompanied by decreases in Faecalibacterium prausnitzii, Bifidobacterium adolescentis, Dialister invisus, and an unknown species from Clostridium cluster XIVa [28]. This signature exemplifies the multifaceted nature of dysbiosis, encompassing both the loss of beneficial taxa and the expansion of potentially detrimental ones. The functional implications are significant, as F. prausnitzii represents a major butyrate-producing bacteria in the intestines, and its reduction compromises energy supply to colonocytes and weakens the epithelial barrier [28].
The composition of a "healthy" microbiota varies substantially between individuals and is influenced by factors including age, genetics, and early life exposures [30] [2]. However, core principles of a healthy gut microbiota include high taxonomic diversity, stable core microbiota, and functional redundancy that ensures ecosystem resilience [2]. Quantitative assessments reveal that dysbiosis often involves measurable shifts in the relative abundances of key bacterial groups, which can be tracked through dysbiosis indices. Interestingly, research has shown that unaffected relatives of patients with Crohn's disease also exhibit altered intestinal microbiota compared to healthy controls, suggesting dysbiosis may precede clinical disease manifestation in genetically susceptible individuals [28].
Table 2: Quantitative Microbial Changes in Dysbiosis-Associated Conditions
| Condition | Increased Taxa | Decreased Taxa | Functional Metrics |
|---|---|---|---|
| Inflammatory Bowel Disease | Ruminococcus gnavus, Enterobacteriaceae, Sulphate-Reducing Bacteria [28] | Faecalibacterium prausnitzii, Bifidobacterium adolescentis, Dialister invisus, Clostridium cluster XIVa, Firmicutes, Bacteroidetes [28] | Reduced butyrate production; Increased hydrogen sulfide; Bile acid dysmetabolism [28] |
| Obesity (Model Systems) | Firmicutes (in some studies) [28] | Bacteroidetes (in some studies) [28] | Increased energy harvest; Altered SCFA profiles; Fecal transplant transmissibility [28] [32] |
| Antibiotic-Induced Dysbiosis | Enterobacteriaceae, Lactobacillaceae, Verrucomicrobiaceae [29] | Bifidobacterium, Lactobacillus, Faecalibacterium prausnitzii, Clostridiales clusters [29] | Reduced microbial diversity; Loss of colonization resistance [29] [2] |
Mechanisms of Dysbiosis in Disease Pathogenesis
Immune Dysregulation and Barrier Disruption
The mechanistic links between dysbiosis and disease pathogenesis involve complex interactions between microbial communities and host systems. One well-established pathway involves the disruption of intestinal barrier function coupled with dysregulated immune responses. In a healthy state, commensal bacteria such as Bacteroides fragilis and certain Clostridium strains induce regulatory T cells (Tregs) through specific mechanisms—PSA polysaccharide signaling through TLR2 in the case of B. fragilis, and TGF-β induction by Clostridium strains—which maintains immune tolerance and protects against inflammation [29]. During dysbiosis, the loss of these beneficial organisms diminishes Treg induction, creating an environment permissive to inflammation.
Concurrently, dysbiosis characterized by a decrease in butyrate-producing bacteria (e.g., F. prausnitzii) and an increase in sulphate-reducing bacteria leads to a compromised epithelial barrier [28]. Butyrate serves as a crucial energy source for colonocytes and supports the expression of tight junction proteins, while hydrogen sulfide produced by sulphate-reducing bacteria can inhibit butyrate utilization and directly damage the epithelium [28]. This combination of reduced butyrate and increased hydrogen sulfide diminishes barrier integrity, allowing bacterial translocation into the lamina propria. In genetically susceptible individuals with impaired bacterial clearance mechanisms, this translocation triggers excessive Toll-like receptor stimulation, pro-inflammatory cytokine secretion, and activation of adaptive immune responses, culminating in chronic inflammation [28].
Metabolic Consequences of Dysbiosis
Dysbiosis significantly alters the metabolic landscape of the gut environment, with systemic implications. The bile acid metabolism pathway represents a crucial mechanism linking microbial imbalance to disease. Under healthy conditions, Firmicutes and Bacteroides—the major bacterial groups decreased in IBD-associated dysbiosis—perform deconjugation of bile acids through bile salt hydrolase activity [28]. During dysbiosis, reduced capacity for bile acid transformation disrupts the anti-inflammatory signaling normally mediated by bile acids, potentially exacerbating intestinal inflammation [28]. This defective bile acid metabolism is particularly evident during IBD flares, suggesting it may serve both as a marker and mediator of disease activity.
Another emerging mechanism involves oxygenation of the gut environment. The healthy intestine maintains a low oxygen level that supports obligate anaerobes. Dysbiosis frequently features a decrease in Firmicutes (obligate anaerobes) and an increase in facultative anaerobes like Enterobacteriaceae, suggesting a fundamental disruption of the anaerobic gut environment [28]. This shift may be driven by increased reactive oxygen species during inflammation, creating a selective advantage for oxygen-tolerant bacteria and further perpetuating dysbiosis [28]. The resulting alteration in microbial metabolism affects the production of short-chain fatty acids (SCFAs), which normally influence everything from normal muscle function to inflammatory responses [32].
Diagram 1: The transition from symbiotic health to dysbiosis-associated disease involves multiple interconnected pathways. Environmental triggers, host genetics, antibiotics, and diet can disrupt the balanced microbiota, leading to functional impairments that drive disease pathogenesis.
Experimental Models and Methodologies
Animal Models for Dysbiosis Research
The investigation of dysbiosis mechanisms relies heavily on animal models, particularly germ-free (GF) mice, which provide a controlled system for studying host-microbe interactions. These models have been instrumental in establishing causality rather than mere association between microbial communities and disease phenotypes. For instance, studies have demonstrated that germ-free mice receiving fecal microbiota transplants from obese donors gain significantly more weight than those receiving transplants from lean donors, directly implicating the microbiota in metabolic disease [32]. Similarly, research using GF mice colonized with specific bacterial consortia has identified particular organisms, such as Bacteroides fragilis and certain Clostridium strains, that induce regulatory T cells and protect against inflammatory conditions [29].
The translation of findings from rodent models to humans requires careful consideration of interspecies differences in microbiota composition and host physiology. While human and murine gut microbiota share approximately 90% overlap at the phyla and genera levels, significant differences exist in the relative abundances of specific taxa [2]. The Firmicutes/Bacteroidetes ratio is notably higher in humans than in mice, and each species harbors unique genera—humans carry Faecalibacterium and Megasphera, while mice harbor Mucispirillum [2]. Additionally, differences in immune system regulation and transcription factor binding sites between species necessitate validation of rodent findings in human contexts [2]. Despite these limitations, rodent models remain invaluable for probing mechanistic pathways and testing therapeutic interventions in a controlled manner.
Table 3: Experimental Models in Dysbiosis Research
| Model System | Key Applications | Advantages | Limitations |
|---|---|---|---|
| Germ-Free (GF) Mice | Establishing causality; Studying microbial colonization; Host immune development [29] [2] | No resident microbiota; Controlled microbial exposure; Direct manipulation of variables [2] | Artificial environment; Immature immune system; Limited translational relevance [2] |
| Humanized Mice (GF mice + human microbiota) | Studying human-specific microbes; Personalized microbiota responses [2] | Human-relevant microbial communities; Maintains experimental control [2] | Still artificial environment; Mouse physiology differs from human [2] |
| Canine Models | Natural disease studies; Translational research for IBD, obesity [32] | Shared environment with humans; Spontaneous diseases; Similar gut microbiome to humans [32] | Genetic heterogeneity; Limited reagents; Ethical considerations [32] |
| Porcine Models | Nutrition studies; Microbiome development [32] | Similar GI tract and diet to humans; Comparable phenotype [32] | Cost; Housing requirements; Limited genetic tools [32] |
Methodologies for Dysbiosis Characterization
The comprehensive characterization of dysbiosis requires multi-omics approaches that capture taxonomic composition, functional potential, and metabolic activity. High-throughput 16S rRNA gene sequencing enables taxonomic profiling of bacterial communities, while shotgun metagenomics provides a broader view of the entire genetic repertoire, including bacteria, viruses, fungi, and archaea [28] [2]. Metatranscriptomics, metaproteomics, and metabolomics further illuminate the functional state of the microbial community by measuring gene expression, protein production, and metabolic output, respectively [6] [2].
Standardized protocols for sample collection, DNA extraction, and bioinformatic analysis are critical for generating comparable data across studies. For intestinal dysbiosis assessment, fecal samples represent the most accessible material, but mucosal biopsies may provide more relevant information for diseases like IBD where mucosa-associated microbes directly interact with host tissues [32]. Comprehensive digestive stool analysis examines the types and amounts of bacteria and yeast present, though these studies can be complex to perform and interpret [32]. Emerging techniques include the use of gas-sensing capsules to measure intraluminal gas production [6] and analysis of bacterial DNA in blood as a potential biomarker for systemic microbial translocation [6]. The field is also developing standardized dysbiosis indices, such as the GA-map Dysbiosis Test, to quantify the degree of microbial imbalance in clinical and research settings [6].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Platforms for Dysbiosis Investigation
| Reagent/Platform | Function | Application Examples |
|---|---|---|
| Germ-Free (GF) Rodent Systems | Provides microbiota-free baseline for colonization studies; Enables determination of causal relationships [29] [2] | Studying immune development; Microbial colonization resistance; Fecal microbiota transplantation [29] [2] |
| Gnotobiotic Animals | Animals with defined, known microbial consortia; Enables reductionist approaches to community function [29] | Identifying minimal functional communities; Probing microbe-microbe interactions; Determining keystone species [29] |
| 16S rRNA Sequencing Reagents | Amplification and sequencing of bacterial 16S rRNA gene; Taxonomic profiling of microbial communities [28] [2] | Comparative community analysis; Dysbiosis indices; Tracking microbial changes over time [28] [6] |
| Shotgun Metagenomics Kits | Comprehensive DNA sequencing of all microbial genomes in a sample; Functional gene cataloging [2] | Discovering novel organisms; Identifying metabolic pathways; Strain-level analysis [2] |
| Metabolomics Platforms | Measurement of microbial metabolites (SCFAs, bile acids, neurotransmitters) [6] | Connecting microbial function to host physiology; Identifying bioactive molecules; Biomarker discovery [28] [6] |
| Cell Culture Systems (e.g., organoids, transwell models) | Modeling host-microbe interactions in vitro; Studying barrier function and immune responses [29] | Mechanistic studies of specific host-microbe interactions; High-throughput screening of microbial products [29] |
| Riociguat | Riociguat|Soluble Guanylate Cyclase (sGC) Stimulator | Riociguat is a first-in-class sGC stimulator for pulmonary hypertension research. This product is for Research Use Only (RUO). Not for human consumption. |
| Bisphenol A-13C2 | Bisphenol A-13C2, CAS:263261-64-9, MF:C15H16O2, MW:230.27 g/mol | Chemical Reagent |
Diagram 2: Integrated experimental workflow for dysbiosis research, spanning sample collection, multi-omics characterization, bioinformatic analysis, and mechanistic validation in model systems.
Dysbiosis represents a critical transition from a mutually beneficial host-microbe relationship to a pathological state characterized by microbial imbalance and functional disruption. The comprehensive definition of dysbiosis encompasses three interrelated phenomena: loss of beneficial microorganisms, expansion of potentially harmful organisms, and reduction in overall microbial diversity [28] [29]. These changes disrupt essential microbial functions, including immune education, barrier maintenance, and metabolic regulation, creating pathways to disease [28] [29]. The mechanistic understanding of how dysbiosis contributes to conditions like IBD, obesity, and metabolic disorders has advanced significantly through integrated approaches combining multi-omics technologies, gnotobiotic animal models, and sophisticated bioinformatic analyses [28] [6] [29].
Future research directions will focus on moving beyond associations to establish causal mechanisms, with particular emphasis on microbiome metrics for clinical application [6], personalized microbiome-based interventions [6], and therapeutic strategies such as next-generation probiotics, prebiotics, and targeted microbial consortia [6] [30]. The ongoing development of standardized dysbiosis indices and validated protocols will enhance reproducibility and clinical translation. As our understanding of the transition from symbiosis to dysbiosis deepens, so too will opportunities to develop novel diagnostics and therapeutics that target the microbiome to restore health and prevent disease.
From Correlation to Causation: Advanced Methodologies for Functional Microbiome Research
The human gut microbiome plays a crucial role in both health and disease, influencing conditions ranging from metabolic disorders to inflammatory bowel disease and colorectal cancer. The choice of sequencing technology—16S ribosomal RNA (rRNA) gene sequencing or whole-genome shotgun metagenomics—profoundly impacts the resolution, depth, and biological insights attainable from microbial community analysis. This technical review provides a comprehensive comparison of these foundational methodologies, examining their theoretical principles, practical performance in disease association studies, and methodological considerations for implementation. Within the context of gut microbiome-health research, we demonstrate that while 16S rRNA sequencing offers a cost-effective entry point for taxonomic profiling, shotgun metagenomics provides superior taxonomic resolution and direct functional insights, albeit with higher computational and financial costs. Evidence from multiple clinical studies reveals that both techniques can effectively distinguish disease-associated dysbiosis, though shotgun sequencing often captures a more comprehensive picture of microbial community structure and function.
The human gut microbiome constitutes a complex ecosystem of bacteria, archaea, viruses, and eukaryotes that collectively contribute to host physiology through metabolic functions, immune modulation, and barrier protection [33]. Dysbiosis, or an alteration in this microbial community, has been associated with numerous disease states including inflammatory bowel diseases (IBD), metabolic dysfunction-associated steatotic liver disease (MASLD), colorectal cancer, and autoimmune disorders [34] [35]. Understanding the precise nature of these microbial alterations requires sophisticated analytical approaches that can characterize community composition and function.
The evolution of culture-independent techniques revolutionized microbiome research, with next-generation sequencing (NGS) technologies now enabling comprehensive profiling of microbial communities [33]. Two principal NGS approaches have emerged: 16S rRNA gene sequencing and shotgun metagenomic sequencing. The 16S method targets the conserved 16S ribosomal RNA gene as a phylogenetic marker, while shotgun sequencing randomly fragments and sequences all DNA present in a sample [36] [37]. The choice between these methods carries significant implications for project design, analytical capabilities, and biological interpretation, particularly in the context of gut microbiome-disease association studies where resolution, cost, and functional insights must be carefully balanced.
Technical Foundations of 16S and Shotgun Sequencing
16S rRNA Gene Sequencing
The 16S rRNA gene is a highly conserved bacterial marker containing nine variable regions (V1-V9) that provide taxonomic discrimination between organisms [35]. This method employs polymerase chain reaction (PCR) to amplify specific hypervariable regions (typically V3-V4 or V4) using universal primers, followed by sequencing of the resulting amplicons [38] [37].
Key technical considerations:
- Region selection: Different variable regions offer varying degrees of taxonomic resolution; no single region perfectly discriminates all species [38]
- PCR biases: Primer specificity and amplification efficiency can skew abundance measurements [38]
- Gene copy number variation: Bacteria contain varying copies of the 16S rRNA gene (e.g., 1-15 copies), potentially distorting abundance estimates [38]
- Database dependence: Taxonomic classification relies on reference databases (SILVA, Greengenes, RDP) that differ in size, curation, and update frequency [38]
Recent advancements include full-length 16S sequencing using long-read technologies (e.g., PacBio), which provides enhanced taxonomic resolution compared to short-read approaches targeting specific variable regions [35].
Shotgun Metagenomic Sequencing
Shotgun metagenomics applies random fragmentation to all DNA in a sample, followed by high-throughput sequencing without target-specific amplification [37]. This approach enables:
- Strain-level discrimination of microorganisms
- Identification of viruses, fungi, and archaea alongside bacteria
- Direct assessment of functional potential through gene content analysis [38] [39]
Technical challenges include:
- Host DNA contamination: Particularly problematic in tissue samples, requiring depletion strategies or increased sequencing depth [37]
- Computational complexity: Substantial hardware and bioinformatics resources needed for analysis [38]
- Reference database limitations: Unknown or uncharacterized taxa may remain unidentified despite sequencing [38]
Table 1: Core Technical Specifications of 16S rRNA and Shotgun Metagenomic Sequencing
| Parameter | 16S rRNA Sequencing | Shotgun Metagenomics |
|---|---|---|
| Target Region | 16S rRNA gene (specific variable regions) | Entire genome (all DNA) |
| PCR Amplification | Required (primers target 16S) | Not required (random fragmentation) |
| Taxonomic Resolution | Genus level (species level with full-length) | Species and strain level |
| Multi-Kingdom Coverage | Bacteria and Archaea only | Bacteria, Archaea, Viruses, Fungi, Protists |
| Functional Profiling | Indirect inference from taxonomy | Direct assessment of genes and pathways |
| Host DNA Interference | Minimal (PCR enriches microbial target) | Significant (may require depletion) |
| Reference Databases | SILVA, Greengenes, RDP | NCBI RefSeq, GTDB, UHGG |
Performance Comparison in Disease Association Studies
Taxonomic Resolution and Diversity Assessments
Multiple studies have directly compared the performance of 16S and shotgun sequencing in clinical contexts. A 2024 study comparing both techniques in colorectal cancer (CRC), advanced colorectal lesions, and healthy gut microbiota found that 16S detects only part of the gut microbiota community revealed by shotgun, with 16S abundance data being sparser and exhibiting lower alpha diversity [38]. At lower taxonomic ranks (species level), the two methods showed substantial disagreement, partially attributable to differences in reference databases [38].
In pediatric ulcerative colitis research, both 16S and shotgun sequencing consistently identified reduced alpha diversity in patients compared to healthy controls, though shotgun data provided superior species-level resolution of the dysbiotic taxa [40]. Notably, both methods achieved similar predictive accuracy for disease status (AUROC ≈ 0.90), suggesting that for case-control discrimination, 16S may provide sufficient resolution [40].
Functional Insights and Metabolic Pathways
A key advantage of shotgun sequencing is its capacity for direct functional profiling. By sequencing entire genomes, shotgun data enables reconstruction of metabolic pathways and identification of specific genes associated with disease states [36]. For example, shotgun analyses have revealed enrichment of specific enzymatic pathways in IBD and obesity, including nitrate reductase, choline metabolism, and carbohydrate assimilation pathways [36].
In contrast, 16S sequencing only permits inferred functionality based on taxonomic assignments, which may not accurately reflect the actual functional capacity of the microbial community [37]. This limitation significantly constrains mechanistic insights into host-microbiome interactions in disease contexts.
Diagnostic and Predictive Performance
The comparative predictive value of these techniques varies by disease context and specific implementation:
- In metabolic dysfunction-associated steatotic liver disease (MASLD), full-length 16S sequencing demonstrated significantly better predictive performance (AUC = 86.98%) compared to standard V3-V4 16S sequencing (AUC = 70.27%) in random forest models [35]
- In pediatric ulcerative colitis, both 16S and shotgun data yielded similar high prediction accuracy (AUROC ≈ 0.90) for disease status [40]
- For bacterial endophthalmitis diagnosis, metagenomic analysis significantly increased pathogen detection sensitivity compared to culture (61.9% vs. 28.5%), particularly in culture-negative cases [41]
Table 2: Comparative Performance in Disease Association Studies
| Disease Context | 16S rRNA Performance | Shotgun Metagenomics Performance | Key Findings |
|---|---|---|---|
| Colorectal Cancer [38] | Partial community detection; lower alpha diversity | More comprehensive profiling; higher resolution | Shotgun reveals broader diversity; 16S emphasizes dominant taxa |
| Pediatric Ulcerative Colitis [40] | AUROC ≈ 0.90; identifies major dysbiosis patterns | AUROC ≈ 0.90; provides species-level resolution | Comparable predictive accuracy despite resolution differences |
| MASLD [35] | FL16S: AUC = 86.98%; V3-V4: 70.27% | Not assessed in study | Full-length 16S outperforms short-read 16S |
| Endophthalmitis [41] | Not assessed | 61.9% detection rate vs. 28.5% for culture | Effective for pathogen detection in culture-negative cases |
| Interkingdom Interactions [39] | Limited to bacteria | Reveals bacteria-fungi nutrient competition | Shotgun enables multi-kingdom analysis |
Figure 1: Comparative Workflows of 16S rRNA and Shotgun Metagenomic Sequencing
Methodological Considerations and Experimental Design
Sample Preparation and Sequencing Protocols
DNA Extraction Methods:
- 16S sequencing: Compatible with lower DNA inputs (<1 ng); successful with minimal biomass [37]
- Shotgun sequencing: Requires higher DNA inputs (typically >1 ng/μL); challenging with low-biomass samples [37]
Enrichment Strategies: For shotgun sequencing of low-abundance community members (e.g., fungi), enrichment protocols can improve detection. Centrifugation-based size separation effectively enriches fungal cells (2-10 μm) from bacterial cells (0.2-2 μm) [39].
Sequencing Depth Requirements:
- 16S sequencing: Typically 10,000-100,000 reads per sample
- Shotgun sequencing: 5-20 million reads per sample for standard depth; "shallow shotgun" approaches reduce costs but provide less comprehensive data [37]
Bioinformatics and Computational Analysis
16S Data Processing:
- Quality filtering and trimming of raw reads (e.g., DADA2, QIIME2)
- Amplicon Sequence Variant (ASV) inference for high-resolution taxonomic units
- Taxonomic classification against reference databases (SILVA, Greengenes)
- Diversity analyses (alpha/beta diversity) and differential abundance testing [38] [36]
Shotgun Data Processing:
- Host DNA removal (e.g., KneadData, Bowtie2 against human genome)
- Taxonomic profiling using marker genes (MetaPhlAn) or reference mapping
- Functional annotation (HUManN2, MG-RAST) for pathway analysis
- Assembly and binning for metagenome-assembled genomes (MAGs) [36] [39]
Table 3: Essential Research Reagents and Computational Tools
| Category | Specific Tools/Reagents | Application/Purpose |
|---|---|---|
| DNA Extraction Kits | QIAamp PowerFecal Pro DNA Kit, NucleoSpin Soil Kit, DNeasy PowerLyzer Powersoil kit | Standardized microbial DNA isolation [38] [35] |
| 16S Primers | 341F/806R (V3-V4), 27Fmod/338R (V1-V2) | Amplification of specific variable regions [35] [41] |
| Sequencing Platforms | Illumina MiSeq/NextSeq, PacBio Sequel IIe | Amplicon and whole-genome sequencing [38] [35] |
| Quality Control | Trim Galore, FastQC, DADA2 | Sequence quality assessment and filtering [38] [40] |
| Taxonomic Classification | QIIME2, SILVA, Greengenes, GTDB, Kraken2 | Taxonomic assignment of sequences [38] [36] |
| Functional Profiling | HUManN2, MG-RAST, FunOMIC-T (fungal) | Metabolic pathway analysis [36] [39] |
| Statistical Analysis | R, Python, JMP, PERMANOVA | Diversity analysis and differential abundance testing [38] [34] |
Figure 2: Decision Framework for Selecting Appropriate Sequencing Technology
The choice between 16S rRNA and shotgun metagenomic sequencing involves careful consideration of research objectives, budget, and desired analytical outcomes. 16S sequencing provides a cost-effective approach for bacterial composition analysis, particularly in large cohort studies or when working with low-biomass samples, with full-length 16S offering improved resolution over short-read approaches [35]. Shotgun metagenomics delivers superior taxonomic resolution, strain-level discrimination, and direct functional insights, enabling more comprehensive mechanistic studies of host-microbiome interactions in health and disease [38] [39].
For gut microbiome-disease association research, evidence suggests both methods can identify dysbiotic patterns and generate predictive models with comparable accuracy for case-control classification [40]. However, shotgun sequencing provides the additional advantage of functional pathway analysis and multi-kingdom assessment, which may be crucial for understanding disease mechanisms and developing targeted interventions [39].
Future methodological developments will likely focus on hybrid approaches that leverage the cost-efficiency of 16S for large-scale screening with targeted shotgun sequencing for deep functional analysis. Additionally, integration with other omics technologies (metatranscriptomics, metabolomics) will provide more comprehensive insights into the dynamic interactions between gut microbes and host health [36]. As sequencing costs continue to decline and analytical methods improve, shotgun metagenomics is poised to become the gold standard for comprehensive microbiome analysis, though 16S sequencing will retain utility for specific applications where cost constraints or sample type make shotgun sequencing impractical.
The study of the gut microbiome has evolved far beyond taxonomic cataloging using genomic sequencing. While metagenomics has been pivotal in identifying microbial composition and its association with human health and disease, it primarily reveals functional potential, not biological activity. The integration of metatranscriptomics, metaproteomics, and metabolomics now provides a comprehensive, multi-dimensional view of microbiome function and host-microbe interactions. This technical guide details the methodologies and applications of these post-genomic omics layers, framing them within gut microbiome-health research. By capturing the actively transcribed genes, expressed proteins, and dynamic metabolite pools, researchers can move from correlation to causation, uncovering the mechanistic drivers of diseases such as inflammatory bowel disease, cancer, and allergic rhinitis, thereby informing novel diagnostic and therapeutic strategies.
Metagenomics, the DNA-level analysis of microbial communities, has been a cornerstone of microbiome research, enabling the profiling of microbial taxonomy and the genetic potential of complex ecosystems without the need for cultivation [42]. Landmark projects like the Human Microbiome Project (HMP) and Metagenomics of the Human Intestinal Tract (MetaHIT) established extensive reference databases of gut microbial genes and genomes, revealing that while taxonomic profiles vary greatly between individuals, a core set of functional genes is often conserved [42].
However, a primary limitation of metagenomics is its inability to distinguish between active and dormant members of the community or to reveal the real-time functional state of the ecosystem. It answers "What could happen?" based on genetic potential, but not "What is happening?" in a specific physiological or disease context [42]. Microbial functions are dynamically regulated in response to the host environment, and this functional plasticity is a key feature in health and disease. For instance, a metagenomic study might identify the presence of genes for short-chain fatty acid (SCFA) production, but only through metabolomics can the actual, clinically relevant levels of these anti-inflammatory metabolites be quantified [43].
This critical gap is bridged by the sequential, functional omics layers:
- Metatranscriptomics reveals the genes that are actively being transcribed, providing a view of microbial responses to their environment.
- Metaproteomics identifies and quantifies the proteins that execute cellular functions, serving as a direct link between genetic potential and biochemical activity.
- Metabolomics profiles the end-products and signaling molecules of metabolic pathways, offering a snapshot of the functional output that directly influences host physiology.
The integration of these technologies is transforming gut microbiome research from a descriptive field to a mechanistic science, enabling the development of personalized microbiome-based diagnostics and therapeutics.
Metatranscriptomics: Profiling Community-Wide Gene Expression
Metatranscriptomics involves the comprehensive analysis of RNA molecules, primarily messenger RNA (mRNA), extracted directly from a microbial community. It aims to characterize the transcriptomic profile and identify the actively expressed genes within a complex sample [44].
The typical workflow begins with the extraction of total RNA from a sample, such as stool or a gut biopsy. A critical and challenging step is the enrichment of microbial mRNA and the removal of abundant host and microbial ribosomal RNA (rRNA). The purified mRNA is then reverse-transcribed into complementary DNA (cDNA), which is prepared into libraries and sequenced using high-throughput platforms. The resulting sequences (RNA-Seq) are then processed bioinformatically: host-derived reads are filtered out, and the remaining reads are aligned to reference genomic databases for taxonomic assignment and functional analysis [44] [45]. A key advantage is its ability to reveal the functional expression of microbial genes, providing insights into the activity of microorganisms, including those that are uncultivable in vitro [44].
Application in Gut Microbiome Research
Metatranscriptomics provides unparalleled insight into the dynamic responses of the gut microbiota. A prime example is its application in studying urinary tract infections (UTIs), which offers a parallel for understanding gut pathobiology. One study integrated metatranscriptomic sequencing with genome-scale metabolic modeling (GEMs) to characterize the active metabolic functions of patient-specific urinary microbiomes [45]. This approach revealed significant inter-patient variability not just in microbial composition, but in transcriptional activity and metabolic behavior of the primary pathogen, E. coli. The study showed that virulence strategies, such as the expression of adhesion genes (fimA, fimI) and iron acquisition genes (chuY, chuS, iroN), varied markedly across patients, underscoring the pathogen's adaptability [45].
Furthermore, by constraining metabolic models with gene expression data, researchers can predict context-specific metabolic fluxes, moving beyond static gene lists to dynamic functional predictions. For instance, pathways like 'arginine and proline metabolism' and the 'pentose phosphate pathway' showed highly variable activity across different patient samples, highlighting the metabolic heterogeneity that would be invisible to metagenomics alone [45].
Table 1: Key Metatranscriptomics Findings in Microbiome Studies
| Study Focus | Key Metatranscriptomic Insight | Reference |
|---|---|---|
| Uropathogenic E. coli (UPEC) Infection | Revealed patient-specific variability in virulence gene expression (e.g., adhesion, iron acquisition) and active metabolic pathways. | [45] |
| Vaginal Microbiome | Showed how G. vaginalis circumvents antibiotic stress by expressing DNA repair genes. | [45] |
| General Workflow | Identifies active metabolic pathways and quantifies gene expression levels, providing a dynamic view of community function. | [44] |
Figure 1: Metatranscriptomics Workflow. The process from sample collection to functional interpretation, highlighting key steps like mRNA enrichment and bioinformatic filtering.
Metaproteomics: Identifying and Quantifying Expressed Proteins
Metaproteomics is the large-scale characterization of the entire protein complement recovered directly from a microbial community in an environmental sample [44]. Proteins are the functional effectors of the cell, catalyzing reactions, providing structure, and facilitating signaling. Therefore, metaproteomics provides a direct measure of the physiological state and functional activity of a microbiome.
The standard workflow involves protein extraction from a complex sample, followed by digestion into peptides using an enzyme like trypsin. These peptides are then separated by liquid chromatography (LC) and analyzed by tandem mass spectrometry (MS/MS). The mass spectra generated are matched against protein sequence databases derived from metagenomic or genomic data to identify the proteins present. Quantitative metaproteomics can be achieved through label-free methods or by using stable isotope labels, allowing researchers to compare protein abundance across different conditions (e.g., health vs. disease) [44]. Recent advances, such as the integration of metaproteomics with metagenomics using tools like Unipept, have significantly improved the resolution of microbial community function in complex environments [44].
Application in Gut Microbiome Research
Metaproteomics bridges the gap between genetic potential and metabolic output. By quantifying the enzymes actually being produced by the gut microbiota, it reveals which metabolic pathways are actively operating. This is crucial for understanding the microbial contribution to host physiology. For example, the quantification of enzymes involved in the production of SCFAs like butyrate provides direct evidence of the microbiome's capacity to generate these key anti-inflammatory and energy substrates for the host colonocytes.
While the provided search results note that metaproteomics is less frequently applied to skin microbiome research due to technical challenges like low biomass [44], these challenges are also present in gut research, particularly when studying mucosal biopsies. However, fecal samples provide sufficient biomass for robust analysis. The integration of metaproteomic data with other omics layers creates a powerful framework for understanding host-microbiome interactions. For instance, correlating the abundance of bacterial enzymes with host receptor proteins can illuminate specific mechanisms of cross-talk.
Metabolomics: Profiling the Functional Readout of Microbial Activity
Metabolomics involves the comprehensive profiling of the complete set of small molecule metabolites (<1.5 kDa) within a biological system. In microbiome research, it captures the final functional readout of microbial activity and the key signaling molecules that mediate host-microbe interactions [46] [43]. These metabolites include SCFAs, bile acids, amino acid derivatives (like tryptophan catabolites), vitamins, and lipids.
There are two primary analytical approaches:
- Untargeted Metabolomics: A global, hypothesis-generating approach that aims to detect and measure as many metabolites as possible from a sample.
- Targeted Metabolomics: A hypothesis-driven approach that focuses on the accurate quantification of a predefined set of metabolites, often related to a specific pathway.
Both approaches typically rely on mass spectrometry (MS), often coupled with a separation technique like gas chromatography (GC) or liquid chromatography (LC). The resulting data is complex and requires sophisticated bioinformatics tools for peak identification, alignment, and statistical analysis to identify metabolites that are differentially abundant between experimental groups.
Application in Gut Microbiome Research
Metabolomics is instrumental in linking gut microbial function to host health and disease. A study on allergic rhinitis (AR) exemplifies this power. Integrated 16S rRNA sequencing and untargeted metabolomics of fecal samples from AR patients and healthy controls revealed significant disturbances in microbial metabolites. The study identified dysregulation in pathways for pantothenate and CoA biosynthesis, glycolysis, and pyruvate metabolism. Key discriminatory metabolites like maltol and 4-coumaric acid were discovered, and integrative analysis revealed significant correlations between specific bacteria and metabolites; for instance, Faecalibacterium was correlated with D-phenyllactic acid [43]. This directly implicates microbial-derived metabolites in the immune dysregulation of AR via the "gut-nose axis."
Another key example is tryptophan metabolism. A mouse study using targeted quantitative metabolomics demonstrated that the cecal microbiota massively impacts tryptophan metabolism both in the gut and systemically [46]. Tryptophan is metabolized into a wide array of bioactive molecules (e.g., indole derivatives, serotonin, kynurenine) by host and microbial enzymes, and these metabolites are crucial for maintaining immune homeostasis and intestinal barrier function.
Table 2: Key Microbial Metabolites and Their Roles in Host Health
| Metabolite Class | Example Metabolites | Postulated Role in Health & Disease |
|---|---|---|
| Short-Chain Fatty Acids (SCFAs) | Butyrate, Acetate, Propionate | Primary energy source for colonocytes; anti-inflammatory; regulate immune homeostasis [43]. |
| Tryptophan Catabolites | Indole, Indole-3-propionic acid, Kynurenine | Activate aryl hydrocarbon receptor (AhR); regulate immune responses and mucosal barrier integrity [46]. |
| Bile Acids | Secondary bile acids (e.g., deoxycholic acid) | Regulate host metabolism, function as signaling molecules, possess anti-inflammatory properties [43]. |
| Dysregulated Metabolites in AR | Maltol, 4-Coumaric acid, D-phenyllactic acid | Associated with allergic rhinitis pathogenesis; potential biomarkers for disease [43]. |
Figure 2: Gut Microbiota Derived Metabolites and Host Physiology. Microbial metabolites act as key signaling molecules that influence critical host functions including immune regulation, barrier maintenance, and metabolism.
The Scientist's Toolkit: Essential Reagents and Methods
Table 3: Research Reagent Solutions for Multi-Omics Microbiome Analysis
| Item / Reagent | Function / Application | Technical Notes |
|---|---|---|
| Stool DNA/RNA Kits | Simultaneous or separate isolation of high-quality genomic DNA and total RNA from stool samples. | Critical for paired metagenomic/metatranscriptomic analysis; should include steps to remove PCR inhibitors. |
| rRNA Depletion Kits | Selective removal of abundant ribosomal RNA to enrich for messenger RNA (mRNA) prior to metatranscriptomic sequencing. | Essential for reducing sequencing costs and increasing coverage of informative transcripts. |
| Protein Lysis Buffers | Efficient extraction of proteins from complex, hard-to-lyse bacterial communities in stool or biopsy samples. | Must be compatible with downstream mass spectrometry analysis. |
| Metabolite Extraction Solvents | Deproteinization and extraction of small molecule metabolites from biofluids (serum, urine) or fecal samples. | Typically methanol/acetonitrile/water mixtures; method depends on targeted metabolite class (e.g., SCFAs require acidification). |
| 16S rRNA Gene Primers | Amplification of hypervariable regions for bacterial community profiling via amplicon sequencing. | Choice of primer set (e.g., V3-V4) influences taxonomic resolution and bias [44]. |
| In silico Urine Medium | A defined, virtual culture medium for genome-scale metabolic modeling (GEM) simulations of microbial communities. | Based on databases like the Human Urine Metabolome Database; constrains models to a physiologically relevant environment [45]. |
| Virulence Factor Database (VFDB) | A curated resource for annotating bacterial virulence-associated genes from sequencing data. | Used to identify and interpret expression of pathogenicity factors, e.g., in UPEC studies [45]. |
| Phenprocoumon-d5 | Phenprocoumon-d5, MF:C18H16O3, MW:285.3 g/mol | Chemical Reagent |
| Bambuterol-d9hydrochloride | Bambuterol-d9hydrochloride, MF:C18H30ClN3O5, MW:413.0 g/mol | Chemical Reagent |
Integrated Multi-Omics Workflow and Data Integration
The true power of these technologies is realized not in isolation, but through their integration. A synergistic multi-omics workflow provides a more complete picture of the microbiome-host interface, from genetic potential (metagenomics) to active gene expression (metatranscriptomics), to functional protein machinery (metaproteomics), and finally to the metabolic activity and signaling (metabolomics).
This integrated approach is being propelled by initiatives like the Integrative Human Microbiome Project (iHMP), which applies multi-omics strategies to investigate the dynamics of host-microbiome interactions in health and disease [42]. The analytical challenge lies in the computational integration of these vast, heterogeneous datasets. Advanced statistical methods, correlation networks (like those used in the AR study to link bacteria and metabolites [43]), and systems biology approaches, such as the constraint-based metabolic modeling used in the UTI study [45], are essential for deriving biologically meaningful insights.
By weaving together these four layers of omic data, researchers can construct detailed, mechanistic models of how the gut microbiome influences human health, paving the way for targeted interventions such as personalized probiotics, prebiotics, and microbiome-based diagnostics for conditions ranging from allergic disease to cancer immunotherapy response.
The human microbiome plays a vital role in controlling fundamental physiological functions, including immune system development, protection against pathogens, and modulation of the central nervous system [47]. In the last decade, dramatic increases in microbiome publications have revealed compelling discoveries linking the microbiome to metabolic diseases, digestive diseases, and cardiovascular conditions [48]. However, low concordance between studies examining microbiota in human diseases presents a pervasive challenge that limits the capacity to identify causal relationships between host-associated microbes and pathology [49]. Wide inter-individual heterogeneity in microbiota composition, likely due to population-wide differences in human lifestyle and physiological variables, exacerbates the risk of obtaining false positives in human microbiota research [49].
Meticulous study design represents a foundational step toward obtaining meaningful results in microbiome research [48]. The complexity of microbiome data, characterized by zero inflation, overdispersion, high dimensionality, and sample heterogeneity, demands rigorous methodological approaches [47]. Furthermore, appropriate statistical methods are crucial for accurate interpretation of microbiome data, particularly when transitioning from correlational observations to causative mechanistic insights [50]. This technical guide synthesizes current evidence and methodologies to equip researchers with strategies for designing robust human microbiome studies that can effectively distinguish true disease-associated signals from spurious associations.
Foundational Concepts in Microbiome Research
Terminology and Metrics
Understanding core concepts and metrics is essential for proper study design in microbiome research. The terms microbiota and microbiome are often used interchangeably, but have distinct meanings: microbiota refers specifically to the microorganisms inhabiting a specific site on or in the body, consisting of bacteria, archaea, viruses, fungi, and protozoans, while microbiome encompasses the entire habitat, including the microorganisms, their genomes, and surrounding environmental conditions [48]. Key diversity metrics include α-diversity, measuring diversity within a single sample through indices such as Chao1 (richness), Shannon-Wiener (combining richness and evenness, weighted toward rare species), and Simpson (also combining richness and evenness but emphasizing common species) [48]. β-diversity quantifies microbiota differences between samples or groups using measures like Bray-Curtis dissimilarity (compositional dissimilarity emphasizing common species) and UniFrac distance (phylogenetic-based, either unweighted focusing on presence/absence or weighted incorporating abundance information) [48].
Analytical Approaches in Microbiome Data
Microbiome data analysis typically focuses on three principal areas: (1) differential abundance analysis, detecting differentially abundant taxa across phenotype groups; (2) integrative analysis, identifying associations between taxonomies and covariates; and (3) network analysis, characterizing associations between taxa across the entire microbiome network [47]. The choice of sequencing technology—16S ribosomal RNA (rRNA) gene sequencing versus metagenomic shotgun sequencing (MSS)—represents a fundamental design decision with implications for resolution, cost, and analytical approach [47]. 16S rRNA sequencing provides a cost-effective method for identifying and classifying bacteria and archaea at higher taxonomic levels (phyla and genera), while MSS offers superior resolution for classifying bacteria at the species level and can additionally identify viruses, fungi, and protozoa [47].
Table 1: Key Diversity Metrics in Microbiome Research
| Metric Type | Index Name | What It Measures | Interpretation |
|---|---|---|---|
| α-diversity | Chao1 | Richness (estimated total species) | Higher value = more species |
| Shannon-Wiener | Richness + evenness (weights rare species) | Higher value = more diversity (generally <5.0) | |
| Simpson | Richness + evenness (weights common species) | Higher value = more diversity (0-1 range) | |
| β-diversity | Bray-Curtis dissimilarity | Compositional dissimilarity | 0 = identical composition, 1 = no shared species |
| Unweighted UniFrac | Phylogenetic distance (presence/absence) | Sensitive to rare species | |
| Weighted UniFrac | Phylogenetic distance (abundance-weighted) | Reduces contribution of rare species |
Methodological Framework for Cohort Design
Study Design Schemes
The most prevalent study designs in medical microbiome research include cross-sectional studies, case-control studies, longitudinal studies, and randomized controlled trials (RCTs) [48]. Cross-sectional studies can be descriptive (characterizing microbiota composition in populations) or analytical (exploring associations between microbiome and health outcomes), but face limitations in establishing causal relationships because microbiome and outcomes are measured simultaneously [48]. Case-control designs compare microbiota between individuals with specific conditions (cases) and those without (controls), though this approach risks confounding if cases and controls differ systematically in other variables that affect microbiota [49]. Longitudinal studies collect data from the same individuals over time, providing insights into temporal dynamics of microbiome changes in relation to health outcomes, while randomized controlled trials (RCTs) represent the gold standard for establishing causal relationships by intentionally applying interventions and randomly assigning subjects to treatment groups [48].
Sample Size Considerations
Appropriate sample size calculation is essential for ensuring sufficient statistical power in microbiome studies. A threshold of approximately 500 cases and controls has been shown to maximize Random Forests model performance in microbiome analyses [49]. However, optimal sample size depends on multiple factors, including effect size expectations, sequencing technology, and analytical approach. Researchers should consider performing formal power calculations specific to their primary outcomes during the study design phase, acknowledging that many microbiome effect sizes may be modest and require larger sample sizes for reliable detection.
Confounder Management in Microbiome Studies
Identification of Key Confounding Variables
Confounding variables represent perhaps the most significant challenge in observational microbiome studies. These are factors that differ between case and control groups and independently influence microbiota composition, potentially creating spurious associations if unevenly distributed. Through machine learning approaches applied to large datasets, researchers have identified the most robust sources of human gut microbiota variability, with surprising findings that some host variables previously underappreciated exert strong effects on microbiota composition [49].
Table 2: Major Confounding Variables in Microbiome Studies
| Confounder Category | Specific Variables | Impact on Microbiome | Recommendation |
|---|---|---|---|
| Demographic | Age, Sex, Geographical location | Significant association with composition [49] | Match cases/controls or statistically adjust |
| Lifestyle/Diet | Alcohol consumption frequency, Dietary intake patterns (meat, vegetables, whole grains) | Robust, dose-dependent segregation of microbiota profiles [49] | Record and control through study design |
| Physiological | Body Mass Index (BMI), Bowel movement quality | Among strongest microbiota covariates [49] [51] | Measure and match participants |
| Medical | Medication use (especially metformin), Dental status | Dramatic shifts in microbiota composition [48] [51] | Document and account for in analysis |
| Inflammatory Markers | Fecal calprotectin | Primary microbial covariate, supersedes variance explained by CRC diagnostic groups [51] | Quantify and control analytically |
| Gut Function | Transit time (moisture content) | Biggest explanatory power for overall gut microbiota variation in multiple cohorts [51] | Measure and include as covariate |
Strategies for Confounder Control
Subject Matching
Pairwise matching of case and control subjects represents one of the most effective approaches for mitigating confounding effects. This process involves identifying for each case subject a control individual matched for values of key microbiota-associated confounding variables using Euclidean distance-based processes [49]. Empirical evidence demonstrates that matching cases and controls for confounding variables significantly reduces observed microbiota differences and incidence of spurious associations [49]. For example, when type 2 diabetes cases and controls were matched for alcohol intake frequency, BMI, and age, initially significant microbiota differences substantially diminished or became non-significant [49].
Statistical Adjustment
Statistical methods provide an alternative or complementary approach for addressing confounding. Linear mixed effects models can incorporate confounding variables as covariates to adjust for their effects [49]. However, evidence suggests that statistical adjustments alone may be insufficient, as they can fail to discern true signal from confounding factors. In type 2 diabetes studies, adding BMI, age, and alcohol intake as covariates in linear mixed effects models reduced the number of spurious amplicon sequence variants (ASVs) identified as significantly different, but some spurious observations remained [49]. Thus, statistical adjustment works best when combined with careful subject selection rather than as a standalone solution.
Quantitative Microbiome Profiling
The transition from relative microbiome profiling (RMP) to quantitative microbiome profiling (QMP) represents a crucial methodological advancement. Relative profiling expresses taxon abundances as percentages, creating compositionality constraints where changes in one taxon's abundance necessarily affect the apparent abundances of all others [51]. In contrast, QMP utilizes experimental approaches to determine absolute microbial abundances, facilitating normalized comparisons across different samples or conditions and reducing both false-positive and false-negative rates [51]. In colorectal cancer studies, applying QMP combined with rigorous confounder control revealed that transit time, fecal calprotectin, and BMI served as primary microbial covariates, superseding variance explained by cancer diagnostic groups [51].
Experimental Protocols and Workflows
Standardized Experimental Workflow
A robust microbiome study requires meticulous attention to experimental workflows, from study design through sample collection, processing, and data analysis. The following diagram illustrates a comprehensive approach integrating confounder control throughout the research process:
Sample Collection and Processing
Sample collection protocols must be standardized across all study participants to minimize technical variability. Key considerations include: (1) consistent timing of collection relative to physiological processes; (2) standardized storage conditions immediately after collection; (3) use of uniform collection materials across all participants; and (4) documentation of collection time and conditions [48]. For low microbial biomass samples (e.g., human milk, skin), stringent negative and positive controls need to be included to detect and account for contamination, which is omnipresent in microbiome studies [52]. Several approaches are available to prevent and detect contamination, including sterile sampling and spike-in quantitative approaches for low biomass communities [52].
DNA extraction represents another critical source of technical variability. Selection of extraction methodology should be based on the sample type and should remain consistent throughout the study. Validation experiments comparing extraction efficiency across different sample types may be necessary when studying multiple body sites. The inclusion of internal standards or spike-ins during the extraction process can help normalize for technical variability and enable more quantitative comparisons [51].
Analytical Approaches and Statistical Methods
Differential Abundance Analysis
Multiple statistical methods have been developed specifically for detecting differentially abundant taxa in microbiome data, each with distinct approaches to handling data characteristics like zero inflation, compositionality, and overdispersion. Key methods include:
edgeR: Originally developed for RNA-Seq data, it uses a negative binomial model to account for biological and technical variability, with TMM (trimmed mean of M-values) normalization as the default approach [47].
DESeq2: Similarly employs a negative binomial model but incorporates additional features for handling outliers and small sample sizes, using RLE (relative log expression) normalization [47].
metagenomeSeq: Specifically designed for microbiome data, it addresses zero inflation through cumulative sum scaling (CSS) normalization and a zero-inflated Gaussian model [47].
ANCOM (Analysis of Compositions of Microbiomes): Accounts for compositionality through log-ratio transformations of the abundance data, making fewer assumptions about distributional properties [47].
corncob: Uses a beta-binomial model to explicitly model the mean and overdispersion of taxon abundances as functions of covariates [47].
Method selection should be guided by study design, data characteristics, and specific research questions. For studies with pronounced compositionality concerns, composition-aware methods like ANCOM may be preferable, while studies with complex experimental designs may benefit from the flexibility of corncob's modeling approach.
Data Normalization Strategies
Normalization represents a critical transformation step that accounts for technical variability in sequencing technology. Commonly used normalization methods include:
Total Sum Scaling (TSS): Converts raw counts to relative abundances by dividing each count by the total reads in the sample.
Cumulative Sum Scaling (CSS): Part of the metagenomeSeq package, CSS normalizes based on the cumulative distribution of counts up to a data-derived percentile.
Relative Log Expression (RLE): The default method in DESeq2, which calculates size factors based on the geometric mean of counts across samples.
Trimmed Mean of M-values (TMM): Implemented in edgeR, TMM trims extreme log fold-changes and large counts to calculate scaling factors.
Centered Log-Ratio (CLR): A compositionally aware transformation that log-transforms ratios of counts to the geometric mean of the sample.
The choice of normalization method should align with both the statistical method being employed and the specific characteristics of the dataset. For quantitative microbiome profiling, additional normalization based on flow cytometry counts or internal standards may be incorporated to obtain absolute abundances [51].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Microbiome Studies
| Category | Item/Reagent | Function/Application | Considerations |
|---|---|---|---|
| Sample Collection | Stool collection kits with DNA/RNA stabilizers | Preserves microbial composition at time of collection | Ensure compatibility with downstream applications |
| Skin swabs with transport media | Standardized collection from skin surfaces | Critical for low-biomass sites | |
| DNA Extraction | Kit with bead-beating step | Mechanical disruption of tough microbial cell walls | Essential for Gram-positive bacteria |
| Internal standard spikes (e.g., mock communities) | Quantification and quality control | Distinguishes technical from biological zeros | |
| Library Preparation | 16S rRNA gene primers (e.g., V4 region) | Target amplification for bacterial communities | Region selection affects taxonomic resolution |
| Shotgun metagenomic kit | Comprehensive genomic analysis | Higher cost but superior resolution | |
| Sequencing | High-throughput sequencing platforms (Illumina) | Generating sequence data | Read length and depth requirements vary by application |
| Computational Tools | QIIME2, MOTHUR, DADA2 | Bioinformatic processing of raw sequence data | DADA2 produces ASVs; traditional approaches produce OTUs |
| R packages (phyloseq, microbiome, vegan) | Statistical analysis and visualization | Extensive resources for diverse analyses | |
| Standards & Controls | Negative extraction controls | Detection of contamination | Essential for low-biomass samples |
| Positive controls (mock communities) | Assessment of technical variability | Should represent expected community composition | |
| Ranitidine-d6 | Ranitidine-d6, CAS:1185514-83-3, MF:C13H22N4O3S, MW:320.441 | Chemical Reagent | Bench Chemicals |
| Metolachlor-d6 | Metolachlor-d6, CAS:1219803-97-0, MF:C15H22ClNO2, MW:289.83 g/mol | Chemical Reagent | Bench Chemicals |
The field of human microbiome research has evolved from initial descriptive studies to more sophisticated analytical approaches capable of identifying robust, reproducible associations. By implementing rigorous cohort designs with appropriate confounder control, utilizing quantitative profiling methods, and applying appropriate statistical analyses, researchers can significantly enhance the validity and translational potential of their findings. The framework presented in this guide provides a roadmap for designing microbiome studies that effectively distinguish true biological signals from spurious associations, ultimately advancing our understanding of the critical role the microbiome plays in human health and disease. As the field continues to mature, these methodological rigor standards will be essential for generating findings that can successfully transition from correlation to causation and ultimately to clinical applications.
The gut microbiota is now recognized as a forgotten organ, playing a critical role in a vast array of physiological activities across different body organs through neurological, metabolic, immune, and endocrine pathways [53]. Within this research landscape, germ-free (GF) animal models serve as indispensable tools for moving beyond correlation to establish causality in host-microbe interactions. These models provide a blank microbial background, enabling researchers to directly assess the role of microbiota in all aspects of physiology and disease, and to verify the effects of colonization with specific microbial species [53] [54]. For researchers and drug development professionals investigating microbiome-mediated health and disease associations, GF mice represent a biological model system that allows for precise dissection of mechanisms and validation of therapeutic targets, free from the confounding influences of an established microbial community [53]. This in-depth technical guide explores the development, application, and methodological considerations for utilizing gnotobiotic mice in mechanistic research, providing a foundation for rigorous experimental design in microbiome therapeutics.
Germ-Free and Alternative Microbiota-Modified Models
Model Selection: Germ-Free vs. Antibiotic-Treated Mice
Two primary methods are employed to explore microbiota effects in mice: isolated germ-free models and antibiotics treatment regimens. The table below compares their core characteristics.
Table 1: Comparison of Germ-Free and Antibiotic-Treated Mouse Models
| Feature | Germ-Free (GF) Mice | Antibiotic-Treated (ABX) Mice |
|---|---|---|
| Microbial Status | Complete absence of detectable microbes [54] [55] | Broad depletion, but not complete elimination, of gut microbiota [55] |
| Key Advantage | "Gold standard"; pristine blank slate for mono-association or humanization [54] [55] | Rapid, accessible, and inexpensive; applicable to any genotype [55] |
| Developmental Immunity | Broadly impaired in early immune development and education [55] | Allows study of bacterial role in maintaining immunity after development [55] |
| Technical Requirements | Specialized, labor-intensive isolator facilities; high cost [53] [55] | Standard housing; minimal technical expertise required [55] |
| Experimental Limitations | Limited genotype availability; impractical for some behavioral/infection studies [55] | Potential for antibiotic off-target effects; risk of antibiotic-resistant bacterial outgrowth [54] [55] |
While antibiotic-treated models offer accessibility, GF models are considered the gold standard for mechanistic validation because they avoid the potential off-target effects of antibiotics and provide a truly microbe-free starting point [54]. For instance, studies have shown that results from antibiotic-treated models can be confounded by the drugs' unintended effects, whereas GF conditions provide clearer causal evidence [54].
The Humanized Gnotobiotic Mouse Model
A powerful extension of the GF model is the humanized gnotobiotic mouse, created by transplanting human fecal microbiota into GF mice [54]. This model provides an innovative tool to mimic the human microbial system within a controllable laboratory animal, bridging the gap between human and animal gut physiology [54]. The successful creation of this model depends on a continuous and faithful progression of human flora in the mouse, requiring careful consideration of factors related to the human donor and the murine host environment to ensure clinical relevance and reproducibility [54].
Core Experimental Workflows and Methodologies
Workflow for Establishing a Humanized Gnotobiotic Model
The process of creating and utilizing humanized gnotobiotic mice for mechanistic studies involves a multi-stage workflow, from donor selection to phenotypic analysis.
Key Considerations for Experimental Design
Donor Selection: The choice of human donor is paramount. Variations in gut flora based on geography, diet, ethnicity, and health status will inevitably result in different outcomes in the mouse model [54]. For example, studies comparing rural non-western and western populations show distinct microbial clustering, with non-western children having higher flora diversity and different relative abundances of major phyla like Bacteroidetes and Firmicutes [54]. Standardizing donor criteria or deliberately selecting donors based on these variables is critical for reproducible and targeted research.
Recipient Factors: The genetic background of the GF mouse recipient can influence how microbial communities colonize and interact with the host. Matching the murine context (e.g., immune status, genetic susceptibility to disease) to the research question is essential for faithful modeling of human conditions [54].
Validation of Engraftment: Successful colonization requires rigorous validation beyond 16S rRNA gene sequencing. This includes functional assessments like global metabolomics of cecal contents to confirm that the transplanted microbiota not only resembles the donor's community structure but also replicates its metabolic activity [56]. Transfer of non-bacterial constituents (fungi, viruses) and pathogens should also be characterized where relevant [56].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Gnotobiotic Research
| Reagent/Material | Function/Application | Technical Notes |
|---|---|---|
| Germ-Free Mice | A microbe-free in vivo system for establishing causality in host-microbe interactions [53] [54]. | Must be regularly monitored for contamination via culturing, serology, and PCR [55]. Available from specialized vendors (e.g., Taconic, Jackson Laboratory, Charles River). |
| Defined Microbial Consortia | Used to colonize GF mice with a simplified, known community to study specific microbe-host functions [53]. | Lacks the complexity of natural microbiota but offers high reproducibility [56]. |
| Natural Gut Microbiota (Wildling-derived) | A complex, resilient microbial community transplanted from wild mice to create models with a more mature, human-like immune system [56]. | Can be viably preserved, bio-banked, and engrafted into lab mice via oral gavage to create "TXwildlings" [56]. |
| Antibiotic Cocktails | Used to deplete, rather than eliminate, the gut microbiota as an alternative to GF models [55]. | Common components: ampicillin, vancomycin, neomycin, metronidazole [55]. Often includes antifungals (e.g., amphotericin B). |
| Fecal Microbiota Transplantation (FMT) Material | The inoculum for humanizing GF mice, typically from characterized human donors or other animal models [54] [56]. | Must be processed (homogenization, filtration) under anaerobic conditions to preserve viability of obligate anaerobes. |
| Gnotobiotic Isolators | Flexible film or rigid steel chambers that provide a sterile environment for housing and manipulating GF mice [53]. | Require specialized sterilization protocols (e.g., vapor-phase hydrogen peroxide) and aseptic techniques for maintenance. |
| PGDM | PGDM (Tetranor Prostaglandin D Metabolite) – Research Use Only | PGDM is a key biomarker for in vivo PGD2 biosynthesis. This product is for Research Use Only. Not for diagnostic or therapeutic applications. |
Mechanistic Insights and Therapeutic Target Validation
Signaling Pathways Modulated by the Microbiota
GF mice have been instrumental in uncovering how specific microbial signals regulate host pathways. The diagram below illustrates a key pathway validated using this model.
Germ-free models have revealed that the gut microbiota suppresses tonic Hedgehog (Hh) signaling in the small intestine, a mechanism critical for regulating intestinal barrier function. This suppression occurs through Toll-like receptor (TLR2/TLR1) signaling in the intestinal epithelium, with GF studies identifying intestinal epithelial neuropilin-1 (NRP1) as a microbiota-dependent Hh regulator [53]. Furthermore, microbiota-derived metabolites, such as short-chain fatty acids (SCFAs), promote homeostasis by regulating interleukin-10 (IL-10) receptor signaling [57], while specific commensal bacteria like indigenous Clostridium species promote the induction of colonic regulatory T cells (Tregs) [57].
Validating Therapeutic Targets in Disease Contexts
Humanized GF mice are a powerful platform for validating that disease-associated microbial changes are causative and for testing microbe-based therapeutics.
- Inflammatory Bowel Disease (IBD): GF mice transplanted with microbiota from IBD patients have been used to identify specific bacterial and metabolic targets. This approach has helped validate the therapeutic potential of certain Clostridium species for inducing Tregs and ameliorating colitis [57].
- Cancer Immunity: The influence of human gut microbes on cancer immunity has been elucidated using humanized gnotobiotic murine models, revealing how specific bacterial consortia can modulate responses to immunotherapy [54].
- Metabolic Disease: Studies comparing GF mice colonized with microbiota from lean versus obese donors have provided causal evidence for the role of the microbiome in energy harvest and storage, leading to the identification of specific taxa and functions that contribute to metabolic phenotypes [53] [54].
Innovations and Future Directions: Enhancing Physiological Relevance
A significant innovation in the field is the development of the TXwildling model. This approach involves transplanting the natural gut microbiota from wild mice (wildlings) into standard laboratory mice [56]. A single oral gavage is sufficient for the wildling microbiota to outcompete and replace the laboratory microbiota, resulting in a mouse model (TXwildling) with a structural and functional wildling-like microbiota [56]. This model possesses a more mature immune system with characteristics similar to adult humans, addressing a key limitation of conventional lab mice and potentially improving the reproducibility and translational success of preclinical research [56]. This model represents a significant advance for validating microbial targets in a context that more closely mirrors the complexity and resilience of a naturally co-evolved mammalian microbiome.
The human gut microbiome, a complex community of trillions of microorganisms, plays a critical role in regulating intestinal homeostasis, modulating immune responses, and influencing overall host physiology [58]. Imbalances in this microbial ecosystem, known as dysbiosis, have been associated with a wide spectrum of human diseases, including inflammatory bowel disease (IBD), metabolic disorders, autoimmune conditions, and colorectal cancer (CRC) [59] [60]. The high-dimensionality, complexity, and compositional nature of microbiome data generated by modern high-throughput sequencing technologies present significant analytical challenges that extend beyond the capabilities of traditional statistical methods [59] [61].
Artificial intelligence (AI) and machine learning (ML) have emerged as transformative approaches for deciphering complex microbiome datasets, enabling researchers to identify subtle, disease-relevant patterns and discover novel therapeutic targets [59] [60]. This technical guide explores the state-of-the-art applications of AI in microbiome analysis, with a specific focus on pattern recognition and target discovery within the context of gut microbiome-health disease associations. We provide comprehensive methodological frameworks, quantitative comparisons of analytical approaches, and visualization of core workflows to equip researchers and drug development professionals with practical tools for advancing microbiome-based healthcare.
AI-Driven Pattern Recognition in Microbial Communities
Machine Learning Approaches for Disease Classification
Machine learning algorithms excel at identifying complex, non-linear patterns in high-dimensional microbiome data that may elude conventional statistical tests. Several ML approaches have demonstrated particular utility in classifying health and disease states based on microbial signatures:
Random Forest (RF): This ensemble learning method constructs multiple decision trees during training and outputs the mode of their classes for classification tasks. RF has shown superior performance in distinguishing patients with colorectal cancer from healthy controls based on gut microbiota data, achieving a precision of 0.729 ± 0.038 and an area under the Precision-Recall curve of 0.668 ± 0.016 [58]. The algorithm's inherent feature importance metrics also help identify taxa most relevant to classification.
XGBoost (Extreme Gradient Boosting): As a more advanced implementation of gradient boosted trees, XGBoost employs sparsity-aware split finding to handle missing values effectively and utilizes regularization to prevent overfitting [58]. Optimal performance in microbiome classification tasks has been achieved with parameters including max depth ε {None, 3, 5}, col sample bytree ε {0.1-0.9}, and n estimators ε {50-250} [58].
Support Vector Machines (SVM): SVMs construct hyperplanes in high-dimensional spaces to separate different classes of samples. While effective for some microbiome classification tasks, they typically underperform compared to tree-based ensembles like RF and XGBoost for gut microbiota analysis [58].
Table 1: Performance Comparison of Machine Learning Classifiers for Colorectal Cancer Detection Using Microbiome Data
| Algorithm | Precision | Area Under Precision-Recall Curve | Key Advantages |
|---|---|---|---|
| Random Forest | 0.729 ± 0.038 | 0.668 ± 0.016 | Robust to outliers, provides feature importance metrics |
| XGBoost | Variable with parameters | Variable with parameters | Handles missing values, regularization prevents overfitting |
| Support Vector Machine | Lower than RF | Lower than RF | Effective in high-dimensional spaces |
Explainable AI for Interpretable Biomarker Discovery
The "black box" nature of complex AI models presents a significant challenge for clinical translation and biological insight. Explainable Artificial Intelligence (XAI) methods address this limitation by making model decisions transparent and interpretable [58].
SHAP (SHapley Additive exPlanations): This game theory-based approach quantifies the contribution of each feature (microbial taxon) to individual predictions [59] [58]. SHAP analysis has identified specific CRC-associated bacteria including Fusobacterium, Peptostreptococcus, and Parvimonas, whose abundance appears significantly associated with the diseased state, while also highlighting protective taxa associated with healthy controls [58].
LIME (Local Interpretable Model-agnostic Explanations): This technique approximates complex models with locally interpretable surrogates to explain individual predictions [59]. While not as computationally rigorous as SHAP, LIME provides intuitive explanations for model outputs.
The implementation of XAI frameworks enables researchers to move beyond correlation to identify potentially causal microbial features that drive disease phenotypes, thereby facilitating targeted intervention strategies [58].
Figure 1: AI and Explainable AI Workflow for Microbiome Biomarker Discovery
Target Discovery and Mechanistic Insights
Predicting Microbial Responses to Perturbations
AI models are advancing beyond static classification to predict dynamic microbial community responses to environmental perturbations, including pharmaceutical interventions. Recent research demonstrates that common medications reshape the gut microbiome in predictable ways primarily through nutrient competition dynamics [7].
Nutrient Competition Models: When medications reduce certain bacterial populations, they alter nutrient availability, creating competitive advantages for bacteria best able to capitalize on these changes [7]. Stanford researchers developed computer models that accurately predict microbial community responses to drugs by factoring in both the sensitivity of different bacterial species to specific medications and the competitive landscape for nutritional resources [7].
Ecological Forecasting: This framework models drugs as ecosystem perturbations rather than simple antimicrobial agents, enabling prediction of winner and loser taxa following treatment based on understanding of ecological principles [7]. This approach has revealed that 141 of 707 clinically relevant drugs significantly alter microbiome composition, with some short-term treatments creating enduring changes by entirely eliminating specific microbial species [7].
Bacteriophage-Based Therapeutic Targeting
The viral component of the gut microbiome represents a promising frontier for targeted therapeutic interventions. Recent discoveries of hundreds previously unknown bacteriophages (viruses that infect bacteria) living inside gut bacteria have opened new paths for microbiome medicine [62].
Phage Activation Mechanisms: Research has identified that specific compounds, including the sugar substitute Stevia and molecules released by human gut cells, serve as potent activators for temperate bacteriophages in the gut [62]. When exposed to human gut cells, the activation rate of dormant viruses increases significantly, suggesting human biology actively shapes the gut viral landscape [62].
CRISPR-Based Engineering: Scientists have utilized CRISPR technology to identify mutations in viral genes that prevent activation, providing insights into how some gut viruses become permanently dormant [62]. This knowledge enables the engineering of probiotic strains with tailored viral functions and the development of precision phage therapies for conditions including inflammatory bowel disease and cancer [62].
Table 2: Omics Technologies for Microbiome Analysis and Their Applications in AI-Driven Research
| Technology | Benefits | Limitations | AI Applications |
|---|---|---|---|
| 16S rRNA Profiling | High sensitivity for microbial identification, cost-effective | Limited taxonomic resolution, PCR amplification biases | Disease classification, community dynamics analysis |
| Shotgun Metagenomics | Species- and strain-level classification, functional insights | Reference database dependency, computational intensity | Strain-level biomarker discovery, functional pathway analysis |
| Metatranscriptomics | Insights into functional gene expression | mRNA instability, analytical complexity | Identification of actively expressed pathways |
| Metabolomics | Quantifies metabolites driving interactions | Difficulty annotating unknown metabolites | Linking microbial functions to host phenotypes |
| Metaproteomics | Insights into signaling peptides | Database construction challenges, limited applications | Host-microbiome interaction mapping |
Experimental Protocols and Methodological Frameworks
Microbiome Data Preprocessing Pipeline
Robust preprocessing is essential for generating reliable AI model inputs. The following protocol outlines critical steps for preparing microbiome data for AI analysis [58]:
Taxonomic Filtering: Remove non-informative features using abundance/prevalence thresholds (e.g., features present in <10% of samples) and eliminate biologically irrelevant taxa or potential contaminants [58].
Compositional Data Normalization: Apply Aitchison's methodology for compositional data using centered log-ratio (CLR) transformation to address sampling depth variability and data sparsity [58]. This technique transforms feature counts into log-ratios within each sample, preserving relative abundance relationships.
Feature Selection: Implement variance-based filtering or correlation analysis to reduce dimensionality while preserving biologically meaningful signals [58].
Data Partitioning: Employ stratified sampling techniques during training-test splits to maintain class distribution integrity, particularly crucial for unbalanced datasets common in case-control studies [58].
Model Training and Validation Framework
A rigorous validation framework is essential for developing clinically relevant AI models:
Cross-Validation: Implement repeated stratified k-fold cross-validation (e.g., 20 repetitions of 5-fold stratification) to obtain robust performance estimates and minimize overfitting [58].
Hyperparameter Optimization: Utilize grid or random search strategies to identify optimal model parameters. For Random Forest, key parameters include number of trees (n_estimators), maximum depth, and minimum samples per leaf [58].
Multi-Study Validation: Train and validate models across independent cohorts from different geographical regions to assess generalizability and mitigate batch effects [58].
Performance Metrics: Evaluate models using clinically relevant metrics including precision, recall, area under the Precision-Recall curve (especially important for imbalanced datasets), and ROC-AUC [58].
Figure 2: Multi-Omics Data Integration and Validation Workflow
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Computational Tools for AI-Driven Microbiome Research
| Category | Specific Tools/Reagents | Function/Application | Key Considerations |
|---|---|---|---|
| Sequencing Technologies | 16S rRNA kits (V4 region), Shotgun metagenomics kits, Long-read sequencing (Oxford Nanopore, PacBio) | Microbial community profiling, strain-level resolution, functional annotation | Choice depends on resolution needs and budget; combining short and long-read technologies improves assembly quality |
| Reference Databases | Greengenes, SILVA, GTDB, HUMAnN | Taxonomic classification, functional pathway analysis | Database selection significantly impacts results; standardized databases enable cross-study comparisons |
| Bioinformatics Tools | QIIME 2, mothur, MetaPhlAn, HUMAnN | Data preprocessing, taxonomic profiling, functional inference | Pipeline choice affects downstream analysis; consistent parameters essential for reproducibility |
| AI/ML Frameworks | Scikit-learn, XGBoost, TensorFlow, PyTorch | Model development, classification, feature importance | Python ecosystem dominates; R available for specialized packages |
| XAI Libraries | SHAP, LIME, Eli5 | Model interpretation, biomarker identification | Critical for translational applications and biological insight |
| Culture Resources | Australian Microbiome Culture Collection (AusMiCC), Anaerobic chambers | Bacteriophage isolation, functional validation | Specialized growth conditions required for anaerobic gut microbes |
AI-driven microbiome analysis represents a paradigm shift in how researchers approach pattern recognition and target discovery in gut microbiome-health associations. The integration of machine learning with multi-omics data, coupled with emerging explainable AI frameworks, is accelerating the identification of clinically relevant biomarkers and therapeutic targets across a spectrum of human diseases [59] [60] [58].
Future advancements in this field will likely focus on several key areas: improved handling of longitudinal data to model temporal dynamics of microbiome ecosystems [7]; development of more sophisticated integration methods for heterogeneous multi-omics datasets [60]; implementation of federated learning approaches to overcome data privacy barriers and enable larger, more diverse cohorts [59]; and the creation of increasingly sophisticated synthetic microbial communities based on AI-derived design principles [60] [62].
As these technologies mature, AI-powered microbiome analysis will increasingly transition from research settings to clinical applications, enabling personalized therapeutic interventions based on an individual's unique microbial ecology [59] [60]. This evolution promises to unlock novel diagnostic modalities and precision medicine approaches for complex diseases linked to gut microbiome dysbiosis.
Navigating Research and Therapeutic Roadblocks in Microbiome Manipulation
Establishing causal relationships between gut microbiome alterations and disease represents a fundamental challenge in biomedical research. While numerous studies have identified associations between dysbiosis and various conditions—from inflammatory bowel disease to neurological disorders—proving that microbial changes drive disease pathology rather than merely reflecting its consequences requires sophisticated methodological approaches [63]. This conundrum lies at the heart of translating microbiome research into effective therapeutics, as drug development depends on identifying true molecular drivers of disease rather than correlated epiphenomena. The field has moved beyond simple correlation studies toward establishing causal inference through a multidisciplinary toolkit encompassing genetic epidemiology, advanced modeling, and carefully designed experimental systems.
The complexity of host-microbiome interactions creates significant challenges for causal inference. Microbiome composition is influenced by numerous confounding factors including diet, medications, genetics, and environment, making it difficult to isolate microbial effects. Furthermore, the relationship between host and microbiota is often bidirectional, with diseases potentially altering the microbiome while being influenced by it [64]. This creates a "chicken-and-egg" problem that demands specialized approaches to unravel. Overcoming these challenges requires integrating methods from multiple disciplines, including epidemiology, statistics, microbiology, and systems biology.
Analytical Frameworks for Causal Inference
Mendelian Randomization and Genetic Correlation Approaches
Mendelian Randomization has emerged as a powerful statistical technique for strengthening causal inference in microbiome research. This method uses genetic variants as instrumental variables to explore causal relationships between microbial exposures and health outcomes, helping to mitigate confounding factors and reverse causation bias [64]. MR analyses follow three core assumptions: (1) genetic variants strongly associate with the exposure (gut microbiota), (2) these variants are independent of confounders, and (3) they affect the outcome only through the exposure [64].
A comprehensive 2025 study applied both MR and Linkage Disequilibrium Score Regression to systematically investigate connections between gut microbiota, aging indicators (telomere length, frailty index, facial aging), and 14 age-related diseases [64]. The analysis revealed gut microbiota as a potential risk factor for multiple age-related conditions, with causal effects on chronic kidney disease, cirrhosis, and heart failure partially mediated by aging indicators. This approach demonstrates how genetic correlation and causal relationship analyses can identify microbial biomarkers with predictive value for disease development (average AUC = 0.731) [64].
Table 1: Causal Inference Methods in Microbiome Research
| Method | Underlying Principle | Key Applications | Strengths | Limitations |
|---|---|---|---|---|
| Mendelian Randomization | Uses genetic variants as instrumental variables | Testing causal directions in microbiome-disease relationships | Reduces confounding and reverse causation | Requires large sample sizes for robust genetic instruments |
| Linkage Disequilibrium Score Regression | Estimates genetic correlation from GWAS summary statistics | Assessing shared genetic architecture between microbiome and disease | Accounts for sample overlap; provides genetic correlation estimates | Does not establish direction of causality |
| Causal Structure Learning | Discovers causal networks from observational data | Identifying complex interaction patterns in microbial communities | Can reveal direct and indirect causal pathways | Sensitive to model assumptions; computational complexity |
Causal Discovery from Metagenomic Data
Beyond MR approaches, causal structure learning methods have shown promise for inferring causal effects directly from metagenomic data [65]. These approaches can model the complex web of interactions within microbial communities and their hosts, though they face unique challenges including compositionality, sparsity, and high dimensionality of microbiome data. Methodological advances in causal discovery over the past five years have improved the potential for data-driven prediction of causal effects in large-scale biological systems, offering new opportunities for causal reasoning in microbiome research [65].
The implementation of these methods typically begins with quality-controlled microbiome data, often represented as amplicon sequence variant (ASV) or operational taxonomic unit (OTU) tables. Analytical workflows then apply causal discovery algorithms to identify potential causal networks, which must be validated through experimental approaches. These computational methods serve as hypothesis-generating tools that can prioritize microbial taxa and functions for further mechanistic investigation.
Experimental Models for Establishing Causality
Preclinical Model Systems
Preclinical models provide essential platforms for experimentally testing causal relationships between gut microbiota and disease phenotypes. A 2025 Delphi survey by the Human Microbiome Action Consortium evaluated the utility of various model systems, generating consensus statements on their appropriate applications [63].
Table 2: Experimental Models for Host-Microbiome Interaction Research
| Model System | Key Features | Best Applications | Technical Considerations |
|---|---|---|---|
| Germ-free Animals | No resident microbiota; can be colonized with defined microbial communities | Establishing causal effects of specific microbes; microbiome reconstitution studies | Requires specialized facilities; may have immune system abnormalities |
| Human Microbiota-Associated (HMA) Mice | Germ-free mice colonized with human donor microbiota | Studying human-relevant microbial functions in controlled setting | Limited translation due to host-specific factors; diet critically important |
| Organoids | 3D cell cultures derived from stem cells that mimic organ architecture | Studying host-microbe interactions at cellular level; epithelial barrier function | Lack full microenvironment (immune, stromal, vascular components) |
| Gut-on-a-Chip | Microfluidic devices simulating physiological conditions | Real-time monitoring of cellular responses to microbial stimuli | Technical complexity; challenges maintaining stable microbial communities |
| In vitro Fermentation Systems | Controlled cultivation of human-derived fecal samples | Studying microbial metabolism and community dynamics | No host components; limited physiological relevance |
Germ-free animal models represent a cornerstone for causal inference in microbiome research. These models enable researchers to test hypotheses about specific microorganisms by introducing them into previously sterile hosts and monitoring resulting phenotypes [63]. The Delphi survey emphasized that while these models offer crucial insights, they require improved standardization and translational relevance, including the implementation of bacterial isolates of relevance to humans [63].
Human microbiota-associated mouse models have shown particular promise for bridging the gap between human association studies and mechanistic insights. By transferring fecal microbiota from healthy and diseased human donors into germ-free animals, researchers can observe whether disease-associated microbial communities can transfer phenotypic traits [63]. However, these models have limitations in fully replicating the human gut microbiome and disease pathophysiology.
Advanced Culturing Systems
Ex vivo organoid cultures derived from primary tissue or pluripotent stem cells provide a controlled environment for investigating host-microbiome interactions at the cellular level, particularly for studying epithelial barrier function, immune responses, and metabolic pathways [63]. These systems recapitulate native tissue architecture but lack key elements of the complete microenvironment, including peristalsis and full immune, stromal, and vascular components.
Organ-on-a-chip platforms have emerged as innovative tools that offer higher physiological relevance through microfluidic devices that recreate tissue-level complexity [63]. These systems enable real-time monitoring of cellular responses to microbial stimuli, barrier integrity, and drug metabolism. However, challenges remain in optimizing scaling, maintaining stable microbial communities, and replicating the full complexity of human physiology.
Analytical and Visualization Approaches
Standardized Diversity Metrics
Robust analytical methods are essential for accurately characterizing microbial communities and identifying meaningful associations. A 2025 analysis of alpha diversity metrics provided guidelines for standardized approaches to microbiome analysis [66]. The study categorized 19 metrics into four distinct groups based on their mathematical properties and biological interpretations:
- Richness metrics (Chao1, ACE, Fisher, Margalef, Menhinick, Observed, Robbins): Describe the number of microbial taxa in a sample
- Dominance metrics (Berger-Parker, Dominance, Simpson, ENSPIE, Gini, McIntosh, Strong): Reflect the evenness of species abundance distribution
- Phylogenetic metrics (Faith): Incorporate evolutionary relationships between microbes
- Information metrics (Shannon, Brillouin, Heip, Pielou): Derived from information theory, combining richness and evenness
The analysis recommended that microbiome studies include metrics from multiple categories to capture complementary aspects of microbial communities, as overreliance on a single metric may obscure biologically relevant patterns [66]. For example, the Berger-Parker index has a clear biological interpretation (the proportion of the most abundant taxa), while the Gini index does not correlate well with other dominance metrics and should be interpreted with caution.
Visual Analytics and Data Exploration
Interactive data visualization and visual analytics have become increasingly important in microbiome research, particularly for discovery-driven exploration of complex datasets [67]. These approaches facilitate hypothesis generation by enabling researchers to identify patterns, outliers, and relationships that might not be detected through purely hypothesis-driven statistical models.
Effective visualization tools for microbiome research must address multiple analytical tasks, including:
- Comparison of taxonomic abundance across samples or groups
- Assessment of alpha and beta diversity patterns
- Visualization of multivariate relationships using methods like PCoA plots
- Exploration of time-series data in longitudinal studies
- Integration of microbiome data with host metadata and omics measurements
Workshops with domain experts have identified that successful visualization tools require close collaboration between microbiome researchers and visualization specialists to ensure that analytical needs are effectively translated into visual representations [67].
From Causality to Therapeutic Applications
Microbiome-Targeted Interventions
Establishing causal relationships between gut microbes and disease opens avenues for developing targeted therapies. Recent research has explored various intervention strategies:
Probiotics and prebiotics show promise for managing gastrointestinal disorders and beyond. Clinical research presented at NeuroGASTRO 2025 demonstrated the successful translational validation of Bifidobacterium longum APC1472 for attenuating obesity-related parameters in otherwise healthy individuals with overweight/obesity [6]. Unpublished findings in mice further showed that this strain could attenuate the enduring effects of early-life high-fat high-sugar diet, including food intake dysregulation and hypothalamic molecular alterations.
Next-generation probiotics represent an emerging frontier, with potential applications including metabolic health, reducing gut inflammation in IBD, and increasing satiety [6]. These advanced microbial therapeutics face regulatory challenges but offer novel mechanisms for manipulating host physiology through the microbiome.
Bacteriophage-based therapies constitute another promising approach. A groundbreaking 2025 study discovered hundreds of previously unknown viruses living inside gut bacteria, revealing that compounds produced by human gut cells can activate dormant viruses [62]. This suggests that human biology actively shapes the viral landscape of the gut, with implications for diseases like inflammatory bowel disease where inflammation and cell death are common. Using CRISPR-based genetic engineering, researchers identified mutations in viral genes that prevent activation, offering insights for future therapeutic strategies aimed at manipulating the gut microbiome [62].
Biomarker Discovery and Personalized Approaches
Causal understanding of microbiome-disease relationships enables the development of biomarkers for disease prediction and monitoring. Microbial features identified through genetic correlation and causal relationship analyses exhibit predictive properties for disease development [64]. Integrating these microbial biomarkers with host factors significantly improves disease prediction models (increasing average AUC from 0.808 to 0.832) [64].
The emerging field of personalized microbiome interventions recognizes that individual differences in microbial community composition and function influence responses to therapies. For example, if an individual possesses gut microbes capable of converting soy isoflavones to equol, they may experience a 75% greater reduction in menopausal symptoms when supplemented with isoflavones compared to someone lacking those specific microbial species [6]. This highlights the importance of considering microbiome composition when designing nutritional and therapeutic interventions.
Integrated Workflows and Future Directions
Multi-Omics Integration
Bridging correlation and causation requires integrating multiple data types and analytical approaches. The combination of metagenomics, metatranscriptomics, metabolomics, and host omics data provides a more comprehensive understanding of microbial contributions to health and disease. For example, mining the literature to identify microbial-derived metabolites with neuroactive potential has led to the definition of 56 different gut-brain modules, each corresponding to a neuroactive compound production or degradation process [6].
Future work aims to expand these catalogs by incorporating the so-far uncultivated fraction of the human microbiome and incorporating metabolomic analyses to explore the relevance of these modules across different neuropsychiatric conditions [6]. Such integrated approaches help move beyond taxonomic associations toward functional mechanistic insights.
Consensus Guidelines and Standardization
The field is moving toward greater standardization through consensus-building efforts like the Delphi survey conducted by the Human Microbiome Action Consortium [63]. These initiatives bring together diverse stakeholders to establish best practices for model selection, methodological approaches, and analytical frameworks. Key priorities identified through these efforts include:
- Advancing biomarker discovery with robust validation pipelines
- Integrating multi-omics approaches to unravel microbiome complexity
- Addressing ethical, regulatory, and economic challenges
- Ensuring equitable access to microbiome-based diagnostics and therapies
Standardization is particularly important for clinical translation, as inconsistency in methods and analysis approaches makes it difficult to compare results across studies and build cumulative knowledge [66].
Causal Inference Workflow in Microbiome Research
Multi-Omics Integration for Causal Inference
Table 3: Essential Research Reagents and Materials for Microbiome Causal Studies
| Category | Specific Reagents/Materials | Key Applications | Technical Considerations |
|---|---|---|---|
| Model Systems | Germ-free rodent strains; Anaerobic chambers; Organoid culture kits | Establishing causal relationships in controlled systems | Requires specialized facilities and training; strict protocols for gnotobiotic experiments |
| Microbial Culturing | Australian Microbiome Culture Collection; Gifu Anaerobic Medium; Pre-reduced anaerobically sterilized media | Isolation and cultivation of human gut microbes | Most gut bacteria require anaerobic conditions; specialized preservation methods needed |
| Molecular Analysis | 16S rRNA primers; Shotgun metagenomics kits; CRISPR-Cas9 systems for bacterial engineering | Microbial community profiling and genetic manipulation | Choice of 16S region affects taxonomic resolution; DNA extraction method influences results |
| Activation Compounds | Stevia; Bile acids; Short-chain fatty acids; Neurotransmitter analogs | Inducing phage activation or microbial functional shifts | Concentration-dependent effects; host-specific responses |
| Analytical Tools | QIIME 2; DEBLUR; DADA2; Phylogenetic placement algorithms | Bioinformatic analysis of microbiome data | Pipeline choice affects ASV/OTU definition; standardization challenges across studies |
Resolving the "causality conundrum" in microbiome research requires multidisciplinary approaches that integrate computational methods with experimental validation. While significant challenges remain, emerging methodologies in causal inference, sophisticated model systems, and multi-omics integration are progressively enabling researchers to distinguish microbial drivers from disease consequences. The field is moving toward a future where microbiome-based diagnostics and therapies can be developed based on robust causal understanding rather than mere association, ultimately fulfilling the potential of microbiome science to transform human health.
In gut microbiome health and disease association research, the ability to detect true biological signals is often confounded by substantial technical variability introduced at every stage of sequencing and analysis. Next-generation sequencing (NGS) has revolutionized our capacity to study microbial communities, but the inherent flexibility of these methods has created significant challenges for data comparability and reproducibility [68]. The fundamental problem lies in the fact that differences in laboratory protocols, bioinformatic pipelines, and analytical approaches can generate variability that obscures genuine biological relationships and compromises the validity of research findings.
The particular interdisciplinary nature of human microbiome research makes organization and reporting of results spanning epidemiology, biology, bioinformatics, translational medicine, and statistics particularly challenging [69]. This challenge is especially acute in gut microbiome studies aimed at drug development, where subtle microbial signatures may serve as critical biomarkers for therapeutic efficacy or disease diagnosis. When laboratories employ different data processing pipelines, substantial differences in variant calling emerge in combined datasets, historically necessitating computationally expensive reprocessing to enable meaningful aggregation [70]. The establishment of standardized frameworks is therefore essential not only for scientific rigor but also for accelerating the translation of microbiome research into clinical applications.
Pre-analytical and Laboratory Processing Variability
Technical variability begins even before sequencing, with sample collection, preservation, and DNA extraction methods introducing significant biases. In microbiome research, these pre-analytical factors can dramatically alter the apparent composition of microbial communities. The STORMS (Strengthening The Organization and Reporting of Microbiome Studies) guidelines emphasize that because participant characteristics such as environment, lifestyle behaviors, diet, biomedical interventions, and demographics can correspond with substantial differences in the microbiome, comprehensive reporting of these variables is essential [69]. Furthermore, information about antibiotics or other treatments that could affect the microbiome must be described, as well as any exclusion criteria related to recent medication use.
During laboratory processing, batch effects represent a major source of technical variability. The evolving approaches to laboratory processing in microbiome studies come with elevated potential for batch effects that must be carefully controlled and documented [69]. Library preparation protocols, sequencing platforms, and sequencing depths all contribute to variability that can obscure true biological signals if not properly accounted for in experimental design and statistical analysis.
Bioinformatics Pipeline Variability
Once sequencing data is generated, bioinformatic processing introduces additional layers of variability. The research community has developed variant file specifications to support a broad range of research applications, but their inherent flexibility has resulted in variation among laboratories with respect to how content is represented [68]. This flexibility, while valuable for research, generates challenges for clinical applications and cross-study comparisons.
Table 1: Major Sources of Technical Variability in Microbiome Sequencing Studies
| Pipeline Stage | Sources of Variability | Impact on Results |
|---|---|---|
| Wet Lab | DNA extraction methods, PCR amplification cycles, library prep kits, sequencing platforms | Differences in microbial community representation, introduction of batch effects |
| Computational | Read trimming parameters, reference databases, alignment algorithms, clustering thresholds | Variability in taxonomic assignment, diversity estimates, and differential abundance |
| Analytical | Normalization methods, statistical approaches, contamination handling, phylogenetic methods | Altered effect sizes, false positive/negative findings, reduced reproducibility |
Several variant file formats have been established, including VCF (Variant Call Format), genomeVCF, and genome variation format (GVF) [68]. These formats were primarily generated to support research rather than clinical applications and were designed to either catalog population variations or capture deep annotation of a single personal genome. Without consistent conventions for describing sequence findings, the usefulness of data returned from database queries to identify clinically relevant variants may be compromised because the base coordinate systems may be different [68].
Frameworks and Strategies for Standardization
Establishing Functional Equivalence in Processing Pipelines
The concept of functional equivalence (FE) provides a powerful framework for addressing pipeline variability. FE is defined as a shared property of two pipelines that can be run independently on the same raw whole genome sequencing data to produce two output files that, upon analysis by the same variant caller(s), produce virtually indistinguishable genome variation maps [70]. The fundamental principle is that data processing pipelines should introduce much less variability in a single DNA sample than independent WGS replicates of DNA from the same individual.
A collaboration of major U.S. genome sequencing centers and NIH programs has defined data processing and file format standards to guide sequencing studies [70]. Notable features of their data processing standard include alignment with BWA-MEM, adoption of a standard GRCh38 reference genome with alternate loci, and improved duplicate marking. File format standards include a 4-bin base quality scheme, CRAM compression, and restricted tag usage, which in combination reduced file size more than 3-fold [70]. This approach focuses on harmonizing upstream steps prior to variant calling, thus reducing trivial variability in core pipeline components while promoting the application of diverse and complementary variant calling methods.
Standardized Reporting Frameworks for Microbiome Research
The STORMS checklist provides a comprehensive reporting framework specifically tailored to microbiome studies [69]. This 17-item checklist is organized into six sections corresponding to the typical sections of a scientific publication and includes both elements adapted from existing observational and genetic study guidelines as well as new reporting elements developed specifically for microbiome research. Of the items in the STORMS checklist, nine items or sub-items were unchanged from STROBE (Strengthening the Reporting of Observational Studies in Epidemiology), three were modified from STROBE, one was modified from STREGA (Strengthening the REporting of Genetic Association Studies), and 57 new guidelines were developed specifically for microbiome research [69].
Key reporting elements specific to microbiome studies include:
- Detailed description of body site(s) sampled and sampling procedures
- Information about antibiotics or other treatments that could affect the microbiome
- Specification of laboratory processing methods, including target gene regions for amplification
- Bioinformatics methods for processing sequence data
- Statistical methods for analyzing sparse, high-dimensional compositional data
The adoption of such standardized reporting guidelines promotes research consistency and, as a consequence, encourages reproducibility and improved study design [69].
Data Harmonization Processes and Workflows
Data harmonization is the process of standardizing and integrating data that comes in from different disparate data fields, formats, and dimensions [71]. It aims to improve the quality and usability of data and typically follows a semi-automated process involving a set of activities customized to a specific business model. For microbiome research, this process typically involves five key steps:
- Acquire: Identify relevant data sources and acquire data, creating datasets from sources such as target business documents, consumer research information, or market research information [71].
- Mapping: Create a single schema for the whole data to follow, containing all necessary fields and validations [71].
- Ingest and clean: Ingest raw data into a system, then evaluate it for integrity and validity. Identify and modify incorrect, inaccurate, or inconsistent parts of the data according to the schema [71].
- Harmonize and evaluate: Apply the defined schema to raw data to obtain harmonized data, then perform analyses to ensure the harmonized data meets quality standards with no loss in accuracy or originality [71].
- Deployment: Deploy harmonized data on the system for further processing, making it accessible across organizational teams [71].
Table 2: Key Quality Control Checkpoints in NGS Workflows
| Workflow Stage | QC Checkpoints | Recommended Metrics |
|---|---|---|
| Sample Preparation | DNA quality and quantity, contamination checks | DNA integrity number, spectrophotometric ratios, qPCR amplification efficiency |
| Library Preparation | Library concentration, size distribution, adapter contamination | Fragment analyzer profiles, qPCR quantification, molar concentration |
| Sequencing | Cluster density, phasing/prephasing, base call quality | Q-scores, error rates, percent bases above Q30 |
| Data Analysis | Read quality, alignment rates, coverage uniformity | FastQC reports, mapping percentages, duplicate rates, coverage depth |
A critical component of successful data harmonization is the implementation of common data elements (CDEs) and metadata standards. The FAIR Data Principles (Findable, Accessible, Interoperable, and Reusable) provide guidelines for improving the integration capability of openly shared datasets [72]. A FAIR dataset should include all information necessary to understand and interact with the data, including detailed descriptions of how the data was generated, study design, experimental conditions, and sample processing metadata [72].
Experimental Protocols for Standardization and Validation
Protocol: Establishing Functional Equivalence Between Pipelines
To establish functional equivalence between different bioinformatics pipelines, researchers can implement the following experimental protocol, adapted from the approach used by major sequencing centers [70]:
Select a reference dataset: Obtain a set of well-characterized genomes with diverse ancestry, including independently sequenced replicates of reference materials such as NA12878 (CEPH) and NA19238 (Yoruban). The 14-genome test set used in the FE validation included four independently-sequenced replicates of NA12878 and two replicates of NA19238 [70].
Process data through multiple pipelines: Run the same raw sequencing data through each of the pipelines being evaluated, using fixed variant calling software and parameters to isolate the effects of alignment and read processing on variant calling. In the FE study, researchers used GATK for single nucleotide variants (SNVs) and small insertion/deletion (indel) variants, and LUMPY for structural variants (SVs) [70].
Quantify pairwise variability: Calculate pairwise variability in SNV, indel, and SV callsets generated separately from each pipeline. Compare this variability to that between WGS data replicates. In validated FE pipelines, variability between harmonized pipelines (mean 0.4%, 1.8%, and 1.1% discordant for SNVs, indels, and SVs, respectively) should be an order of magnitude lower than between replicate WGS datasets (mean 7.1, 24.0, and 39.9% discordant) [70].
Validate with Mendelian inheritance patterns: Apply the pipelines to family-based genome sets (trios or quads) and assess Mendelian error rates. In the FE study, researchers used 100 genomes comprising 8 trios from the 1000 Genomes Project and 19 quads from the Simons Simplex Collection [70].
Assess region-specific performance: Evaluate concordance rates in high-confidence genomic regions versus difficult-to-assess regions laden with segmental duplications and high copy repeats. The FE study found that 58% of discordant SNV calls were found in the 8.5% most difficult-to-analyze subset of the genome [70].
Protocol: Validation of Sequencing Workflows for Clinical Applications
For laboratories implementing sequencing workflows for clinical applications, including microbiome-based diagnostics, the following validation protocol based on established guidelines is recommended:
Determine accuracy: Analyze a minimum of 50 samples composed of different material types, comparing results to a gold standard reference. Accuracy in NGS assays is based on depth of coverage and quantity of reads associated with a respective base call [73].
Assess robustness: Evaluate the likelihood of assay success across different sample types and conditions.
Establish precision: Determine both repeatability (ability to return identical results under identical conditions) and reproducibility (ability to return identical results under changed conditions). This requires sequencing the same reference sequence several times under the same conditions for repeatability, and processing the upstream pipeline in multiple laboratories using different devices for reproducibility [73].
Calculate sensitivity and specificity: Determine positive and negative percent agreement compared to a gold standard method.
Define reportable and reference ranges: Establish the boundaries for normal and abnormal results based on the validated performance characteristics [73].
Sequencing Workflow Quality Control Pipeline
Visualization and Analysis of Standardized Microbiome Data
Selecting Appropriate Visualizations for Microbiome Data
Microbiome data presents unique visualization challenges due to its high dimensionality, sparsity, and compositional nature [61]. Selecting the appropriate visualization method depends on the type of analysis being performed and whether the focus is on individual samples or group comparisons:
- Alpha diversity (within-sample diversity): For comparing all samples, use scatterplots; for comparing groups, box plots with jitters (non-overlapping individual data points) are more appropriate [61].
- Beta diversity (between-sample diversity): For examining overall variation between groups, ordination plots such as Principal Coordinates Analysis (PCoA) are ideal. For comparing individual samples, dendrograms or heatmaps may be better [61].
- Relative abundance: For comparing groups, bar charts or pie charts can be effective. For comparing all samples, heatmaps work better [61].
- Differential abundance: Between-group comparisons are best visualized with bar graphs showing effect sizes.
- Core taxa: For defining core taxa across groups and samples, UpSet plots are more effective than Venn diagrams, especially when comparing four or more groups [61].
- Microbial interactions: Network analysis plots or correlograms effectively display correlations between different microbial features.
Optimizing Visualizations for Readability and Impact
After selecting the appropriate visualization type, optimizing the figure for clarity and impact is essential [61]. Key considerations include:
- Adding informative titles: Include the type of analysis and comparison being made, keeping titles informative but concise.
- Proper labeling: Ensure x- and y-axes are labeled correctly with appropriate scales. Label outliers or important features, but avoid labeling all samples with large sample numbers.
- Color selection: Use consistent colors for the same categories across multiple graphs in a publication or report. When using more than seven colors, consider alternative graph types. Use color-blind friendly palettes like viridis [61].
- Data ordering: Reorder categorical variables by median, number of observations, or other relevant parameters rather than accepting default alphabetical sorting.
- Faceting: Split graphs into groups (faceting) to highlight important patterns while retaining all information.
Microbiome Visualization Selection Framework
Implementation Tools and Quality Management
Table 3: Research Reagent Solutions for Standardized Microbiome Analysis
| Resource Category | Specific Tools/Standards | Function and Application |
|---|---|---|
| Reporting Standards | STORMS checklist, MIxS standards, FAIR Principles | Ensure complete reporting of methods and metadata for reproducibility and data integration |
| Bioinformatics Pipelines | VCF specification, BWA-MEM alignment, GRCh38 reference | Provide standardized methods for data processing and variant calling to enable data harmonization |
| Quality Control Tools | FastQC, MultiQC, Bioanalyzer, qPCR assays | Assess quality at each stage of the workflow from sample preparation to final data output |
| Reference Materials | Genome in a Bottle (GIAB) references, mock microbial communities | Enable validation and performance monitoring across laboratories and platforms |
| Data Visualization | R packages (ggplot2, phyloseq, UpSetR), PCoA plots | Facilitate appropriate representation and interpretation of complex microbiome data |
Quality Management and Documentation Systems
Implementing robust quality management systems is essential for maintaining standardization in sequencing and analysis pipelines. Key components include:
Technical Notes (TN): Acting as preventive quality assurance methods, TNs serve as inspection records that accompany samples through the entire workflow. After project completion, the TN represents a quality certificate for delivery [73].
Laboratory accreditation checklists: The College of American Pathologist's (CAP) NGS Work Group developed 18 laboratory accreditation checklist requirements for upstream analytic processes and downstream bioinformatics solutions for NGS in clinical applications [73]. These requirements include standards for documentation, validation, quality assurance, confirmatory testing, exception logs, monitoring of upgrades, variant interpretation and reporting, incidental findings, data storage, version traceability, and data transfer confidentiality.
Standard Operating Procedures (SOPs): Development and adherence to detailed SOPs for each stage of the sequencing workflow, including sample evaluation, fragmentation, library assessment, sequencing monitoring, and raw data analysis [73].
Quality records: Comprehensive documentation providing verifiable origin of sequencing data, including used devices, reagent lot numbers, and any deviation from standard procedures [73].
Addressing technical variability in sequencing and analysis pipelines through standardization is not merely an academic exercise—it is a fundamental requirement for advancing our understanding of gut microbiome health and disease associations. The frameworks, protocols, and tools outlined in this technical guide provide a roadmap for researchers to enhance the reproducibility, comparability, and translational potential of their microbiome studies. As the field moves toward clinical applications and precision medicine approaches, the implementation of these standardization practices will become increasingly critical for generating reliable, actionable insights from microbiome research.
By adopting functional equivalence standards, implementing comprehensive data harmonization workflows, utilizing appropriate visualization methods, and maintaining rigorous quality management systems, researchers can overcome the significant hurdles posed by technical variability. This will ultimately accelerate the discovery of robust microbiome-disease associations and facilitate the development of novel microbiome-based diagnostics and therapeutics.
The prevailing scientific narrative has predominantly highlighted antibiotics as the primary pharmaceutical disruptors of the gut microbiome. However, emerging research underscores that a broad spectrum of common non-antibiotic drugs induces predictable and often persistent alterations in gut microbial communities. The gut microbiome, a complex ecosystem of trillions of microorganisms, is integral to host metabolism, immune function, and overall health [74]. Dysbiosis, an imbalance in this community, is linked to a wide array of diseases, including gastrointestinal disorders, metabolic syndromes, neurological conditions, and cardiovascular diseases [74] [75] [76]. This whitepaper synthesizes recent evidence demonstrating that medications beyond antibiotics, including antidepressants, beta-blockers, and proton pump inhibitors, significantly reshape the gut ecosystem. By framing these findings within a broader thesis on gut-health disease associations, we reveal that drug-induced microbiome disruption follows discernible ecological rules, primarily driven by competition for nutrients and resource reshuffling [7]. This paradigm shift opens new avenues for predictive modeling, personalized medicine, and the development of gut-healthy therapeutic strategies.
Quantitative Evidence of Drug-Induced Microbiome Alteration
Large-scale clinical and preclinical studies have systematically documented the impact of diverse drug classes on gut microbiome composition and function. The quantitative data summarized in the table below provides a comparative overview of these effects.
Table 1: Documented Effects of Non-Antibiotic Drugs on the Gut Microbiome
| Drug Class | Specific Drug(s) Studied | Key Microbiome Changes | Persistence of Effects | Proposed Primary Mechanism |
|---|---|---|---|---|
| Antidepressants | Selective Serotonin Reuptake Inhibitors (SSRIs) [77] | Distinct microbial "fingerprint"; altered community structure [77] | Lasting changes observed years after use [77] | Direct inhibition and nutrient competition [7] |
| Beta-Blockers | Not Specified | Distinct microbial "fingerprint" [77] | Lasting changes observed years after use [77] | Not Specified |
| Proton Pump Inhibitors | Pantoprazole [77] [78] | Altered microbiome composition; increased infection risk [77] [78] | Persistent effects confirmed [77] | Not Specified |
| Benzodiazepines | Diazepam, Alprazolam [77] | Alterations similar to broad-spectrum antibiotics; variation between drugs in the same class [77] | Lasting changes observed years after use [77] | Not Specified |
| Cardiac Glycoside | Digoxin [78] | Selective reduction of specific microbial species; loss of colonization resistance [78] | Not Specified | Host-mediated: triggers release of antimicrobial proteins into the gut [78] |
| Antipsychotic | Quetiapine [78] | Altered composition; increased pathogen infection risk [78] | Not Specified | Not Specified |
The evidence for these long-term changes comes from significant research efforts. A study of over 2,500 individuals in the Estonian Biobank found that past use of many common drugs was a "surprisingly strong factor in explaining individual microbiome differences," with effects lingering years or even decades after treatment ceased [77]. Notably, the same study found that drugs within the same class, such as the benzodiazepines diazepam and alprazolam, can vary in their disruptive impact, highlighting the need for precision in understanding drug effects [77].
Mechanisms of Action: Ecological and Molecular Pathways
The disruption caused by non-antibiotic drugs is not random but follows predictable ecological patterns. Research indicates that the primary force behind community response is competition for nutrients [7].
Nutrient Competition as an Ecological Driver
When a medication inhibits susceptible bacterial species, it alters the availability of nutrients in the gut environment. The bacteria that are most capable of capitalizing on these newly available resources thrive, leading to a reshuffling of the microbial community structure [7]. This can be conceptualized as the drug altering the "buffet" in our gut, and the ensuing competition for food shapes the final winners and losers [7].
Host-Mediated Mechanisms
An alternative mechanism was identified for the heart failure drug digoxin. Instead of directly targeting bacteria, digoxin triggers a host biological pathway that causes the release of antimicrobial proteins into the small intestine [78]. These proteins selectively target a small number of microbial species, but their elimination has an enormous impact, as it depletes key species that keep the immune system on alert, thereby increasing susceptibility to pathogens like Salmonella [78].
The following diagram illustrates the two primary mechanisms by which non-antibiotic drugs disrupt the gut microbiome.
Experimental Protocols for Microbiome-Drug Interaction Research
To generate the data discussed herein, researchers employ sophisticated experimental workflows that combine in vitro systems, animal models, and human population studies.
In Vitro Culturing and Screening
The Stanford team developed a protocol using complex microbial communities derived from human fecal samples to systematically test drug effects [7].
- Sample Preparation: Fecal samples from healthy donors are collected and processed under anaerobic conditions to preserve the viability of obligate anaerobic bacteria.
- Culturing: The microbial communities are cultured in a controlled environment that mimics the gut.
- Drug Exposure: These communities are systematically exposed to a library of hundreds of clinically relevant drugs.
- Multi-Modal Analysis: Post-treatment, the following analyses are performed:
- Growth Metrics: Changes in the growth of individual bacterial species are measured.
- Community Composition: 16S rRNA gene sequencing or shotgun metagenomic sequencing is used to track shifts in the overall microbial population structure.
- Metabolomics: The mix of small molecules (metabolomes) produced and consumed by the microbes is analyzed to understand functional changes.
- Computational Modeling: The data on species' drug sensitivity and nutrient competition networks are integrated into predictive computational models [7].
Animal Model Validation
The Yale study utilized a mouse model to confirm drug-microbiome interactions identified from epidemiological data [78].
- Hypothesis Generation: Analysis of medical records from a million individuals identified prescription drugs associated with an increased risk of GI infection, a proxy for microbiome disruption.
- In Vivo Dosing: Mice are treated with the candidate drugs (e.g., digoxin, pantoprazole) over a defined period.
- Longitudinal Sampling: Fecal samples are collected from the mice before, during, and after drug treatment.
- Microbiome Analysis: Sequencing of fecal DNA is used to monitor changes in the composition of the gut microbiota.
- Pathogen Challenge: To assess functional consequences, mice are exposed to a pathogen like Salmonella to test if drug pre-treatment increases susceptibility to infection.
- Humanized Model: To validate findings, experiments are repeated in mice colonized with human gut microbes [78].
The workflow below integrates these methodologies into a cohesive pipeline for identifying and validating microbiome-active drugs.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Research into drug-microbiome interactions relies on a specific set of reagents, tools, and methodologies. The following table details key resources used in the featured experiments.
Table 2: Key Research Reagents and Methodologies for Microbiome-Drug Studies
| Reagent / Solution / Method | Function in Research |
|---|---|
| Donor Fecal Samples | Serves as a source of complex, human-derived microbial communities for in vitro culturing and transplantation into humanized mouse models [7] [78]. |
| Defined Drug Libraries | A curated collection of clinically relevant pharmaceuticals used for systematic high-throughput screening against microbial communities [7]. |
| Anaerobic Chamber | Provides an oxygen-free environment essential for the cultivation and manipulation of obligate anaerobic gut bacteria, preserving community viability [7]. |
| Shotgun Metagenomic Sequencing | Enables comprehensive profiling of all microbial DNA in a sample, allowing for strain-level identification and functional gene analysis beyond 16S rRNA [7] [75]. |
| 16S rRNA Gene Sequencing | A cost-effective method for profiling the bacterial composition of a community and tracking broad shifts in taxonomy following drug treatment [7] [79]. |
| Mass Spectrometry | Used in metabolomic analyses to identify and quantify small-molecule metabolites (the metabolome) produced by the microbiome in response to drugs [7]. |
| Gnotobiotic Mice | Germ-free mice that can be colonized with defined microbial communities, allowing for controlled studies of cause and effect in a complex living host [78]. |
| AI-Based Docking Models (e.g., DiffDock) | Computational tools that predict how a small molecule (like a drug) binds to a bacterial protein target, rapidly generating testable hypotheses for mechanism of action [80]. |
Discussion and Future Directions in Microbiome-Targeted Therapeutics
The predictable nature of drug-induced microbiome disruption provides a foundational framework for designing next-generation therapeutic strategies. The goal is shifting from simply treating disease to also preserving or restoring a healthy microbiome ecosystem.
Predictive Modeling and Personalized Medicine
The finding that disruption follows ecological rules enables the creation of computational models that factor in an individual's microbiome composition, diet, and medication history to predict personal susceptibility to drug side effects [7] [77]. This paves the way for personalized drug selection and dosing.
Adjunctive Therapies
Understanding these mechanisms opens the door to interventions that mitigate negative effects. These could include co-administering prebiotic nutrients to support susceptible beneficial bacteria, specific probiotics to replenish lost taxa, or even "rescue" molecules that block the drug's off-target effects on microbes [7].
Precision Antimicrobials
The use of AI to identify narrow-spectrum compounds, like enterololin, represents a paradigm shift in antibiotic development [80]. This approach aims to precisely target pathogens while minimizing collateral damage to the commensal microbiome, potentially revolutionizing treatment for conditions like Crohn's disease and combating antimicrobial resistance.
In conclusion, viewing non-antibiotic drugs as predictable modifiers of the gut ecosystem transforms our understanding of pharmacology. Integrating microbiome health into drug development and treatment regimens promises to improve therapeutic outcomes and open new frontiers in precision medicine.
Engraftment failure represents a significant bottleneck in the development of effective microbiome-based therapeutics. This technical guide synthesizes current scientific understanding of the biological mechanisms governing microbial persistence and provides a comprehensive framework of advanced strategies to overcome colonization barriers. Within the broader context of gut microbiome-health disease association research, we examine how microbial ecology, host factors, and technological innovations intersect to determine engraftment success. The whitepaper details cutting-edge methodologies from engineered control systems to pharmacological modeling of live biotherapeutic products, providing researchers and drug development professionals with actionable experimental protocols and analytical tools to advance the field of microbiome therapeutics.
The human gut microbiome constitutes a complex ecosystem comprising bacteria, archaea, fungi, viruses, and other microorganisms that collectively encode over 3 million genes—far exceeding the human genome [21]. This microbial community plays pivotal roles in nutrient metabolism, immune system maturation, and host physiology through multiple biochemical pathways [21]. Within this framework, engraftment failure describes the inability of administered beneficial microbes to establish sustained colonization within the gut ecosystem, significantly limiting the efficacy of microbiome-based interventions.
Research on gut microbiome-disease associations has revealed that successful microbial engraftment is governed by a complex interplay of factors including microbial competition, host immune responses, environmental conditions, and nutrient availability [81] [21]. The gastrointestinal tract presents numerous ecological barriers to incoming microbes, including competition with established residents, host immune surveillance, and varying physicochemical conditions throughout different gut regions. Understanding and overcoming these barriers is essential for advancing microbiome therapeutics from proof-of-concept to clinical application.
This technical guide examines the mechanisms underlying engraftment failure and provides evidence-based strategies to enhance microbial persistence, with particular emphasis on applications within disease contexts where microbiome manipulation shows therapeutic promise. The strategies discussed herein integrate insights from microbial ecology, immunology, bioengineering, and computational biology to provide a multidisciplinary approach to this fundamental challenge.
Mechanisms of Engraftment Failure
Ecological Barriers to Engraftment
The gut microbiome represents a highly competitive environment where established microbial communities resist colonization by newcomers through multiple mechanisms:
Niche Occupation: Resident microbes utilize available nutrients and occupy physical adhesion sites, creating resource limitation for incoming therapeutic strains [81]. The concept of "microbial niche" encompasses both metabolic requirements and spatial considerations within the gastrointestinal tract.
Microbial Antagonism: Commensal organisms produce bacteriocins, short-chain fatty acids, and other antimicrobial compounds that inhibit the growth of competing strains [81] [21]. This represents a natural defense mechanism against newcomers.
Priority Effects: Early colonizing species can create ecological trajectories that are resistant to change, making established gut communities particularly resilient to modification [81].
The compositional complexity of native gut microbiota, rather than being a limitation, is increasingly recognized as a feature that enables adaptation and resilience to environmental changes and insults [81]. Studies comparing defined microbial consortia versus complete donor-derived communities (as in fecal microbiota transplantation) suggest that diverse communities may provide functional stability that simple consortia lack [81].
Host-Derived Barriers
The host contributes multiple mechanisms that limit microbial engraftment:
Immune Surveillance: The intestinal immune system continuously monitors and regulates the gut microbiota, eliminating microorganisms that trigger inflammatory responses [82] [83]. Pattern recognition receptors (TLRs, NLRs) on host cells detect microbial-associated molecular patterns, initiating immune responses against newcomers.
Mucosal Barrier Function: Intestinal epithelial cells form a physical barrier through tight junctions, separating the intestinal lumen from host tissues [82]. Goblet cells secrete mucins that create a viscous barrier largely impermeable to most bacteria, while Paneth cells secrete antimicrobial peptides (α-defensins, REG3α) that directly inhibit microbial growth [82].
Bile Acid Metabolism: Host-produced bile acids possess antimicrobial properties that can inhibit engraftment of sensitive strains, particularly before they undergo host-mediated structural modifications [81].
Table 1: Primary Mechanisms of Engraftment Failure
| Barrier Category | Specific Mechanism | Impact on Engraftment |
|---|---|---|
| Ecological | Nutrient competition | Limits energy sources and building blocks for new microbes |
| Spatial exclusion | Prevents access to adhesion sites and optimal microenvironments | |
| Microbial antagonism | Direct inhibition via antimicrobial compounds | |
| Host-Derived | Immune clearance | Elimination of newcomers by host defense mechanisms |
| Mucosal barriers | Physical separation from epithelium and host tissues | |
| Bile acid toxicity | Chemical inhibition of microbial growth | |
| Environmental | Antibiotic exposure | Non-selective reduction of microbial populations |
| Dietary variations | Fluctuations in nutrient availability | |
| Inflammation | Alteration of gut environment and immune activity |
Pharmacokinetic Framework for Microbial Engraftment
Traditional pharmacological parameters (Absorption, Distribution, Metabolism, Excretion) provide a poor fit for characterizing live biotherapeutic products [81]. For microbiome-based therapeutics, a modified framework termed EMDA more appropriately describes their pharmacokinetics:
- Engraftment: The initial colonization and establishment of administered microbes within the gastrointestinal tract.
- Metagenome: The introduction of new functional genetic elements and their potential horizontal transfer to resident microbes.
- Distribution: The spatial localization of therapeutic microbes within different gastrointestinal regions and microenvironments.
- Adaptation: The evolutionary changes in both therapeutic and resident microbes in response to new selective pressures.
This conceptual framework mirrors classic ADME parameters while accounting for the unique properties of living therapeutics [81]. The EMDA framework provides a more comprehensive description of the fate of live biotherapeutic products in the body, encompassing both community-level and strain-level dynamics.
Diagram 1: Pharmacokinetic framework comparison: traditional ADME vs. microbial EMDA
Advanced Strategies to Enhance Engraftment
Nutritional Support and Niche Creation
Providing selective nutritional advantages represents a powerful strategy to enhance engraftment:
Prebiotic Supplementation: Administration of non-digestible carbohydrates that selectively stimulate growth of beneficial microbes. Psyllium and inulin-type fructans have demonstrated efficacy in clinical studies [6]. These compounds resist host digestion and become available for microbial utilization in the distal gut.
Privileged Nutrient Systems: Engineering strains to utilize novel dietary substrates not metabolized by resident microbes. The porphyran utilization system represents a sophisticated example where engineered bacteria utilize seaweed-derived polysaccharides unavailable to other gut microbes [84].
Synergistic Nutrient Formulations: Combining multiple complementary nutrient sources to support different aspects of microbial metabolism and growth requirements. Studies show that fermentable fibers can be combined with modified fiber gels (methylcellulose, psyllium) to alter the rate of colonic gas production and improve tolerance [6].
Table 2: Nutritional Support Strategies for Enhanced Engraftment
| Strategy | Mechanism of Action | Evidence Level | Key Considerations |
|---|---|---|---|
| Prebiotics | Selective growth stimulation | Clinical studies [6] | Requires compatibility with therapeutic strain metabolism |
| Privileged Nutrients | Creation of exclusive nutritional niche | Preclinical validation [84] | Requires dietary control and strain engineering |
| Synbiotic Formulations | Combined probiotic-prebiotic approach | Mixed clinical results [6] | Optimal pairing is strain-specific |
| Dietary Pattern Modulation | Holistic modification of gut environment | Epidemiological support [21] | Complex implementation; multiple confounding factors |
Microbial Community Engineering
Rather than introducing single strains, engineering complete microbial communities may enhance overall persistence:
Strain Co-operation: Designing consortia where different strains provide complementary functions or cross-feeding relationships, creating stabilized ecological networks [81].
Donor Selection: Utilizing donors with high microbial diversity may provide more complete functional guilds. Studies show that pooled donations from multiple donors allow for greater consistency in relative abundances among major bacterial taxa and ensure presence of desired microbial groups [81].
Ecological Succession Planning: Introducing strains in specific sequences to mimic natural colonization patterns, potentially bypassing priority effects that limit simultaneous introduction of multiple new strains.
Interestingly, although the microbial richness of FMT preparations made from pooled donations is very high, it quickly becomes comparable to the level measured in individual donors, suggesting severe ecological and physiological constraints on microbial diversity in the human gut [81]. This observation highlights the importance of understanding the carrying capacity and competitive exclusion principles governing the gut ecosystem.
Engineered Control Systems
Recent advances in synthetic biology have enabled development of microbial strains with precisely controlled persistence:
Reversible Engraftment System
A groundbreaking approach published in 2025 demonstrates a two-component system for controlling bacterial engraftment [84]:
Molecular Mechanism: The system involves engineering bacteria to become dependent on porphyran—a seaweed-derived polysaccharide—for survival by placing an essential gene (arginyl-tRNA synthetase) under a porphyran-inducible promoter [84]. This creates a bacterial strain that requires dietary porphyran for survival.
Experimental Workflow:
- Strain Engineering: Introduction of porphyran utilization genes and essential gene regulatory elements
- In Vitro Validation: Confirmation of porphyran-dependent growth and survival
- Animal Testing: Assessment of engraftment and clearance in humanized mice
- Therapeutic Application: Engineering of the controlled strain to express therapeutic functions (e.g., oxalate degradation pathway)
Performance Metrics: In a hyperoxaluria model, the reversibly engrafting strain (NB1000S) reduced oxalate in urine by approximately 50% in rats. After 4 weeks, removing porphyran from the diet cleared NB1000S in five of eight mice [84], demonstrating controllable reversal of engraftment.
Diagram 2: Molecular mechanism of reversible engraftment control system
Analytical Methods for Engraftment Assessment
Tracking and Quantification Methods
Accurate measurement of microbial engraftment requires sophisticated molecular and computational approaches:
Metagenomic Sequencing: Whole-genome shotgun sequencing provides strain-level resolution and functional potential assessment. The MAGEnTa pipeline represents a cost-efficient analytic tool that uses metagenome-assembled genomes directly from donor and pre-treatment metagenomic data, without relying on an external database [81].
Strain-Level Tracking: Single-nucleotide variant analysis and strain-specific marker genes enable precise discrimination between therapeutic and resident strains of the same species [81].
Longitudinal Sampling: Multiple timepoint collection allows for dynamics assessment rather than single snapshot measurements, providing insights into colonization stability.
The current approaches for characterizing FMT pharmacokinetics center on three major features: Community Coalescence (merging of donor and recipient communities), Indicator Feature tracking (monitoring specific taxonomic or functional markers), and long-term Resilience (stability of the newly formed community) [81].
Functional Engraftment Assessment
Beyond taxonomic presence, functional integration represents the ultimate goal of engraftment:
- Metatranscriptomics: RNA sequencing reveals actively expressed functions rather than simply present genes.
- Metabolomic Profiling: Measurement of microbial-derived metabolites (SCFAs, bile acids, neurotransmitters) indicates functional output of engrafted communities.
- Host Response Monitoring: Assessment of host markers (inflammatory cytokines, barrier function indicators) provides indirect evidence of functional microbial integration.
These functional assessments are particularly important as studies reveal that taxonomic presence does not always correlate with functional activity, and that microbial communities may exhibit functional redundancy where different species perform similar metabolic roles.
Table 3: Analytical Methods for Engraftment Assessment
| Method Type | Specific Technique | Information Provided | Limitations |
|---|---|---|---|
| Taxonomic | 16S rRNA sequencing | Community composition, diversity | Limited resolution, no functional data |
| Metagenomic sequencing | Strain-level identification, functional potential | Computational complexity, cost | |
| Strain-Level | SNV analysis | Strain discrimination, population dynamics | Requires reference genomes |
| Marker gene tracking | Specific strain monitoring | Limited to known markers | |
| Functional | Metatranscriptomics | Gene expression patterns | RNA stability, technical variability |
| Metabolomics | Metabolic output, host-microbe interactions | Cannot always trace metabolites to source | |
| Spatial | Fluorescence in situ hybridization | Microbial localization | Limited throughput, gut accessibility |
Research Reagent Solutions
Table 4: Essential Research Reagents for Engraftment Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Culture Media | Gifu Anaerobic Medium | Cultivation of anaerobic gut species | Requires anaerobic chamber |
| Porphyran-supplemented media | Selection of engineered strains | Purity and source of porphyran critical | |
| Molecular Tools | Porphyran-inducible promoters | Controlled gene expression | Leakiness must be minimized |
| Essential gene knockouts | Creating auxotrophic strains | Conditional lethality required | |
| Sequencing Kits | Metagenomic library prep | Community composition analysis | Bias in fragmentation and amplification |
| 16S rRNA amplification primers | Taxonomic profiling | Variable region selection affects resolution | |
| Animal Models | Humanized mice | In vivo engraftment testing | Human microbiome transfer required |
| Germ-free animals | Controlled colonization studies | Extensive facility requirements | |
| Bioinformatics Tools | MAGEnTa pipeline | Strain tracking without reference databases | Requires computational expertise |
| Phylogenetic analysis software | Evolutionary relationship determination | Algorithm selection affects results |
Overcoming engraftment failure requires a multidisciplinary approach integrating microbial ecology, synthetic biology, computational modeling, and clinical translation. The strategies outlined in this technical guide—from nutritional support and community engineering to controllable persistence systems—provide a roadmap for enhancing microbial engraftment in therapeutic contexts. As the field advances, the development of standardized assessment methods and robust analytical frameworks will be crucial for comparing results across studies and building cumulative knowledge. The reversible engraftment system represents a particularly promising direction, offering precise control over therapeutic microbial persistence. By addressing the fundamental challenge of engraftment failure, researchers can unlock the full potential of microbiome-based therapeutics for a wide range of diseases linked to microbial dysbiosis.
The escalating crisis of antimicrobial resistance (AMR), responsible for over 1 million global deaths annually, necessitates a paradigm shift from broad-spectrum antibiotic use toward precise, ecological targeting strategies [85]. The gut microbiome, a critical mediator of human health and disease, presents both a target for these novel interventions and a reason for their adoption. This whitepaper details the therapeutic potential and technical application of two such ecological agents: bacteriophages (phages) and bacteriocins. Phages, viruses that specifically infect and lyse bacteria, can be evolutionarily guided to overcome resistance [85]. Bacteriocins, ribosomally synthesized antimicrobial peptides, offer targeted activity against pathogens with minimal disruption to commensal microbes [86] [87]. Framed within gut microbiome-disease association research, this document provides a technical guide for researchers and drug development professionals, encompassing mechanisms of action, quantitative efficacy data, detailed experimental protocols, and visualization of critical pathways.
The human gut microbiome is a complex ecosystem whose dysbiosis is increasingly linked to a spectrum of age-related diseases, inflammatory conditions, and metabolic disorders [88]. Conventional broad-spectrum antibiotics, while life-saving, often exacerbate this dysbiosis by indiscriminately eliminating beneficial commensals alongside pathogens, thereby compromising colonization resistance and potentially accelerating the onset of chronic diseases [7]. Ecological targeting aims to supplant or augment these blunt instruments with precision tools that selectively remove pathogenic or pathobiont strains while preserving the integrity of the microbial community.
This approach is supported by causal inference studies linking specific gut microbial features to host physiology. For instance, Mendelian randomization has identified replicable causal relationships between gut microbial characteristics and levels of inflammatory and cardiometabolic proteins like ApoM, as well as disease risk for conditions such as age-related macular degeneration [88]. These findings illuminate precise therapeutic targets for phage and bacteriocin interventions, moving beyond correlation to causality.
Bacteriophages: Precision-Guided Evolvable Therapeutics
Mechanisms of Action and Bacterial Resistance
Phages initiate infection through highly specific molecular interactions between their receptor-binding proteins (RBPs) and bacterial surface structures, such as outer membrane proteins, lipopolysaccharides (LPS), pili, or flagella [85]. This specificity is the foundation of ecological targeting. The subsequent lytic cycle leads to bacterial cell death and the release of new phage progeny.
Bacteria deploy multiple defense mechanisms, outlined in Table 1, which phages can counter through co-evolution. Critically, bacterial resistance to phages often incurs fitness trade-offs, such as restored antibiotic susceptibility or reduced virulence, which can be therapeutically exploited [85].
Table 1: Bacterial Resistance Mechanisms and Corresponding Phage Adaptations
| Bacterial Resistance Mechanism | Description | Phage Adaptive Response |
|---|---|---|
| Surface Receptor Modification | Alteration or loss of phage-binding receptors (e.g., LPS, outer membrane proteins) [85]. | Mutation of tail fibers or baseplate proteins to recognize modified or alternative receptors [85]. |
| CRISPR-Cas Immune Systems | Sequence-specific acquisition and cleavage of invasive phage DNA [85]. | Evolution of anti-CRISPR proteins or genome sequence modifications to evade targeting [85]. |
| Restriction-Modification Systems | Cleavage of non-host methylated foreign DNA at specific sites [85]. | Phage DNA methylation or mutation of restriction enzyme recognition sites [85]. |
| Biofilm Formation | Production of extracellular polymeric substances (EPS) that shield cells and receptors [85]. | Production of depolymerases or enzymes to degrade the biofilm matrix (e.g., EPS) [85]. |
| Receptor Masking via Capsules | Physical shielding of receptor sites by capsules or extracellular polysaccharides [85]. | Evolution of phages with enzymatic activity to degrade capsules or polysaccharides [85]. |
The following diagram illustrates the dynamic co-evolutionary arms race between phages and their bacterial hosts, which can be harnessed in the lab to generate enhanced therapeutic phages.
Quantitative Clinical Evidence and Applications
Phage therapy is demonstrating promise in treating complex, device-related infections, which are often linked to gut-derived pathogens. The data in Table 2 summarizes key clinical findings, particularly in periprosthetic joint infections (PJI), a model for difficult-to-treat biofilm-associated diseases.
Table 2: Quantitative Clinical Outcomes of Phage Therapy for Orthopedic Infections
| Study (Country) | Patients (N) | Pathogen | Key Clinical Outcome |
|---|---|---|---|
| Fedorov et al. (Prospective) [89] | 23 (Phage) vs. 22 (Control) | Mixed PJI pathogens | PJI relapse rate was 8 times higher in the control group at 1-year follow-up [89]. |
| Farry et al. [89] | 1 | P. aeruginosa & S. aureus | No clinical signs of infection at 18-month follow-up after DAIR and phage/antibiotic therapy [89]. |
| Tkhilaishvili et al. [89] | 1 | MDR P. aeruginosa | Favorable recovery after prosthesis reimplantation; negative cultures post-treatment [89]. |
Experimental Protocol: Adaptive Phage Evolution (Appelmans Protocol)
The Appelmans protocol is a classic method for experimentally driving phage evolution to expand host range and overcome bacterial resistance [85].
Methodology:
- Preparation: Co-culture a mixture of the primary bacterial target strain and one or more resistant or initially non-susceptible bacterial strains in a nutrient broth. The resistant strains should possess known resistance mechanisms (e.g., receptor mutants).
- Initial Infection: Introduce the initial clonal phage population to the mixed bacterial culture at a high multiplicity of infection (MOI >1).
- Incubation and Lysis: Incubate the culture until visible lysis is observed.
- Harvesting: Centrifuge the lysate and filter it through a 0.22 µm filter to remove bacterial debris and any remaining live bacteria, collecting the phage-containing filtrate.
- Serial Passage: Use a small aliquot (e.g., 1-2%) of the filtered lysate to infect a fresh, actively growing mixed bacterial culture.
- Iteration: Repeat steps 3-5 for numerous serial passages (e.g., 20-50 cycles) under controlled and selective pressures, which can include variations in nutrient availability, oxygen tension, or the presence of sub-inhibitory antibiotics to simulate in vivo conditions [85].
- Plaque Assay and Isolation: After the final passage, perform plaque assays on both the original target strain and the resistant strains. Isolate individual plaques that appear on the initially resistant bacterial lawns.
- Characterization: Amplify and purify these evolved phage clones. Characterize them through genome sequencing (to identify mutations in RBP genes), burst size assays, and host range profiling against a panel of clinically relevant strains.
Bacteriocins: Targeted Molecular Snipers
Classification and Mechanisms of Action
Bacteriocins are ribosomal-synthesized antimicrobial peptides produced by virtually all bacterial lineages, most notably Lactic Acid Bacteria (LAB) [86] [87]. Their primary mechanism involves interacting with the cytoplasmic membrane of susceptible bacteria, leading to pore formation, depolarization, and leakage of cellular contents [86]. They are classified based on their structural properties, as detailed in Table 3.
Table 3: Classification and Properties of Key Bacteriocins from Gram-Positive Bacteria
| Class | Key Features | Prominent Examples | Primary Target/Spectrum |
|---|---|---|---|
| Class I (Lantibiotics) | Small, post-translationally modified peptides (<5 kDa) containing lanthionine [87]. | Nisin, Lacticin 3147 [90] [87]. | Broad-spectrum activity against Gram-positive pathogens, including Listeria, Clostridium, Staphylococcus [90]. |
| Class II (Non-lantibiotics) | Small, heat-stable, non-modified peptides (<10 kDa) [87]. Subclasses: IIA (Pediocin-like, anti-Listeria), IIB (Two-peptide), IIC (Non-pediocin single peptide) [87]. | Pediocin PA-1, Enterocin AS-48, Lactococcin A [90] [87]. | Primarily Gram-positives; some show activity against Gram-negatives if the outer membrane is disrupted [87]. |
| Class III | Large, heat-labile proteins (>30 kDa) [87]. | Helveticin J, Enterolysin A [87]. | Gram-positive bacteria [87]. |
| Class IV | Complex bacteriocins with lipid or carbohydrate moieties [87]. | Leuconocin S, Lactocin 27 [87]. | Gram-positive bacteria [87]. |
Quantitative Efficacy in Food and Emerging Health Applications
The efficacy of bacteriocins is well-quantified in food preservation models, providing a foundation for their therapeutic use.
Table 4: Quantified Efficacy of Selected Bacteriocins in Preservation and Health
| Bacteriocin | Application Context | Quantified Efficacy |
|---|---|---|
| Nisin | Beer preservation against Lactobacillus brevis spoilage [86]. | Stable in acidic conditions; can eliminate up to 90% of Gram-positive bacteria without affecting S. cerevisiae fermentation [86]. |
| Pediocin | Biopreservation in vegetable and meat products [90]. | Shows high efficacy against Listeria species [90]. |
| Thuricin CD | Potential therapeutic for Clostridioides difficile infection [87]. | A two-peptide bacteriocin with narrow-spectrum activity against C. difficile [87]. |
| Multiple Bacteriocins | Anticancer, antiviral, and anti-biofilm properties [87]. | Emerging evidence shows efficacy against clinically significant pathogens, viral infections, and cancer cells, though largely in pre-clinical stages [87]. |
The following diagram maps the logical flow of bacteriocin biosynthesis from gene to mature, active compound, a key process for their laboratory production and engineering.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 5: Key Reagent Solutions for Phage and Bacteriocin Research
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| Bacterial Strain Libraries | Targets for host range determination, resistance evolution studies, and efficacy testing. | Clinical isolates of target pathogens (e.g., MDR K. pneumoniae, P. aeruginosa, S. aureus); lab strains with defined resistance mutations [85]. |
| Phage Libraries / Biobanks | Source of diverse, characterized phages for therapy and cocktail development. | Pre-established collections from environmental or clinical sources; platforms for rapid matching [85]. |
| Lactic Acid Bacteria (LAB) | Producers of many GRAS-status bacteriocins. | Lactococcus lactis (Nisin), Pediococcus acidilactici (Pediocin), other Lactobacillus and Enterococcus spp. [86] [87]. |
| Cell Culture Models | Assessing intracellular activity, host-cell interactions, and cytotoxicity. | Caco-2, HT-29 cells for gut barrier studies; macrophage models for immunomodulation [89]. |
| Biofilm Reactors | Mimicking in vivo biofilm growth for testing anti-biofilm efficacy. | Calgary biofilm device, flow-cell systems; used for both phage and bacteriocin studies [85] [87]. |
| Animal Disease Models | In vivo efficacy and safety testing. | Mouse models of C. difficile infection, PJI, NEC, or gut-derived sepsis [91]. |
| Analytical Chromatography (HPLC, FPLC) | Purification and quantification of bacteriocins from culture supernatants. | Essential for producing high-purity bacteriocins for experimental use [86]. |
| Genomic Sequencing Platforms | Characterizing phage genomes, identifying RBP mutations, and detecting bacteriocin gene clusters. | Whole-genome sequencing of evolved phages; metagenomics for community impact analysis [85]. |
Regulatory and Production Landscapes
A significant regulatory breakthrough occurred in 2025 with France's authorization of a personalized phage therapy platform for veterinary use [92]. This model departs from approving static formulations and instead approves a framework for producing tailored phage combinations, allowing for rapid updates as resistance emerges. This platform approach serves as a vital regulatory model for future human applications [92].
For both phages and bacteriocins, innovative formulation strategies are being employed to overcome stability and delivery challenges. These include:
- Encapsulation with nanoparticles (e.g., silver) to enhance stability and efficacy of bacteriocins [87].
- Incorporation into active packaging films and coatings for food preservation, a strategy transferable to medical device coatings [86] [87].
- Development of defined synthetic bacterial communities that can deliver bacteriocins or other beneficial functions in a stable, robust manner to the gut ecosystem [91].
Bench to Bedside: Validating Microbiome-Based Interventions in Clinical Practice
The human gut microbiome, a complex ecosystem of trillions of microorganisms, plays an integral role in maintaining gastrointestinal, immune, and nervous system homeostasis. [93] Dysbiosis—disturbances in this microbial community—is associated with numerous gastrointestinal and extra-intestinal disorders. [93] Fecal microbiota transplantation (FMT), the transfer of processed fecal matter from a healthy donor to a recipient's gastrointestinal tract, has emerged as a powerful therapeutic approach to correct this dysbiosis by restoring a balanced microbiome. [93]
While FMT's efficacy in treating recurrent Clostridioides difficile infection (rCDI) is well-established, its application is expanding into novel clinical domains, particularly oncology. [93] [94] This whitepaper synthesizes current evidence on FMT's mechanism, efficacy, and protocols in rCDI, and explores its promising role as an adjunctive therapy to enhance cancer immunotherapy, framing these advances within the broader context of gut microbiome health-disease association research.
Efficacy and Mechanisms of FMT in RecurrentC. difficileInfection
Clinical Efficacy Data
rCDI represents a significant clinical challenge, as standard antibiotic therapy often fails to break the cycle of recurrence. [95] FMT addresses the underlying dysbiosis, making it a profoundly effective intervention. A 2025 systematic review and meta-analysis of 15 studies involving 1,452 patients demonstrated that FMT was significantly superior to standard antibiotic therapy (vancomycin or fidaxomicin) for rCDI, with a relative risk (RR) of 1.85 (95% CI: 1.62-2.11, p < 0.001). [95] The recurrence rate was 16% for FMT versus 42% for antibiotics. [95] Subgroup analyses confirmed efficacy regardless of delivery method—colonoscopy, nasogastric tube, or capsules. [95]
Recent real-world evidence and studies of FDA-approved live biotherapeutic products corroborate these findings. The Phase 3b CDI-SCOPE trial of REBYOTA (fecal microbiota, live – jslm) reported a 95% treatment success rate at 8 weeks post-administration via colonoscopy. [96]
Table 1: Summary of Key Clinical Efficacy Outcomes for FMT in rCDI
| Study / Trial | Design | Patient Population | Comparison | Primary Outcome | Result |
|---|---|---|---|---|---|
| Meta-analysis 2025 [95] | Systematic Review & Meta-analysis | 1,452 patients with rCDI | FMT vs. Standard Antibiotics | Recurrence Rate | FMT: 16% vs. Antibiotics: 42% (RR=1.85, 95% CI: 1.62-2.11, p<0.001) |
| CDI-SCOPE (Phase 3b) [96] | Multicenter, Single-Arm | 41 adults with rCDI | REBYOTA (single-dose) | Treatment Success at 8 Weeks | 95% (39/41) |
| Real-world Study [97] | Retrospective Analysis | 130 patients with rCDI | REBYOTA within vs. beyond standard washout | Recurrence Rate | ≤3-day washout: 25.3% vs. >3-day washout: 3.2% (p=0.008) |
Mechanisms of Action
The therapeutic mechanism of FMT in rCDI involves restoring a healthy gut microbial community to re-establish colonization resistance and normal metabolic function.
- Microbial Restoration: FMT replenishes beneficial bacterial taxa that are depleted in rCDI, such as Bacteroidia and Clostridia, while reducing the abundance of disease-associated classes like Gammaproteobacteria and Bacilli. [96] This shift is quantifiable through metrics like the Microbiome Health Index for post-antibiotic dysbiosis (MHI-A), which shows sustained improvement for at least six months after FMT. [96]
- Bile Acid Metabolism: A healthy gut microbiota is essential for converting primary bile acids (e.g., cholic acid), which promote C. difficile spore germination, into secondary bile acids (e.g., deoxycholate), which inhibit germination and growth. [93] This conversion is mediated by the bacterial enzyme 7-alpha-dehydroxylase. [93]
- Short-Chain Fatty Acid (SCFA) Production: Donor microbiota restore the production of SCFAs like butyrate, which inhibits C. difficile growth, promotes secondary bile acid conversion, and supports immune modulation within the colonic mucosa. [93]
The following diagram illustrates the core mechanisms by which FMT restores gut homeostasis to combat rCDI:
Standardized FMT Protocols and Methodologies
Donor Screening and FMT Preparation
Rigorous donor screening is paramount for safety. Protocols typically involve a multi-step process to exclude donors with risk factors for transmissible diseases. [93]
- Questionnaire: Initial screening assesses general health, travel history, antibiotic use, and risk factors for infectious diseases. [93]
- Comprehensive Serologic and Stool Testing: This excludes asymptomatic pathogen carriers. Testing includes blood tests for HIV, Hepatitis A, B, and C, and syphilis, and stool tests for enteric pathogens, C. difficile, and multi-drug resistant organisms. [93] [96]
- Product Preparation: Fecal samples can be prepared as fresh or frozen suspensions. Meta-analyses show no clinically significant difference in efficacy for rCDI, though frozen products enhance availability and reduce costs. [93] FDA-approved live biotherapeutic products (LBPs) like REBYOTA offer a standardized, pre-packaged formulation. [96]
Administration Methods
The choice of administration route depends on clinical presentation, availability, and patient factors. All routes are generally safe, with the most common adverse events being mild abdominal discomfort, bloating, and diarrhea. [93]
- Lower-GI Delivery: Colonoscopy allows for direct delivery to the colon and visual assessment of the mucosa. Enema is less invasive and can be self-administered. [93]
- Upper-GI Delivery: Nasogastric/nasoduodenal tubes or oral capsules offer non-invasive alternatives. Encapsulated formulations are particularly appealing for patient convenience. [93]
Table 2: Essential Research Reagents and Materials for FMT Studies
| Category / Item | Specific Examples / Methods | Primary Function in FMT Research |
|---|---|---|
| Donor Screening | Serological tests, Stool PCR/multiplex panels, Medical history questionnaires | Ensures safety by screening for transmissible pathogens and health risks. [93] |
| FMT Product | Fresh fecal suspension, Frozen fecal suspension, Lyophilized powder, FDA-approved LBP (REBYOTA) | The active therapeutic material; different formulations impact stability and administration. [96] [93] |
| Microbiome Analysis | 16S rRNA sequencing, Shotgun metagenomics, Metabolomics (SCFAs, Bile Acids) | Characterizes microbial composition, function, and engraftment post-FMT. [96] [98] |
| Administration Tools | Colonoscope, Enema kit, Nasogastric tube, Capsule-in-capsule technology | Enables delivery of the FMT product to the gastrointestinal tract. [93] |
| Immunological Assays | Flow cytometry (e.g., for T cell populations), Cytokine profiling (ELISA/MSD), Immunohistochemistry | Measures host immune response in conditions like UC and cancer. [99] [94] |
The workflow for a typical FMT procedure for rCDI, from donor to recipient, is summarized below:
Emerging Applications in Oncology
FMT to Enhance Cancer Immunotherapy
The gut microbiome significantly influences the immune system and can modulate responses to cancer therapy, particularly immune checkpoint inhibitors (ICIs). [99] [94] FMT is being investigated as an adjunctive therapy to overcome resistance to ICIs.
A 2025 systematic review evaluated FMT's impact in cancer patients receiving immunotherapy, chemotherapy, or radiotherapy. [99] While large-scale RCTs are pending, preliminary findings from 45 studies suggest FMT is safe and feasible during cancer treatment. [99] Mechanistically, donor FMT appears to reprogram the gut ecosystem, leading to observed increases in tumor-infiltrating CD8+ T lymphocytes (critical for anti-tumor cytotoxicity) and lower levels of regulatory T cells (which suppress immune responses). [99] This creates a more favorable tumor microenvironment for immunotherapy to work. Furthermore, FMT has shown promise in managing ICI-induced colitis, a common immune-related adverse event, by restoring gut microbial diversity and reducing colonic CD8+ T cell infiltration. [99]
Proposed Mechanism in Oncology
The proposed mechanism for FMT in enhancing ICI response involves a complex interplay between the gut microbiota and the host immune system:
The success of FMT in oncology may depend on recipient factors, with a key hypothesis being that patients with low baseline gut microbial diversity are most likely to benefit. [99] This underscores the importance of patient stratification in future clinical trials.
FMT represents a paradigm shift in managing recurrent C. difficile infection, offering a superior alternative to standard antibiotics by targeting the underlying dysbiosis. Strong evidence supports its efficacy and safety, leading to its standardization in clinical guidelines and the development of FDA-approved live biotherapeutic products.
The application of FMT is now extending into oncology, where it holds significant promise for modulating the tumor immune microenvironment and enhancing responses to immunotherapy. While current data are preliminary, they highlight the immense potential of microbiome-based interventions in cancer treatment. Future research must focus on large-scale randomized controlled trials, mechanistic studies to elucidate donor-recipient interactions, and the development of standardized protocols and predictive biomarkers to guide patient selection and donor matching. As part of the broader gut microbiome health-disease association research landscape, FMT stands as a powerful tool for translating microbiome science into transformative clinical therapies.
The field of next-generation probiotics (NGPs) represents a paradigm shift in microbiome-based therapeutics, moving beyond traditional probiotics to defined microbial consortia with specific mechanistic functions. Akkermansia muciniphila, a mucin-degrading commensal bacterium, has emerged as a cornerstone NGP candidate with demonstrated efficacy in metabolic disorders, inflammatory conditions, and neurological diseases. This technical review comprehensively examines the scientific foundation, mechanistic insights, experimental methodologies, and translational applications of NGPs, with particular emphasis on A. muciniphila and defined microbial communities. We integrate current research findings, detailed experimental protocols, and analytical frameworks to provide researchers and drug development professionals with a comprehensive resource for advancing NGP development. The convergence of synthetic biology, multi-omics technologies, and precision medicine approaches is accelerating the transition from correlation-based observations to mechanism-driven therapeutic interventions, positioning NGPs as transformative tools for managing chronic diseases through gut microbiome modulation.
Definition and Scope
Next-generation probiotics (NGPs) represent an advanced class of therapeutic microorganisms derived from the human gut microbiome, distinct from traditional probiotics (e.g., Lactobacillus and Bifidobacterium species) in their origin, mechanisms, and applications [100]. Unlike conventional probiotics that primarily undergo transient gastrointestinal passage, NGPs are typically anaerobic, human-native bacteria capable of persistent colonization and specialized host interactions [101]. The NGP landscape encompasses strains from the genera Bacteroides, Faecalibacterium, Akkermansia, and Clostridium, which exhibit sophisticated functional capabilities including immunomodulation, metabolic regulation, and gut barrier reinforcement [100] [102].
Evolution from Traditional Probiotics
The transition from traditional probiotics to NGPs marks a fundamental shift from broad-spectrum supplementation to targeted, mechanism-based interventions. This evolution is characterized by three critical advancements: (1) the identification of bacterial species with specific host-interactive capabilities beyond nutrient fermentation; (2) the development of sophisticated delivery systems to overcome the oxygen sensitivity and nutritional fastidiousness of anaerobic gut species; and (3) the integration of precision medicine approaches based on individual microbiome composition [102]. A. muciniphila exemplifies this transition, possessing unique mucosal colonization capacity, potent anti-inflammatory and metabolic regulatory capabilities through specific functional proteins, and a complete mucin-degrading enzymatic system that directly participates in mucosal homeostasis regulation [101].
Physiological Characteristics and Ecological Niche
A. muciniphila is a mucin-degrading commensal bacterium that colonizes the intestinal mucus layer, representing 1-4% of the total gut microbiota in healthy individuals [103]. As a specialist mucin glycan-degrader, it relies completely on mucins as a carbon and energy source and possesses a complete mucin-degrading enzymatic system that distinguishes it from generalist glycan-degraders [104] [101]. This specialized ecological adaptation allows A. muciniphila to maintain mucosal homeostasis through controlled degradation and regeneration of the mucus layer, positioning it as a keystone species in gut ecosystem stability [101].
Functional Components and Molecular Mechanisms
The therapeutic effects of A. muciniphila are mediated through multiple functional components that operate via distinct molecular mechanisms (Table 1).
Table 1: Key Functional Components of A. muciniphila and Their Mechanisms of Action
| Functional Component | Molecular Structure | Primary Mechanism | Biological Effect |
|---|---|---|---|
| Outer membrane protein Amuc_1100 | Tetrametric pore-forming protein | Activates TLR2 signaling; enhances SOD activity; reduces MDA markers [101] | Improves gut barrier function; reduces oxidative stress; modulates immunity |
| Short-chain fatty acids (SCFAs) | Acetate, propionate | Modulates TLR2/MyD88/NF-κB signaling; regulates gut hormones GLP-1 and PYY [101] [102] | Anti-inflammatory; enhances gut barrier; regulates energy homeostasis |
| Extracellular vesicles (EVs) | Membrane-bound nanoparticles | Facilitates interbacterial communication via membrane fusion; modulates MAPK signaling [101] | Reinforces intestinal barrier function; ameliorates oxidative damage |
| Mucin-degrading enzymes | Glycoside hydrolases, proteases | Degrades mucin glycans; produces SCFAs and other metabolites [104] [101] | Maintains mucus layer turnover; provides substrates for other microbes |
Signaling Pathways Regulating Oxidative Stress
A. muciniphila modulates host oxidative stress through multiple interconnected signaling pathways (Figure 1). The outer membrane protein Amuc_1100 activates both the PI3K-AKT signaling pathway and the Keap1-Nrf2/HO-1 pathway, effectively mitigating oxidative stress [101]. Simultaneously, microbial-derived SCFAs remodel the intestinal microenvironment by modulating TLR2/MyD88/NF-κB signaling pathways, thereby enhancing the host's antioxidant defense mechanisms [101]. These pathways collectively regulate the expression of antioxidant enzymes including superoxide dismutase (SOD) and glutathione peroxidase (GPx), while reducing oxidative damage markers such as malondialdehyde (MDA) [101].
Figure 1: A. muciniphila Signaling Pathways in Oxidative Stress Regulation
Experimental Models and Methodologies for NGP Research
In Vitro Synthetic Microbial Community Models
Reduced-complexity synthetic communities provide controlled systems for investigating microbial interactions, engraftment dynamics, and functional outcomes. The mucin-degrading synthetic community (MDSC) model exemplifies this approach for studying A. muciniphila integration [104].
MDSC Composition and Cultivation
The MDSC comprises 14 bacterial species representing three trophic levels: (1) mucin glycan-degraders (Bacteroides caccae, Bacteroides fragilis, Bacteroides thetaiotaomicron, Phocaeicola vulgatus, Ruminococcus gnavus, Ruminococcus torques); (2) secondary degraders that produce butyrate (Anaerostipes caccae, Faecalibacterium duncaniae, Anaerobutyricum hallii, Agathobacter rectalis, Roseburia intestinalis); and (3) hydrogen consumers (Desulfovibrio piger, Methanobrevibacter smithii, Blautia hydrogenotrophica) [104].
Table 2: In Vitro Experimental Protocol for Assessing NGP Engraftment
| Step | Procedure | Parameters | Quality Control |
|---|---|---|---|
| Preculture preparation | Grow individual strains in anoxic serum bottles with mucin medium | 0.5% (w/v) porcine gastric mucin Type III, 1 g/L yeast extract, bicarbonate-buffered anoxic medium [104] | Verify purity and growth phase (overnight cultures) |
| Bioreactor setup | DASGIP Parallel Bioreactor System operated in continuous mode | Duplicate reactors, anaerobic conditions, constant mucin supply [104] | Monitor stabilization (typically 72-96 hours) |
| NGP introduction | Inoculate A. muciniphila at 0.1% v/v from preculture | Addition at t=96h after community stabilization [104] | Confirm viable cell count (10^10 CFU/mL) |
| Sampling and analysis | Collect samples at defined intervals for multi-omics analysis | 16S rRNA sequencing, metaproteomics, qPCR [104] | Include negative controls and mock communities |
Analytical Methods for Engraftment Assessment
Post-inoculation analysis employs integrated multi-omics approaches:
- 16S rRNA gene amplicon sequencing: V4 region amplification with barcoded primers, sequencing on Illumina NovaSeq 6000, data processing with NG-Tax 2.0 pipeline [104]
- Metaproteomic analysis: LC-MS/MS quantification of key enzymatic activities including peptidases, fucosidases, galactosidases, sulfatases, and sialidases [104]
- qPCR validation: Total bacterial abundance quantification and specific genus ratios (e.g., Bacteroides spp. to P. vulgatus) [104]
In Vivo Validation Models
Animal models, particularly high-fat diet (HFD)-induced obese mice, have been instrumental in validating the therapeutic effects of A. muciniphila. Seminal studies demonstrate that both live and pasteurized A. muciniphila significantly ameliorate obesity, insulin resistance, and adipose tissue inflammation in HFD-fed mice [101]. The pasteurized form has shown superior efficacy in improving metabolic parameters, attributed to the enhanced stability and bioavailability of key components like Amuc_1100 [101].
Defined Microbial Consortia: Design Principles and Applications
Rational Design of Synthetic Communities
Defined microbial consortia represent an advanced approach beyond single-strain NGPs, enabling the reconstitution of complex ecological functions through strategically selected complementary species. Rational design principles include:
- Functional complementarity: Selection of species with complementary metabolic capabilities (e.g., primary degraders, secondary fermenters, hydrogenotrophs) [104] [102]
- Trophic integration: Assembly of species that form complete metabolic pathways through cross-feeding interactions [104]
- Ecological stability: Inclusion of species that create stable coexistence through niche partitioning [104] [102]
Engineering Strategies for Enhanced Functionality
Advanced engineering approaches are being applied to enhance the functionality and efficacy of defined microbial consortia:
- CRISPR-based gene editing: Precision modification of bacterial genomes to enhance therapeutic properties or introduce novel functions [102] [62]
- Synthetic biology circuits: Design of genetic circuits that enable programmed behaviors such as pathogen sensing and therapeutic response [102]
- Biomimetic delivery systems: Development of microencapsulation and other delivery technologies to enhance bacterial viability and targeted delivery [101]
Translational Applications and Clinical Evidence
Metabolic Disorders
A. muciniphila demonstrates compelling clinical efficacy in metabolic disorders. A landmark human trial showed that daily supplementation with pasteurized A. muciniphila (10^10 CFU/day) for 3 months increased insulin sensitivity by 28.62 ± 7.02% in overweight individuals [101]. More recently, a large randomized controlled trial demonstrated that specific live A. muciniphila strains were markedly more effective than inactivated cells in improving metabolic parameters, challenging conventional beliefs about bacterial viability requirements [101].
Gastrointestinal and Inflammatory Disorders
The therapeutic potential of A. muciniphila and defined consortia extends to various gastrointestinal conditions:
- Inflammatory Bowel Disease (IBD): A. muciniphila abundance is inversely correlated with IBD severity, and its components demonstrate efficacy in reducing intestinal inflammation through reinforcement of gut barrier function [101] [103]
- Irritable Bowel Syndrome (IBS): Defined consortia including multi-strain probiotics specifically formulated for IBS show promise in clinical trials [6]
- Clostridioides difficile infection: Fecal microbiota transplantation and defined microbial consortia have demonstrated high efficacy in recurrent infections, with formal clinical pathways now established [105]
Neurological Disorders
Emerging evidence indicates gut-brain axis mediation of neurological benefits:
- Parkinson's Disease: Reduced fecal A. muciniphila abundance correlates with elevated cerebrospinal fluid α-synuclein oligomers, and supplementation shows potential in mitigating pathology by regulating α-synuclein oligomerization [101]
- Depression and Quality of Life: Population cohort studies using gut-brain module analysis have identified specific microbial pathways linking A. muciniphila and related species to mental health outcomes [6]
Commercial Landscape and Regulatory Framework
The microbiome therapeutics market is experiencing rapid expansion, valued at USD 187.13 million in 2024 and projected to reach USD 3,405.99 million by 2034, representing a CAGR of 33.67% [105]. This growth is fueled by increasing investment in advanced microbiome research and expanding applications in treating complex diseases. The market encompasses various product types, with probiotics currently holding a considerable share but postbiotics projected for the highest growth CAGR between 2025 and 2034 [105].
Table 3: Global Microbiome Therapeutics Market Segmentation
| Segment Category | Dominant Segment (2024) | Fastest Growing Segment | Key Market Players |
|---|---|---|---|
| Product Type | Probiotics | Postbiotics | Seres Therapeutics, Vedanta Biosciences |
| Therapeutic Application | Gastrointestinal Disorders | Oncology | Enterome Bioscience, 4D Pharma |
| Mode of Administration | Oral | Rectal (FMT delivery) | Rebiotix, Microbiome Therapeutics |
| Region | North America (49% share) | Asia Pacific | Yakult Honsha, Second Genome |
Regulatory Considerations
The regulatory landscape for NGPs is evolving, with regional variations in approval pathways:
- United States: FDA oversight through IND (Investigational New Drug) Application and BLA (Biologics License Application) pathways, with enforcement discretion for Fecal Microbiota Transplantation (FMT) for specific indications [105]
- European Union: EMA regulation under Clinical Trial Authorization and Advanced Therapy Medicinal Products frameworks [105]
- Novel Food Authorization: The European Commission authorized Pasteurized A. muciniphila as a novel food in 2022, specifying a maximum daily intake of 3.4 × 10^10 CFU for both adults and children [101]
Technological Innovations and Future Directions
Advanced Analytics and Artificial Intelligence
Technological innovations are dramatically accelerating NGP discovery and development:
- AI-driven discovery: Machine learning algorithms rapidly identify new live biotherapeutics and engineered microbial strains, reducing the need for extensive empirical testing [105]
- Multi-omics integration: Combined metagenomic, metabolomic, and proteomic analyses enable comprehensive functional assessment of NGPs and defined consortia [102] [105]
- Microbiome-based diagnostics: Gut microbiome profiling is increasingly used in preventive healthcare to identify individuals who would benefit most from targeted NGP interventions [105]
Personalized NGP Formulations
The future of NGPs lies in personalized formulations tailored to individual microbiome compositions and host factors. Factors influencing personalization include:
- Microbiome composition: Baseline microbiota analysis to identify missing keystone species or functional deficiencies [102]
- Host genetics: Genetic variations in carbohydrate-active enzyme genes (e.g., sucrase-isomaltase) that influence response to specific NGPs [6]
- Dietary patterns: Background diet as a significant modifier of NGP efficacy through changes in gut microenvironment [6]
Research Reagent Solutions
Table 4: Essential Research Reagents for NGP Investigation
| Reagent Category | Specific Products | Research Application | Technical Considerations |
|---|---|---|---|
| Bacterial Culture Media | Bicarbonate-buffered anoxic medium with porcine gastric mucin (Type III) [104] | Cultivation of oxygen-sensitive NGPs | Requires anaerobic chambers; mucin as primary carbon source |
| Molecular Biology Tools | 16S rRNA primers (V4 region); FastDNA SPIN Kit for Soil [104] | Microbiome composition analysis | Standardized protocols essential for cross-study comparisons |
| Cell Culture Systems | Caco-2 cells; HT-29-MTX-E12 co-cultures | Gut barrier integrity assessment | Permeability measurements via TEER; mucin production quantification |
| Analytical Standards | SCFA reference standards; cytokine ELISA kits | Metabolite and inflammatory marker quantification | LC-MS/MS for SCFA detection; multiplex assays for cytokines |
| Animal Models | High-fat diet-induced obese mice; germ-free models | In vivo efficacy validation | Controlled microbiota status essential for interpretation |
Next-generation probiotics, exemplified by Akkermansia muciniphila and advancing toward defined microbial consortia, represent a transformative approach in microbiome-based therapeutics. The field has progressed from correlation observations to mechanistic understanding of specific bacterial components and their molecular interactions with the host. Current research demonstrates that A. muciniphila operates through multiple synchronized mechanisms—including outer membrane proteins, SCFAs, extracellular vesicles, and mucin-degrading enzymes—to exert systemic effects on metabolic health, inflammatory processes, and neurological function. The successful development of NGPs requires sophisticated experimental models, advanced analytical techniques, and careful consideration of regulatory pathways. As synthetic biology, AI-driven discovery, and personalized medicine approaches continue to mature, NGPs and defined microbial consortia are poised to revolutionize therapeutic interventions for chronic diseases across multiple organ systems.
The human gut microbiome, a complex ecosystem of trillions of microorganisms, has emerged as a critical regulator of human health and disease. Its homeostasis is indispensable for regulating intestinal inflammation, maintaining metabolic equilibrium, supporting immune system maturation, and facilitating neurological functions [106] [107]. Disruptions in gut microbiota homeostasis, known as dysbiosis, are increasingly implicated in the pathogenesis of a wide spectrum of conditions, including inflammatory bowel disease, obesity, type 2 diabetes, cardiovascular diseases, and neurodegenerative disorders such as Alzheimer's disease [106] [107]. This understanding has catalyzed the development of therapeutic strategies aimed at modulating the gut ecosystem, primarily through the administration of "biotics"—a family of interventions that include probiotics, prebiotics, synbiotics, and postbiotics.
Among these, prebiotics and postbiotics represent complementary yet distinct approaches to microbiome modulation. Prebiotics are defined as "substrates that are selectively utilized by host microorganisms, conferring a health benefit on the host" [108]. They essentially function as specialized nutrients for beneficial gut bacteria. In contrast, postbiotics are "preparations of inanimate microorganisms and/or their components that confers a health benefit on the host" [108]. This category includes inactivated microbial cells, cell fragments, and microbial metabolites that provide health benefits without requiring live organisms.
The growing scientific and commercial interest in these interventions reflects a paradigm shift in therapeutic strategy—from targeting single pathways with synthetic medicines to restoring ecological balance within the gut microenvironment. This whitepaper provides a comprehensive technical analysis of the comparative mechanisms and clinical advantages of prebiotics and postbiotics, contextualized within the broader framework of gut microbiome-health-disease associations. It is intended to equip researchers, scientists, and drug development professionals with the latest evidence and methodological considerations for advancing this promising field.
Defining the Landscape: Prebiotics and Postbiotics
Prebiotics: Selective Microbial Substrates
Prebiotics are typically non-digestible food components, primarily dietary fibers, that resist gastric acidity and hydrolysis by mammalian enzymes, allowing them to reach the colon intact where they are selectively fermented by beneficial members of the gut microbiota [109]. Common examples include fructooligosaccharides (FOS), galactooligosaccharides (GOS), and inulin [109]. The prebiotic effect is mediated through the enrichment of commensal bacteria such as Bifidobacterium and Lactobacillus, which metabolize these substrates into health-promoting metabolites, most notably short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate [109].
The International Scientific Association for Probiotics and Prebiotics (ISAPP) maintains that for a substance to be classified as a prebiotic, it must demonstrate: (1) resistance to gastric acidity and mammalian enzyme hydrolysis; (2) fermentation by intestinal microbiota; and (3) selective stimulation of growth and/or activity of intestinal bacteria associated with health and wellbeing [108].
Postbiotics: Inactivated Microbial Components
Postbiotics represent a more recent conceptual advancement in biotic therapeutics. They are defined as "preparations of inanimate microorganisms and/or their components that confer a health benefit on the host" [108]. The composition of postbiotics is heterogeneous, encompassing:
- Inactivated microbial cells (heat-killed, radiation-treated, or high-pressure processed)
- Microbial cell structures (cell wall fragments, surface proteins, peptidoglycans)
- Microbial metabolites (short-chain fatty acids, organic acids, vitamins, extracellular polysaccharides) [110]
Unlike probiotics, postbiotics do not require the administration of live microorganisms, which fundamentally alters their safety profile, stability, and potential mechanisms of action [110]. Notable examples include heat-killed Lactobacillus acidophilus strain LB, heat-killed Bifidobacterium bifidum MIMBb75, and pasteurized Akkermansia muciniphila [109].
Table 1: Comparative Definitions and Compositions
| Feature | Prebiotics | Postbiotics |
|---|---|---|
| Definition | Substrates selectively utilized by host microorganisms, conferring a health benefit [108] | Preparation of inanimate microorganisms and/or their components that confers a health benefit [108] |
| Composition | Non-digestible carbohydrates (e.g., FOS, GOS, inulin) [109] | Inactivated microbes, cell fragments, metabolites (e.g., SCFAs, teichoic acids) [110] |
| Viability Requirement | No live components | No viability required; often contain inactivated cells |
| Primary Targets | Indigenous gut microbiota (e.g., Bifidobacterium, Lactobacillus) [109] | Host cells (immune, epithelial) and resident microbiota [110] |
Comparative Mechanisms of Action
Prebiotics and postbiotics employ distinct yet potentially complementary biological pathways to promote host health. These mechanisms can be broadly categorized into direct effects on host cellular pathways and indirect effects mediated through modulation of the gut microbiota and its metabolic output.
Mechanism of Prebiotic Action
The fundamental mechanism of prebiotics involves selective stimulation of beneficial gut bacteria, leading to changes in microbial community structure and function [108] [109]. This process follows a sequential pathway:
Selective Utilization: Prebiotics serve as specialized growth substrates for specific beneficial bacterial taxa, particularly Bifidobacterium and Lactobacillus species, giving them a competitive advantage over other microbes in the gut ecosystem [109].
Fermentation and Metabolic Output: These bacteria ferment prebiotics, producing SCFAs (acetate, propionate, butyrate) as primary metabolic end products [109]. Butyrate serves as the primary energy source for colonocytes and enhances epithelial barrier function by upregulating tight junction proteins (occludins, claudins, zonula occludens-1) [107]. SCFAs also exert systemic anti-inflammatory effects and modulate host metabolism.
Microbial Cross-Feeding: The initial metabolites produced by primary fermenters often serve as substrates for secondary microbial conversions, creating complex metabolic networks within the gut ecosystem that further influence host physiology.
Pathogen Inhibition: The expansion of beneficial microbiota and their production of antimicrobial substances creates an environment that is less favorable for pathogens, providing colonization resistance [109].
The following diagram illustrates the sequential mechanism of prebiotic action:
Diagram 1: Prebiotic Action Mechanism (65 characters)
Mechanism of Postbiotic Action
Postbiotics exert their effects through more direct interactions with host cells and tissues, bypassing the need for microbial fermentation or growth within the host [110]. Their mechanisms include:
Direct Receptor-Mediated Signaling: Microbial cell wall components (peptidoglycans, teichoic acids, lipoteichoic acids) and other structural elements in postbiotics can directly engage with host pattern recognition receptors (e.g., Toll-like receptors) on epithelial and immune cells, modulating inflammatory pathways and enhancing barrier defense [110].
Provision of Bioactive Metabolites: Postbiotic preparations often contain pre-formed microbial metabolites (SCFAs, neurotransmitters, vitamins) that can directly influence host physiology without requiring microbial metabolism in situ [110].
Competitive Exclusion: Even inanimate microbial cells can adhere to intestinal epithelia, potentially preventing pathogen attachment through receptor competition [110].
Regulation of Immune Responses: Postbiotics can modulate the host immune system by promoting anti-inflammatory cytokine production (e.g., IL-10) while suppressing pro-inflammatory responses (e.g., TNF-α, IL-6, IL-8) [110] [109].
The following diagram illustrates the direct mechanism of postbiotic action:
Diagram 2: Postbiotic Action Mechanism (66 characters)
Integrated Pathways in the Gut-Brain Axis
The gut-brain axis represents a bidirectional communication network through which prebiotics and postbiotics can influence neurological function and potentially modify neurodegenerative disease progression [107]. Both prebiotics and postbiotics modulate this axis through multiple interconnected pathways:
Neuroimmune Pathways: By reducing systemic and neuroinflammation through cytokine modulation, particularly in glial cells (astrocytes and microglia) implicated in Alzheimer's disease pathology [107].
Neuroendocrine Pathways: Influencing the hypothalamic-pituitary-adrenal (HPA) axis stress response and the production of gut hormones that can cross the blood-brain barrier.
Neural Pathways: Direct activation of the vagus nerve by gut-derived signals [107].
Microbial Metabolite Pathways: Production or direct provision of neuroactive metabolites (GABA, serotonin, dopamine) and SCFAs that can directly or indirectly influence brain function [107] [111].
The following diagram illustrates the integrated gut-brain axis pathways:
Diagram 3: Gut-Brain Axis Modulation (63 characters)
Table 2: Comparative Mechanisms of Action
| Mechanism | Prebiotics | Postbiotics |
|---|---|---|
| Primary Pathway | Indirect, through microbiota modulation | Direct, through host cell interactions |
| Microbiome Dependency | Essential for mechanism [108] | Not essential; can function independently [108] |
| Key Metabolites | Stimulate endogenous SCFA production [109] | Deliver pre-formed metabolites [110] |
| Immune Modulation | Indirect, via microbial metabolites | Direct, via microbial component-host receptor interactions [110] |
| Barrier Enhancement | Via butyrate-induced tight junction protein expression [107] | Direct effect on epithelial cells; competitive exclusion [110] |
| Onset of Action | Delayed (requires microbial growth) | Potentially immediate |
Clinical Evidence and Clinical Advantages
Therapeutic Applications and Clinical Evidence
Both prebiotics and postbiotics have demonstrated efficacy across various clinical conditions, with emerging evidence supporting their use as complementary therapeutic approaches.
Prebiotics in Clinical Practice:
- Mental Health: A 2025 randomized controlled trial investigating galacto-oligosaccharides (GOS) supplementation in young females (17-25 years) found that while it did not significantly reduce trait anxiety, it modulated neurochemical GABA levels in brain regions and increased Bifidobacterium abundance, indicating potential gut-brain axis effects [111].
- Constipation: Clinical studies demonstrate that prebiotics like inulin-type fructans significantly improve stool consistency and gut microbiota composition in constipated patients, with increases in beneficial Bifidobacterium longum and decreases in constipation-related bacteria [111].
- Allergic Disorders: A 2025 randomized trial in patients with lipid transfer protein (LTP) allergy to peach showed that esterified pectins (both low and high methoxyl) decreased inflammatory cytokines associated with allergic response (IL-13) and modulated gut microbiota, leading to significant improvements in allergen tolerance [111].
Postbiotics in Clinical Practice:
- Hyperuricemia: A 2024 study demonstrated that a heat-killed postbiotic from Pediococcus acidilactici GQ01 effectively treated hyperuricemia in mice by inhibiting xanthine oxidase activity, upregulating kidney ABCG2 transporters, promoting uric acid excretion, and restoring healthy gut microbiota structure [112].
- Animal Health Applications: Postbiotics have shown significant benefits in animal health, enhancing disease resistance in aquatic animals, improving intestinal health and meat quality in broiler chickens, and promoting nutrient absorption in ruminants [110]. In weaned lambs, postbiotic L. plantarum RG14 improved rumen papilla growth, immune status, antioxidant capacity, and growth performance [110].
- General Health: Postbiotics exhibit potential for anti-allergy applications, prevention of respiratory/digestive tract infections, adjunct therapy for cancer, and improvement of liver cirrhosis [110].
Comparative Clinical Advantages
Table 3: Comparative Clinical and Practical Advantages
| Parameter | Prebiotics | Postbiotics |
|---|---|---|
| Safety Profile | Generally safe; may cause bloating initially | Superior safety; no risk of infection or gene transfer [110] |
| Stability & Shelf Life | Generally stable | Excellent stability; no viability concerns [110] |
| Production Requirements | Standard manufacturing | No need to maintain viability; simpler production [110] |
| Applicable Populations | General population; may not suit severe dysbiosis | Immunocompromised, critically ill, allergic individuals [110] |
| Onset of Action | Gradual (days to weeks) | Potentially faster (hours to days) |
| Dose Precision | Variable due to microbiome differences | More predictable and precise dosing |
| Regulatory Status | EFSA-approved claims for some (e.g., inulin) [6] | Emerging regulatory framework |
Experimental Methodologies and Research Tools
Key Experimental Models and Protocols
Research in the biotic field employs a multi-faceted approach utilizing various experimental models to elucidate mechanisms and therapeutic potential.
In Vitro Digestion and Fermentation Models: These systems simulate human gastrointestinal conditions to assess the stability, digestibility, and fermentability of prebiotics and postbiotics. Static models (e.g., INFOGEST) offer a rapid, cost-effective screening tool, while dynamic models (e.g., TIM, SHIME) provide more physiologically relevant conditions with continuous pH adjustment, metabolite removal, and gradual transit [112]. These models are particularly valuable for studying the degradability of microbial polysaccharides and their effects on intestinal health [112].
Encapsulation Techniques for Enhanced Stability: Research has demonstrated that encapsulation methods significantly impact the stability and delivery of biotic compounds. Calcium alginate encapsulation combined with hydrocolloids (gelatin, carrageenan) has been shown to boost Lactobacillus rhamnosus GG viability and phenolic content retention in fermented foods compared to alginate alone [112]. The choice of encapsulation material also affects survival through simulated digestion, with calcium alginate-gelatin beads showing the highest probiotic survival rates [112].
Animal Models: Animal studies remain crucial for evaluating mechanistic pathways and efficacy before human trials. Key protocols include:
- Allergy Models: Ovalbumin-induced allergic mice models demonstrate anti-allergic effects of biotic interventions through measurement of allergy scores, serum OVA-sIgE, cytokine expression (IL-4, IL-5, IL-10, IFN-γ, IL-2), and intestinal flora analysis [112].
- Metabolic Disease Models: High-fat diet-induced obesity models in C57BL/6J mice assess anti-obesity effects through monitoring of weight gain, liver/fat indexes, hyperlipidemia, serum triglycerides, liver enzymes (ALT/AST), inflammatory cytokines (TNF-α, IL-1β), and lipid metabolism gene expression (ACC1, PPAR-γ, SREBP-1, Fasn) [112].
- Neurodegenerative Disease Models: Transgenic Alzheimer's models evaluate gut-brain axis modulation through assessment of neuropathological markers (beta-amyloid plaques, neurofibrillary tangles), neuroinflammation, microglial activation, and cognitive behavioral tests [107].
Human Clinical Trial Designs: Recent advances in clinical trial methodology for biotics include:
- Randomized Controlled Trials (RCTs): The gold standard for efficacy evaluation, typically employing double-blind, placebo-controlled designs with parallel or crossover arms [111].
- Multi-omics Approaches: Integration of metagenomic shotgun sequencing (for microbiome composition), metabolomic profiling (for SCFAs, bile acids, neurotransmitters), and proteomic/transcriptomic analyses to provide comprehensive mechanistic insights [111].
- Neuroimaging Integration: Advanced techniques like proton magnetic resonance spectroscopy (H-MRS) to measure neurochemical changes (e.g., GABA levels) in response to intervention, particularly in gut-brain axis studies [111].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents and Materials
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Prebiotic Substrates | Selective stimulation of beneficial microbiota | Galacto-oligosaccharides (GOS) [111], Fructo-oligosaccharides (FOS), Inulin-type fructans (ITFs) [109], Esterified pectins (LMP, HMP) [111] |
| Postbiotic Preparations | Source of inanimate microbes/components | Heat-killed Lactobacillus acidophilus LB [109], Heat-killed Bifidobacterium bifidum MIMBb75 [109], Pasteurized Akkermansia muciniphila [109], Cell-free supernatants [110] |
| Encapsulation Matrices | Enhanced stability and targeted delivery | Calcium alginate, Gelatin, Carrageenan [112] |
| In Vitro Digestion Models | Simulating GI conditions for stability assessment | INFOGEST (static), TIM system (dynamic), SHIME (fermentation) [112] |
| Cell Culture Models | Mechanistic studies of host-microbe interactions | Caco-2 (intestinal epithelium), HT-29, IPEC-J2, Primary immune cells [110] |
| Analytical Standards | Quantification of microbial metabolites | SCFA standards (acetate, propionate, butyrate), Bile acids, Neurotransmitters (GABA, serotonin) [111] |
| DNA Extraction Kits | Microbiome composition analysis | Kits optimized for fecal samples, with bead-beating for Gram-positive bacteria |
| Cytokine Assays | Immune response evaluation | ELISA, Multiplex immunoassays for TNF-α, IL-1β, IL-4, IL-5, IL-6, IL-8, IL-10, IL-13 [111] [112] |
The comparative analysis of prebiotics and postbiotics reveals two distinct but complementary approaches to modulating the gut microbiome and promoting host health. Prebiotics function through selective stimulation of indigenous beneficial microbiota, resulting in the production of health-promoting metabolites like SCFAs. Their effects are inherently dependent on the existing microbial ecosystem and develop gradually as the microbial community restructures itself. In contrast, postbiotics provide more direct intervention through pre-formed microbial components and metabolites that can immediately engage with host signaling pathways, independent of the resident microbiota.
The clinical advantages of each approach must be considered within the context of the target population and desired outcomes. Postbiotics offer significant practical benefits in terms of safety (particularly for immunocompromised individuals), stability, and precise dosing, making them attractive candidates for pharmaceutical development. Prebiotics, while requiring a functioning microbial ecosystem for efficacy, provide a more natural approach to gradually shifting the microbial community toward a healthier state and may be particularly suitable for long-term preventive strategies.
Future research directions should focus on elucidating the precise molecular mechanisms of both interventions, particularly their effects on specific host receptors and signaling pathways. Additionally, more head-to-head clinical trials comparing prebiotics and postbiotics in specific patient populations are needed to establish evidence-based guidelines for their application. The development of personalized approaches based on individual microbiome profiles represents perhaps the most promising frontier, enabling the matching of specific biotic interventions to patient characteristics for optimized therapeutic outcomes.
As the field advances, both prebiotics and postbiotics are poised to play increasingly important roles in the therapeutic arsenal, potentially revolutionizing approaches to managing a wide range of microbiome-associated diseases and promoting overall health.
The human gut microbiome, a complex ecosystem of bacteria, fungi, archaea, and viruses, has emerged as a critical regulator of systemic immunity and a promising determinant of therapeutic response [113]. With the rapid integration of immunotherapies, particularly immune checkpoint inhibitors (ICIs), into standard cancer treatment, the substantial inter-patient variation in treatment efficacy has created an urgent need for reliable predictive biomarkers [114]. Current biomarkers, including PD-L1 expression and tumor mutational burden (TMB), suffer from limitations such as assay heterogeneity and sampling bias [114]. The gut microbiome, containing up to 60-70% of the body's peripheral immune cells and interacting with a substantial number of microbiota, represents the largest peripheral immune organ [113]. This technical review examines the evidentiary foundation for the microbiome as a predictive biomarker, detailing specific microbial taxa, analysis methodologies, mechanistic pathways, and therapeutic applications, with a specific focus on advancing gut microbiome health-disease association research.
Microbial Signatures as Predictive Biomarkers
Clinical and preclinical studies have consistently demonstrated that specific microbial compositions and diversity metrics correlate significantly with immunotherapy outcomes. The predictive value stems from both viral status and specific bacterial communities.
Viral Signatures and ICI Response
A comprehensive meta-analysis of 71 studies (41 viral, 30 bacterial) revealed that viral status, particularly hepatitis B virus (HBV) and human papillomavirus (HPV), significantly associates with improved objective response rate (ORR) and disease control rate (DCR) in patients undergoing ICI treatment [115]. The pooled relative risk (RR) across 34 cohorts was 1.29 (95% CI: 1.07–1.55, P = 0.049), indicating a significant association between baseline microbiota and ICI efficacy [115]. Subgroup analysis demonstrated a pooled RR of 1.28 (95% CI: 1.11–1.47, P < 0.001) for virus-related cohorts, with lower heterogeneity (I² = 47.9%), establishing baseline viral status as a critical predictor of ICI response [115].
Table 1: Viral Associations with ICI Treatment Response
| Viral Factor | Associated Cancers | Impact on ICI Response | Reported Effect Size (RR/HR) |
|---|---|---|---|
| Hepatitis B Virus (HBV) | Hepatobiliary Cancers | Significant association with ORR and DCR | RR = 1.28 (95% CI: 1.11–1.47) [115] |
| Human Papillomavirus (HPV) | Not Specified | Significant association with ORR and DCR | RR = 1.28 (95% CI: 1.11–1.47) [115] |
| Viral Status (General) | Multiple | Enhanced response to single-agent ICI therapy | RR = 1.40 (95% CI: 1.23–1.60) [115] |
Bacterial Signatures and ICI Response
Specific bacterial taxa are enriched in patients responding to ICIs, with effects varying by cancer type and ICI regimen. Multi-microbiome models demonstrate superior outcome prediction compared to single-taxon approaches, with microbial diversity correlating with improved progression-free survival (PFS hazard ratio [HR] = 0.64, 95% CI: 0.42–0.98) [115]. Bacterial enrichment is particularly impactful in specific cancers, with hepatobiliary cancers showing a hazard ratio of 4.33 (95% CI: 2.20–8.50) for overall survival (OS), and lung cancer demonstrating a PFS HR of 1.70 (95% CI: 1.04–2.78) [115].
Table 2: Bacterial Taxa Associated with Enhanced ICI Response
| Bacterial Taxa | Associated Cancer Types | Therapy Context | Proposed Mechanism |
|---|---|---|---|
| Akkermansia muciniphila | Non-Small Cell Lung Cancer (NSCLC), Renal Cell Carcinoma (RCC), Hepatocellular Carcinoma (HCC) | Anti-PD-1/PD-L1 [113] | Immune cell recruitment and activation [113] |
| Bifidobacterium spp. | Melanoma | Anti-PD-L1, Anti-CTLA-4 [113] | Dendritic cell maturation, CD8+ T cell activation [113] |
| Bacteroides fragilis | Melanoma | Anti-CTLA-4 [113] | Th1 cell activation in lymph nodes [113] |
| Coriobacteriaceae | Melanoma | Anti-PD-1 [113] | Not Specified |
| Ruminococcaceae | Melanoma | Anti-PD-1 [113] | Not Specified |
| Lachnospiraceae | Melanoma | Anti-PD-1 [113] | Not Specified |
| Faecalibacterium spp. | Multiple Cancers | Anti-PD-1/PD-L1 [115] | Promotion of anti-tumor immunity; associated with improved PFS [115] |
| Bifidobacterium longum | Melanoma | Anti-PD-1 [113] | Not Specified |
| Collinsella aerofaciens | Melanoma | Anti-PD-1 [113] | Not Specified |
| Enterococcus faecium | Melanoma | Anti-PD-1 [113] | Not Specified |
Mechanisms of Microbiome-Mediated Immunomodulation
The gut microbiome influences systemic antitumor immunity through multiple interconnected mechanisms, primarily involving microbial components and metabolites that directly and indirectly modulate host immune responses.
Direct Immune Stimulation
Microbial structural components directly stimulate pattern recognition receptors on immune cells. For example, Bacteroides fragilis stimulates Th1 cell activation in tumor-draining lymph nodes, enhancing intra-tumoral dendritic cell maturation and anti-CTLA-4 efficacy [113]. Similarly, bacterial lipopolysaccharide (LPS) activates the Toll-like receptor (TLR)-4 pathway, which is crucial for the effectiveness of adoptive cell transfer therapies [113].
Metabolite-Mediated Regulation
Microbial metabolites significantly shape immune responses. Short-chain fatty acids (SCFAs) and bile acids (BAs) play crucial roles in shaping both innate and adaptive immune responses [113]. These metabolites can influence immune cell differentiation, function, and trafficking, thereby altering the tumor microenvironment and enhancing T-cell infiltration and activity [113] [114]. A multi-omics approach characterized five response-associated gut phenotypes, identifying specific metabolites like phenylethyl fluoride that were negatively associated with response and shown to attenuate anti-PD-1 efficacy in vivo [113].
Diagram 1: Gut Microbiome Immunomodulation Pathways. This figure illustrates the primary mechanisms through which the gut microbiome influences response to immunotherapy.
Methodological Framework for Microbiome Analysis
Robust microbiome biomarker analysis requires standardized pipelines from sample collection through data interpretation. Variations at any step can significantly impact reproducibility and results.
Sample Collection and Processing
Multiple sample types can be utilized for microbiome profiling, each with distinct advantages and limitations [114].
Table 3: Sample Types for Microbiome Profiling in Immunotherapy Studies
| Sample Type | Advantages | Limitations | Primary Application |
|---|---|---|---|
| Fecal Samples | Non-invasive, gold standard for distal colon community, sufficient biomass [114] | Requires immediate cryopreservation at -80°C, standardization critical [114] | Primary biomarker discovery and validation |
| Oral Samples | Readily accessible [114] | Low microbial biomass, high human DNA contamination, site variability [114] | Exploratory biomarker studies |
| Tumor Tissue | Direct assessment of intratumoral microbiome, reveals host-tissue interactions [114] | Invasive procedure, technical complexity in analysis [114] | Mechanism investigation and niche-specific profiling |
| Direct Gut Sampling | Direct mucosal assessment, targeted location sampling [114] | Highly invasive, requires special preparation, not routine [114] | Specialized mechanistic studies |
Analytical Approaches: Sequencing and Quantification
Two primary sequencing approaches dominate microbiome research: 16S rRNA gene sequencing, a cost-effective method targeting a universal bacterial barcode gene, and shotgun metagenomics, which sequences all genetic material and provides higher resolution including strain-level and functional data [114]. A critical methodological consideration is the distinction between relative and absolute quantification. While relative abundance (proportion of each microbe) is the default sequencing output, it is prone to compositionality bias, where changes in one taxon artificially appear to change others [114]. Absolute abundance measurement, achieved through techniques like qPCR, flow cytometry, or spike-in standards, provides the actual microbial concentration and is essential for robust biological interpretation [114].
Diversity Metric Analysis and Interpretation
Alpha diversity metrics, describing within-sample diversity, should be selected and interpreted based on their mathematical foundations and biological relevance. These metrics can be categorized into four groups, each capturing different aspects of the microbial community [66].
Table 4: Key Alpha Diversity Metric Categories and Applications
| Metric Category | Representative Metrics | What It Measures | Clinical/Biological Interpretation |
|---|---|---|---|
| Richness | Chao1, ACE, Observed ASVs [66] | Number of distinct taxa (e.g., ASVs) in a sample | Higher richness often correlates with better ICI response [113] [115] |
| Dominance/Evenness | Berger-Parker, Simpson, ENSPIE [66] | Distribution uniformity of taxa abundances | Lower dominance (higher evenness) indicates balanced community |
| Phylogenetic Diversity | Faith's PD [66] | Evolutionary relationships among taxa | Captures phylogenetic breadth, influenced by ASV count and singletons [66] |
| Information Indices | Shannon, Brillouin, Pielou [66] | Combines richness and evenness into single value | Higher Shannon diversity associates with improved clinical outcomes [115] ``` |
Diagram 2: Microbiome Biomarker Analysis Workflow. This figure outlines the standard pipeline from sample collection to clinical correlation.
Therapeutic Modulation of the Microbiome
The established correlation between specific microbial features and treatment response has prompted the development of therapeutic strategies aimed at modulating the microbiome to enhance clinical outcomes.
Microbiome-Based Interventions
Fecal Microbiota Transplantation (FMT): FMT from ICI responders has demonstrated potential to overcome resistance in refractory melanoma patients. Initial clinical trials show that FMT, combined with anti-PD-1 therapy, can recondition the tumor microenvironment and restore therapeutic response [113] [114].
Probiotics and Prebiotics: Targeted supplementation with specific bacterial strains shows promise in enhancing ICI efficacy. Oral administration of Bifidobacterium was shown to enhance anti-PD-L1 efficacy by promoting dendritic cell maturation and increasing tumor-specific CD8+ T cell activity [113]. Prebiotics provide selective substrates to encourage growth of beneficial taxa.
Dietary Interventions: Nutritional strategies modulate microbial composition and metabolite production, potentially creating a favorable environment for immunotherapy response [113]. These interventions represent a non-invasive approach to microbiome modulation.
Engineered Microbial Strains: Synthetic biology approaches are developing engineered microbial strains designed to deliver specific immunomodulatory compounds directly to the tumor microenvironment [114].
The Scientist's Toolkit: Essential Research Reagents
Table 5: Key Research Reagent Solutions for Microbiome-Immunotherapy Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Sample Preservation | Commercial preservation buffers, Cryostorage at -80°C [114] | Maintains microbial integrity post-collection | Critical for reproducible results; standardization essential [114] |
| DNA Extraction Kits | Qiagen DNeasy PowerSoil, MoBio PowerLyzer [67] | Isolation of high-quality microbial DNA | Must efficiently lyse diverse bacterial cell walls |
| Sequencing Platforms | Illumina (16S, Shotgun), Third-generation sequencing [113] | Microbiome profiling and community analysis | Shotgun provides strain-level resolution and functional genes [114] |
| Spike-in Standards | Synthetic microbial cells, Reference DNA [114] | Enables absolute quantification | Mitigates compositionality bias; essential for robust quantification [114] |
| Bioinformatic Tools | QIIME 2, DADA2, DEBLUR [67] [66] | Processing raw sequences into ASV/OTU tables | DEBLUR preserves singletons needed for some diversity metrics [66] |
| Cell Culture Media | Anaerobic culture systems, Gnotobiotic media [113] | Culturing specific bacterial strains | Anaerobic conditions essential for obligate anaerobes |
| Animal Models | Germ-free mice, Gnotobiotic models [113] | In vivo mechanistic validation | FMT from human responders into mice validates causal relationships [113] |
The gut microbiome has firmly established itself as a significant biomarker for predicting response to immunotherapy and other treatments. The integration of microbiome data with established biomarkers like PD-L1 and TMB represents a promising path toward more precise patient stratification. Future research must prioritize standardized methodologies, absolute quantification approaches, and large-scale randomized controlled trials to translate these findings into clinical practice. As our understanding of host-microbiome interactions deepens, targeted modulation of the gut ecosystem through FMT, probiotics, dietary interventions, or engineered microbes offers a compelling therapeutic strategy to enhance immunotherapy efficacy and expand its benefit to more patients.
The human gut microbiome, a complex ecosystem of bacteria, archaea, fungi, and viruses, is now recognized as a virtual organ that plays a critical role in health and disease. Comprising an estimated 10-100 trillion microorganisms in the gastrointestinal tract alone, its collective genetic material (the microbiome) exceeds human genomic content by a factor of at least 100 [116]. This "organ" performs myriad functions, including nutrient production, immune system regulation, energy homeostasis, and pathogen protection. However, dysbiosis—a deviation from a healthy microbial state—has been implicated in a wide range of diseases, including inflammatory bowel diseases, cancer, neuropsychiatric disorders, and cardiometabolic conditions [116]. The emerging frontiers of phage therapy, precision nutrition, and targeted delivery systems represent transformative approaches to modulating this ecosystem. These strategies leverage a deepening understanding of microbial ecology and host-microbe interactions to develop novel interventions for complex diseases, positioning the gut microbiome as a central target for next-generation therapeutics.
Phage Therapy: Harnessing Bacterial Viruses
Fundamental Principles and Mechanisms
Bacteriophages (phages) are viruses that specifically infect and replicate within bacterial hosts. The term "bacteriophage" derives from "bacteria" and the Greek word "phagein," meaning "to devour" [117]. They are the most abundant biological entities on Earth, with an estimated 10^31 phages inhabiting the planet [117]. Phages exhibit highly specific targeting, often infecting only particular strains within a bacterial species. Their basic structure typically includes a protein capsid enclosing their nucleic acid genome (which can be DNA or RNA, single or double-stranded) and a tail structure that serves as a delivery apparatus [117].
Phages initiate infection by binding to specific receptors on the bacterial cell surface, then inject their genetic material into the host cytoplasm. Once inside, they follow one of two replication pathways:
- Lytic Cycle: The phage immediately hijacks the host's cellular machinery to synthesize viral components, assembling new phage particles that are released through cell lysis, destroying the host bacterium [117] [118].
- Lysogenic Cycle: The phage integrates its DNA into the bacterial chromosome (becoming a prophage) and replicates passively with the host cell. Environmental stressors can trigger a switch to the lytic cycle [117] [118].
Therapeutic applications primarily utilize lytic phages due to their direct bactericidal activity.
Advancements in Clinical Applications
Phage therapy has demonstrated notable efficacy against multidrug-resistant (MDR) infections, which are now the second leading cause of mortality globally, surpassed only by ischemic heart disease [118]. Clinical reports indicate efficacy rates of 50%-70% with an excellent safety profile [118]. The table below summarizes key clinical evidence:
| Infection Type | Causative Pathogen | Therapeutic Approach | Reported Outcome | Source |
|---|---|---|---|---|
| Diabetic Foot Ulcers | Staphylococcus aureus | Topical phage preparation | Six patients recovered from antibiotic-resistant infections | [117] |
| CRAB Pneumonia | Acinetobacter baumannii | Monophage therapy | Precise eradication while conserving commensal microbiota | [118] |
| Diverse Infections (100 patients) | P. aeruginosa, E. coli, etc. | Phage-Antibiotic Combination | 70% superior eradication rates vs. monotherapy | [118] |
| Burn Wound Infections | Acinetobacter baumannii | Phage-loaded hydrogel | Significantly accelerated wound healing and bacterial clearance in murine models | [117] |
Therapeutic modalities have evolved to include:
- Monophage Therapy: Uses a single phage type for targeted infections with well-defined pathogens [118].
- Phage Cocktails: Mixtures of different phages that target multiple bacterial receptors or species, broadening therapeutic coverage and reducing resistance emergence [117] [118].
- Phage-Antibiotic Synergy (PAS): Combines phages with antibiotics, where phages can disrupt biofilms and resensitize bacteria to conventional drugs [117] [118].
- Bacteriophage-Derived Enzymes: Endolysins and depolymerases directly lyse bacterial cells or degrade surface polysaccharides, rarely inducing resistance [118].
Experimental Protocols and Methodologies
A. Phage Experimental Evolution for Broadened Host Range
Purpose: To enhance phage ability to kill diverse bacterial strains, including multidrug-resistant variants. Methodology (as implemented for Klebsiella pneumoniae [119]):
- Co-culture: Phages and bacteria are cultivated together in a controlled laboratory setting for an extended period (e.g., 30 days).
- Selective Pressure: The system allows phages to continuously adapt to evolving bacterial defenses.
- Genetic Analysis: Evolved phages are sequenced to identify mutations, particularly in genes responsible for host recognition and binding. Outcome: Significant improvements in the phage's lytic capability against a wide spectrum of bacterial strains and enhanced suppression of bacterial growth over time.
B. Isolation and Characterization of Temperate Gut Phages
Purpose: To study dormant (temperate) phages in the human gut and identify factors that reactivate them [62]. Methodology:
- Sample Source: Bacterial isolates are sourced from curated collections (e.g., Australian Microbiome Culture Collection).
- Anaerobic Culture: Bacteria are grown in specialized anaerobic chambers to mimic the gut environment.
- Induction Screening: Cultures are exposed to diverse compounds (e.g., sweeteners like Stevia, host-derived molecules).
- Activation Assessment: Phage activation is measured, with a focus on responses to compounds derived from human gut cells.
- CRISPR Engineering: Used to identify viral gene mutations that prevent activation, informing therapeutic design.
Key Signaling Pathways and Workflows
The following diagram illustrates the core decision-making workflow for implementing phage therapy, from diagnosis to treatment monitoring:
Precision Nutrition: Dietary Modulation of the Microbiome
Core Principles and Mechanistic Insights
Precision nutrition is an emerging field that tailors dietary interventions to an individual's unique biological profile, including their gut microbiome. This approach recognizes that interpersonal differences in microbial composition and functionality create highly individualized responses to dietary inputs [120]. The gut microbiome serves as a critical intermediary between diet and disease, particularly in cancer, where microbial communities can act as both biomarkers for early detection and active participants in carcinogenesis [120].
Key mechanisms linking diet, microbiome, and health include:
- Short-Chain Fatty Acid (SCFA) Production: Beneficial gut bacteria ferment dietary fiber to produce SCFAs (butyrate, acetate, propionate), which regulate immune function, maintain intestinal barrier integrity, and exhibit anti-inflammatory effects [121] [116] [120].
- Microbial Metabolite Signaling: Gut microbes transform dietary components and host-derived compounds into bioactive molecules that can influence host metabolism, immunity, and even cancer progression [116] [120].
- Pathogen Inhibition: A healthy, diverse microbiome provides colonization resistance against pathogens through competitive exclusion and production of antimicrobial compounds [116].
Impact of Specific Dietary Components
Research has elucidated how specific dietary patterns and components shape the gut microbiome and influence disease risk:
| Dietary Component | Microbial Shifts | Functional Consequences | Health Associations |
|---|---|---|---|
| Dietary Fiber | Enriches SCFA-producers (e.g., Faecalibacterium prausnitzii, Roseburia spp.) [120] | Enhanced gut barrier integrity; reduced inflammation; strengthened anti-tumor immunity [121] [120] | Reduced colorectal cancer risk; improved checkpoint inhibitor efficacy [120] |
| Fermented Foods | Variable impacts on microbial diversity [121] | Potential immunomodulation; improved gut health (limited high-quality evidence) [121] | Cardiometabolic health (kefir); digestive health (anecdotal) [121] |
| High-Fat/Western Diet | Favors pro-inflammatory, genotoxin-producing microbes [120] | Increased gut permeability; systemic inflammation; impaired treatment response [116] [120] | Promotes tumor progression; linked to metabolic diseases [116] [120] |
| Ketogenic Diet | Reduces pathogenic Th17 cells in intestine [120] | Alters immune cell populations in tumor microenvironment | Potential adjunct in cancer therapy [120] |
The AI-Powered Digital Gut Twin
A groundbreaking development in precision nutrition is the Digital Gut Twin (DGT), a virtual replica of an individual's gastrointestinal ecosystem [120]. The DGT integrates patient-specific data—including microbiome composition, dietary habits, genomics, and clinical history—to simulate how that person's gut microbiota would respond to various dietary interventions.
Framework and Workflow:
- Data Integration: Multidimensional data (diet, microbiome, host omics, immune status) is aggregated.
- Modeling and Simulation: AI and systems biology models predict individual responses to dietary inputs.
- Intervention Optimization: The model identifies optimal, personalized diets to support clinical outcomes, such as enhancing cancer therapy efficacy or reducing side effects.
The diagram below visualizes the data integration and predictive workflow of a Digital Gut Twin:
Targeted Delivery Systems for Colonic Health
Technological Approaches and Formulations
Targeted drug delivery systems (DDS) are engineered to release therapeutic agents at specific sites in the body at controlled rates, maximizing efficacy while minimizing systemic side effects. For colonic health, Colon-Targeted Drug Delivery Systems (CTDDS) enable localized therapy for disorders like inflammatory bowel disease (IBD) and colorectal cancer [122]. Recent advances include:
- pH-Dependent Systems: Utilize polymers that remain intact in the stomach's acidic environment but dissolve at the higher pH of the colon [122].
- Enzyme-Responsive Formulations: Designed to be degraded by specific enzymes (e.g., azoreductases, glycosidases) produced by the colonic microbiota [122].
- Time-Controlled Formulations: Engineered to delay drug release until the formulation reaches the colon, based on transit time [122].
- Advanced Methodologies: Emerging strategies include ligand/receptor-mediated targeting, pressure-controlled systems, osmotic-controlled systems, and the application of 3D printing technologies for precision fabrication [122].
Synergy with Microbiome-Targeted Therapies
Targeted delivery systems are particularly suited for microbiome-focused therapies because they can protect sensitive biologicals (e.g., phages, bacterial consortia, enzymes) from degradation in the upper GI tract and ensure their precise delivery to the colonic microbiome. For example, phage-loaded hydrogels represent a convergence of phage therapy and targeted delivery, providing a sustained-release system directly at the infection site, such as a wound [117]. Similarly, CTDDS can deliver precise combinations of prebiotics, probiotics, or phage-derived enzymes to reshape the microbial community in the colon [122].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs key reagents and materials essential for conducting research in the featured emerging frontiers.
| Reagent/Material | Primary Function | Research Application | Example Use Case |
|---|---|---|---|
| Phage DNA Isolation Kit | Purifies high-quality viral DNA from phage preparations | Genomic characterization and sequencing of bacteriophages | Used to assemble the complete 67,539 bp genome of phage Bm1 for therapeutic development [117] |
| Anaerobic Chamber | Creates an oxygen-free environment for microbial culture | Cultivation of obligate anaerobic gut bacteria and their associated phages | Essential for isolating and studying temperate phages from human gut samples [62] |
| Specialized Growth Media | Supports the propagation of fastidious gut microbes | Establishing complex microbial communities from fecal samples ex vivo | Used to culture donor-derived microbial communities for drug-microbiome interaction studies [7] |
| CRISPR-Cas9 Systems | Enables precise genetic manipulation | Functional genomics and engineering of therapeutic phages | Identifying viral genes controlling dormancy and engineering phages with enhanced host ranges [118] [62] |
| pH-Sensitive Polymers | Forms the capsule or matrix of colon-targeted formulations | Protects drug cargo until it reaches the specific pH of the colon | Core component of pH-dependent CTDDS for treating colonic disorders [122] |
Integrated Experimental Workflow: A Convergent Approach
The diagram below outlines a comprehensive experimental workflow that integrates concepts from phage therapy, precision nutrition, and targeted delivery to develop a novel microbiome-based therapeutic.
Conclusion
The convergence of advanced sequencing, functional validation, and ecological understanding is rapidly translating gut microbiome research into tangible therapeutic strategies. Key takeaways include the critical role of microbial metabolites in host physiology, the feasibility of targeting specific pathobionts with precision tools like phages, and the promising clinical outcomes of FMT and next-generation probiotics in areas like immuno-oncology. Future directions must focus on establishing causal mechanisms, developing universal standards for research and therapy production, and deeply personalizing interventions based on individual microbiome signatures. The integration of microbiome science into drug development pipelines promises a new era of microbiome-based diagnostics and therapeutics for a wide spectrum of human diseases.
References
- 1. Microbiota vs Microbiome: Key Differences [https://www.allucent.com/resources/blog/what-difference-between-microbiome-and-microbiota]
- 2. Microbiota in health and diseases [https://www.nature.com/articles/s41392-022-00974-4]
- 3. Microbiome Vs Microbiota - Know the Difference! [https://www.fiosgenomics.com/microbiome-vs-microbiota/]
- 4. A population-scale analysis of 36 gut microbiome studies ... [https://www.nature.com/articles/s41522-024-00567-9]
- 5. Comparing Published Gut Microbiome Taxonomic Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8740627/]
- 6. Nutrition & microbiome research highlights NeuroGASTRO ... [https://www.gutmicrobiotaforhealth.com/nutrition-and-microbiome-research-highlights-from-neurogastro-2025/]
- 7. Medications change our gut microbiome in predictable ways [https://news.stanford.edu/stories/2025/11/medications-gut-microbiome-bacteria-digestive-system-research]
- 8. The Association between Early-Life Gut Microbiota and Long ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7865818/]
- 9. The early-life gut microbiome in common pediatric diseases [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1597206/full]
- 10. Intestinal Microbiota in Early Life: Latest Findings ... [https://www.mdpi.com/2072-6643/17/13/2071]
- 11. Microbiome and Immune System Maturation in Infants and ... [https://brieflands.com/journals/archcid/articles/163648]
- 12. Characterizing the Composition of the Pediatric Gut Microbiome [https://pmc.ncbi.nlm.nih.gov/articles/PMC7019424/]
- 13. The Gut Microbiome, Aging, and Longevity - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7762384/]
- 14. Development of the gut microbiota in infancy and its impact ... [https://www.sciencedirect.com/science/article/pii/S1323893017301119]
- 15. Persistent reduction of Bifidobacterium longum in the infant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119681/]
- 16. Microbiome highlights from Digestive Disease Week 2025 [https://www.gutmicrobiotaforhealth.com/microbiome-highlights-from-digestive-disease-week-2025/]
- 17. Heterogeneity of Gut Spatial along the... Microbial Composition [https://pmc.ncbi.nlm.nih.gov/articles/PMC5036816/]
- 18. Frontiers | Enhanced metagenomic strategies for elucidating the... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1626002/full]
- 19. Innovative new tool helps understand how gut microbes ... [https://www.news-medical.net/news/20251120/Innovative-new-tool-helps-understand-how-gut-microbes-interact-to-influence-health.aspx]
- 20. Gut microbiome compositional and functional features ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12221809/]
- 21. The human gut microbiota is associated with host lifestyle [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1549160/full]
- 22. The Role of Short-Chain Fatty Acids From Gut Microbiota in ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.00025/full]
- 23. Health Benefits and Side Effects of Short-Chain Fatty Acids [https://pmc.ncbi.nlm.nih.gov/articles/PMC9498509/]
- 24. Gut Microbiome Integration in Drug Discovery and ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624011498]
- 25. Bile Acids and the Gut Microbiome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4215539/]
- 26. Microbiota-derived bile acid metabolic enzymes and their ... [https://www.sciencedirect.com/science/article/pii/S2772892725000392]
- 27. Metabolic and functional interplay between gut microbiota ... [https://pubmed.ncbi.nlm.nih.gov/32715724/]
- 28. Current understanding of dysbiosis in disease in human and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4838534/]
- 29. Defining dysbiosis and its influence on host immunity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4143175/]
- 30. Have you heard of "dysbiosis"? | Content for the lay public [https://www.biocodexmicrobiotainstitute.com/en/have-you-heard-dysbiosis]
- 31. Dysbiosis: What It Is, Symptoms, Causes, Treatment & Diet [https://my.clevelandclinic.org/health/diseases/dysbiosis]
- 32. Gut Microbial Dysbiosis - One Health Institute [https://onehealth.colostate.edu/2022/02/03/gut-microbial-dysbiosis/]
- 33. Analysis of the Human Gut Microbiome and Association ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3822013/]
- 34. Health and disease markers correlate with gut microbiome ... [https://www.nature.com/articles/s41467-020-18871-1]
- 35. Full-length 16S rRNA Sequencing Reveals Gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11912586/]
- 36. Characterization of the Gut Microbiome Using 16S or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4837688/]
- 37. 16S vs Metagenomics: What's the Difference? [https://www.cosmosid.com/blog/16s-vs-metagenomics-whats-the-difference/]
- 38. Comparison between 16S rRNA and shotgun sequencing in ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10621-7]
- 39. Shotgun metagenomics reveals interkingdom ... - Microbiome [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-023-01693-w]
- 40. 16S rRNA and metagenomic shotgun sequencing data ... [https://www.nature.com/articles/s41598-022-07995-7]
- 41. Comparative evaluation of 16S rRNA metagenomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10503327/]
- 42. Advancing Gut Microbiome Research: The Shift from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12010094/]
- 43. Integrated gut microbiome and metabolomics analysis ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1652915/full]
- 44. A Focus on Metagenomics, Metatranscriptomics, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388303/]
- 45. Metatranscriptomics-based metabolic modeling of patient ... [https://www.nature.com/articles/s41522-025-00823-6]
- 46. Metabolomics and metagenomics in mice reveal the role of ... [https://pubmed.ncbi.nlm.nih.gov/41234773/]
- 47. A Survey of Statistical Methods for Microbiome Data Analysis [https://www.frontiersin.org/journals/applied-mathematics-and-statistics/articles/10.3389/fams.2022.884810/full]
- 48. A guide to human microbiome research: study design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7469990/]
- 49. Host variables confound gut microbiota studies of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7677204/]
- 50. From big data and experimental models to clinical trials [https://www.sciencedirect.com/science/article/pii/S0092867425001072]
- 51. Microbiome confounders and quantitative profiling ... [https://www.nature.com/articles/s41591-024-02963-2]
- 52. A reconceptualized framework for human microbiome ... [https://www.nature.com/articles/s41467-025-61998-2]
- 53. What we need to know about the germ-free animal models [https://pmc.ncbi.nlm.nih.gov/articles/PMC10955174/]
- 54. Of men in mice: the development and application ... [https://www.nature.com/articles/s12276-020-0473-2]
- 55. Mouse Microbiota Models: Comparing Germ-Free Mice ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2018.01534/full]
- 56. Laboratory mice engrafted with natural gut microbiota ... [https://www.nature.com/articles/s41467-025-60554-2]
- 57. Using gnotobiotic mice to discover and validate ... [https://www.sciencedirect.com/science/article/pii/S1740675719300180]
- 58. Explainable artificial intelligence for microbiome data ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1348974/full]
- 59. Smart Microbiomes: How AI Is Revolutionizing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466996/]
- 60. AI in microbiomeâ€related healthcare - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11530995/]
- 61. Choosing the Perfect Way to Visualize Your Microbiome Data [https://bitesizebio.com/78637/visualize-microbiome-data/]
- 62. Human gut virus discoveries open new field of microbiome ... [https://hudson.org.au/news/new-human-gut-virus-discoveries-open-new-paths-to-studying-the-microbiome/]
- 63. A Consensus Statement on establishing causality ... [https://www.nature.com/articles/s41575-025-01041-3]
- 64. Causal Analysis Between Gut Microbes, Aging Indicator ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12266770/]
- 65. Causal discovery for the microbiome [https://www.sciencedirect.com/science/article/pii/S2666524722001860]
- 66. Key features and guidelines for the application of microbial ... [https://www.nature.com/articles/s41598-024-77864-y]
- 67. Exploring the Microbiome Analysis and Visualization Landscape [https://pmc.ncbi.nlm.nih.gov/articles/PMC9580862/]
- 68. Principles and Recommendations for Standardizing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5417043/]
- 69. Reporting guidelines for Human Microbiome Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC9105086/]
- 70. Functional equivalence of genome sequencing analysis ... [https://www.nature.com/articles/s41467-018-06159-4]
- 71. Data harmonization: Steps and best practices [https://datavid.com/blog/data-harmonization]
- 72. A Guide to Developing Harmonized Research Workflows in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12233188/]
- 73. Standardization and quality management in next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5025460/]
- 74. The relationship between gut microbiome and human ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1516010/full]
- 75. New Study Links Gut Microbes to Common Heart Disease [https://asm.org/press-releases/2025/november/new-study-links-gut-microbes-to-common-heart-disea]
- 76. The Gut Microbiome as a Possible Mediator in ... [https://www.sciencedirect.com/science/article/abs/pii/S000294402500358X]
- 77. Common medications may secretly rewire your gut for years [https://www.sciencedaily.com/releases/2025/10/251008030953.htm]
- 78. Non-Antibiotic Drugs Also Disrupt the Microbiome [https://medicine.yale.edu/news-article/non-antibiotic-drugs-also-disrupt-the-microbiome/]
- 79. Microbiota in Health and Disease - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471161/]
- 80. AI maps how a new antibiotic targets gut bacteria [https://news.mit.edu/2025/ai-maps-how-new-antibiotic-targets-gut-bacteria-1003]
- 81. The challenges and opportunities in the expanding horizons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584655/]
- 82. Advancing therapeutic strategies for graft-versus-host disease ... [https://molmed.biomedcentral.com/articles/10.1186/s10020-024-01060-x]
- 83. The microbiome in graft-versus-host disease: a tale of two ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291514/]
- 84. Reversible engraftment of an engineered microbe in the ... [https://www.nature.com/articles/s41587-025-02790-x]
- 85. Phage Therapy as a Novel Alternative to Antibiotics Through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562026/]
- 86. Revisiting the application, current trends, and prospect of ... [https://link.springer.com/article/10.1007/s44187-025-00472-w]
- 87. Expanding Layers of Bacteriocin Applications: From Food ... [https://www.mdpi.com/2311-5637/11/3/142]
- 88. Gut Microbiome Influences Proteins That Drive Aging and ... [https://www.aging-us.com/news-room/gut-microbiome-influences-proteins-that-drive-aging-and-disease]
- 89. Current Applications and the Future of Phage Therapy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189447/]
- 90. a comprehensive review of bacteriocins in the food industry [https://pubmed.ncbi.nlm.nih.gov/40259615/]
- 91. Present and future of microbiome-targeting therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12126222/]
- 92. Alternatives to antibiotics in the fight against superbugs [https://www.weforum.org/stories/2025/10/this-regulatory-shift-is-unlocking-alternatives-to-antibiotics-in-the-fight-against-superbugs/]
- 93. Fecal microbiota transplantation: Current evidence and ... [https://www.ccjm.org/content/92/7/421]
- 94. Fecal Microbiota Transplantation for Immune Regulation [https://pubmed.ncbi.nlm.nih.gov/40592776/]
- 95. Efficacy of Fecal Microbiota Transplantation (FMT) Versus ... [https://pubmed.ncbi.nlm.nih.gov/40978956/]
- 96. Ferring Presents New Data Analyses for REBYOTA® (fecal ... [https://ferringusa.com/?press=ferring-presents-new-data-analyses-for-rebyota-fecal-microbiota-live-jslm-at-acg-2025]
- 97. Real-world Effectiveness of Fecal Microbiota ... [https://www.sciencedirect.com/science/article/pii/S1542356524005147]
- 98. Fecal microbiota transplantation: application scenarios ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1556827/full]
- 99. Fecal microbiota transplantation to enhance cancer ... [https://www.sciencedirect.com/science/article/pii/S0305737225001471]
- 100. Next generation probiotics for human health: An emerging ... [https://www.sciencedirect.com/science/article/pii/S2405844024120117]
- 101. Akkermansia muciniphila: a microbial guardian against ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07149-z]
- 102. Gut microbiome engineering with probiotics: current trends ... [https://link.springer.com/article/10.1007/s42452-025-07622-w]
- 103. The worldview of Akkermansia muciniphila, a bibliometric ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1500893/full]
- 104. Probiotic Engraftment of Akkermansia muciniphila in an In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619756/]
- 105. Microbiome Therapeutics Market Size 2025 to 2034 [https://www.precedenceresearch.com/microbiome-therapeutics-market]
- 106. Probiotics, prebiotics, and postbiotics in health and disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC10625129/]
- 107. The role of probiotics, prebiotics, and postbiotics: cellular ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1598011/full]
- 108. The microbiome: An actor or stage for the beneficial action ... [https://www.sciencedirect.com/science/article/abs/pii/S1931312825001507]
- 109. A Review of the Influence of Prebiotics, Probiotics ... [https://www.mdpi.com/2077-0383/14/11/3673]
- 110. Current research status and trends in the bioactivity of ... [https://www.frontiersin.org/journals/food-science-and-technology/articles/10.3389/frfst.2025.1692683/full]
- 111. What's the Latest in Prebiotic Research? – October 2025 ... [https://prebioticassociation.org/whats-the-latest-in-prebiotic-research-october-2025-edition/]
- 112. Probiotics, Prebiotics, Synbiotics, Postbiotics, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346543/]
- 113. Gut microbiota shapes cancer immunotherapy responses [https://www.nature.com/articles/s41522-025-00786-8]
- 114. The Gut Microbiome as a Biomarker and Therapeutic ... [https://www.mdpi.com/2073-4409/14/22/1779]
- 115. Microbiome meets immunotherapy: unlocking the hidden ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405452/]
- 116. Precision Nutrition and the Microbiome, Part I - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6520976/]
- 117. Phage Therapy: The Future of Fighting Antibiotic Resistance [https://norgenbiotek.com/blog/phage-therapy-future-fighting-antibiotic-resistance?srsltid=AfmBOoq7LhKADkYXY0bC0SxLK6PYj0_2cgDy89xgcTQkqodfHMyy-YX9]
- 118. Phage therapy as a revitalized weapon for treating clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540056/]
- 119. UC San Diego Researchers Expand Virus-Based Treatment ... [https://today.ucsd.edu/story/uc-san-diego-researchers-expand-virus-based-treatment-options-for-antibiotic-resistant-infections]
- 120. Precision nutrition and the gut microbiome: Harnessing AI ... [https://www.sciencedirect.com/science/article/abs/pii/S1931312825001945]
- 121. How to Improve Your Gut Health and Microbiome [https://www.precisionnutrition.com/how-to-improve-gut-health]
- 122. Exploring Recent Advances in Colon-targeted Drug ... [https://pubmed.ncbi.nlm.nih.gov/41082057/]