Validating Microbiome Analysis: From Consensus Standards to Clinical Translation
This article synthesizes current international consensus and best practices for validating microbiome analysis approaches, targeting researchers and drug development professionals.
Validating Microbiome Analysis: From Consensus Standards to Clinical Translation
Abstract
This article synthesizes current international consensus and best practices for validating microbiome analysis approaches, targeting researchers and drug development professionals. It explores the foundational principles of microbiome science, evaluates methodological pipelines from 16S rRNA to multi-omics technologies, addresses critical troubleshooting and optimization challenges in standardization, and establishes validation frameworks for comparative analysis. By integrating the latest evidence from clinical practice, drug development pipelines, and analytical benchmarking studies, this resource provides a comprehensive roadmap for implementing robust, reproducible microbiome analysis that bridges the gap between research findings and clinical application.
Establishing the Groundwork: Core Concepts and Evolving Definitions in Microbiome Science
In microbiome research, the terms "microbiome" and "microbiota" are frequently used interchangeably, creating confusion within the scientific community and in literature. However, these terms represent distinct concepts with important differences in scope and meaning. A precise understanding of this terminology is fundamental for rigorous scientific communication, especially in the context of validating consensus approaches for microbiome analysis. This guide provides a detailed comparison of these core concepts, tracing their historical development and contextualizing them within contemporary analytical frameworks. Establishing this conceptual clarity is essential for researchers, scientists, and drug development professionals working to standardize methodologies and interpret data across studies.
Core Definitions and Conceptual Distinctions
Defining Microbiota and Microbiome
The fundamental distinction lies in the scope of each term. Microbiota refers specifically to the community of living microorganisms themselves—the bacteria, archaea, fungi, algae, and small protists—inhabiting a defined environment [1] [2] [3]. In contrast, the microbiome encompasses a broader ecological landscape, including not only the microorganisms but also their "theatre of activity" [4] [5] [3]. This comprises their structural elements (e.g., microbial and host), metabolites, mobile genetic elements, and the surrounding environmental conditions [1] [2]. In essence, the microbiota constitutes the living inhabitants, while the microbiome represents the entire habitat, including the inhabitants, their functions, and their interactions.
Table 1: Comparative Analysis of Microbiota and Microbiome
| Feature | Microbiota | Microbiome |
|---|---|---|
| Core Definition | The community of living microorganisms in a defined environment [1] [2] | The entire habitat, including microorganisms, their activities, and the environmental conditions [4] [3] |
| Composition | Bacteria, Archaea, Fungi, Protists [1] [3] | Microbiota, their genomes, metabolites, and the surrounding environment [1] [2] |
| Genetic Focus | Not applicable to the term itself | Includes the collective genetic material (metagenome) of the community [1] [6] |
| Key Scope | Taxonomic composition and abundance of organisms [2] | Structural and functional ecology of the microbial niche [4] [5] |
The "Theatre of Activity": Understanding the Microbiome's Breadth
The phrase "theatre of activity," originating from the influential 1988 definition by Whipps et al., is crucial for understanding the microbiome's comprehensive nature [4] [5] [3]. It signifies that the microbiome includes:
- The Microorganisms: The entire cast of microbial players (the microbiota).
- Their Genomic Blueprints: The collective genetic information (the metagenome) that dictates functional potential [1].
- Their Metabolic Outputs: The molecules produced and consumed, such as nutrients, signaling molecules, and waste products.
- The Environmental Stage: The surrounding physicochemical conditions that shape and are shaped by the microbial community.
This holistic view positions the microbiome as a dynamic, interactive system rather than merely a list of inhabitants.
Visualizing the Conceptual Relationship
The following diagram illustrates the hierarchical relationship between the key concepts of microbiota, metagenome, and microbiome, showing how they collectively form a functional ecological unit.
Historical Evolution of the Concepts
Key Milestones in Microbiome Research
The field of microbiome research did not emerge in a vacuum; it evolved from centuries of microbiological discovery, driven by technological innovation and paradigm shifts in understanding microbes' roles in health and disease. The following timeline captures the pivotal moments in this scientific journey.
Table 2: Historical Timeline of Key Concepts and Discoveries
| Year(s) | Key Figure(s) | Conceptual or Technological Advancement | Significance |
|---|---|---|---|
| 1670s | Antonie van Leeuwenhoek [3] | Discovery of microorganisms using first microscopes [4] [3] | Revealed the previously invisible world of microbes |
| 1880s | Robert Koch [3] | Koch's postulates linking microbes to disease [4] [3] | Established medical microbiology; focus on pathogens |
| 1888-1920s | Sergei Winogradsky [5] [3] | Founded microbial ecology; studied nitrification and chemosynthesis [4] [5] | Paradigm shift to beneficial environmental microbes and communities |
| 1988 | Whipps et al. [5] | First formal definition of the "microbiome" [4] [5] [3] | Introduced holistic concept of microbes plus their "theatre of activity" |
| 1977 | Carl Woese & George Fox [4] [3] | 16S rRNA gene as a phylogenetic marker [4] [3] | Enabled cultivation-independent community analysis |
| 2001 | Lederberg & McCray [1] | Popularized the term "microbiome" in genomics context [1] | Brought term to wider scientific audience |
| 2008-Present | NIH & International Consortium [1] [4] | Human Microbiome Project and related large-scale initiatives [1] [4] | High-throughput sequencing revealed microbiome's critical role in host health |
The Origin of "Microbiome" and a Paradigm Shift
A common misconception is that Nobel laureate Joshua Lederberg coined the term "microbiome" in 2001. While he and McCray played a key role in popularizing it within genomics, the term first appeared in a 1988 paper by Whipps and colleagues [5]. Critically, the word is a portmanteau of "microbe" and "biome," emphasizing an ecological system, and is not a direct derivative of the '-omics' family of terminology [5]. This origin underscores that the term was conceived from an ecological perspective to describe a microbial habitat, not merely a genomic catalogue.
The intellectual foundation for microbiome research traces back to the pioneering work of Sergei Winogradsky in the late 19th century. His development of the Winogradsky Column and his studies on nitrifying bacteria demonstrated that microbes function as interconnected communities in their natural environments, with the metabolic products of some species creating niches for others [5]. This stood in stark contrast to the pure-culture techniques of medical microbiology and established the core principle of microbial ecology: to understand microbes, one must study them in context [5]. This represents a fundamental paradigm shift from viewing microbes as isolated pathogens to understanding them as cooperative communities essential for ecosystem functioning.
Methodological Approaches and Research Toolkit
Standardized Analytical Workflows
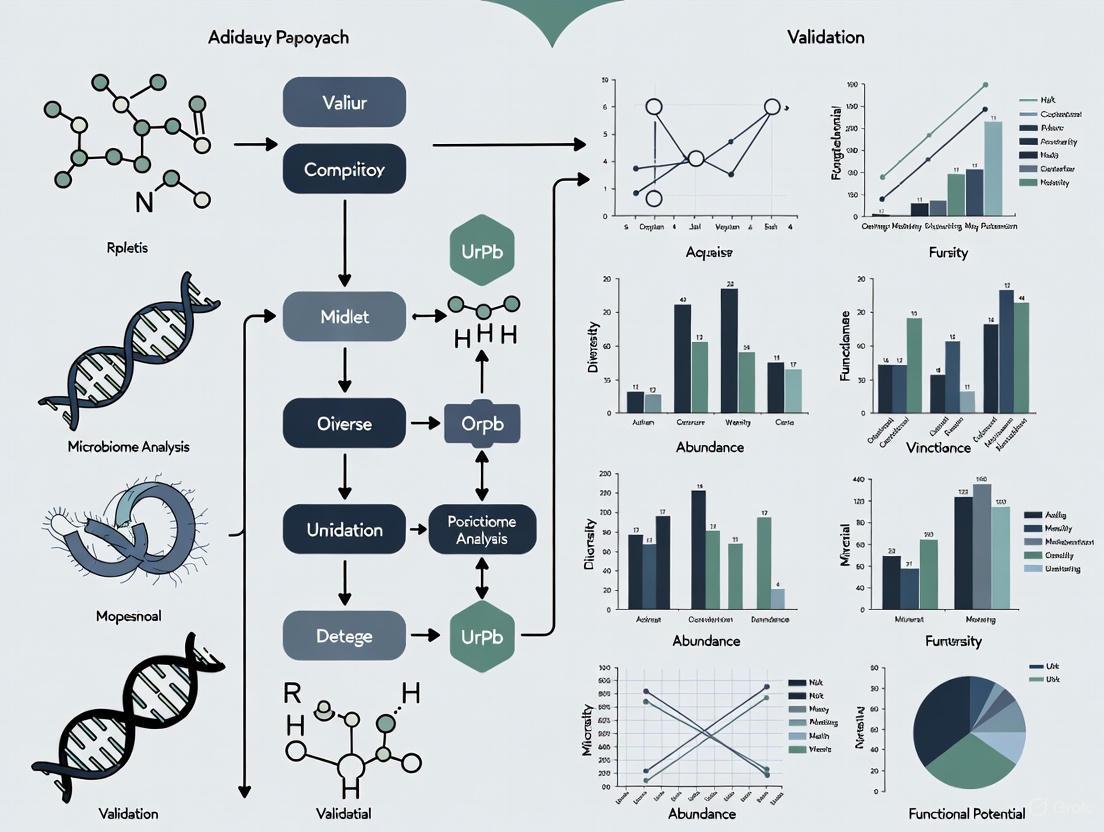
Modern microbiome analysis relies on a multi-layered, omics-driven approach to move beyond cataloging microbiota members (who is there) to understanding functional potential and activity (what they are doing). The international scientific community emphasizes the need for standardization across this workflow to ensure data comparability and reproducibility [4] [7]. The following diagram outlines the core steps in a comprehensive microbiome analysis protocol, from sample collection to functional interpretation.
Essential Research Reagents and Technologies
Executing the workflows above requires a suite of specialized reagents and technologies. The following table details key components of the researcher's toolkit for conducting robust microbiome studies.
Table 3: Essential Research Reagent Solutions for Microbiome Analysis
| Reagent / Technology | Primary Function | Application in Microbiome Research |
|---|---|---|
| Sample Stabilization Buffers | Preserves nucleic acid integrity at point of collection [7] | Critical for accurate representation of microbial community; prevents shifts post-sampling |
| DNA Extraction Kits (for stool, soil, etc.) | Lyses diverse cell walls and purifies total community DNA [7] | Yield of pure, inhibitor-free DNA is a major confounder; must be standardized for comparison |
| 16S/ITS rRNA Primer Sets | Amplifies hypervariable regions for taxonomic identification [4] [3] | Workhorse for cost-effective community profiling; defines microbiota composition |
| Shotgun Metagenomic Library Prep Kits | Prepares entire genomic DNA for high-throughput sequencing [7] | Enables analysis of all genes (metagenome) and organisms, including viruses and archaea |
| PCR Enzymes & Master Mixes | Amplifies target DNA sequences for detection and sequencing [4] | Used in amplicon sequencing and qPCR for absolute quantification of taxa |
| Bioinformatics Pipelines | Processes raw sequence data into biological insights [7] | For sequence quality control, taxonomy assignment, and functional annotation |
Consensus and Validation in Clinical Translation
Current State of Microbiome Testing
A significant outcome of microbiome research is the potential for clinical diagnostics and therapeutics. However, a 2024 international consensus statement highlights that the transition from research to routine clinical practice remains challenging [7]. The consensus panel, comprising multidisciplinary experts, concluded that there is currently insufficient evidence to widely recommend the routine use of microbiome testing in clinical practice [7]. This cautious stance stems from several factors: the complexity of sequencing datasets, difficulty disentangling correlation from causation, and the absence of a standardized framework for test interpretation and validation [7].
The consensus strongly recommends that providers of microbiome testing must communicate a "reasonable, reliable, transparent, and scientific representation of the test," making clients and clinicians aware of its limited evidence base [7]. Key technical recommendations for validation include:
- Appropriate Methodologies: Community profiling should use either amplicon sequencing (e.g., 16S rRNA) or shotgun metagenomic sequencing. Techniques like multiplex PCR or bacterial culture alone are not considered sufficient for microbiome testing [7].
- Reporting Standards: Test reports should detail the patient's medical history and the full test protocol, including methods of collection, storage, DNA extraction, and bioinformatic analysis to ensure transparency and reproducibility [7].
- Focus on Function: Moving beyond relative abundance data to functional metrics (e.g., gut microbiome health indices) is essential for future clinical applicability [7] [8].
Public and Professional Awareness
The need for validation and education is reflected in public understanding. A 2025 international survey revealed that while 71% of the public has heard the term "microbiota," only 24% know what it means exactly. Furthermore, awareness of "dysbiosis" (microbial imbalance) is even lower, at 34% [9]. The survey identified healthcare professionals as the most trusted source of information (81%), underscoring their critical role in guiding the validated application of microbiome science [9].
Distinguishing between microbiota as the community of microorganisms and microbiome as the comprehensive habitat including their genomic and metabolic activity is fundamental for scientific precision. This conceptual clarity, rooted in the ecological principles of Winogradsky and formally defined by Whipps, is a prerequisite for rigorous research. As the field advances, the consensus within the scientific community is clear: validating analytical protocols and establishing standardized frameworks are the critical next steps. For researchers and drug development professionals, this means prioritizing functional insights over mere compositional catalogs and adhering to evolving best practices. This disciplined approach is essential for translating the profound potential of microbiome research into reliable diagnostics and therapeutics.
The field of human microbiome research has witnessed explosive growth, revealing compelling associations between gut microbial communities and a vast range of intestinal and extraintestinal disorders [7]. This has catalyzed intense interest in exploiting the gut microbiome as a diagnostic, prognostic, and therapeutic monitoring tool in clinical practice [10]. Consequently, a burgeoning direct-to-consumer (DTC) market for microbiome testing has emerged, often claiming to guide clinical management. However, this enthusiasm has vastly outstripped the established scientific evidence, creating a landscape fraught with unsubstantiated claims, non-standardized methodologies, and potential for misdirected healthcare resources [10] [7] [11].
Recognizing these challenges, a multinational, multidisciplinary panel of 69 experts from 18 countries was convened to establish a foundational framework for the responsible development and use of microbiome diagnostics [10] [12] [13]. Using a structured Delphi method to achieve consensus, this panel produced a set of authoritative guidelines aimed at standardizing best practices, defining minimum requirements, and paving the way for evidence-based application in clinical medicine [7] [12]. This guide distills the core principles and technical standards from this consensus, providing researchers, scientists, and drug development professionals with a critical benchmark for evaluating, developing, and implementing clinical microbiome testing.
Core Consensus Principles and Minimum Requirements
The international consensus establishes a comprehensive framework organized around five key domains, from general principles to future outlook. The following table summarizes the pivotal statements ratified by the expert panel.
Table 1: Key Consensus Statements on Microbiome Testing in Clinical Practice
| Working Group Focus | Core Consensus Statement | Agreement Rate |
|---|---|---|
| General Principles & Minimum Requirements | Providers must communicate the test's limited clinical evidence transparently to customers and clinicians. | >80% [7] |
| Procedural Steps Before Testing | Direct patient requests for testing without clinical recommendation are discouraged. | >80% [7] |
| Microbiome Analysis | Appropriate modalities for community profiling are amplicon sequencing and whole-genome sequencing. | >80% [7] |
| Characteristics of Reports | Patient medical history and detailed test protocol must be included in the report. | >80% [7] |
| Relevance in Clinical Practice | There is currently insufficient evidence to recommend routine microbiome testing in clinical practice. | >80% [7] |
Pre-Testing Protocols and Patient Preparation
A critical recommendation is that microbiome testing should be initiated by a licensed healthcare professional—such as a physician, pharmacist, or dietitian—based on a clear clinical rationale [14] [12]. Self-prescription by patients is strongly discouraged to prevent inappropriate testing and misinterpretation of results [7]. The consensus advises against patients making changes to their usual diet or suspending treatments before sample collection, as the test should reflect the steady-state microbiome under normal conditions [14].
The collection of comprehensive clinical metadata is considered indispensable for contextualizing microbiome data. Essential variables include [7] [14] [12]:
- Personal patient features: Age, gender, body mass index (BMI), and gut transit time.
- Health status: Current and past medical conditions.
- Medications: Detailed history of drug intake, particularly antibiotics.
- Dietary information: Recent dietary patterns.
For sample integrity, the consensus emphasizes the use of a stool collection kit with a DNA preservative, testing within a recommended time frame, and long-term storage of fecal samples at -80°C in the laboratory [14].
Analytical Methods: From Sampling to Sequencing
The consensus provides clear guidance on the methodologies deemed appropriate for gut microbiome community profiling.
Table 2: Recommended Analytical Methods for Microbiome Testing
| Method | Description | Consensus Recommendation |
|---|---|---|
| 16S rRNA Gene Amplicon Sequencing | Sequences hypervariable regions of the bacterial 16S rRNA gene for taxonomic profiling. | Recommended for community profiling [7] [14] |
| Shotgun Metagenomic Sequencing (MGS) | Random sequencing of all DNA in a sample, allowing for taxonomic and functional gene analysis. | Recommended for community profiling [7] [14] |
| Quantitative PCR (qPCR) & Bacterial Culture | Targets specific, pre-defined pathogens or genes; culture isolates specific culturable organisms. | Not a proxy for microbiome testing; useful for narrow, hypothesis-driven identification [7] [14] |
The expert panel unequivocally states that while techniques like multiplex PCR and bacterial culture are valuable for identifying specific pathogens, they "cannot be considered microbiome testing nor can be used as a proxy for microbiome profiling" [7]. This distinction is crucial for researchers designing validation studies.
For DNA analysis, the entire process must be meticulously controlled. This includes using optimized DNA extraction protocols with bead-beating for thorough cell lysis [15], incorporating appropriate controls throughout the process, and employing validated bioinformatics pipelines for data analysis [7]. The use of negative controls and biological mock communities is essential to account for contamination and technical biases, especially in low-biomass samples [15].
Diagram 1: The end-to-end workflow for clinically relevant microbiome testing, as recommended by the international consensus. The process emphasizes the central role of healthcare professionals and the critical steps of metadata collection and standardized laboratory protocols.
Reporting Standards and Interpretation
The consensus provides explicit guidance on the elements that must be included and excluded from a clinically-oriented microbiome test report.
Essential Components of the Report
- Patient Medical History: The report must be contextualized with relevant clinical information [7].
- Test Protocol Transparency: Detailed methodology covering stool collection, storage, DNA extraction, sequencing, and post-sequencing analyses must be provided [7] [14].
- Ecological and Taxonomic Measures: Reports should include alpha and beta diversity measures and a complete taxonomic profile at the deepest possible resolution (ideally species-level) [14].
- Comparison to Matched Controls: Results should be benchmarked against a matched control group (e.g., healthy individuals with similar age, BMI, and geography) to aid interpretation [14] [12].
What to Exclude from Reports
- Dysbiosis Indices and Phylum-Level Ratios: The consensus strongly advises against reporting oversimplified metrics like the Firmicutes/Bacteroidetes ratio, as they "do not capture the variation in the gut microbiome within the same host and between hosts and there is insufficient evidence to establish a causal relationship" with health [14] [12].
- Post-Testing Therapeutic Advice: A pivotal recommendation is that the testing provider should not offer specific therapeutic advice based on the results. This responsibility falls solely to the referring healthcare provider who understands the patient's full clinical context [14] [12].
The Scientist's Toolkit: Essential Research Reagents and Materials
Robust microbiome science depends on carefully selected reagents and materials at every stage. The following table details key components of a validated workflow.
Table 3: Essential Research Reagent Solutions for Microbiome Testing
| Item | Function/Description | Technical Considerations |
|---|---|---|
| Stool Collection Kit with DNA Preservative | Stabilizes microbial DNA at room temperature for transport. | Critical for preserving nucleic acid integrity; allows for practical sample collection outside lab [16]. |
| Bead-Beating Lysis Tubes | Homogenization and mechanical breakage of tough microbial cell walls. | Essential for DNA extraction from Gram-positive bacteria and spores; prevents taxonomic bias [15]. |
| Validated DNA Extraction Kit | Isolates total genomic DNA from complex stool matrix. | Must be optimized for fecal material; performance varies significantly between kits [15]. |
| PCR Primers for 16S rRNA Gene | Amplifies target hypervariable regions for sequencing. | Choice of region (e.g., V4) impacts taxonomic resolution; must be well-validated [17] [15]. |
| Mock Microbial Communities | Defined mixtures of known microorganisms or their DNA. | Serves as a positive control to benchmark accuracy, precision, and bias in the entire workflow [15]. |
| Negative Control Reagents | Sterile water or buffer taken through the entire extraction and sequencing process. | Identifies contamination from reagents, kits, or the laboratory environment [15]. |
| Bioinformatic Pipelines & Databases | Software for processing raw sequences into taxonomic and functional profiles. | Must use curated, up-to-date databases (e.g., GTDB, SILVA); parameters significantly impact results [7] [15]. |
Current Clinical Relevance and Future Directions
The consensus is unequivocal about the current state of the field: "there is insufficient evidence to widely recommend the routine use of microbiome testing in clinical practice" [7] [14]. The foundational role of this consensus is to provide a framework for the dedicated studies needed to build this evidence.
Future progress hinges on a concerted shift from descriptive, association-based research to mechanistic studies that elucidate cause-and-effect relationships [14]. This will require:
- Standardization and Quality Control: Widespread adoption of the minimum requirements and best practices outlined in the consensus.
- Advanced Study Designs: Implementation of large, longitudinal cohorts with deep phenotyping to control for confounders that obscure causal links with human diseases [7] [14].
- Functional Insights: Leveraging multi-omics approaches (metatranscriptomics, metabolomics, proteomics) to move beyond taxonomy and understand microbial function in situ [17].
- Rigorous Diagnostic Accuracy Studies: Conducting studies that meet regulatory standards to demonstrate clinical utility for specific indications [12].
In conclusion, while the promise of microbiome-based diagnostics is immense, its path to clinical integration must be paved with rigorous science, standardized methods, and tempered expectations. This international consensus provides the essential roadmap, ensuring that the field develops in a manner that is reliable, reproducible, and ultimately, beneficial for patients.
The human microbiome, defined as the collective genome of the trillions of microorganisms inhabiting our bodies, has transitioned from being perceived as a mere collection of passengers to being recognized as a functional human organ that is integral to physiology and homeostasis. This complex ecosystem of bacteria, archaea, viruses, and eukaryotes exceeds the number of human cells, performing critical functions including immune regulation, breakdown of dietary compounds, production of essential nutrients, and protection against pathogens [18]. Groundbreaking developments in sequencing technologies and analytical methods have fundamentally advanced our understanding of the microbiome's structure and function, revealing its operation through intricate ecological principles [18].
This review synthesizes current conceptual frameworks for understanding the microbiome as a human organ and examines the ecological principles guiding its study and manipulation. We explore how these theoretical advances are being translated into validated analytical approaches and therapeutic strategies, with a particular focus on the emerging international consensus that is shaping the future of microbiome research and its clinical application. By integrating foundational concepts with cutting-edge ecological engineering and consensus-driven validation protocols, we aim to provide a comprehensive comparison of the frameworks and methodologies that are defining this rapidly evolving field.
Conceptual Frameworks for Understanding the Microbiome as an Organ
Systematic Theoretical Frameworks
A systematic framework proposed in Signal Transduction and Targeted Therapy integrates knowledge from anatomy, physiology, immunology, histology, genetics, and evolution to reconceptualize the human-microbe relationship [19]. This framework introduces several key concepts that reframe our understanding of the microbiome's role in human biology. The "innate and adaptive genomes" concept enhances genetic and evolutionary understanding by distinguishing between the inherent human genetic blueprint (innate genome) and the dynamic, acquired microbial genes (adaptive genome) that together contribute to total host phenotypic variation [19].
The "germ-free syndrome" challenges the traditional view of "microbes as pathogens" by demonstrating through germ-free animal models that microorganisms are actually necessary for normal health and development [19]. The "slave tissue" concept posits a symbiotic relationship where microbes function as exogenous tissues under the regulation of human master tissues (nerve, connective, epithelial, and muscle tissues), highlighting the complex interplay between host systems and microbial communities [19]. Furthermore, the "acquired microbial immunity" framework positions the microbiome as an adjunct to the human immune system, providing a scientific rationale for probiotic therapies and judicious antibiotic use [19].
Table 1: Key Conceptual Frameworks for Understanding the Microbiome as a Human Organ
| Conceptual Framework | Key Principle | Implication for Research and Medicine |
|---|---|---|
| Innate & Adaptive Genomes | Distinguishes inherent human genes from acquired microbial genes | Expands understanding of host phenotypic variation and genetic diversity |
| Germ-free Syndrome | Demonstrates necessity of microbes for normal health | Challenges pathogen-centric view of microorganisms |
| Slave Tissue Concept | Frames microbes as exogenous tissues under host regulation | Elucidates symbiotic host-microbe control mechanisms |
| Acquired Microbial Immunity | Positions microbiome as immune adjunct | Supports rational probiotic and antibiotic use |
| Meta-host Model | Broadens host definition to include symbiotic microbes | Explains disease heterogeneity and transplantation outcomes |
Ecological and Evolutionary Frameworks
The reconceptualized 4 W framework for human microbiome acquisition provides a nuanced approach to understanding microbial transmission, particularly during early life [20]. This framework addresses the limitations of traditional "vertical versus horizontal" transmission models from infectious disease epidemiology by instead focusing on four key components: "what" (the transmitted microbial elements, including cells, structural elements, or metabolites), "where" (the source and destination sites), "who" (the source of the microbes, such as parents, household members, or the environment), and "when" (the timing of transmission events) [20]. This multifaceted framework more accurately captures the complexity of microbiome assembly across the human lifespan, particularly during critical developmental windows.
The "health-illness conversion model" encapsulates the interplay between innate and adaptive genomes and patterns of dysbiosis, providing a systematic way to understand how microbiome disturbances contribute to disease states [19]. Additionally, the "cell-microbe co-ecology model" describes the symbiotic regulation and co-homeostasis between microbes and human cells, emphasizing the dynamic balance that characterizes health [19]. These frameworks collectively position the microbiome not as a separate entity, but as an integrated physiological system that obeys ecological principles while being subject to host evolutionary pressures.
Ecological Principles Informing Microbiome Research
Translation of Macroecological Principles
Microbiome engineering efforts increasingly leverage principles from decades of macroecology research, particularly those governing the relationship between biodiversity and ecosystem function [21]. The translation of these ecological principles to microbiome engineering focuses on three critical stages: microbiome design, colonization, and maintenance [21]. A key insight from this translation is that many engineering efforts fail due to inadequate design principles that result in the loss of key microorganisms and disruption of functional links between the engineered community and its intended ecosystem service [21].
Niche theory, originally developed for macroecosystems, has proven particularly valuable for understanding and manipulating microbial communities in host-associated environments [21]. The ecological niche concept explains how microorganisms occupy specific functional roles and spatial locations within the host ecosystem, and how these niches can be manipulated to optimize community stability and function. This approach emphasizes the importance of niche dynamics in optimizing the diversity and abundance of microbial taxa to promote both stability and functionality, especially in therapeutic contexts [21].
Table 2: Ecological Principles Applied to Microbiome Engineering
| Ecological Principle | Source in Macroecology | Application to Microbiome Engineering |
|---|---|---|
| Biodiversity-Ecosystem Function | Tilman et al., 2014 [21] | Guides optimization of microbial diversity for desired therapeutic functions |
| Niche Theory | Hutchinson, 1957 [21] | Informs design of microbial communities with complementary functional roles |
| Succession Theory | Clements, 1936 [21] | Models ecological progression during microbiome assembly and manipulation |
| Stability-Diversity Relationship | MacArthur, 1955 [21] | Shapes communities resistant to perturbation and resilient to disturbance |
| Competitive Exclusion | Gause, 1930s (not in results) | Guides selection of compatible consortium members to enhance persistence |
Ecological Models for Microbiome Dynamics
The application of ecological principles has led to the development of specific models that capture the dynamics of host-microbiome systems. The "ecosystem on a leash" model conceptualizes the host microbiome as an ecosystem under host control mechanisms, illustrating the tension between microbial community self-organization and host regulation [21]. This model helps explain how host factors such as diet, immune responses, and physical niches shape the composition and function of microbial communities while still allowing for ecological processes to operate within constraints set by the host.
The emphasis on host physical niches highlights how anatomical and physiological features create distinct microbial habitats that maintain community composition and stability [21]. These physical niches—including the gastrointestinal crypt architecture, mucosal surfaces, and skin microenvironments—provide the structural foundation upon which ecological interactions between microbial taxa unfold. Understanding these physical determinants of community assembly is essential for effectively engineering microbiomes for therapeutic purposes, as they define the environmental parameters that support or inhibit particular microbial functions.
Analytical Methodologies and Consensus Approaches
Standardization of Microbiome Testing
An international consensus statement on microbiome testing in clinical practice has established a standardized framework for the development and application of microbiome-based diagnostics [7]. Developed through a Delphi process involving 69 experts from 18 countries, this consensus provides critical guidance on the appropriate use and interpretation of microbiome analyses [7] [14]. The consensus strongly emphasizes that microbiome testing should be initiated by licensed healthcare providers based on clinical rationale rather than through direct-to-consumer requests, which risk misinterpretation and inappropriate interventions [12].
Regarding analytical methodologies, the consensus recommends that appropriate modalities for gut microbiome community profiling include amplicon sequencing (e.g., 16S rRNA gene sequencing) and whole genome sequencing (shotgun metagenomics) [7] [14]. In contrast, techniques such as multiplex PCR and bacterial cultures, while potentially useful for specific pathogen detection, cannot be considered comprehensive microbiome testing methods and should not be used as proxies for microbiome profiling [7]. This distinction is crucial for ensuring that research and clinical practice employ methodologies capable of capturing the full complexity of microbial communities.
Methodological Standards and Reporting
The international consensus establishes minimum requirements for microbiome testing quality, emphasizing that providers must adhere to high-quality standards and maintain transparency about the current limited evidence for clinical applicability [7]. The consensus specifies that comprehensive taxonomic profiling should be reported with the deepest possible resolution, while commonly used but poorly validated metrics such as the Firmicutes/Bacteroidetes ratio should be excluded from clinical reports due to insufficient evidence supporting their clinical utility [14] [12].
Critical to the interpretation of microbiome data is the collection of detailed clinical metadata, including patient age, body mass index, diet, medications, and gut transit time, which provide essential context for understanding variations in microbiome composition and function [7] [14]. Additionally, the consensus strongly recommends that microbiome test reports include comparison to matched healthy control groups to facilitate meaningful interpretation of results [14]. Perhaps most significantly, the consensus states that post-testing therapeutic advice should remain the responsibility of the referring healthcare provider rather than the testing provider, reinforcing the need for clinical expertise in translating microbiome data into patient care [12].
Experimental Approaches and Research Methodologies
Validated Experimental Workflows
The following workflow diagram illustrates the standardized approach for microbiome analysis based on international consensus guidelines and ecological principles:
Research Reagent Solutions and Essential Materials
The following table details key research reagents and materials essential for conducting robust microbiome research according to consensus guidelines and ecological principles:
Table 3: Essential Research Reagents and Materials for Microbiome Analysis
| Research Reagent/Material | Function/Purpose | Technical Specifications |
|---|---|---|
| Stool Collection Kit with DNA Stabilizer | Preserves microbial community structure during sample transport and storage | Must contain genome preservative; maintain stability at recommended time frames [7] |
| DNA Extraction Kits | Isolates high-quality microbial DNA from complex samples | Should be validated for diverse bacterial taxa; include mechanical lysis steps for tough Gram-positive species |
| 16S rRNA Gene Primers | Amplifies variable regions for amplicon sequencing | Target appropriate hypervariable regions (V3-V4); include barcodes for multiplexing [20] |
| Shotgun Metagenomic Library Prep Kits | Prepares sequencing libraries for whole-genome analysis | Should minimize host DNA amplification bias; optimized for low-biomass samples |
| Reference Databases | Enables taxonomic classification and functional assignment | Curated databases (e.g., Greengenes, SILVA, GTDB) for accurate taxonomic profiling [14] |
| Bioinformatics Pipelines | Processes sequencing data and calculates ecological metrics | Must generate alpha diversity (within-sample) and beta diversity (between-sample) measures [7] |
| Positive Control Communities | Validates sequencing and analysis workflow performance | Defined mock microbial communities with known composition and abundance |
Therapeutic Development Approaches
The development of microbiome-based therapeutics requires specialized methodologies that account for the unique properties of living microbial products. Several distinct therapeutic modalities have emerged, each with its own development pathway and technical requirements [22]. Fecal Microbiota Transplantation (FMT) involves the transfer of minimally manipulated microbial communities from screened donors to recipients, primarily used for recurrent Clostridioides difficile infection but under investigation for other indications [22]. Live Biotherapeutic Products (LBP) are biological products containing defined live microorganisms, which may consist of single or multiple strains, developed under regulatory frameworks similar to traditional biologics [22].
Additional therapeutic approaches include Antimicrobial Peptides (AMPs), which are multifunctional peptides with targeted antibacterial effects, and phage therapy, which utilizes bacteriophages for precise targeting of pathogenic bacterial infections [22]. The development of these therapeutics requires interdisciplinary resources, professional experience, and state-of-the-art facilities capable of maintaining microbial viability throughout manufacturing and storage [22]. Each approach presents distinct challenges in quality control, potency assessment, and stability testing that must be addressed through specialized analytical methods developed specifically for live microbial products.
Comparative Analysis of Microbiome Conceptualization Approaches
Framework Integration and Complementarity
The various conceptual frameworks for understanding the microbiome as a human organ demonstrate significant complementarity when analyzed collectively. The systematic framework emphasizing "innate and adaptive genomes" [19] aligns well with the ecological principles of host-microbe coevolution [21], together providing a more comprehensive understanding of how host genetics and microbial ecology interact to influence health outcomes. Similarly, the "slave tissue" concept [19] finds operational expression in the "ecosystem on a leash" model [21], both capturing the dynamic tension between host control mechanisms and microbial community self-organization.
The 4 W transmission framework [20] enhances the "acquired microbial immunity" concept [19] by providing a structured approach to investigating how microbial exposures during critical developmental windows shape immune function across the lifespan. This integration of conceptual models with operational frameworks is essential for advancing from theoretical understanding to practical intervention strategies. Furthermore, the international consensus on microbiome testing [7] provides the necessary methodological standardization that enables robust comparison of findings across different research programs applying these conceptual frameworks.
Translational Applications and Therapeutic Development
The conceptualization of the microbiome as a human organ has direct implications for therapeutic development and clinical translation. The ecological principle that biodiversity supports ecosystem function [21] informs the design of microbial consortia for Live Biotherapeutic Products (LBPs), guiding selection of complementary strains with diverse functional attributes [22]. Similarly, the understanding of microbial niches [21] helps predict which introduced strains will persist in specific host environments and which functions they are likely to perform in different anatomical sites.
The international consensus statement establishes critical quality standards for developing these therapeutics, emphasizing the need for high-quality accredited laboratories, validated analytical methods, and comprehensive reporting [7] [14]. This consensus approach is particularly important for addressing the current limitations in evidence supporting routine clinical use of microbiome testing, while simultaneously building the methodological foundation needed to generate the robust evidence required for regulatory approval of microbiome-based diagnostics and therapies [7]. As the field advances, the integration of conceptual frameworks, ecological principles, and consensus standards will be essential for realizing the full potential of microbiome science to improve human health.
The conceptualization of the human microbiome as an organ represents a paradigm shift in human biology, with profound implications for understanding health and disease. The integration of systematic theoretical frameworks, ecological principles, and standardized analytical approaches provides a robust foundation for both basic research and therapeutic development. While significant challenges remain—particularly in establishing causal mechanisms and validating clinical utility—the convergence of these complementary perspectives promises to accelerate the translation of microbiome science into effective interventions for a wide range of diseases. As consensus standards mature and ecological principles are more effectively applied to microbial community engineering, the vision of harnessing the microbiome as a therapeutic target is increasingly becoming a clinical reality.
The human gut microbiome, a complex ecosystem of bacteria, viruses, fungi, and archaea, is increasingly recognized as a fundamental regulator of human health and disease. Recent advances in high-throughput sequencing technologies have revolutionized our understanding of microbial communities, revealing their crucial roles in metabolic regulation, immune function, and neurological development [23]. Despite exponential growth in basic science research, the clinical translation of microbiome discoveries remains markedly limited. A significant translational chasm exists between compelling research associations and validated clinical applications, creating a landscape filled with promising yet unproven diagnostic and therapeutic tools [7] [24]. This gap is particularly problematic given the proliferation of direct-to-consumer microbiome testing services that often outpace evidence-based validation [7].
The current evidence gaps span multiple domains, including insufficient standardization, limited causal understanding, and inadequate clinical trial validation. An international consensus statement on microbiome testing in clinical practice highlights that "there is currently limited evidence for the applicability of gut microbiome testing in clinical practice," directly cautioning against its routine use without stronger supporting studies [7] [14]. This review systematically examines these evidence gaps, compares current technological approaches, details experimental methodologies, and identifies the critical pathway forward for validating microbiome-based applications in clinical practice.
Current Evidence Gaps in Clinical Applications
Diagnostic and Therapeutic Limitations
Table 1: Key Evidence Gaps in Microbiome Clinical Applications
| Domain | Specific Gap | Clinical Implications | Current Consensus View |
|---|---|---|---|
| Diagnostic Applications | Lack of validated reference ranges for "healthy" microbiome | Inability to define dysbiosis thresholds for clinical diagnosis | "No common definition of dysbiosis is available at this point" [14] |
| Causality Establishment | Difficulty distinguishing causal from correlative relationships | Limited understanding of microbiome's role in disease pathogenesis | "Defining the exact nature of dysbiosis is essential for clinical and therapeutic applications" [25] |
| Methodological Standardization | Absence of unified protocols for sample collection, processing, and analysis | Limited reproducibility and comparability across studies | "Lack of standardized protocols, inconsistent reproducibility, complex data interpretation" [23] |
| Clinical Trial Validation | Insufficient interventional studies with clinical endpoints | Microbiome manipulation strategies lack evidence of efficacy | "Human trials are essential for establishing the efficacy of these interventions" [25] |
| Regulatory Frameworks | Absence of established pathways for microbiome-based diagnostic approval | Unregulated direct-to-consumer tests with unproven clinical value | "Absence of established regulations and framework for the clinical translation" [7] |
The clinical application of microbiome science faces fundamental challenges that span the entire translational pathway. A primary limitation is the absence of standardized diagnostic criteria for dysbiosis. Unlike traditional laboratory values with established reference ranges, microbiome composition exhibits substantial inter-individual variation influenced by age, diet, geography, medication use, and host genetics [24] [26]. This variability complicates the establishment of universal diagnostic thresholds. The international consensus statement explicitly notes that commonly used metrics like the Firmicutes/Bacteroidetes ratio "do not capture the variation in the gut microbiome within the same host and between hosts and there is insufficient evidence to establish a causal relationship between specific dysbiosis indices and host health" [14].
A second critical gap lies in establishing causality rather than correlation between microbiome profiles and disease states. While numerous studies have identified microbial signatures associated with conditions ranging from inflammatory bowel disease to neurological disorders, "determining the underlying mechanisms and establishing cause and effect is extremely difficult" [25]. This challenge is compounded by the fact that many microbiome-disease relationships may be bidirectional, with disease states simultaneously altering and being altered by microbial communities [25].
Methodological and Regulatory Challenges
The field also grapples with significant methodological heterogeneity that limits comparability across studies. Variations in sample collection methods, DNA extraction techniques, sequencing platforms, and bioinformatic analyses introduce substantial variability that confounds cross-study comparisons and meta-analyses [23]. The international consensus panel identified this as a major barrier, noting "methodological variability, incomplete functional annotation of microbial 'dark matter,' and underrepresentation of global populations" as key limitations [23].
Perhaps most importantly, there is a dearth of large-scale, prospective interventional trials demonstrating that microbiome-based diagnostics or therapies improve clinically meaningful endpoints. While mechanistic studies and association analyses abound, evidence from randomized controlled trials with patient-centered outcomes remains limited [7]. The consensus statement concludes that "at the present time, there is insufficient evidence to widely recommend the routine use of microbiome testing in clinical practice, which should be supported by dedicated studies" [7].
The regulatory landscape for microbiome-based applications remains underdeveloped, creating an environment where direct-to-consumer tests can proliferate without demonstrated clinical utility. This regulatory gap has allowed commercial entities to offer microbiome testing services that "often claims to drive the clinical management of patients with dysbiosis-associated diseases" despite limited evidence supporting these claims [7].
Comparative Analysis of Microbiome Testing Methodologies
Technical Approaches and Their Limitations
Table 2: Comparison of Microbiome Analysis Methodologies
| Method | Resolution | Primary Applications | Advantages | Limitations | Evidence Gap |
|---|---|---|---|---|---|
| 16S rRNA Amplicon Sequencing | Genus to species level | Microbial community profiling, diversity assessment | Cost-effective, well-established protocols, standardized analysis pipelines | Limited taxonomic and functional resolution, primer bias | Inability to detect strain-level variation or functional capacity [23] |
| Shotgun Metagenomics | Species to strain level, functional genes | Comprehensive taxonomic profiling, functional potential assessment | Strain-level resolution, identification of non-bacterial members, functional gene content | Higher cost, computational demands, database limitations | Functional predictions not necessarily reflective of actual microbial activity [23] |
| Metatranscriptomics | Gene expression | Active microbial functions, response to interventions | Insights into microbial community activity rather than potential | Technical challenges with RNA stability, higher cost and complexity | Limited standardization, unclear how to interpret transcriptional changes clinically [27] |
| Metabolic Profiling | Metabolite level | Functional output of microbiome, host-microbe interactions | Direct measurement of functional molecules, integrative view | Difficulty distinguishing microbial vs host metabolites, dynamic fluctuations | Lack of reference ranges, uncertain clinical correlates [24] |
The choice of analytical methodology significantly influences the results and interpretation of microbiome studies. 16S rRNA gene sequencing remains the most widely used approach due to its cost-effectiveness and established bioinformatic pipelines. However, this method provides limited taxonomic resolution and no direct information about functional capacity [14]. The international consensus recommends either 16S rRNA sequencing or whole-genome sequencing for gut microbiome community profiling but notes that "multiplex PCR and bacterial cultures, although potentially useful, neither can be considered microbiome testing nor can be used as a proxy for microbiome profiling" [7].
Shotgun metagenomics provides higher taxonomic resolution and insights into functional potential by sequencing all genomic material in a sample. This approach has enabled the identification of specific microbial strains and functional pathways associated with conditions like inflammatory bowel disease and colorectal cancer [23]. However, a significant evidence gap persists between predicting functional potential and demonstrating actual microbial activity, as "functional predictions not necessarily reflective of actual microbial activity" [23].
Emerging approaches like metatranscriptomics and metabolic profiling aim to bridge this gap by measuring RNA expression or metabolite production, respectively. These methods offer insights into the active functions of the microbial community but come with their own technical challenges and interpretive complexities [27]. The integration of these multi-omics approaches represents a promising direction but requires further standardization and validation.
Analytical Standardization Challenges
A critical evidence gap across all methodologies is the lack of analytical standardization. Differences in sample collection methods (including storage conditions and preservatives), DNA extraction techniques, sequencing platforms, and bioinformatic pipelines can all introduce significant variability that compromises reproducibility and cross-study comparability [7]. The international consensus emphasizes that "appropriate modalities for gut microbiome community profiling include amplicon sequencing and whole genome sequencing" but notes the importance of standardizing pre-analytical conditions [7].
Another limitation is the inadequate representation of global populations in reference databases. Most existing microbiome databases are skewed toward Western populations, limiting their applicability to diverse ethnic and geographic groups [23]. This representational bias may obscure important microbial signatures relevant to different populations and compromise the generalizability of findings.
Experimental Protocols for Validating Clinical Applications
Establishing Causal Relationships
Figure 1: Framework for Establishing Microbiome-Disease Causality
Overcoming the correlation-causation gap requires rigorous experimental approaches. The scientific consensus emphasizes that "preclinical models, including germ-free animals, organoids and ex vivo systems, are essential tools to understand the functional role of host-microbiome interactions" but notes they "require improved standardization and translational relevance" [25]. The following protocols represent current best practices for establishing causal relationships:
Gnotobiotic Mouse Models Protocol:
- Animal Preparation: Maintain germ-free mice in sterile isolators to prevent unintended microbial colonization.
- Microbial Inoculation: Introduce human-derived microbial communities via fecal microbiota transplantation from well-characterized donors (healthy vs diseased).
- Phenotypic Monitoring: Assess disease-relevant phenotypes through physiological, metabolic, and immunological parameters.
- Mechanistic Investigation: Utilize multi-omics approaches to identify specific microbial taxa, genes, or metabolites driving observed phenotypes.
- Interventional Validation: Test hypotheses through targeted microbial interventions (specific probiotics, prebiotics, or faecal microbiota transplantation).
This approach has been instrumental in demonstrating causal roles for the microbiome in conditions like hypertension, where "fecal microbiota transplantation from hypertensive donors to germ-free mice can directly elevate blood pressure" [26]. However, limitations remain in translating findings from mouse models to human applications due to physiological differences and simplified microbial communities.
Human Intervention Trial Protocol:
- Participant Stratification: Recruit well-characterized participant groups based on clinical phenotypes, and consider microbiome composition if validated stratification biomarkers exist.
- Intervention Design: Implement targeted microbiome interventions (dietary modification, probiotics, prebiotics, or faecal microbiota transplantation) with appropriate control groups.
- Multi-omics Profiling: Collect longitudinal samples for comprehensive microbiome analysis (16S rRNA, metagenomics, metabolomics) alongside clinical metadata.
- Clinical Endpoint Assessment: Measure predefined clinical endpoints relevant to the condition under investigation.
- Integration Analysis: Apply advanced computational methods to identify associations between microbiome changes and clinical outcomes.
Recent trials exemplifying this approach include the ADDapt trial, which demonstrated that "emulsifier dietary restriction reduces symptoms and inflammation in patients with active Crohn's disease" [28], and the Be GONE Trial, which found that "adding navy beans to the usual diet was a safe, scalable dietary strategy to favorably modulate the gut microbiome of patients with obesity and a history of colorectal cancer" [28].
Artificial Intelligence and Machine Learning Approaches
Figure 2: AI-Driven Microbiome Analysis Workflow
Advanced computational approaches are increasingly employed to navigate the complexity of microbiome data. Artificial intelligence (AI) and machine learning (ML) techniques "enable the discovery of non-invasive microbial biomarkers, refined risk stratification, and prediction of treatment response" [27]. Key methodological considerations include:
Data Preprocessing Protocol:
- Quality Control: Filter sequences based on quality scores, remove chimeras, and correct for sequencing depth variations.
- Normalization: Apply appropriate normalization methods to account for compositionality of microbiome data.
- Feature Engineering: Select biologically relevant features (taxa, genes, pathways) while reducing dimensionality.
Predictive Modeling Protocol:
- Algorithm Selection: Choose appropriate ML algorithms based on data characteristics and research question (Random Forest for classification, regression for continuous outcomes).
- Cross-Validation: Implement rigorous cross-validation strategies to avoid overfitting.
- Interpretation: Apply explainable AI (xAI) approaches like SHAP (SHapley Additive exPlanations) to identify features driving predictions.
These approaches have shown promise in areas like inflammatory bowel disease, where "omics-based signatures have been shown to be a diagnostic marker of IBD to differentiate between CD and UC" [27]. However, limitations persist regarding "data variability, the lack of methodological standardization, and challenges in clinical translation" [27].
Essential Research Reagent Solutions
Table 3: Essential Research Reagents for Microbiome Studies
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| DNA Extraction Kits | QIAamp PowerFecal Pro Kit, DNeasy PowerSoil Kit | Efficient lysis of diverse microbial cells, inhibitor removal | Critical for data comparability; extraction method significantly impacts results [7] |
| Storage/Preservation Solutions | DNA/RNA Shield, RNAlater | Stabilize microbial community composition between collection and processing | Preservation method affects DNA yield and community representation [7] |
| Sequencing Standards | ZymoBIOMICS Microbial Community Standards, NIST stool reference materials | Quality control, cross-study comparability | Enable assessment of technical variability and methodological biases [23] |
| Cell Culture Media | Brain Heart Infusion broth, YCFA medium | Cultivation of fastidious anaerobic gut bacteria | Essential for moving beyond sequencing to functional validation [25] |
| Gnotobiotic Animal Models | Germ-free mice, Humanized microbiota mice | Establishing causality in host-microbiome interactions | Require specialized facilities and expertise [25] |
| Multi-omics Assays | Metabolomics kits, Proteomics platforms | Integrative analysis of microbiome function | Technical variability requires careful standardization [27] |
The reliability and reproducibility of microbiome research depend critically on standardized reagent systems. The international consensus emphasizes that "providers of microbiome testing should communicate a reasonable, reliable, transparent, and scientific representation of the test" and adhere to high-quality standards [7]. Several key reagent categories deserve particular attention:
DNA Extraction Kits specifically designed for complex stool samples are essential for obtaining representative microbial DNA. Different extraction methods can significantly impact the apparent community composition due to varying efficiency in lysing different bacterial taxa [7]. The consensus recommends that "the report should briefly detail the test protocol, including methods of stool collection and storage, DNA extraction, amplification, sequencing, and post-sequencing analyses" to enable proper interpretation [7].
Reference Materials such as mock microbial communities with known composition are critical for quality control and cross-study comparisons. Initiatives like the NIST (National Institute of Standards and Technology) stool reference material help standardize methodology across laboratories [23]. The use of such standards allows researchers to distinguish technical artifacts from true biological signals.
Specialized Culture Media enabling the growth of previously uncultivated microbes represents an advancing frontier. Moving from sequencing-based observations to functional validation requires the ability to culture and manipulate specific microbial strains [25]. Recent advances in culturomics have expanded the range of cultivable gut bacteria, opening new avenues for mechanistic studies.
The field of microbiome research stands at a critical juncture, with compelling associative data outpacing validated clinical applications. Significant evidence gaps persist in diagnostic standardization, causal understanding, and clinical trial validation. Overcoming these limitations requires coordinated efforts across multiple domains: standardization of analytical methods, development of robust reference materials, implementation of rigorous experimental designs establishing causality, and execution of well-controlled clinical trials with meaningful endpoints.
The international consensus statement provides a framework for this progression, emphasizing that "before microbiome tests become integrated into clinical practice, microbiome science must shift from descriptive to mechanistic approaches involving host physiology features and control for confounders that hinder the causal connection with human diseases" [14]. Future research priorities should include large-scale longitudinal studies, diverse population representation, standardized multi-omics protocols, and development of interpretative frameworks that translate microbial measurements into clinically actionable information.
As the field matures, the integration of artificial intelligence with multi-omics data and rigorous experimental validation offers promise for bridging the current evidence gaps. However, this will require interdisciplinary collaboration among microbiologists, clinicians, computational biologists, and regulatory scientists to ensure that microbiome-based applications meet the rigorous standards required for clinical implementation. Only through such coordinated efforts can the tremendous potential of microbiome science be responsibly translated into meaningful clinical applications that improve patient care.
This guide provides a comparative analysis of the core concepts shaping contemporary microbiome research: dysbiosis, core microbiome, and keystone species. For researchers and drug development professionals, understanding the methodologies to define and measure these concepts is crucial for validating microbiome analysis approaches and developing targeted therapies. We objectively compare the performance of different definitions, analytical techniques, and biomarkers used to quantify these states, supported by experimental data from recent studies and clinical trials. The synthesis presented here aims to inform the selection of appropriate models and metrics for consensus approach validation in microbiome research.
The complex ecosystem of microorganisms inhabiting the human body, particularly the gut, profoundly influences host health through metabolic regulation, immune modulation, and maintenance of ecological balance [29] [25]. Three fundamental concepts form the cornerstone of microbial-host interaction research: dysbiosis refers to a disruption of the microbial community structure associated with disease; the core microbiome represents the set of microbial taxa or functions consistently present in healthy individuals; and keystone species are highly influential taxa whose impact on ecosystem stability is disproportionate to their abundance [29] [30] [31]. These concepts are intrinsically linked, as keystone species often carry out essential functions that contribute to a healthy core microbiome, and their loss can be a driving factor in dysbiosis [31]. The field is moving beyond simple taxonomic classification toward functional and strain-resolved analyses to better understand the mechanisms governing host health [32]. This evolution reflects the growing consensus that microbial community function, rather than mere composition, ultimately determines host physiological outcomes.
Comparative Analysis of Dysbiosis Indexes and Measurement Approaches
Dysbiosis is an imbalance in the gut microbial community that has been associated with numerous gastrointestinal, metabolic, and neurological disorders [33] [25]. However, due to high inter-individual variability in healthy microbiomes, no single gold standard for defining dysbiosis exists. Instead, researchers have developed various dysbiosis indexes, each with distinct methodologies, strengths, and limitations, suited to different research or clinical contexts [33]. The table below compares five primary categories of dysbiosis indexes.
Table 1: Comparison of Dysbiosis Index Methodologies
| Index Category | Description | Representative Indexes | Disease/Condition Application | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Large-Scale Bacterial Marker Profiling | Uses a predefined set of bacterial markers (e.g., 54 probes covering 300+ markers) to calculate a dysbiosis score [33]. | GA-map Dysbiosis Index [33] | Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD) [33] | Standardized, commercially available; provides a simple numerical score. | Proprietary calculation method; may not capture cohort-specific variations. |
| Relevant Taxon-Based Methods | Calculates ratios or formulas based on specific taxa known to be altered in a given condition [33]. | Firmicutes/Bacteroidetes ratio [33]; MHI-A [34] | Obesity, Liver Cirrhosis, Post-Antibiotic Dysbiosis [34] [33] | Intuitively simple to calculate and interpret; hypothesis-driven. | Oversimplifies complex communities; ratios can be misleadingly compositional. |
| Neighborhood Classification | Measures the distance (e.g., Bray-Curtis) between a test sample and a reference set of healthy samples [33]. | Median Bray-Curtis to Healthy Reference [33] | Ulcerative Colitis, Crohn's Disease [33] | Holistic, captures overall community structure difference. | Highly dependent on the choice and size of the reference cohort. |
| Random Forest Prediction | Machine learning models trained to classify samples as dysbiotic or healthy based on microbiome features [33]. | Random Forest Classifiers [33] [32] | Various, including Colorectal Cancer [32] | Handles complex, high-dimensional data well; can identify novel biomarkers. | "Black box" nature; requires large, well-curated training datasets. |
| Combined Alpha-Beta Diversity | Integrates measures of within-sample (alpha) and between-sample (beta) diversity [33]. | Alpha-Beta Diversity Combined Index [33] | General dysbiosis assessment | Captures multiple ecological dimensions of the microbial community. | Complex to interpret clinically; lacks universal thresholds for dysbiosis. |
Experimental Protocol: Validating a Microbiome Health Index for Post-Antibiotic Dysbiosis
The Microbiome Health Index for post-Antibiotic dysbiosis (MHI-A) is a relevant taxon-based index developed to specifically distinguish post-antibiotic dysbiosis from a healthy microbiota state [34]. Its development and validation offer a template for a robust methodological approach.
- Objective: To develop a univariate biomarker capable of differentiating a dysbiotic, post-antibiotic gut microbiome from a healthy one [34].
- Data Sources: Longitudinal gut microbiome data from participants in Phase II and III clinical trials of RBX2660 and RBX7455 (investigational Live Biotherapeutic Products for recurrent Clostridioides difficile infection, rCDI). Pre-treatment samples represented post-antibiotic dysbiosis, while the therapeutic doses themselves, manufactured from healthy donors, represented the healthy state [34].
- Algorithm Derivation: Dirichlet-multinomial recursive partitioning (DM-RPart) was used to identify taxonomic classes that most strongly separated baseline (dysbiotic) and post-treatment (restored) samples. Four classes were identified: Gammaproteobacteria and Bacilli were dominant in dysbiosis, while Bacteroidia and Clostridia were dominant in healthy/restored states. A multivariate logistic regression model determined the optimal formula was the ratio of (
Bacteroidia + Clostridia) to (Gammaproteobacteria + Bacilli), termed the MHI-A [34]. - Validation: The diagnostic utility of MHI-A was tested using receiver operating characteristic (ROC) analysis, showing high accuracy in distinguishing dysbiotic and healthy states in the PUNCH CD2 trial. Validation was reinforced with public data from healthy or antibiotic-treated populations, showing MHI-A values were consistent across healthy cohorts and significantly shifted by microbiota-disrupting antibiotics [34].
Figure 1: MHI-A Calculation Workflow. This diagram outlines the key steps for calculating the Microbiome Health Index for post-Antibiotic dysbiosis from raw sequencing data.
Defining the Core Microbiome: From Taxonomy to Function
The "core microbiome" has historically been defined as the set of microbial taxa common to all or most healthy individuals. However, large-cohort studies like the Human Microbiome Project (HMP) revealed that no universal taxonomic core exists due to immense inter-individual variation influenced by diet, genetics, and geography [32]. This has prompted a paradigm shift from a taxonomy-based to a function-based definition of the core microbiome.
The Evolving Definition of "Core"
- Traditional View: Focused on the abundance of specific taxa (e.g., Bacteroides, Faecalibacterium) and metrics like microbial diversity or the Firmicutes-to-Bacteroidetes ratio. These have proven unreliable as universal health indicators, as they are strongly influenced by non-health factors like diet [32].
- Modern View: Emphasizes the preservation of core microbial functions essential for host health, rather than the specific species carrying them out. A promising framework is the "Two Competing Guilds" (TCGs) model, which posits that a healthy microbiome is characterized by a balance between a guild of microbes performing beneficial functions (e.g., fiber fermentation, butyrate production) and a guild enriched in virulence factors and antibiotic resistance genes [32]. The balance between these functional groups may serve as a more robust biomarker for health than taxonomic composition alone.
The HACK Index: A Novel Functional Ranking of Taxa
A significant recent advancement is the development of the Health-Associated Core Keystone (HACK) index [35]. This index moves beyond mere presence/absence by ranking 201 taxa based on their association strengths with:
- Prevalence and co-occurrence patterns in non-diseased subjects.
- Longitudinal stability within individuals.
- Overall host health status [35].
Derived from a meta-analysis of 45,424 gut microbiomes across 141 study cohorts, the HACK index is reproducible across different sequencing methods and cohort lifestyles. Consortia of high HACK-index taxa have been shown to respond positively to interventions like the Mediterranean diet and to reflect responsiveness to immune checkpoint inhibitor therapy, providing a rational basis for designing microbiome-based therapeutics [35].
Keystone Species: The Pivotal Players in Microbial Ecosystems
In ecology, a keystone species is an organism that has a disproportionately large effect on its environment relative to its abundance. The term, coined by Robert Paine after his work with Pisaster sea stars, describes species that are crucial for maintaining the structure and stability of their ecosystem [30] [31]. Their removal triggers a cascade of effects that can drastically alter the ecosystem and reduce biodiversity [30].
Roles of Keystone Species Across Ecosystems
Keystone species can exert their influence through various mechanisms, illustrated in the following diagram and table.
Figure 2: Keystone Species Roles. This diagram categorizes the primary ecological roles played by keystone species and their downstream effects on the ecosystem.
Table 2: Keystone Species in the Human Gut Microbiome
| Keystone Species | Proposed Function | Method of Identification | Disease Association |
|---|---|---|---|
| Akkermansia muciniphila | Mucin degradation, gut barrier integrity [31] | Empirical culture-based studies [31] | Depleted in intestinal inflammation, obesity, and metabolic diseases [31] |
| Faecalibacterium prausnitzii | Butyrate production, anti-inflammatory effects [31] | Presence/absence correlation in cohorts [31] | Depleted in Crohn's disease and Ulcerative Colitis [31] |
| Christensenella minuta | Stimulates ecosystem diversity, acetate production [31] | Co-occurrence network analysis and empirical validation [31] | Associated with lean phenotypes; depleted in obesity and Crohn's disease [31] |
| Ruminococcus bromii | Key degrader of resistant starch; butyrate producer [31] | Empirical studies on starch degradation [31] | Highly prevalent in healthy individuals [31] |
| Bacteroides thetaiotaomicron | Degradation of complex dietary carbohydrates [31] | Empirical studies on carbohydrate metabolism [31] | Controversial and unclear association with IBD [31] |
Experimental Workflow for Identifying Keystone Species
Identifying keystone species requires a combination of advanced bioinformatic analyses and empirical validation.
- Step 1: Metagenomic Sequencing and Metabolomic Profiling. Shotgun metagenomic sequencing of cohort samples is performed to achieve strain-level resolution. This is increasingly paired with metabolomic profiling of stool and serum to link microbial genes to functional outputs [32].
- Step 2: Network Analysis. Co-occurrence and co-abundance networks are constructed from the microbial abundance data. Keystone taxa are identified as highly connected "hubs" within these networks, indicating a central role in the microbial community structure irrespective of their abundance [29] [31].
- Step 3: Functional Annotation. Metagenomic data are annotated using databases like KEGG and MetaCyto to predict the metabolic capabilities of identified keystone hubs, highlighting functions like butyrogenesis or bile acid metabolism [29].
- Step 4: In Vivo Validation. The causal role of candidate keystone species is tested using gnotobiotic mouse models (germ-free animals colonized with defined microbial communities). The impact of adding or removing the candidate species on community structure and host phenotype is assessed to confirm its keystone status [25].
The Scientist's Toolkit: Essential Reagents and Models
This section details key reagents, tools, and models essential for research into dysbiosis, core microbiome, and keystone species.
Table 3: Research Reagent Solutions for Microbiome-Host Interaction Studies
| Item | Function/Application | Examples & Notes |
|---|---|---|
| Gnotobiotic Mice | Causality testing; animals raised germ-free and then colonized with defined human microbial communities to study host-microbiome interactions [25]. | Humanized Microbiota-Associated (HMA) mice are a key model for validating keystone species function and studying dysbiosis mechanisms [25]. |
| Organoids & Gut-on-a-Chip | Ex vivo models for studying host-microbiome interactions at the cellular level, including epithelial barrier function and immune responses [25]. | Lack full physiological context but useful for mechanistic studies and personalized therapy development [25]. |
| Live Biotherapeutic Products (LBPs) | Investigational products containing live organisms (e.g., RBX2660) to correct dysbiosis; used as tools to understand microbial restoration [34]. | Provide a defined intervention to test hypotheses about core microbiome restoration and keystone species reintroduction. |
| Multi-Omics Integration Platforms | Combining metagenomics, metabolomics, transcriptomics, and proteomics to connect microbial community activity with host biological responses [32]. | Essential for moving beyond correlation to mechanism; a cornerstone of the HMP2 [32]. |
| Batch Effect Correction Algorithms | Computational tools to remove technical noise from multi-cohort microbiome data, enabling robust meta-analyses [36]. | Methods like ConQuR (Conditional Quantile Regression) are critical for large-scale, reproducible biomarker discovery [36]. |
| AI-Based Causal Inference Tools | Machine learning algorithms to elucidate complex, non-linear associations and infer causality between microbial features and health outcomes [32]. | Helps overcome limitations of traditional statistical methods (e.g., Mendelian randomization) when dealing with complex microbiome datasets [32]. |
The validation of a consensus approach in microbiome analysis hinges on a nuanced understanding of dysbiosis, the core microbiome, and keystone species. The field is rapidly evolving from descriptive, taxonomy-based assessments toward functional, mechanistic, and causal insights. The development of robust indexes like MHI-A and HACK, alongside advanced analytical tools and preclinical models, provides the much-needed framework for this transition. For researchers and drug developers, the future lies in integrating strain-resolved multi-omics data, cross-cohort validation, and AI-driven causal inference to identify universally applicable biomarkers and therapeutic targets. This integrated approach will ultimately power the development of effective, microbiome-based precision medicines.
Analytical Pipelines in Practice: From Sequencing Technologies to Clinical Applications
16S ribosomal RNA (rRNA) gene amplicon sequencing remains a cornerstone technique in microbiome research, providing a powerful and cost-effective method for profiling microbial communities across diverse environments. Despite its widespread adoption, the field continues to grapple with fundamental questions regarding the technique's optimal implementation and inherent limitations. The ongoing evolution of sequencing technologies, from short-read platforms to emerging long-read capabilities, has further complicated platform selection while simultaneously expanding the methodological landscape. This comparison guide examines the current state of 16S rRNA amplicon sequencing, evaluating technological alternatives through an evidence-based analysis of their respective advantages, limitations, and taxonomic resolution boundaries to inform researcher decision-making in microbiome analysis consensus approach validation.
Technology Platform Comparison
The choice of sequencing platform significantly influences the depth and accuracy of microbial community analysis. The table below summarizes the key characteristics of major sequencing technologies used for 16S rRNA amplicon sequencing.
Table 1: Performance comparison of major 16S rRNA amplicon sequencing platforms
| Platform | Read Length | Target Region | Key Advantages | Major Limitations | Taxonomic Resolution |
|---|---|---|---|---|---|
| Illumina | Short-read (300-600 bp) | Single or multiple hypervariable regions (e.g., V4, V3-V4) | High throughput, low per-sample cost, established protocols | Limited to partial gene sequencing, ambiguous taxonomic assignments | Genus-level typically, species-level for some taxa [37] [38] |
| PacBio (Sequel IIe) | Full-length (~1500 bp) | V1-V9 (complete gene) | Exceptional accuracy (>99.9%) with circular consensus sequencing, reduces ambiguous assignments | Higher cost, lower throughput than Illumina, complex data processing | Species-level and strain-level for many taxa [37] [39] [38] |
| Oxford Nanopore (GridION, MinION) | Full-length (~1500 bp) | V1-V9 (complete gene) | Real-time sequencing, long reads, portable options | Higher error rates than PacBio, improving with recent chemistry | Species-level, improved polymicrobial detection [40] [37] |
| Sanger Sequencing | Full-length (~1500 bp) | V1-V9 (complete gene) | High accuracy, well-established | Low throughput, unsuitable for complex communities | Species-level for monobacterial samples only [40] |
Recent comparative studies demonstrate that full-length 16S rRNA sequencing platforms provide significant advantages for taxonomic resolution. PacBio's circular consensus sequencing (CCS) model achieves exceptional accuracy exceeding 99.9% by making multiple passes of the same DNA molecule [37]. Oxford Nanopore Technologies (ONT) has substantially improved its basecalling accuracy, with recent studies reporting Q-scores approaching Q28 (~99.84% base accuracy) with updated flow cells (R10.4.1) and algorithms [37]. When directly comparing platforms for soil microbiome analysis, both PacBio and ONT provided comparable bacterial diversity assessments, with PacBio showing slightly higher efficiency in detecting low-abundance taxa [37].
For clinical diagnostics, ONT sequencing demonstrated superior performance compared to Sanger sequencing, particularly for polymicrobial samples. One study reported a higher positivity rate for clinically relevant pathogens with ONT (72%) versus Sanger sequencing (59%), with ONT detecting more samples with polymicrobial presence (13 vs. 5) [40]. In a notable case, ONT identified Borrelia bissettiiae in a joint fluid sample that Sanger sequencing missed [40].
Taxonomic Resolution Boundaries
The taxonomic resolution achievable through 16S rRNA sequencing depends on multiple factors, including the target region, sequence length, and reference database quality. The following table outlines the typical resolution boundaries under different experimental conditions.
Table 2: Taxonomic resolution boundaries under different experimental designs
| Sequencing Strategy | Species-Level Identification Capability | Key Limitations | Optimal Clustering Thresholds |
|---|---|---|---|
| Full-length 16S | High resolution for most species | Intragenomic variation complicates strain-level identification | Species: ~99% identity (0.01 divergence) [41] [38] |
| V3-V4 regions only | Moderate (limited to distinctive species) | Cannot differentiate closely related species (e.g., E. coli vs Shigella) | Genus: 92-96% identity (0.04-0.08 divergence) [41] [42] |
| V4 region only | Poor species-level discrimination | Lowest discrimination power among common targets | Varies significantly by taxonomic branch [41] [38] |
| ASV-based approaches | Single-nucleotide resolution | May oversplit genuine biological variants into multiple ASVs | 100% identity (by definition) [43] [42] |
Evidence confirms that sequencing the full-length 16S gene provides significantly better taxonomic resolution compared to partial gene sequencing. In silico experiments demonstrate that the V4 region fails to confidently classify 56% of sequences at the species level, whereas full-length sequences achieve nearly perfect species-level classification [38]. Different hypervariable regions also exhibit taxonomic biases; for instance, the V1-V2 region performs poorly for classifying Proteobacteria, while V3-V5 struggles with Actinobacteria [38].
The transition from Operational Taxonomic Units (OTUs) to Amplicon Sequence Variants (ASVs) represents another significant methodological evolution. ASV methods like DADA2 achieve single-nucleotide resolution through denoising algorithms that distinguish true biological variation from sequencing errors [43]. However, benchmarking analyses reveal that ASV algorithms tend to suffer from over-splitting, while OTU algorithms (particularly UPARSE) achieve clusters with lower errors but more over-merging [43].
For the V3-V4 regions, species-level identification requires moving beyond fixed similarity thresholds. Research shows that applying flexible, species-specific thresholds (ranging from 80% to 100% identity) significantly improves classification accuracy compared to the traditional 98.7% fixed cutoff [42]. This approach helps resolve misclassifications between closely related species and reduces false negatives due to high intraspecies variability.
Experimental Protocols and Methodologies
Full-Length 16S rRNA Sequencing Protocol (PacBio Platform)
For comprehensive species-level analysis, full-length 16S rRNA sequencing on the PacBio platform offers the highest resolution. The following protocol is adapted from published methodologies [37] [39]:
- DNA Extraction: Use mechanical lysis with bead beating combined with column-based purification (e.g., Quick-DNA Fecal/Soil Microbe Microprep kit) to ensure broad taxonomic representation.
- PCR Amplification: Amplify the full-length 16S rRNA gene using universal primers:
- Forward: 5'-AGRGTTYGATYMTGGCTCAG-3'
- Reverse: 5'-RGYTACCTTGTTACGACTT-3'
- Reaction Conditions:
- 5 ng genomic DNA template
- KAPA HiFi HotStart ReadyMix
- Thermal cycling: 95°C for 3 min; 25-30 cycles of 95°C for 30s, 55-57°C for 30s, 72°C for 60s; final extension at 72°C for 5 min
- Library Preparation: Use SMRTbell Prep Kit 3.0 with barcoded adapters for multiplexing
- Sequencing: Run on PacBio Sequel IIe system with 10-hour movie time
- Data Processing: Process Circular Consensus Sequencing (CCS) reads using SMRT Link software with minimum predicted accuracy threshold of 0.9
This approach generates high-fidelity (HiFi) reads with predicted accuracy exceeding Q30 (99.9%) through multiple passes of the same DNA molecule [39].
ONT Sequencing for Polymicrobial Sample Analysis
For complex polymicrobial samples, ONT sequencing provides robust identification of multiple pathogens. The established protocol includes [40]:
- Library Preparation: SQK-SLK109 kit with additional reagents from New England Biolabs
- Sequencing: GridION or MinION with FLO-MIN104/R9.4.1 flow cells
- Run Settings:
- Super-accurate basecalling
- Minscore: 60
- Read filtering minqscore: 10
- Minbases: 200, maxbases: 500
- Data Analysis: EPI2ME platform's Fastq 16S workflow or in-house pipeline using k-mer alignment (KMA) tool mapping to NCBI RefSeq and SILVA 138.1 databases
This protocol successfully identified an average of 2.3 bacterial genera per sample in clinical specimens, outperforming Sanger sequencing in polymicrobial detection [40].
DNA vs. RNA-Based 16S Analysis Protocol
For distinguishing active versus total bacterial communities, a combined DNA and RNA approach is recommended [44]:
- Simultaneous DNA/RNA Extraction: Use AllPrep DNA/RNA/miRNA Universal Kit with extended lysis (10 min shaking at 1500 rpm)
- RNA Reverse Transcription: Generate cDNA using random hexamers
- 16S Amplicon Generation:
- DNA template: 20 ng input in 12.5 μL reaction
- RNA template: cDNA equivalent to 20 ng DNA
- Primers: Pro341F/Pro805R targeting V3-V4 region
- Blocking oligonucleotides for host DNA contamination
- Library Preparation and Sequencing: Illumina MiSeq with 300bp paired-end reads
- Bioinformatic Analysis: DADA2 pipeline for ASV inference
RNA-based approaches demonstrate approximately 10-fold higher sensitivity for low-biomass samples like uterine microbiota, revealing additional taxonomic units undetected by DNA-based analysis [44].
Visual Guide to 16S rRNA Sequencing Selection
The diagram below illustrates the decision pathway for selecting appropriate 16S rRNA sequencing strategies based on research objectives and sample characteristics.
Research Reagent Solutions
The table below outlines essential research reagents and materials for implementing robust 16S rRNA amplicon sequencing protocols.
Table 3: Essential research reagents and resources for 16S rRNA amplicon sequencing
| Reagent/Resource | Specific Example | Function/Application | Considerations |
|---|---|---|---|
| DNA Extraction Kit | Quick-DNA Fecal/Soil Microbe Microprep Kit (Zymo Research) | Comprehensive lysis of diverse bacterial species | Bead beating improves Gram-positive bacteria lysis |
| RNA/DNA Co-Extraction Kit | AllPrep DNA/RNA/miRNA Universal Kit (Qiagen) | Simultaneous nucleic acid purification | Essential for DNA/RNA correlation studies |
| High-Fidelity Polymerase | KAPA HiFi HotStart ReadyMix (Roche) | Accurate amplification of target regions | Reduces PCR-induced errors in amplicons |
| PCR Primers | 27F/1492R (full-length); 341F/806R (V3-V4) | Target-specific amplification | Full-length primers enable complete gene coverage |
| Reference Database | MultiTax-Human, GTDB, SILVA | Taxonomic classification accuracy | GTDB provides genome-based taxonomy [41] [45] |
| Bioinformatic Tools | DADA2, QIIME2, EPI2ME | ASV inference, quality control | DADA2 provides precise denoising [43] |
| Mock Community | ZymoBIOMICS Microbial Standards | Protocol validation, error rate estimation | Essential for benchmarking performance |
The evolving landscape of 16S rRNA amplicon sequencing presents researchers with multiple technological pathways, each offering distinct advantages and limitations. Full-length sequencing platforms (PacBio and Oxford Nanopore) demonstrate clear superiority for species-level identification and polymicrobial sample analysis, while short-read platforms (Illumina) remain cost-effective for large-scale genus-level profiling. Critical considerations for experimental design include sample type, community complexity, and required taxonomic resolution. The emergence of improved reference databases like GTDB and MultiTax-Human, coupled with flexible classification thresholds, continues to enhance taxonomic accuracy. As the field progresses toward consensus standards, researchers should prioritize platform selection based on clearly defined research objectives rather than defaulting to traditional methodologies.
Shotgun metagenomics has revolutionized microbiome research by enabling unparalleled resolution in profiling microbial communities. Unlike targeted approaches such as 16S rRNA gene sequencing, shotgun metagenomics sequences all genomic material in a sample, providing two critical advantages: the ability to resolve microorganisms at the strain level and direct access to the functional gene repertoire of the community [46] [47]. This comprehensive profiling is transforming our understanding of microbial ecology and host-microbe interactions in health and disease.
The analytical process involves sophisticated computational workflows that progress from raw sequencing data to assembled genomes and functional annotations. While 16S sequencing offers a cost-effective method for coarse taxonomic profiling, it detects only a portion of the community revealed by shotgun sequencing and provides limited functional insights [48] [46]. As noted in an international consensus statement, both amplicon and whole-genome sequencing are reliable for community profiling, but shotgun metagenomics provides significantly more detailed information [7].
This guide compares the performance of leading shotgun metagenomics tools and methodologies, providing experimental data and protocols to inform researchers' analytical choices.
Performance Comparison of Metagenomic Binning Tools
Metagenomic binning—the process of grouping DNA fragments into metagenome-assembled genomes (MAGs)—is crucial for reconstructing microbial genomes from complex mixtures. Performance varies significantly across tools and depends on sequencing data type and analytical approach.
Benchmarking Across Data Types and Binning Modes
A comprehensive 2025 benchmark evaluated 13 binning tools across seven "data-binning combinations" (specific pairings of data type and binning strategy) [49]. The study assessed recovery of moderate-or-higher quality (MQ, completeness >50%, contamination <10%), near-complete (NC, completeness >90%, contamination <5%), and high-quality (HQ, NC criteria plus rRNA and tRNA genes) MAGs [49].
Table 1: Top-Performing Binning Tools Across Data-Binning Combinations
| Data-Binning Combination | Top-Performing Tools | Key Performance Notes |
|---|---|---|
| Short-read + Multi-sample | COMEBin, MetaBinner | Multi-sample binning recovered 100% more MQ MAGs and 194% more NC MAGs than single-sample in marine data [49] |
| Short-read + Co-assembly | Binny | Ranked first in this specific combination [49] |
| Long-read + Multi-sample | COMEBin, MetaBinner | Recovered 50% more MQ, 55% more NC, and 57% more HQ MAGs versus single-sample in marine data [49] |
| Hybrid + Multi-sample | COMEBin, MetaBinner | Moderate performance improvement over single-sample binning [49] |
| All Combinations | MetaBAT 2, VAMB, MetaDecoder | Highlighted for excellent scalability across diverse datasets [49] |
Multi-sample binning (using coverage information across multiple samples) consistently outperformed single-sample and co-assembly approaches across short-read, long-read, and hybrid data types [49]. In marine datasets with 30 samples, multi-sample binning recovered 100% more MQ MAGs and 194% more NC MAGs compared to single-sample binning with short-read data [49]. This approach also demonstrated superior capability in identifying potential antibiotic resistance gene hosts and biosynthetic gene clusters [49].
Impact of Binning on Functional Insights
The quality of binning directly impacts downstream biological interpretations. Multi-sample binning identified 30%, 22%, and 25% more potential antibiotic resistance gene hosts across short-read, long-read, and hybrid data respectively, compared to single-sample approaches [49]. For biosynthetic gene clusters in near-complete strains, multi-sample binning recovered 54%, 24%, and 26% more potential clusters across the same data types [49].
Table 2: Functional Advantages of Multi-Sample Binning
| Functional Category | Data Type | Improvement over Single-Sample Binning |
|---|---|---|
| ARG Host Identification | Short-read | +30% [49] |
| Long-read | +22% [49] | |
| Hybrid | +25% [49] | |
| BGCs in NC Strains | Short-read | +54% [49] |
| Long-read | +24% [49] | |
| Hybrid | +26% [49] |
Methodologies for Strain-Level Resolution and Functional Profiling
Experimental Workflow for Shotgun Metagenomics
The following diagram illustrates the comprehensive workflow for shotgun metagenomic analysis, from sample preparation through strain-level resolution and functional profiling:
Methodological Details
DNA Extraction and Sequencing
Optimal DNA extraction methods should maximize yield while preserving representation of all community members. For stool samples, the NucleoSpin Soil Kit (Macherey-Nagel) and DNeasy PowerLyzer PowerSoil kit (Qiagen) have been successfully used in comparative studies [46]. Library preparation typically uses Illumina Nextera XT for DNA sequencing [50].
Quality Control and Host DNA Removal
Host DNA contamination can exceed 90% in host-associated samples, significantly impacting downstream analysis [51]. Effective host DNA removal is essential before proceeding with assembly and binning. A 2025 benchmark compared six removal tools and found:
- Kraken2 demonstrated optimal speed and resource efficiency for host removal [51]
- KneadData (which integrates Bowtie2) is widely adopted but more computationally intensive [51]
- Using an accurate host reference genome significantly improves decontamination performance across all tools [51]
Removing host DNA reduces computational time for assembly by 20.55 times and for functional annotation by 7.63 times compared to analyzing raw data with host contamination [51].
Assembly, Binning, and MAG Refinement
The benchmark by [49] employed the following protocol for MAG generation:
- Assembly: MEGAHIT for short-read data, metaSPAdes for hybrid assemblies
- Binning: 13 different tools evaluated including COMEBin, MetaBinner, Binny, MetaBAT 2, VAMB, and MetaDecoder
- MAG Refinement: MetaWRAP, DAS Tool, and MAGScoT were used to combine results from multiple binners
- Quality Assessment: CheckM 2 for assessing completeness and contamination
MetaWRAP showed the best overall performance in recovering high-quality MAGs, while MAGScoT achieved comparable results with better scalability [49].
Strain-Level Resolution Techniques
Strain-level analysis provides critical insights into microbial epidemiology, functional specialization, and host adaptation. The following diagram illustrates the technical approaches for strain-level resolution:
Meteor2 implements strain-level analysis by tracking single nucleotide variants (SNVs) in signature genes of Metagenomic Species Pangenomes (MSPs) [52]. This approach identified 9.8% more strain pairs in human datasets and 19.4% more in mouse datasets compared to StrainPhlAn [52].
Long-read sequencing technologies (PacBio HiFi, Oxford Nanopore) enable more complete genome assemblies by resolving repetitive regions that fragment in short-read data [49] [53]. Hybrid assembly combining short and long reads further enhances assembly quality and strain resolution [49].
Functional Potential Analysis
Functional profiling determines the metabolic capabilities of a microbial community by identifying and quantifying genes and pathways.
Meteor2 provides comprehensive taxonomic, functional, and strain-level profiling (TFSP) using environment-specific microbial gene catalogs [52]. Its annotation pipeline includes:
- KEGG Orthology (KO) for functional orthologs using KofamScan
- Carbohydrate-active enzymes (CAZymes) using dbCAN3
- Antibiotic resistance genes (ARGs) using Resfinder and complementary databases
In benchmarks, Meteor2 improved species detection sensitivity by at least 45% in shallow-sequenced human and mouse gut microbiota compared to MetaPhlAn4 or sylph [52]. For functional profiling, it improved abundance estimation accuracy by at least 35% compared to HUMAnN3 based on Bray-Curtis dissimilarity [52].
Table 3: Key Research Reagent Solutions for Shotgun Metagenomics
| Category | Tool/Resource | Function | Application Notes |
|---|---|---|---|
| Binning Tools | COMEBin | Contig binning using contrastive learning | Top performer in 4/7 data-binning combinations [49] |
| MetaBinner | Ensemble binning algorithm | Top performer in 2/7 data-binning combinations [49] | |
| VAMB, MetaBAT 2 | Variational autoencoders; tetranucleotide+coverage binning | Recommended for excellent scalability [49] | |
| Profiling Platforms | Meteor2 | Taxonomic, functional, strain-level profiling | Uses environment-specific gene catalogs; fast mode available [52] |
| bioBakery Suite | Integrated taxonomy (MetaPhlAn), function (HUMAnN), strain (StrainPhlAn) | Comprehensive but may require additional annotations [52] | |
| Host DNA Removal | Kraken2 | k-mer based host sequence identification | Fast, resource-efficient performance [51] |
| KneadData | Integration of Bowtie2 for host removal | Widely adopted but computationally intensive [51] | |
| MAG Refinement | MetaWRAP | Bin refinement combining multiple tools | Best overall performance in recovering high-quality MAGs [49] |
| MAGScoT | Scalable bin refinement | Comparable to MetaWRAP with better scalability [49] | |
| Functional Databases | KEGG | Metabolic pathway annotation | Annotated via KofamScan in Meteor2 [52] |
| dbCAN | Carbohydrate-active enzyme database | Used for CAZyme annotation [52] | |
| Resfinder | Antibiotic resistance gene database | Clinically relevant ARGs from culturable pathogens [52] |
Consensus Framework for Metagenomic Analysis
An international multidisciplinary expert panel has established consensus recommendations for microbiome testing in clinical practice [7]. While focused on clinical applications, their framework provides valuable guidance for research settings:
- Technology Selection: Both amplicon and whole-genome sequencing are appropriate for community profiling, but researchers should clearly understand their distinct capabilities and limitations [7]
- Standardized Reporting: Results should include details on methods of stool collection, storage, DNA extraction, and sequencing analysis to ensure reproducibility [7]
- Multi-Omics Integration: Combining metagenomics with metabolomics, transcriptomics, and proteomics provides a more comprehensive understanding of microbial community function [47] [53]
The integration of multiple binning tools through refinement pipelines like MetaWRAP and MAGScoT represents a consensus approach in the field, leveraging the complementary strengths of different algorithms to produce superior results [49].
Shotgun metagenomics provides unparalleled resolution for strain-level microbial analysis and functional potential assessment. Multi-sample binning strategies consistently outperform single-sample approaches across sequencing platforms, with COMEBin and MetaBinner emerging as top performers in recent benchmarks. The field is advancing toward consensus frameworks that integrate multiple tools and methodologies to maximize recovery of high-quality metagenome-assembled genomes.
Methodological choices significantly impact results—from host DNA removal through strain-level analysis. Researchers should select tools aligned with their specific research questions, data types, and computational resources. As the field progresses, standardized workflows and reporting practices will enhance reproducibility and enable more meaningful comparisons across studies, ultimately strengthening the translation of microbiome research into clinical and biotechnological applications.
The analysis of complex microbial communities requires moving beyond compositional surveys to a functional understanding of microbiome activity. The integration of metatranscriptomics, metaproteomics, and metabolomics represents a powerful consensus approach that bridges the gap between genetic potential and biochemical reality. While metagenomics reveals "who is there" and their functional potential, it provides limited insight into actual microbial activity [54]. Metatranscriptomics captures community-wide gene expression, revealing which genes are actively transcribed under specific conditions. Metaproteomics identifies and quantifies the proteins executing biological functions, while metabolomics profiles the final metabolic products that represent the ultimate output of microbial activity [54]. This multi-omics framework provides complementary layers of functional evidence that, when integrated, offer a validated consensus view of microbiome functionality that is more robust than any single approach alone.
Recent advances in analytical technologies and computational frameworks have made such integration increasingly feasible, supporting the validation of microbiome functions through cross-omics verification. This comparative guide examines the technical performance, experimental requirements, and complementary strengths of these three omics layers within the context of microbiome analysis consensus approach validation research.
Technology Performance Comparison
The table below summarizes the core performance characteristics, strengths, and limitations of each omics approach for microbiome research.
Table 1: Performance Comparison of Functional Omics Technologies in Microbiome Research
| Parameter | Metatranscriptomics | Metaproteomics | Metabolomics |
|---|---|---|---|
| Analytical Target | Total community RNA (mRNA) | Proteins and peptides | Small molecules and metabolites |
| Key Platforms | RNA-Seq (e.g., Illumina) | LC-MS/MS (Tandem Mass Spectrometry) | LC-MS, GC-MS, NMR |
| Temporal Resolution | Minutes to hours (rapid turnover) | Hours to days (moderate turnover) | Minutes to hours (rapid turnover) |
| Biomass Requirements | Moderate to high (RNA yield critical) | High (microgram protein amounts) | Low (minimal sample volume) |
| Depth of Coverage | 10-100 million reads per sample | 1,000-10,000 protein groups | 100-10,000 metabolites |
| Primary Challenge | Host RNA contamination, RNA stability | Dynamic range, protein extraction | Chemical diversity, quantification |
| Key Strength | Identifies active regulatory mechanisms | Direct measurement of functional elements | Captures end-point phenotype |
Performance Metrics and Data Output
Metatranscriptomics delivers insights into actively regulated pathways rather than simply cataloging genetic potential. Recent studies demonstrate that complementing whole metagenome sequencing with metatranscriptomics data allows for more accurate assessment of gene expression levels, providing functional insights that complement genomic information [54]. However, challenges include substantial host RNA contamination in human-associated samples and the technical difficulty of isolating high-quality microbial mRNA [54].
Metaproteomics provides direct functional evidence by quantifying protein expression. A 2025 large-scale study systematically mapped metaproteomic responses of ex vivo human gut microbiota to 312 compounds, generating 4.6 million microbial protein measurements and identifying significant metaproteomic shifts induced by 47 compounds, with neuropharmaceuticals as the sole drug class significantly enriched among these hits [55]. The main limitations include the requirement for high microbial biomass and challenges in protein extraction efficiency from complex samples.
Metabolomics captures the functional output of microbial communities, offering the most direct representation of microbial activity. Untargeted LC-MS/MS-based metabolomics generates substantial datasets requiring sophisticated visualization strategies for interpretation, including volcano plots for treatment impacts and cluster heatmaps for pattern recognition [56]. The extreme chemical diversity of metabolites presents challenges for comprehensive extraction and identification.
Experimental Protocols and Methodologies
Metatranscriptomics Workflow: metaTP Pipeline
The metaTP pipeline represents a recently developed integrated automated workflow for comprehensive metatranscriptomic analysis [57]. This protocol ensures repeatability, reproducibility, and traceability of results:
Sample Collection and RNA Stabilization: Collect samples in RNAlater or similar stabilization reagent. Immediate freezing at -80°C is acceptable for some sample types.
Total RNA Extraction: Use commercial kits with bead-beating for mechanical lysis of diverse microbial cells. Include DNase treatment to remove genomic DNA contamination.
rRNA Depletion: Employ targeted probes to remove ribosomal RNA (using tools like bowtie2), which typically constitutes >90% of total RNA [57].
Library Preparation and Sequencing: Use strand-specific protocols for Illumina platforms. Recommended sequencing depth: 20-50 million reads per sample for complex communities.
Bioinformatic Analysis with metaTP:
- Quality control with FastQC and adapter trimming with Trimmomatic
- Non-coding RNA removal and transcript assembly using MEGAHIT
- Transcript expression quantification with Salmon (output in TPM)
- Differential gene expression analysis using Wilcoxon rank-sum test
- Functional annotation via eggNOG-mapper against KEGG, GO databases
- Co-expression network analysis using ggClusterNet
The metaTP pipeline utilizes Snakemake for workflow automation, supporting parallel computing and enhanced reproducibility [57].
Metaproteomics Workflow: Clinical Metaproteomics Protocol
A standardized clinical metaproteomics workflow for host-microbiome dynamics has been presented across multiple research forums in 2024-2025 [58]:
Protein Extraction: Use SDS-based lysis buffer with protease inhibitors. Include mechanical disruption (bead-beating or sonication) for comprehensive cell lysis.
Protein Cleanup and Digestion: Perform filter-aided sample preparation (FASP) or in-solution digestion. Use trypsin/Lys-C mixture for overnight digestion at 37°C.
Peptide Fractionation (optional for complex samples): Use high-pH reverse-phase fractionation or SCX chromatography to reduce complexity.
LC-MS/MS Analysis:
- Liquid chromatography: C18 column with 60-120min gradients
- Mass spectrometry: Data-dependent acquisition (DDA) or data-independent acquisition (DIA) on Orbitrap instruments
- Tandem mass tags (TMT) enable multiplexing for high-throughput studies [55]
Database Search and Protein Identification:
- Customized database creation from metagenomic assemblies
- Search against combined host and microbial protein databases
- Use tools like FragPipe, Meta-iPep for immunopeptidomics applications [58]
Metabolomics Workflow: Untargeted LC-MS/MS Approach
For untargeted metabolomics, the following protocol is recommended [56]:
Metabolite Extraction: Use methanol:acetonitrile:water (4:4:2) or similar biphasic solvent system. Maintain consistent sample:solvent ratios.
LC-MS Analysis:
- Reverse-phase chromatography (C18) for non-polar metabolites
- HILIC chromatography for polar metabolites
- High-resolution mass spectrometer (Orbitrap or Q-TOF) in both positive and negative ionization modes
Data Processing:
- Feature detection and alignment (e.g., XCMS, MS-DIAL)
- Peak integration and retention time correction
- Compound identification using spectral libraries (GNPS, HMDB)
- Implement quality control with pooled quality control samples
Integrated Data Analysis Framework
Visualization Strategies for Multi-Omics Data Integration
Effective visualization is crucial for interpreting multi-omics datasets. Recommended strategies include [56] [59]:
- Volcano plots for displaying treatment impacts and significantly altered features
- Cluster heatmaps for visualizing patterns across samples and analytes
- Sankey diagrams for tracing metabolic pathways across omics layers
- Co-expression networks for identifying coordinated biological modules
- Multi-panel figures that show complementary evidence across omics types
Advanced visualization tools enable effective exploration, querying, and analysis of these complex datasets, making them accessible to both bioinformaticians and non-bioinformaticians [59].
Cross-Omics Validation Framework
A robust consensus approach requires cross-validation between omics layers:
Transcript-Protein Correlation: Identify genes with congruent mRNA and protein expression patterns. Discrepancies may indicate post-transcriptional regulation.
Protein-Metabolite Pathway Mapping: Map quantified enzymes to their corresponding metabolic products to validate pathway activity.
Stoichiometric Modeling: Integrate transcript/protein data with genome-scale metabolic models (GEMs) to predict metabolite fluxes and validate with measured metabolomics data.
A 2025 UTI microbiome study successfully integrated metatranscriptomic sequencing with genome-scale metabolic modeling to characterize active metabolic functions of patient-specific urinary microbiomes during acute infection, demonstrating how transcript-constrained models narrow flux variability and enhance biological relevance [60].
Research Reagent Solutions
Table 2: Essential Research Reagents and Platforms for Multi-Omics Microbiome Analysis
| Category | Specific Product/Platform | Application Note |
|---|---|---|
| RNA Stabilization | RNAlater, PAXgene Tissue Systems | Preserves RNA integrity during sample transport and storage |
| rRNA Depletion | Ribo-Zero Plus, NEBNext Microbiome | Critical for enhancing mRNA sequencing depth in metatranscriptomics |
| Protein Digestion | Trypsin/Lys-C mix, Filter-aided sample preparation (FASP) kits | Ensures complete and reproducible protein digestion for metaproteomics |
| Mass Spectrometry | Tandem Mass Tag (TMT) reagents, Orbitrap mass spectrometers | Enables multiplexed quantitative proteomics; high-resolution mass detection |
| Metabolite Extraction | Methanol:acetonitrile:water (4:4:2), Biphasic solvent systems | Comprehensive extraction of diverse metabolite classes |
| Bioinformatic Pipelines | metaTP, HUMAnN2, IMP, Galaxy-P | Integrated workflows for specific omics data analysis |
Signaling Pathways and Workflow Diagrams
Multi-Omics Integration Conceptual Framework
Experimental Workflow for Multi-Omics Microbiome Analysis
The integration of metatranscriptomics, metaproteomics, and metabolomics provides a robust framework for validating microbiome function through consensus evidence across biological layers. While each approach has distinct performance characteristics and technical requirements, their combination enables researchers to distinguish between genetic potential and actual functional activity in microbial communities. Metatranscriptomics reveals rapid regulatory responses, metaproteomics confirms protein expression, and metabolomics captures the resulting biochemical phenotype.
For researchers and drug development professionals, this multi-omics consensus approach offers enhanced validation for microbiome-based diagnostic development and therapeutic target identification. The experimental protocols and analytical frameworks presented here provide a foundation for implementing this integrated approach, with recent studies demonstrating its power in revealing functional responses to pharmaceuticals [55], characterizing infection mechanisms [60], and advancing personalized medicine through microbiome-informed diagnostics [61]. As these technologies continue to evolve, standardized workflows and visualization strategies will be crucial for translating multi-omics data into biologically meaningful insights and clinically actionable findings.
In microbiome research, the analysis of marker genes, such as the 16S rRNA gene, serves as a fundamental tool for linking microbial community composition to ecosystem function through cultivation-independent methods [62]. The certainty of results, independent of bioinformatic handling, is imperative for any scientific advances within the field [62]. Two principal methodological frameworks have emerged for processing sequencing data into biologically meaningful units: Operational Taxonomic Units (OTUs) and Amplicon Sequence Variants (ASVs). These approaches apply fundamentally different principles when dealing with technical sequencing biases and PCR artifacts, leading to distinct implications for data interpretation and biological conclusions [62] [63].
The field is currently undergoing a significant transition. While OTU clustering has been the traditional workhorse for over a decade, recent methodological advances are driving a shift toward ASV-based analysis [64] [65]. This shift reflects an evolving understanding of microbial ecology and the increasing demand for higher resolution and reproducibility in microbiome studies. The choice between these pipelines extends beyond technical preference, directly influencing the ecological narrative that emerges from sequence data, including assessments of diversity, community structure, and functional predictions [66]. Within the context of validating consensus approaches for microbiome analysis, understanding the technical nuances and empirical performance of these methods becomes paramount for generating robust, comparable datasets that can support drug development and clinical applications.
Fundamental Principles and Technical Mechanisms
OTU Clustering: The Traditional Approach
Operational Taxonomic Unit (OTU) clustering is a similarity-based method that groups sequencing reads into clusters based on a predefined identity threshold, traditionally set at 97% [64] [67]. This threshold was historically chosen to approximate the species-level boundary in prokaryotes [65]. The underlying principle of OTU clustering is that related organisms possess similar target gene sequences, and rare sequencing errors will have a trivial contribution to the consensus sequence representing each cluster [63]. This approach effectively "averages out" technical variations by creating abstracted units.
There are three primary methods for generating OTUs, each with distinct operational characteristics. De novo clustering creates OTU clusters entirely from observed sequences without a reference database, requiring significant computational resources and making cross-study comparisons challenging because the same sequence may cluster differently depending on other sequences in the dataset [63]. Closed-reference clustering compares sequences against a pre-existing reference database, offering computational efficiency and easy comparability between studies using the same database, but discards sequences not present in the reference, thereby introducing substantial bias against novel taxa [63]. Open-reference clustering represents a hybrid approach that first clusters sequences against a reference database (like closed-reference) and then clusters the remaining unclassified sequences de novo, attempting to balance computational efficiency with the ability to detect novel organisms [63].
ASV Inference: The High-Resolution Alternative
Amplicon Sequence Variants (ASVs) represent a paradigm shift from clustering to denoising. Instead of grouping similar sequences, ASV methods employ statistical models to distinguish true biological sequences from sequencing errors, resulting in exact, single-nucleotide resolution sequence variants [63] [67]. The ASV approach starts by determining the exact sequences and their frequencies, then combines this information with an error model for the specific sequencing run [63]. This enables a probabilistic determination of whether each exact sequence represents a true biological variant as opposed to a technical artifact.
Several sophisticated algorithms form the foundation of ASV analysis. DADA2 (Divisive Amplicon Denoising Algorithm) uses a parameterized model of substitution errors to infer true sequences, employing a divisive partitioning algorithm that models sequencing errors as a mixture of binomial and gamma distributions [67]. Deblur operates by applying an error profile to identify and remove erroneous sequences in a quality-aware manner, using an iterative process that trims reads to a uniform length and predicts error-free sequences. UNOISE functions by clustering sequences in a dendrogram and then removing branches suspected to represent errors based on their abundance and divergence, effectively filtering out low-count noise sequences.
Table 1: Core Algorithmic Foundations of OTU and ASV Methods
| Method | Representative Tools | Core Algorithmic Principle | Primary Output |
|---|---|---|---|
| OTU Clustering | UPARSE, VSEARCH, mothur | Groups sequences based on pairwise similarity thresholds (typically 97%) | Consensus sequences representing cluster centroids |
| ASV Inference | DADA2, Deblur, QIIME2 | Uses statistical error models to correct sequencing artifacts and identify true biological variants | Exact DNA sequences with single-nucleotide resolution |
Direct Performance Comparison and Experimental Data
Quantitative Differences in Community Composition
Empirical studies directly comparing OTU and ASV pipelines reveal significant quantitative differences in their output. Research analyzing thermophilic anaerobic co-digestion experimental data together with prokaryotic community data found that while both pipelines generally allowed for similar ecological interpretations, they delivered community compositions that differed between 6.75% and 10.81% [62]. These pipeline-dependent discrepancies in taxonomic assignment could lead to different biological conclusions, particularly affecting downstream analyses such as network inference or ecosystem service predictions for misidentified or unidentified species [62].
The fundamental resolution differences between methods are striking. A comprehensive ecological study comparing these approaches across 17 adjacent habitats found that ASV-based analysis consistently provided higher resolution of microbial communities, capturing subtle biological variations that were obscured by OTU clustering [65]. This has direct implications for detecting true microbial diversity, as ASVs can distinguish closely related organisms that would be grouped into a single OTU using the conventional 97% similarity threshold.
Impact on Ecological Diversity Metrics
The choice of bioinformatic pipeline significantly influences alpha, beta, and gamma diversity measures, which are fundamental to ecological interpretation. Research demonstrates that OTU clustering consistently leads to marked underestimation of ecological indicators for species diversity compared to ASV-based analysis [65]. This distortion extends to dominance and evenness indexes, potentially skewing understanding of community structure and dynamics.
Table 2: Comparative Effects on Diversity Metrics Based on Experimental Data
| Diversity Metric | OTU Clustering Effect | ASV Inference Effect | Ecological Interpretation Impact |
|---|---|---|---|
| Alpha Diversity (within-sample) | Underestimation due to clustering of distinct variants | Higher observed richness due to single-nucleotide resolution | ASVs capture more comprehensive diversity, including rare biosphere |
| Beta Diversity (between-sample) | Potentially distorted community relationships | More accurate differentiation between communities | ASV-based ordinations show superior coherence in multivariate space |
| Gamma Diversity (overall regional) | Reduced due to clustering of geographically distinct variants | Preservation of regional diversity patterns | ASVs better capture true biogeographic patterns and endemic taxa |
The performance differences extend to handling technical challenges in microbiome analysis. When studying low-abundance sequences, ASV methods like DADA2 have demonstrated superior sensitivity in distinguishing true rare sequences from technical artifacts [63] [65]. In contamination scenarios, ASV-based approaches showed better ability to differentiate sample biomass from contaminants when the nature of these populations was known [63]. For chimera detection, ASVs offer a distinct advantage because chimeric sequences can be identified as exact recombinants of more prevalent parent sequences within the same sample [63].
Experimental Protocols and Methodological Workflows
Representative Experimental Design
To illustrate the practical implementation of these methods, consider a published experimental setup designed specifically for pipeline comparison [62]. The research employed lab-scale reactors simulating anaerobic co-digestion (Co-AD) of primary and waste-activated sewage sludge (PWASS) with food waste (FW). Six reactors with 500 mL working volume were operated at 55°C over 170 days, with regular feeding and monitoring of performance parameters including methane production, volatile fatty acids (VFAs), pH, and solids content.
Sampling for DNA extraction occurred at the end of each co-substrate addition period from each reactor, alongside PWASS and inoculum samples, resulting in 36 individual samples. DNA was extracted using the Soil DNA Isolation Plus Kit, with concentrations ranging between 10.7 ng and 338.6 ng μL−1. The hypervariable V3–V4 region of the 16S rRNA gene was amplified using primers Pro341f/Pro805r and sequenced on the Illumina MiSeq platform with V2 chemistry [62]. This experimental design provided a realistic, complex microbial community context for evaluating bioinformatic pipeline performance.
Comparative Bioinformatics Workflow
The following diagram illustrates the key procedural differences between OTU and ASV analysis workflows:
Essential Research Reagents and Tools
Table 3: Key Research Reagents and Computational Tools for Pipeline Implementation
| Category | Specific Tools/Reagents | Function in Analysis Pipeline |
|---|---|---|
| Wet Lab Reagents | Soil DNA Isolation Plus Kit (Norgen) | DNA extraction from complex samples |
| Pro341f/Pro805r Primers | Amplification of 16S rRNA V3-V4 region | |
| Illumina MiSeq Platform (V2 chemistry) | High-throughput amplicon sequencing | |
| OTU Analysis Tools | VSEARCH, UPARSE, mothur | Sequence clustering and OTU generation |
| SILVA, Greengenes Databases | Reference databases for taxonomic assignment | |
| ASV Analysis Tools | DADA2 (R package), Deblur (QIIME2) | Error modeling and exact sequence variant inference |
| QIIME2 Platform | Integrated analysis environment for ASVs | |
| Downstream Analysis | phyloseq (R package) | Ecological and statistical analysis of microbiome data |
Consensus and Recommendations for Research Applications
Current Field Consensus and Guidelines
International consensus statements on microbiome testing in clinical practice have provided valuable guidance on analytical methodologies. Expert panels recommend that appropriate modalities for gut microbiome community profiling include both amplicon sequencing and whole genome sequencing, acknowledging the value of different bioinformatic approaches depending on the research context [7]. Currently, there is recognition that the field is transitioning toward methods with increased reproducibility and ease of comparison between studies [63] [7].
The emerging consensus suggests that ASV-based methods present significant advantages for studies exploring novel environments or sample sources where reference databases have limited representation [63]. This is particularly relevant for environmental studies that contain several uncharacterized species, where reference-based OTU clustering would carry disadvantageous biases, including the risk of missing novel taxa not yet represented in databases [65]. For clinical applications, standardization and reproducibility are paramount, making ASVs an increasingly attractive option as the field moves toward diagnostic implementation.
Practical Selection Framework for Researchers
The choice between OTU and ASV methods should be guided by specific research objectives, sample types, and resource considerations. The following decision framework can assist researchers in selecting the appropriate pipeline:
For maximal resolution and reproducibility: ASV-based approaches are strongly recommended, particularly for studies requiring strain-level discrimination or planning future meta-analyses [64] [66]. The exact sequence variants generated by ASV methods enable direct comparison across studies and platforms, facilitating cumulative knowledge building.
For legacy data integration: OTU clustering may be preferable when the primary research goal involves direct comparison with existing datasets generated using OTU methodologies [64] [67]. This maintains methodological consistency for longitudinal or comparative study designs.
For computationally constrained environments: OTU clustering, particularly closed-reference approaches, demands fewer computational resources than ASV inference and may be more practical for very large datasets or limited computing infrastructure [63] [67].
For novel microbial discovery: ASV methods with de novo taxonomic assignment outperform closed-reference OTU clustering in identifying previously uncharacterized taxa, making them superior for exploratory studies in underexplored environments [63] [65].
As the field continues to evolve, methodological standardization will be essential for validating consensus approaches in microbiome analysis. The trajectory clearly points toward higher-resolution, reproducible methods like ASVs as the foundation for robust microbiome research with translational applications in drug development and clinical diagnostics [7] [25].
The human gut microbiome, a complex ecosystem of trillions of microorganisms, has emerged as a crucial therapeutic target for a range of diseases. Over the past decade, microbiome-based therapies have evolved from empirical procedures to standardized pharmaceutical products, creating a new modality in medical treatment. This evolution encompasses several distinct therapeutic classes: traditional Fecal Microbiota Transplantation (FMT), which involves transferring minimally processed stool from healthy donors; Live Biotherapeutic Products (LBPs), which are defined bacterial consortia or single strains manufactured under strict quality control; and microbiome-based drugs that target microbial functions or composition [68] [69]. The successful application of these therapies for recurrent Clostridioides difficile infection (rCDI) has validated the broader concept of manipulating the microbiome to treat disease, sparking investigation into numerous other conditions including inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), metabolic disorders, and even cancer [70] [71]. This guide provides a comprehensive comparison of these therapeutic modalities, their mechanisms, clinical evidence, and practical research considerations to inform development efforts.
Comparative Analysis of Therapeutic Modalities
Fecal Microbiota Transplantation (FMT): From Concept to Regulated Therapy
FMT represents the most direct approach to microbiome manipulation, transferring the complete microbial community from a healthy donor to restore ecological balance in the recipient. Initially used as an unstandardized procedure, FMT has progressively moved toward regulation and standardization [68].
Mechanism of Action: FMT works through ecosystem restoration, reestablishing colonization resistance against pathogens through multiple complementary mechanisms. These include: restoration of secondary bile acid metabolism, regeneration of short-chain fatty acid production, introduction of functional genes via mobile genetic elements, and direct competition for ecological niches [68]. This multi-mechanistic approach distinguishes FMT from more targeted therapies.
Clinical Applications and Efficacy: FMT has demonstrated remarkable success in rCDI, with sustained response rates exceeding 80% in select populations [70]. This efficacy stems from its ability to address the fundamental dysbiosis caused by repeated antibiotic courses. Beyond rCDI, FMT is being investigated for severe and fulminant CDI in patients not responding to antibiotics, with emerging research in decolonizing multidrug-resistant organisms and managing non-infectious conditions like IBD, IBS, liver disease, and metabolic syndrome [70].
Regulatory Landscape: The regulatory status of FMT has evolved significantly. In the United States, the FDA initially classified FMT as a drug and biologic but exercised enforcement discretion for rCDI treatment. With the approval of commercial FMT-based products, this policy has shifted toward requiring investigational new drug applications for stool banks [68] [70]. In contrast, the European Union has implemented the Substances of Human Origin (SoHO) Regulation, which includes fecal microbiota alongside other human-derived substances, aiming to balance patient access with product development [68].
Live Biotherapeutic Products (LBPs): Engineered Microbial Therapeutics
LBPs represent a pharmaceutical approach to microbiome modulation, comprising defined bacterial strains manufactured under controlled conditions. Three distinct product architectures have emerged, each with different clinical applications and manufacturing considerations [69].
Table 1: Architecture of Live Biotherapeutic Products
| Product Architecture | Description | Key Examples | Target Indications |
|---|---|---|---|
| Whole-community LBPs | Standardized formulations preserving microbial diversity of complete fecal microbiota | REBYOTA (Ferring), mBK-01 (Mikrobiomik) | rCDI, with investigation in complex diseases |
| Partial-community/Enriched LBPs | Products enriched for specific functional microbial groups while maintaining substantial diversity | MaaT013 (MaaT Pharma) - enriched for butyrate producers | aGvHD with GI involvement, cancer supportive care |
| Defined-strain LBPs | Precisely defined bacterial consortia or single strains targeting specific mechanisms | VOWST (Seres/Nestlé), VE303, NTCD-M3 | rCDI, IBD, IBS, and other immune-mediated conditions |
Mechanistic Foundations: Unlike FMT's ecosystem restoration approach, defined-strain LBPs operate on the principle that therapeutic effects can be achieved without replicating entire microbial communities. The selection of specific strains is based on mechanism-driven criteria such as bile acid metabolism, immunomodulatory properties, or production of specific metabolites [69]. This targeted approach enables more precise product characterization and consistent manufacturing but may lack the functional redundancy of complete communities.
Manufacturing Considerations: LBP development faces unique manufacturing challenges, particularly in maintaining viability of fastidious anaerobic bacteria through fermentation, lyophilization, and storage. Process optimization must begin pre-IND to avoid late-stage delays, with critical parameters including lyophilization survival (which varies by strain and growth phase), media reformulation for GMP scale-up, and potency assurance through temperature excursion testing [69]. Strain selection profoundly impacts manufacturability, with growth kinetics and lyophilization tolerance being key considerations alongside therapeutic properties.
Microbiome-Based Drugs: Beyond Whole Microbes
The microbiome therapeutic landscape extends beyond whole microbes to include postbiotics (bioactive compounds derived from microbes) and genetically engineered strains with enhanced therapeutic functions. These approaches offer potential advantages in stability, safety, and precise mechanism targeting [71].
Postbiotics: These non-viable bacterial products or metabolic byproducts demonstrate therapeutic potential without requiring microbial viability or colonization. Recent systematic reviews indicate benefits for IBS symptoms, including reduced severity, pain reduction, and improved quality of life [71]. Advantages include better stability, non-viability (making them potentially safer for immunocompromised patients), and longer shelf life compared to live products.
Engineered Microbial Therapeutics: Advanced genetic engineering enables creation of microbial chassis with enhanced therapeutic functions. For example, research presented at Digestive Disease Week 2025 highlighted genetically engineered E. coli Nissle for calprotectin-responsive treatment of IBD and Akkermansia muciniphila that produces inosine to relieve diarrhea-predominant IBS through improved intestinal water absorption [71]. However, significant challenges remain in engraftment and safety assessment, particularly regarding potential genotoxicity of certain microbial strains.
Clinical Performance and Comparative Efficacy
Established Indications: Recurrent Clostridioides difficile Infection
rCDI represents the most established indication for microbiome-based therapies, with robust clinical evidence supporting multiple approaches. The table below summarizes key efficacy data for approved and investigational products.
Table 2: Clinical Efficacy of Microbiome-Based Therapies for rCDI
| Therapeutic Modality | Specific Product/Approach | Clinical Trial Data | Efficacy Results | Safety Profile |
|---|---|---|---|---|
| Traditional FMT | OpenBiome cryopreserved preparation | Retrospective analysis of >60,000 treatments [69] | ~80-90% resolution of rCDI | Generally favorable; infection risks from improper screening |
| Whole-community LBP | REBYOTA (fecal microbiota, live-jslm) | Phase 3 PUNCH CD3 trial [70] [72] | 70.6% success at 8 weeks; 90% sustained response at 6 months | Mild-moderate GI events (abdominal pain, diarrhea, bloating) |
| Whole-community LBP | REBYOTA by colonoscopy | Phase 3b CDI-SCOPE trial [72] | 95% treatment success at 8 weeks | Consistent with pivotal studies; no new safety signals |
| Defined-strain LBP | VOWST (fecal microbiota spores, live-brpk) | Phase 3 ECOSPOR III trial [70] | ~80% efficacy in preventing recurrence | Well-tolerated; mild GI adverse events |
| Enriched LBP | MaaT013 (Microbiome Ecosystem Therapy) | Phase 3 trial (EMA application 2025) [69] | Improved survival in aGvHD with GI involvement | Manageable safety profile in immunocompromised |
Recent real-world evidence continues to support the clinical utility of these approaches. The Phase 3b CDI-SCOPE trial of REBYOTA demonstrated 95% treatment success when administered by colonoscopy, with microbiome analyses showing significant shifts toward healthier composition sustained through six months, including increased beneficial Bacteroidia and Clostridia with decreased disease-associated Gammaproteobacteria and Bacilli [72].
Investigational Applications: Beyond C. difficile
Microbiome-based therapies show promise for diverse conditions characterized by dysbiosis, though evidence levels vary considerably across indications:
Inflammatory Bowel Disease: Systematic reviews indicate that FMT can effectively induce clinical and endoscopic remission in mild-to-moderate ulcerative colitis without significantly increased adverse events [71]. However, data for maintaining remission after FMT remains limited, and results for Crohn's disease are less consistent.
Irritable Bowel Syndrome: A recent systematic review found 64% of FMT participants experienced improved IBS symptoms at 3 months compared to 42% with placebo, though evidence quality was low [71]. The mechanisms may involve modulation of bacterial metabolites like lysophosphatidylcholine (LPC) and lysophosphatidic acid (LPA), which induce neuronal activation and visceral hypersensitivity [71].
Oncology Supportive Care: MaaT Pharma's MaaT013 has shown promise for acute graft-versus-host disease (aGvHD) with gastrointestinal involvement, a life-threatening complication of allogeneic stem cell transplantation with no approved therapies [69]. The company submitted a marketing authorization application to the European Medicines Agency in June 2025 based on improved survival outcomes.
Metabolic and Autoimmune Conditions: Early research suggests potential applications for obesity, type 2 diabetes, and multiple sclerosis, though these remain primarily preclinical or in early clinical development [73] [23].
Experimental Design and Methodological Framework
Pharmacological Characterization of Microbiome Therapies
The complex, living nature of microbiome therapies necessitates adaptation of traditional pharmacological frameworks. A proposed model for FMT pharmacokinetics includes the parameters of Engraftment, Metagenome, Distribution, and Adaptation (EMDA), which mirror the classic ADME parameters for conventional drugs [68].
Diagram 1: Pharmacokinetic Framework for FMT. This model adapts traditional pharmacokinetic concepts to the unique properties of live microbiome therapies, focusing on microbial engraftment, functional gene acquisition, spatial distribution, and ecological adaptation.
For pharmacodynamic assessment, researchers should evaluate both direct effects on the microbiome itself (e.g., content of antibiotic resistance genes, virulence factors) and effects on host physiology through microbial metabolites, immune modulation, and interaction with host systems [68]. Understanding these mechanisms is critical for rational product development.
Analytical Approaches for Microbiome Therapeutic Development
Advanced sequencing technologies and bioinformatic tools are essential for characterizing microbiome therapeutics and their effects. Key methodological considerations include:
Strain-Level Tracking: Tools like MAGEnTa enable cost-efficient tracking of donor microbiota engraftment using metagenome-assembled genomes directly from donor and pre-treatment metagenomic data, without relying on external databases [68]. This approach allows monitoring of both community and strain engraftment dynamics.
Functional Assessment: Beyond taxonomic composition, functional characterization through metagenomics and metabolomics provides critical insights into therapeutic mechanisms. For example, analyzing restoration of secondary bile acid metabolism and short-chain fatty acid production can explain anti-CDI effects, while immunomodulatory metabolite profiling reveals mechanisms relevant to inflammatory conditions [68] [23].
Ecological Metrics: Assessment of alpha diversity (within-sample diversity) and beta diversity (between-sample differences) provides important ecological context, though experts caution against overreliance on oversimplified metrics like the Firmicutes/Bacteroidetes ratio, which lacks sufficient evidence for clinical interpretation [14] [12].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Tools for Microbiome Therapeutic Development
| Tool Category | Specific Technologies/Platforms | Research Application | Key Considerations |
|---|---|---|---|
| Sequencing Technologies | Whole-genome sequencing (WGS), Long-read metagenomics, 16S rRNA sequencing | Strain identification, community profiling, engraftment tracking | WGS as gold standard for strain identification; long-read for improved assembly |
| Bioinformatic Tools | MAGEnTa, metagenome-assembled genomes (MAGs), ecological diversity metrics | Donor-recipient strain tracking, functional potential assessment | Cost-efficient pipelines needed for longitudinal analysis |
| Culture Systems | Anaerobic chambers, customized media, coculture systems | Strain isolation, interaction studies, safety testing | Essential for fastidious anaerobes; coculture for synergy assessment |
| Animal Models | Gnotobiotic mice, humanized microbiome models | Mechanistic studies, efficacy screening | Limited translatability; require human validation |
| Metabolomic Platforms | LC-MS, GC-MS, NMR spectroscopy | Functional assessment, mechanism of action studies | Correlation with microbial functions; multi-omic integration |
Regulatory and Manufacturing Considerations
Evolving Regulatory Frameworks
The regulatory landscape for microbiome therapies continues to evolve, with important differences between regions:
United States Framework: The FDA classifies FMT and LBPs as drugs and biologics, requiring compliance with traditional drug development pathways. The approval of REBYOTA and VOWST has established precedents for regulatory expectations, including rigorous safety profiling, potency assays, and manufacturing controls [68] [70]. The cessation of OpenBiome's operations following FDA approval of commercial products highlights the impact of regulatory decisions on market dynamics [68].
European Approach: The European Union's Substances of Human Origin (SoHO) Regulation takes a different approach, including fecal microbiota alongside other human-derived substances. This framework emphasizes donor safeguards and volunteer participation while attempting to preserve patient access and innovation potential [68]. The regulation aims to harmonize practices across member states while accommodating both traditional FMT and advanced LBPs.
Harmonization Efforts: The 2025 CHINAGUT Conference assembled 63 experts who developed 30 scientific recommendations to advance probiotics, LBPs, and FMT, addressing standardization, translation, supervision, and regulatory harmonization [74]. These interdisciplinary guidelines reflect growing recognition of the need for globally coordinated approaches to microbiome therapeutic development.
Manufacturing and Quality Control
Manufacturing microbiome therapies presents unique challenges that require specialized approaches:
Donor-Derived Products: For FMT and whole-community LBPs, rigorous donor screening is essential, including health assessment, pathogen testing, and longitudinal monitoring. Ethical donor recruitment practices emphasizing humanitarian participation rather than purely monetary incentives may reduce moral hazards and improve program integrity [68]. Pooled donations from multiple donors can ensure consistency and completeness of microbial representation [68] [69].
Defined-Strain Products: LBP manufacturing requires maintaining viability of fastidious anaerobes through fermentation, purification, and lyophilization processes. Co-fermentation of strains offers efficiency advantages but requires careful purity testing, while monoculture-then-blend approaches provide better strain-level control [69]. Process parameters must be optimized for each specific strain, as survival through lyophilization varies by strain and growth phase.
Potency and Stability Assurance: Ensuring consistent potency remains challenging due to the complex, living nature of these products. Stability studies must account for viability loss during storage and establish appropriate shelf life. Temperature excursion monitoring during distribution is critical for product quality [69].
Future Directions and Research Opportunities
The field of microbiome therapeutics continues to advance rapidly, with several promising directions emerging:
Mechanism-Driven Product Design: Future development will increasingly focus on products targeting specific molecular mechanisms rather than broad ecological restoration. This approach requires deeper understanding of microbial pathways influencing host physiology, such as bile acid transformation, immunomodulatory metabolite production, and direct receptor interactions [69] [71].
Personalized Approaches: Microbiome-based patient stratification through enterotyping may enable matching of specific therapeutic formulations to individual microbiome profiles. Research shows that donor-recipient compatibility influences engraftment success, suggesting that personalized donor selection or product formulation could optimize outcomes [23].
Expanded Indication Exploration: While rCDI remains the most validated indication, research continues for numerous other conditions. Promising areas include oncology support (particularly for immunotherapy augmentation), metabolic diseases, neurological conditions through the gut-brain axis, and autoimmune disorders [73] [71].
Technology-Enabled Monitoring: Advanced sequencing technologies and bioinformatic tools will allow more sophisticated therapeutic monitoring, including real-time assessment of engraftment dynamics, functional changes, and ecological stability. These approaches will support pharmacodynamic assessment and personalized treatment optimization [68] [23].
As the field matures, successful therapeutic development will require interdisciplinary collaboration spanning microbial ecology, pharmaceutical sciences, clinical medicine, and regulatory affairs. The continued harmonization of methodological approaches and regulatory standards will be essential for realizing the full potential of microbiome-based therapies across diverse medical applications.
Overcoming Analytical Challenges: Standardization, Contamination and Technical Variability
The field of microbiome research has expanded rapidly, yet the absence of accredited reference materials has been a significant barrier to reproducibility and clinical translation [75]. Effective standardization is essential for the entire microbiome community, as differences in methodologies—from DNA extraction and sequencing platforms to bioinformatics pipelines—introduce substantial variability, making cross-study comparisons challenging and potentially misleading [75]. Reference reagents and mock communities provide a known compositional ground truth, enabling researchers to identify, quantify, and correct for biases inherent in their analytical workflows. Their development and implementation are foundational to the consensus approach for validating microbiome analyses, a point underscored by a recent international expert panel which highlighted the current limited evidence for the routine clinical application of microbiome testing [7] [10]. This guide objectively compares available solutions and details the experimental protocols for their use in quality control, providing a critical resource for researchers, scientists, and drug development professionals.
The Landscape of Available Reference Reagents
Several reference reagents have been developed to address the need for standardization. The table below summarizes key products, their compositions, and their primary applications.
Table 1: Comparison of Key Reference Reagents and Mock Communities
| Reagent Name | Developer/Provider | Composition | Key Characteristics | Primary Application |
|---|---|---|---|---|
| Gut-Mix-RR & Gut-HiLo-RR [75] | National Institute for Biological Standards and Control (NIBSC) | 20 common gut microbiome strains across 5 phyla, 13 families, 16 genera, and 19 species [75]. | Two variants: even (Gut-Mix-RR) and staggered (Gut-HiLo-RR) abundance. Candidate WHO International Reference Reagents [75]. |
Standardizing downstream gut microbiome analyses (library prep, sequencing, and bioinformatics). |
| GA-map Dysbiosis Test [8] | Not specified in context | Not specified in context. | A commercially available test that provides a dysbiosis score [8]. | Used in research to assess microbial imbalance, though noted as not ready for clinical application [8]. |
| Commercially Available Mock Communities [75] | Various commercial entities | Varies by product. | Compositions and complexity differ from site-specific reagents like those from NIBSC [75]. | General pipeline benchmarking; may present less challenge than complex, site-specific reagents [75]. |
A Framework for Evaluating Analytical Performance
The development of reference reagents must be paired with a robust reporting framework to evaluate the performance of bioinformatics tools and pipelines quantitatively. One such framework, developed alongside the NIBSC reagents, uses four key measures to capture common biases in microbiome analysis [75]:
- Sensitivity (True Positive Rate): The percentage of known species in the reagent that are correctly identified by the pipeline. This measures the pipeline's ability to detect true signals.
- False Positive Relative Abundance (FPRA): The total relative abundance in the final dataset assigned to species not present in the reagent. This is crucial because a single high-abundance false positive can be more problematic than several low-abundance ones.
- Diversity (Observed Species): The total number of species reported by the pipeline. This measure indicates whether a method inflates or deflates critical alpha-diversity estimates.
- Similarity (Bray-Curtis): A measure of how well the predicted species composition reflects the actual composition of the reagent. It assesses the overall accuracy of the relative abundance profile.
This framework reveals that a trade-off often exists between sensitivity and FPRA, and that the composition of the mock community significantly impacts benchmarking results. Communities with high complexity and strains relevant to a specific body site, like the gut, present a more challenging and realistic benchmark [75].
Table 2: Experimental Results from Benchmarking Bioinformatics Tools with NIBSC RRs
| Bioinformatics Tool | Sequencing Method | Sensitivity (%) | False Positive Relative Abundance (FPRA) | Diversity (Reported vs. Actual Species) | Similarity (Bray-Curtis) |
|---|---|---|---|---|---|
| MetaPhlAn2 [75] | Shotgun | Variable | Variable | Often inflated | Variable |
| Kraken [75] | Shotgun / 16S | Variable | Variable | Often inflated | Variable |
| Bracken [75] | Shotgun / 16S | Variable | Variable | Often inflated | Variable |
| Kaiju [75] | Shotgun | Variable | Variable | Often inflated | Variable |
| Centrifuge [75] | Shotgun | Variable | Variable | Often inflated | Variable |
| 16S Pipelines [75] | 16S rRNA | Generally lower than shotgun tools | Often higher than shotgun tools | Often inflated | Variable |
Note: The specific values for "Variable" metrics are dependent on the tool, the reference reagent used (even vs. staggered), and the specific parameters of the experiment. The key finding is that all tested tools exhibited biases, and diversity estimates were "largely inflated by the majority of bioinformatics tools" [75].
Detailed Experimental Protocol for Quality Control Implementation
Implementing reference reagents for quality control requires a standardized experimental workflow. The following protocol details the steps for using DNA reference reagents, such as the NIBSC Gut-Mix-RR, to benchmark a microbiome analysis pipeline.
Objective: To quantify the systematic bias and error of a microbiome bioinformatics pipeline by comparing its output against the known composition of a DNA reference reagent.
Materials Required:
- DNA reference reagent (e.g., NIBSC Gut-Mix-RR or Gut-HiLo-RR).
- Library preparation kit compatible with your sequencing platform.
- Next-generation sequencer (e.g., Illumina, PacBio).
- High-performance computing cluster with bioinformatics pipelines installed.
Table 3: The Researcher's Toolkit for QC Experiments
| Item | Function |
|---|---|
| DNA Reference Reagents (e.g., NIBSC Gut-Mix-RR) [75] | Provides a ground truth of known microbial composition and abundance to benchmark the entire wet-lab and computational workflow. |
| Whole-Cell & Matrix-Spiked Reagents [75] | Controls for biases introduced during DNA extraction and the presence of sample matrix inhibitors; essential for comprehensive protocol validation. |
| STORMS Checklist [76] | A reporting guideline (Strengthening The Organization and Reporting of Microbiome Studies) to ensure complete and reproducible method description. |
| Laboratory Information Management System (LIMS) [77] | Tracks samples, manages associated metadata, enforces standardized procedures, and ensures data integrity and regulatory compliance (e.g., 21 CFR Part 11). |
| Bioinformatics Pipelines (e.g., MetaPhlAn2, Kraken) [75] | The tools under evaluation; they process raw sequencing data into taxonomic profiles. |
Step-by-Step Methodology
Experimental Design: Include a minimum of five replicates of the reference reagent to account for technical variation [75]. Sequence these replicates across multiple sequencing runs to identify and control for batch effects.
Library Preparation and Sequencing:
- Process the DNA from the reference reagents alongside your routine patient or research samples using the identical laboratory protocol.
- Prepare sequencing libraries according to the manufacturer's instructions. For shotgun metagenomics, sequence to a depth of at least 500,000 reads per replicate as a baseline for evaluation [75].
- For 16S rRNA sequencing, specify the hypervariable region being amplified (e.g., V4) and use consistent primer sets [76].
Bioinformatics Analysis:
- Process the raw sequencing data through the bioinformatics pipeline you are validating.
- Use the default or commonly recommended parameters for all tools to ensure a fair comparison [75].
- The output should be a taxonomic profile (preferably at the species level) with relative abundances.
Data Analysis and Performance Calculation:
- Calculate Sensitivity: For each replicate, determine the list of species identified by the pipeline. Sensitivity = (Number of correctly identified species / Total number of species in the reagent) * 100.
- Calculate FPRA: Sum the relative abundances of all species in the profile that are not part of the reagent's known composition.
- Calculate Diversity: Compare the total number of species reported by the pipeline (observed species) to the actual number of species in the reagent (20 for NIBSC RRs).
- Calculate Similarity: Compute the Bray-Curtis similarity index between the pipeline's relative abundance profile and the known profile of the reagent.
- Statistical Reporting: Report the mean and standard deviation for each of the four measures across all replicates.
Workflow Visualization
The following diagram illustrates the complete experimental and computational workflow for implementing reference reagents in quality control.
Consensus and Future Directions
The international scientific community is moving toward a consensus on the necessity of standardisation. The recent international consensus statement on microbiome testing strongly discourages direct-to-consumer testing without clinical recommendation due to limited evidence and the absence of a standardized framework [7]. The adoption of globally recognized reference reagents, such as the candidate WHO reagents from NIBSC, is a critical step toward building this evidence base [75]. Future efforts will focus on developing a wider suite of reagents, including whole-cell and matrix-spiked reagents, to control for biases introduced during DNA extraction and from sample matrix effects [75]. Widespread participation in collaborative benchmarking studies using these reagents is essential to establish acceptable levels of error and ultimately translate microbiome research into reliable clinical diagnostics and therapeutics [7] [75].
Accurate microbiome analysis is foundational to advancements in drug development and human health research. The validity of this analysis, however, is entirely dependent on the pre-analytical phases of sample collection, preservation, and nucleic acid extraction. Variations in these initial steps can introduce significant technical biases, such as batch effects, which confound biological signals and jeopardize the consensus validation of microbial profiles. This guide objectively compares current methods for biomass preservation and DNA extraction, drawing on recent experimental data to outline standardized protocols. Focusing on common sample types like dried blood spots (DBS) and subgingival biofilms, it provides a framework for researchers to select optimal techniques that ensure data integrity and reproducibility in microbiome studies.
Biomass Sampling, Storage and Preservation
The integrity of microbiome analysis begins with the proper handling of the source biomass. The chosen methods for sampling and preservation must stabilize the microbial community to prevent shifts in composition between collection and processing.
Sample Collection Techniques
The sampling methodology is tailored to the specific niche being studied.
- Dried Blood Spots (DBS): Capillary blood is collected via finger pricking onto specialized collection cards. A standard 6 mm punch from the card, containing approximately 8.7 µL of blood, is typically used for DNA extraction [78].
- Subgingival Biofilm: Sterile paper points are inserted into the periodontal pocket for 15 seconds to absorb biofilm, crevicular fluid, and bacterial content. For site-specific analysis, a single paper point per pocket is sufficient, which simplifies logistics and reduces patient discomfort [79].
- Environmental Surfaces: Surfaces are swabbed with pre-moistened sampling devices, such as cotton gauze or sponge sticks, to recover biomass. The collected material is then suspended in a buffer like PBS or DNA/RNA shield for stabilization [80].
Preservation and Storage
Immediate stabilization is critical to prevent degradation.
- DBS and Paper Points: After collection, samples are rapidly frozen in liquid nitrogen and transferred to long-term storage at -80 °C until DNA extraction [78] [79].
- Biomass for Biochemical Analysis: A study on microalgal biomass revealed that the optimal preservation method is compound-specific and species-specific. For instance, carbohydrates in Scenedesmus obliquus were best preserved by freezing, whereas proteins in the same species were best maintained by freeze-drying [81]. This underscores the need to align the preservation technique with the target analytes.
Table 1: Comparison of Biomass Sampling Methods
| Sample Type | Collection Method | Typical Sample Size | Recommended Storage | Key Considerations |
|---|---|---|---|---|
| Dried Blood Spot (DBS) | Capillary blood on collection card | 1 x 6 mm punch (≈8.7 µL blood) [78] | -80°C [78] | Minimally invasive; cost-efficient; standardized punch size is key. |
| Subgingival Biofilm | Sterile paper point | 1 paper point per pocket [79] | -80°C [79] | Single point allows for site-specific analysis; 15s sampling time. |
| Environmental Surface | Swab with gauze or sponge stick | N/A (surface dependent) | -80°C (after elution) [80] | Organic matter on surfaces can inhibit downstream PCR [80]. |
Comparative Analysis of DNA Extraction Methods
The DNA extraction process is a major source of variation in microbiome data. The following section compares the performance of different methodologies across various sample types.
DNA Extraction from Dried Blood Spots (DBS)
A 2025 systematic comparison of five DNA extraction methods on twenty DBS samples provided clear performance data [78].
- Chelex Boiling Method: This method yielded significantly higher (p < 0.0001) human DNA concentrations, as measured by qPCR for the ACTB gene, compared to all other methods tested. It was identified as an easy and cost-effective optimized protocol [78].
- Column-Based Kits (e.g., QIAamp, DNeasy): These methods generally showed low DNA recovery. An exception was the High Pure PCR Template Preparation Kit (Roche), which showed significantly higher DNA concentrations than other column-based kits when measured by spectrophotometry (DeNovix DS-11) [78].
- Optimization of Best Performers: Further optimization of the top two methods (Chelex and Roche) found that reducing the elution volume from 150 µL to 50 µL significantly increased the final DNA concentration. In contrast, increasing the starting material from one to two 6 mm punches did not yield a significant improvement [78].
Table 2: Performance Comparison of DNA Extraction Methods for DBS [78]
| Extraction Method | Type | Relative DNA Yield (ACTB qPCR) | Cost & Time | Key Application |
|---|---|---|---|---|
| Chelex Boiling | Boiling / Physical | Highest (p < 0.0001) | Low cost, rapid [78] | Ideal for large-scale screening, low-resource settings. |
| Roche High Pure Kit | Column-based / Chemical | Highest among column kits (spectrophotometry) | Higher cost, standardized [78] | Suitable when purity is a higher priority. |
| QIAamp DNA Mini Kit | Column-based / Chemical | Low | Higher cost, time-consuming [78] | -- |
| DNeasy Blood & Tissue | Column-based / Chemical | Low | Higher cost, time-consuming [78] | -- |
| TE Buffer Boiling | Boiling / Physical | Low | Low cost, rapid [78] | -- |
DNA Extraction from Subgingival Biofilm
A pilot study comparing three commercial DNA extraction kits for low-biomass samples from single paper points found clear performance differences [79].
- DNeasy Blood & Tissue Kit (QIAGEN): This kit demonstrated the highest efficiency, yielding significantly more total dsDNA from both healthy and periodontitis-affected sites compared to the other kits. Bacterial DNA yields were also significantly higher [79].
- NucleoSpin Tissue Mini (MACHEREY‑NAGEL) and ZymoBIOMICS DNA Miniprep (ZYMO RESEARCH): These kits showed lower DNA yields under the tested conditions, which involved very small sample volumes (<10 µL) [79].
Table 3: Performance Comparison of DNA Kits for Subgingival Biofilm (Single Paper Point) [79]
| DNA Extraction Kit | Cell Lysis Method | Relative Total dsDNA Yield | Relative Bacterial DNA Yield | Price per Extraction (€) |
|---|---|---|---|---|
| DNeasy Blood & Tissue (QIAGEN) | Enzymatic & Chemical [79] | Highest [79] | Highest [79] | 4.48 [79] |
| NucleoSpin Tissue Mini (MACHEREY‑NAGEL) | Enzymatic & Chemical [79] | Intermediate [79] | Intermediate [79] | 3.48 [79] |
| ZymoBIOMICS DNA Miniprep (ZYMO RESEARCH) | Mechanical & Chemical [79] | Lowest [79] | Lowest [79] | 6.51 [79] |
DNA Extraction from Feed and Environmental Samples
The optimal extraction method can also vary with complex sample matrices. A study on detecting African Swine Fever Virus (ASFV) in feed and environmental samples found that magnetic bead-based extraction methods performed superior to column-based (PowerSoil Pro) and point-of-care (M1) methods. The magnetic bead-based protocols produced significantly lower Cq values (p < 0.05) in qPCR, indicating higher sensitivity and better detection rates on feed mill surface samples [80].
Understanding and Mitigating Batch Effects
Batch effects are technical variations introduced when samples are processed in different groups or "batches," and they are a major confounder in large-scale microbiome studies.
A key source of batch effects in single-cell ATAC-seq workflows, relevant to microbiome genomics, is variability in the nuclei-to-Tn5 transposase ratio [82]. As Tn5 is a single-turnover enzyme, this ratio dictates the number of fragments generated per nucleus. Studies have demonstrated a significant correlation between transposition batch size and the number of fragments per cell, which in turn biases dimensionality reduction and clustering results [82]. Other common sources include different lots of reagents, personnel handling, and equipment calibration across processing dates.
Strategies for Batch Effect Mitigation
Proactive experimental design is the most effective way to manage batch effects.
- Sample Multiplexing: Technologies like MULTI-ATAC pool samples before the transposition reaction, eliminating batch effects caused by variable nuclei-to-Tn5 ratios. This ensures all samples are processed through the most variable steps of the protocol simultaneously [82].
- Randomization: Distributing samples from different experimental groups (e.g., case and control) across processing batches prevents the confounding of technical and biological variation.
- Statistical Correction: Post-sequencing, computational tools can be used to identify and adjust for residual batch effects, though this is a less reliable substitute for robust experimental design.
Diagram 1: Batch effects can be introduced at multiple stages of the workflow. Proactive mitigation strategies should be applied at corresponding steps.
Detailed Experimental Protocols
Optimized Chelex-100 DNA Extraction from DBS
This protocol is adapted from the 2025 study that identified this method as highly effective [78].
- Punch: Obtain one 6 mm punch from the DBS card and place it in a microcentrifuge tube.
- Soak: Incubate the punch overnight at 4°C in 1 mL of Tween20 solution (0.5% Tween20 in PBS).
- Wash: Remove the Tween20 solution and add 1 mL of PBS. Incubate for 30 minutes at 4°C, then remove the PBS.
- Chelex Incubation: Add 50 µL of a pre-heated 5% (m/v) Chelex-100 solution to the punch.
- Vortex and Boil: Pulse-vortex the mixture for 30 seconds. Incubate at 95°C for 15 minutes, with brief pulse-vortexing every 5 minutes during the incubation.
- Pellet and Recover: Centrifuge for 3 minutes at 11,000 rcf to pellet Chelex beads and paper debris.
- Transfer Supernatant: Carefully transfer the supernatant, which contains the DNA, to a new tube. The extract is ready for downstream applications like qPCR and should be stored at -20°C [78].
DNeasy Blood & Tissue Kit Protocol for Paper Points
This protocol for low-biomass subgingival biofilm samples uses a "casing" method for efficient elution [79].
- Wash Sample from Paper Point:
- Add 1 mL of nuclease-free water and 12 glass beads (1.7–2.1 mm) to the tube containing the paper point.
- Shake at 14,000 rpm for 5 minutes.
- Pierce the bottom of the tube and place it into a 5 mL collection tube.
- Centrifuge at 4,000 x g for 1 minute. Transfer the flow-through from the 5 mL tube to a new 1.5 mL tube.
- Pellet the material by centrifuging for 15 minutes at 10,000 x g. Discard the supernatant.
- Resuspend Pellet: Resuspend the pellet in 180 µL of enzymatic lysis buffer.
- Follow Manufacturer's Protocol: Continue with the kit's standard protocol for "Purification of Total DNA from Animal Tissues," including the recommended incubation steps with Proteinase K.
- Elute: Elute the DNA in 100 µL of Buffer AE [79].
Diagram 2: The optimized Chelex-100 extraction workflow for DBS samples is a rapid, cost-effective physical method [78].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents and Kits for Biomass Sampling, DNA Extraction, and Downstream Analysis
| Item Name | Function/Application | Key Characteristics |
|---|---|---|
| EUROIMMUN Blood Collection Cards | Collection and storage of dried blood spots (DBS) [78]. | Standardized filter paper for consistent blood volume absorption. |
| Sterile Paper Points (Size 50) | Minimally invasive collection of subgingival biofilm [79]. | Fine tip for accessing periodontal pockets; sterile to prevent contamination. |
| Chelex-100 Resin | Medium for rapid, cost-effective DNA extraction via boiling method [78]. | Chelating resin that binds metal ions, inhibiting nucleases. |
| DNeasy Blood & Tissue Kit (QIAGEN) | Column-based purification of DNA from tissues and low-biomass samples [79]. | Efficient for hard-to-lyse samples; provides high DNA yield from paper points. |
| Taco Mini / KingFisher Duo | Automated nucleic acid extraction systems using magnetic bead technology [80]. | High-throughput, consistent recovery of DNA with low cross-contamination risk. |
| AL Lysis Buffer (Qiagen) | Efficient breakdown of cells and viral particles for DNA release [80]. | Contains detergents and salts to lyse samples and prepare for binding. |
| Universal 16S rRNA Primers | qPCR quantification of total bacterial DNA load in a sample [79]. | Targets conserved regions of the bacterial 16S rRNA gene. |
In the evolving field of microbiome research, the translation of microbial signatures into clinically actionable insights faces significant computational challenges. The promise of microbiome-based diagnostics and therapeutics is contingent upon the rigorous validation of analytical methods, a process complicated by two fundamental sources of bias: pipeline-specific artifacts and database dependency issues. These computational biases can distort microbial community representations, impact reproducibility, and ultimately hinder the clinical application of microbiome science.
Recent international consensus statements have highlighted the critical need for standardized frameworks in microbiome testing, emphasizing that methodological variability remains a primary barrier to clinical translation [14] [7]. Without addressing these computational biases, the field risks generating irreproducible findings and unreliable diagnostic models. This review examines the sources and impacts of these biases within the context of microbiome analysis consensus approach validation research, providing researchers and drug development professionals with strategies to enhance analytical rigor.
The Impact of Analytical Pipelines on Microbiome Data
Microbiome analytical pipelines encompass the entire workflow from raw sequencing data to biological interpretation. At each stage, specific choices in data processing can introduce artifacts that systematically distort results and compromise data comparability across studies.
Pipeline-Specific Artifacts in 16S rRNA Sequencing
16S rRNA gene sequencing, while cost-effective for microbial community profiling, is particularly susceptible to pipeline-specific artifacts. The table below summarizes key processing steps and their associated biases:
Table 1: Major Sources of Pipeline-Specific Artifacts in 16S rRNA Analysis
| Processing Step | Source of Bias | Impact on Data | Consensus Recommendations |
|---|---|---|---|
| Sequence Quality Filtering | Variable quality scores, length thresholds | Loss of valid sequences; artificial abundance shifts | Standardize parameters; document thresholds [7] |
| Denoising & Clustering | Algorithm choice (DADA2, Deblur, UNOISE) | Differential resolution of ASVs/OTUs; split/merge errors | Use amplicon sequence variants (ASVs); report parameters [36] |
| Taxonomic Assignment | Reference database selection and version | Variable taxonomic resolution and accuracy | Use curated databases; document versions [7] [23] |
| Chimera Removal | Stringency of detection algorithms | False positives/negatives; abundance artifacts | Apply consensus approaches; report methods [36] |
The impact of these artifacts is not merely theoretical. A 2025 meta-analysis on colorectal cancer (CRC) microbiomes demonstrated that batch effects from different processing pipelines significantly influenced diversity metrics and taxonomic abundances [36]. After applying conditional quantile regression (ConQuR) to remove batch effects, the corrected data revealed more consistent microbial signatures, with Enterobacter and Fusobacterium enriched in CRC patients, while Bacteroides and Faecalibacterium were associated with healthy controls [36]. This demonstrates how pipeline-specific artifacts can obscure genuine biological signals until appropriate correction methods are applied.
Shotgun Metagenomic Sequencing Biases
While shotgun metagenomics provides higher taxonomic resolution and functional insights, it remains vulnerable to computational biases. Database dependency issues are particularly pronounced, as the majority of microbial sequences in environmental samples cannot be mapped to reference genomes from isolated organisms [23]. This "microbial dark matter" problem means that database selection directly determines which taxa can be identified and quantified.
Table 2: Database Dependency Issues in Shotgun Metagenomics
| Database Type | Key Limitations | Impact on Results | Emerging Solutions |
|---|---|---|---|
| Reference Genome Databases | Incomplete representation of strain diversity; population biases | Underestimation of novel taxa; population-specific biases | Expand with metagenome-assembled genomes (MAGs) [23] |
| Functional Databases | Incomplete annotation of microbial gene functions | Limited functional interpretation; pathway gaps | Integrated multi-omics; experimental validation [23] |
| Specialized Databases | Variable curation standards; update frequency | Inconsistent results across studies | Use of standardized resources (e.g., NIST stool reference) [23] |
A 2025 review of gut microbiome metagenomics in clinical practice emphasized that database choice significantly impacts diagnostic accuracy, particularly for pathogen detection and antimicrobial resistance gene profiling [23]. The lack of standardized databases has complicated the establishment of universally accepted diagnostic thresholds for dysbiosis, a challenge acknowledged in recent consensus guidelines [14] [7].
Experimental Evidence of Computational Biases
Case Study: Meta-Analysis of Colorectal Cancer Microbiomes
A comprehensive 2025 meta-analysis of 1,462 samples across 6 cohorts systematically quantified the impact of batch effects and analytical pipelines on CRC microbiome signatures [36]. The experimental protocol involved:
Data Collection: Raw 16S rRNA sequencing data from multiple studies was processed through QIIME2 and DADA2 to generate amplicon sequence variant (ASV) tables [36].
Batch Effect Correction: Conditional quantile regression (ConQuR) was applied to remove technical variability while preserving biological signals [36].
Diversity Analysis: α-diversity (Shannon, Simpson indices) and β-diversity (Bray-Curtis dissimilarity) were calculated before and after correction [36].
Differential Abundance: Linear discriminant analysis Effect Size (LEfSe) identified microbial biomarkers associated with CRC status [36].
The results demonstrated that batch effect correction significantly enhanced the statistical power to detect CRC-associated taxa. Before correction, effect sizes were attenuated and consistency across studies was lower. After implementing ConQuR, the analysis revealed robust associations between CRC and specific microbial genera that were consistent across diverse cohorts [36].
Multi-Omics Integration Studies
Advanced multi-omics approaches have further highlighted the limitations of single-method microbiome analyses. A large-scale integration of over 1,300 metagenomes and 400 metabolomes from inflammatory bowel disease (IBD) patients identified consistent alterations in underreported microbial species (Asaccharobacter celatus, Gemmiger formicilis, Erysipelatoclostridium ramosum) alongside significant metabolite shifts [23]. Diagnostic models built on these integrated signatures achieved exceptional accuracy (AUROC 0.92-0.98), outperforming models based on taxonomic data alone [23]. This demonstrates how multi-omics approaches can mitigate pipeline-specific biases by providing orthogonal validation of microbial signatures.
Diagram 1: Sources of computational biases in microbiome analysis pipelines. Red arrows indicate points where biases are introduced or propagated.
Consensus Approaches for Bias Mitigation
Recent international consensus statements have established frameworks to address computational biases in microbiome analysis. A Delphi process involving 69 experts from 18 countries yielded specific recommendations for standardizing microbiome testing in clinical practice [14] [12] [7].
Standardized Reporting and Methodology
The consensus emphasizes that laboratories providing microbiome testing should adhere to high-quality standards and transparently communicate methodological details [7]. Key recommendations include:
Method Selection: Appropriate microbiome profiling should use either amplicon sequencing (e.g., 16S rRNA) or whole-genome sequencing, while conventional microbial cultures or PCR should not be used as proxies for comprehensive microbiome analysis [7].
Reporting Standards: Test reports should include complete protocol details, including stool collection methods, DNA extraction procedures, sequencing parameters, and post-sequencing analyses [7]. Clinical metadata must be incorporated to provide context for interpretation.
Analytical Transparency: The consensus specifically advises against reporting oversimplified metrics such as the Firmicutes/Bacteroidetes ratio due to insufficient evidence linking these ratios to health outcomes [12] [7]. Instead, comprehensive taxonomic profiling with deep resolution is recommended.
Validation Frameworks for Clinical Translation
For microbiome analysis to achieve clinical utility, consensus approaches emphasize the need for rigorous validation:
Diagram 2: Consensus validation framework for robust microbiome analysis. This multi-step approach addresses computational biases through standardization and orthogonal validation.
Multi-Center Studies: The consensus recommends that microbiome tests should participate in research protocols under strict investigative conditions to generate evidence for this emerging field [7]. This includes cross-validation across multiple cohorts with different demographic characteristics.
Integrated Multi-Omics: Combining metagenomics with metabolomics and other molecular profiling provides orthogonal validation of microbial signatures [23]. For example, the correlation between microbial taxa and metabolite shifts strengthens causal inference in disease mechanisms.
Mechanistic Validation: Advanced computational approaches should be paired with experimental models to establish causal relationships rather than mere associations [23]. This is particularly important for moving from diagnostic signatures to therapeutic targets.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Computational Tools for Mitigating Microbiome Analysis Biases
| Tool Category | Specific Solutions | Function/Purpose | Bias Addressed |
|---|---|---|---|
| Wet Lab Standards | NIST Stool Reference Material | Inter-laboratory standardization; protocol calibration | Pipeline-specific artifacts [23] |
| Computational Tools | ConQuR; MMUPHin; PLSDA-batch | Batch effect correction; data harmonization | Technical variability [36] |
| Reference Databases | Curated genome databases; HMP references | Comprehensive taxonomic profiling | Database dependencies [23] |
| Multi-Omics Platforms | Integrated correlation networks | Connect microbial features to functional outcomes | Biological interpretation [23] |
| Quality Control Metrics | STORMS checklist | Standardized reporting; reproducibility | Overall methodological bias [23] |
Computational biases represent a fundamental challenge in microbiome research, with pipeline-specific artifacts and database dependencies significantly impacting the reproducibility and clinical translation of microbial signatures. International consensus initiatives have established critical frameworks for standardizing analytical approaches, yet substantial work remains to fully harmonize methodologies across the field.
The path forward requires continued development of standardized computational protocols, expansion of reference databases to capture global microbial diversity, and implementation of multi-omics validation strategies. By addressing these computational biases through consensus approaches, researchers and drug development professionals can enhance the reliability of microbiome-based diagnostics and therapeutics, ultimately fulfilling the promise of precision medicine guided by microbial ecosystems.
The standardization of microbiome analysis represents a critical challenge in translational research. The introduction of the Four-Measure Validation Framework—comprising Sensitivity, False Positive Relative Abundance (FPRA), Diversity, and Similarity—provides a robust, standardized method for benchmarking microbiome testing pipelines. This framework, developed alongside well-characterized reference reagents, enables researchers to objectively evaluate biases introduced during DNA extraction, sequencing, and bioinformatic analysis. By applying this consensus approach, the field can improve the reproducibility and reliability of microbiome studies, thereby accelerating the development of microbiome-based diagnostics and therapeutics. This guide objectively compares the performance of various experimental protocols and bioinformatics tools validated using this framework, providing critical data for researchers and drug development professionals.
Microbiome research has profoundly influenced our understanding of human health and disease, with the gut microbiota acting as a key mediator of metabolism, immune regulation, and response to drugs [7]. However, the translation of microbiome research into clinical practice remains limited due to challenges in standardization, the complexity of sequencing datasets, and difficulties in distinguishing correlation from causation [7] [25].
A significant advancement in addressing these challenges came with the development of a structured reporting framework to evaluate the accuracy of microbiome analytical pipelines. This framework utilizes four key metrics to assess how well a pipeline reconstructs known microbial community composition [75] [83]:
- Sensitivity: The proportion of known species in a reference reagent correctly identified by the pipeline.
- False Positive Relative Abundance (FPRA): The total relative abundance in the final dataset attributed to species not actually present in the reference reagent.
- Diversity: The accuracy in reporting the observed number of species present, critical for alpha-diversity estimates.
- Similarity: How well the predicted species composition reflects the actual composition, typically measured using the Bray-Curtis similarity index.
This framework, used in conjunction with physical reference reagents, allows for the precise identification of where biases occur in a microbiome analysis workflow, from DNA extraction to bioinformatic classification [84] [83].
Experimental Protocols for Framework Application
Reference Reagent Preparation
The validation framework depends on using mock microbial communities of known composition ("ground truth"). Two primary types of reference reagents are essential for a complete pipeline evaluation:
Whole Cell Reference Reagents (WC-Gut RR): Used to evaluate DNA extraction protocols. The WHO international whole cell reference reagent (NIBSC 22/210) contains 20 fixed bacterial strains common to the gut microbiome in equal abundance. These strains span 5 phyla and 19 species, including anaerobic and hard-to-lyse bacteria, providing a challenging and realistic standard for gut microbiome research [84] [83].
- Protocol: Lyophilized WC-Gut RR is reconstituted in 600µL of Phosphate Buffered Saline (PBS) as per manufacturer instructions. The fixed cells are then subjected to the DNA extraction method being evaluated [85].
DNA Reference Reagents (DNA-Gut-Mix RR): Used to control for biases in library preparation, sequencing, and bioinformatics. The WHO DNA-Gut reference reagent (NIBSC 20/302) contains genomic DNA from the same 20 strains, in both even (Gut-Mix-RR) and staggered (Gut-HiLo-RR) abundance profiles [75] [85].
DNA Extraction and Sequencing
The performance of DNA extraction kits varies significantly, impacting downstream results. A standardized protocol for evaluation is as follows:
- DNA Extraction: A volume of 200µL of the reconstituted WC-Gut RR is used as input. The extraction should include a bead-beating step to ensure lysis of tough cell walls, which is critical for gram-positive bacteria [15] [83]. Multiple commercial kits can be compared simultaneously.
- Library Preparation and Sequencing:
- For 16S rRNA gene sequencing, the full-length ~1500 bp gene is amplified using universal primers (e.g., 27F and 1492R) and sequenced on a platform like Oxford Nanopore Technology (ONT) for long-read capability [85].
- For shotgun metagenomic sequencing, libraries are prepared using kits such as the Nextera DNA Flex Library Prep Kit and sequenced on platforms like Illumina NextSeq to generate high-throughput short reads [83]. Sequencing depth should be standardized, for example, by subsampling to 500,000 reads per replicate for comparative analysis [75].
Bioinformatics Analysis
Sequencing data is processed through various taxonomic profiling tools. Commands should be run following developer-recommended settings for a fair comparison. Commonly assessed tools include:
- Marker-based: MetaPhlAn2, MetaPhlAn3, MetaPhlAn4 [75] [86].
- k-mer-based: Kraken2, Bracken [75] [86].
- Alignment-based: Kaiju, Centrifuge [75].
- Other Pipelines: JAMS, WGSA2, Woltka [86].
The output of these tools—a taxonomic profile—is then compared against the known composition of the reference reagent to calculate the four key metrics.
Workflow Visualization
The following diagram illustrates the complete experimental workflow for applying the four-measure validation framework:
Comparative Performance of Bioinformatics Pipelines
Benchmarking Shotgun Metagenomic Tools
Independent evaluation using the NIBSC Gut-Mix-RR and the four-measure framework demonstrates significant variability in the performance of taxonomic profilers. The table below summarizes the performance characteristics of several common bioinformatics tools when analyzing shotgun metagenomic data from the defined reference reagent [75].
Table 1: Performance of Bioinformatics Tools on Shotgun Metagenomic Data
| Bioinformatics Tool | Analysis Method | Sensitivity | False Positive Relative Abundance (FPRA) | Reported Diversity | Similarity (Bray-Curtis) | Key Trade-off Identified |
|---|---|---|---|---|---|---|
| MetaPhlAn2 | Marker-based | Moderate | Low | Moderate | Moderate | Balanced sensitivity/FPRA |
| Kraken2/Bracken | k-mer-based | High | High | Inflated | Low | High sensitivity at cost of high FPRA |
| Kaiju | Alignment-based | Low | Lowest | Underestimated | Low | Low FPRA but misses true positives |
| Centrifuge | Alignment-based | Moderate | Low | Moderate | Moderate | Balanced performance |
A more recent, unbiased benchmarking study using 19 publicly available mock communities and a constructed pathogenic gut microbiome sample evaluated four modern pipelines. Performance was assessed using Aitchison distance (a compositionally-aware metric), sensitivity, and total FPRA [86].
Table 2: Contemporary Pipeline Benchmarking on Multiple Mock Communities
| Pipeline | Core Classification Method | Sensitivity | Total FPRA | Overall Accuracy (Aitchison Distance) | Notes |
|---|---|---|---|---|---|
| bioBakery4 | Marker-based & MAG-based | High | Low | Best | Commonly used, requires basic command line knowledge [86]. |
| JAMS | Kraken2-based with assembly | Highest | Moderate | Good | Uses assembly; high sensitivity but complex [86]. |
| WGSA2 | Kraken2-based (assembly optional) | Highest | High | Moderate | Similar sensitivity to JAMS; FPRA can be high [86]. |
| Woltka | Operational Genomic Unit (OGU) | Moderate | Low | Good | Newer phylogeny-based approach [86]. |
A consistent finding across studies is the inverse relationship between sensitivity and FPRA. Tools like Kraken2 and JAMS, which achieve high sensitivity by detecting a large number of species, often do so at the cost of introducing a higher proportion of false positives into the final dataset. In contrast, tools with more stringent classification, such as earlier versions of MetaPhlAn, may have lower FPRA but can miss true low-abundance species [75] [86].
Impact of DNA Extraction Kits
The four-measure framework, when applied to the WC-Gut RR, effectively reveals performance differences between DNA extraction kits. The framework uses both physicochemical DNA measurements (yield, integrity, purity) and the four metrics derived from sequencing to provide a comprehensive kit assessment [83].
Table 3: DNA Extraction Kit Evaluation Using WC-Gut RR and Four-Measure Framework
| DNA Extraction Kit | Physicochemical DNA Yield | Sensitivity | FPRA | Key Bias Identified |
|---|---|---|---|---|
| Kit A | High | High | Low | Effective lysis of Gram-positive bacteria |
| Kit B | Moderate | Moderate | High | Incomplete lysis, higher reagent contamination |
| Kit C | Low | Low | Low | Poor lysis across multiple species |
| Kit D | Highest | High | Moderate | High yield but may co-extract inhibitors |
The combination of the WC-Gut RR and the DNA-Gut-Mix RR allows researchers to attribute biases to specific steps in the pipeline. If a bias is observed with the whole cell reagent but not the DNA reagent, the issue likely lies with the DNA extraction protocol. If the bias is present with both reagents, the problem likely originates from the sequencing or bioinformatic steps [83].
Essential Research Reagent Solutions
The successful implementation of the four-measure validation framework relies on the use of characterized reference materials. The following table details key reagents that have been developed and are critical for standardizing microbiome studies [84] [75] [85].
Table 4: Essential Reference Reagents for Microbiome Pipeline Validation
| Reagent Name | Type | Composition | Primary Function in Validation | Source |
|---|---|---|---|---|
| WC-Gut RR (NIBSC 22/210) | Whole Cell | 20 fixed gut bacterial strains in equal abundance | Evaluate DNA extraction efficiency and bias, including lysis efficiency of tough cells. | MHRA (UK) / WHO |
| DNA-Gut-Mix-RR (NIBSC 20/302) | Genomic DNA | DNA from 20 gut strains in even/staggered mixes | Standardize and evaluate library prep, sequencing, and bioinformatic analysis steps. | NIBSC (UK) / WHO |
| MCM2α & MCM2β | Genomic DNA | 14 clinically relevant bacterial species in variable concentrations | Assess PCR and sequencing efficiency and accuracy in clinical sample contexts. | National Measurement Laboratory (NML, UK) |
The Four-Measure Validation Framework, comprising Sensitivity, FPRA, Diversity, and Similarity, provides a much-needed standardized approach for benchmarking microbiome analysis pipelines. The experimental data and comparisons presented in this guide demonstrate that significant biases are introduced at every stage of microbiome analysis, from DNA extraction to bioinformatic classification. The consistent trade-off observed between sensitivity and false positive relative abundance underscores that there is no single "best" pipeline for all scenarios; rather, researchers must select tools based on the specific requirements of their study.
The widespread adoption of this framework, along with the use of complex, habitat-specific reference reagents, is essential to improve reproducibility, enable reliable comparison across studies, and build the rigorous evidence base required for the eventual clinical translation of microbiome-based diagnostics and therapeutics. Future work will focus on establishing minimum quality thresholds for these metrics through large, interlaboratory collaborative studies.
The global pharmaceutical landscape is in a state of dynamic transformation, shaped by the dual forces of groundbreaking technological innovation and the persistent challenge of high attrition rates in drug development. For researchers and drug development professionals, understanding the differential success rates across emerging therapeutic modalities is not merely an academic exercise but a critical strategic necessity. The clinical trial success rate (ClinSR) serves as a key barometer of developmental efficiency, reflecting the complex interplay between biological insight, technological capability, and regulatory adaptation [87].
This analysis examines the current therapeutic development landscape through a multidimensional lens, comparing success probabilities across conventional and emerging modalities while placing these metrics within the context of a broader scientific movement toward standardization and validation—exemplified by recent international consensus efforts in microbiome research. As the industry navigates the transition from traditional small molecules and biologics to advanced therapies including cell and gene therapies, RNA-based therapeutics, and targeted protein degraders, a sophisticated understanding of developmental bottlenecks becomes increasingly essential for directing resources, mitigating risk, and ultimately delivering transformative treatments to patients [88] [89].
Quantitative Landscape: Clinical Trial Success Rates Across Modalities
Tracking the success rate of clinical drug development is fundamental for pharmaceutical and economic decision-making [87]. Recent analyses of over 20,000 clinical development programs reveal significant variations in success probabilities across different drug modalities, reflecting their distinct technological maturity and biological complexity.
Table 1: Clinical Trial Success Rate (ClinSR) Variations by Drug Modality (2001-2023)
| Drug Modality | Relative Success Rate Trend | Key Influencing Factors | Therapeutic Area Strengths |
|---|---|---|---|
| Monoclonal Antibodies (mAbs) | Strong, stable growth [90] | High target specificity, established manufacturing | Oncology, immunology, expanding to neurology and CV [90] |
| Antibody-Drug Conjugates (ADCs) | Rapid growth (40% value increase past year) [90] | Improved linker technology, targeted cytotoxicity | Oncology (e.g., breast cancer) [90] |
| Cell Therapies (CAR-T) | Rapid evolution, mixed results [90] | Logistical complexity, high manufacturing costs [90] | Hematological malignancies [90] |
| Gene Therapies | Stagnating growth [90] | Safety issues, regulatory scrutiny, commercialization challenges [90] | Rare monogenic disorders [90] |
| RNA Therapeutics | Rapid growth post-COVID-19 [90] | Versatile platform, validated by pandemic | Infectious disease, rare diseases [90] |
| Protein Degraders (PROTACs) | Emerging pipeline | Novel mechanism for "undruggable" targets [88] | Oncology, neurodegenerative diseases [88] |
A comprehensive dynamic analysis of clinical development programs from 2001 to 2023 indicates that the overall ClinSR had been declining since the early 21st century but has recently plateaued and begun to show signs of increase [87]. This trend reversal coincides with the maturation of several emerging modality classes. The analysis reveals "great variations among the ClinSRs of various diseases, developmental strategies, and drug modalities," underscoring the need for modality-specific development strategies [87].
Monoclonal antibodies continue to demonstrate remarkable resilience as a platform, maintaining "strong, stable growth" despite being one of the older categories of new modalities [90]. This robustness stems from continued expansion into new therapeutic areas beyond oncology and immunology, including neurology, rare diseases, gastroenterology, and cardiovascular diseases [90]. In contrast, more complex modalities like cell and gene therapies face steeper paths to commercialization due to multifaceted challenges spanning technical, manufacturing, and regulatory domains [90].
Methodological Framework: Analyzing Development Pipelines
Data Collection and Standardization Protocols
The quantitative assessment of therapeutic development bottlenecks requires rigorous methodology. The analysis presented herein is based on a "rigorous and reproducible procedure for data collection and ClinSR evaluation" developed from examination of 20,398 clinical development programs involving 9,682 molecular entities [87]. This approach utilizes multiple transparent, accessible, and up-to-date public databases, including ClinicalTrials.gov for clinical trial data and Drugs@FDA for approved drug information, ensuring comprehensive coverage [87].
Data standardization followed a systematic protocol to enable valid cross-modal comparisons. Each development program was categorized by modality, therapeutic area, and development stage. Success rates were calculated using a dynamic strategy that enables "continuous evaluations of and effective comparisons among annual ClinSRs," overcoming limitations of previous static analyses that could not adequately reflect the rapidly evolving landscape of emerging modalities [87].
Bottleneck Analysis Framework
The experimental framework for identifying development bottlenecks incorporates multiple analytical dimensions:
- Phase Transition Analysis: Tracking likelihood of progression from Phase I to Phase II, Phase II to Phase III, and Phase III to approval for each modality class.
- Attribution Factor Mapping: Categorizing failure causes into safety, efficacy, commercial, and regulatory factors for each modality.
- Temporal Trend Assessment: Monitoring how success probabilities evolve with technological maturity and regulatory experience.
This methodological framework enables researchers to identify not just which modalities face challenges, but at what specific developmental stages these bottlenecks occur, and how these patterns change over time.
Figure 1: Generalized Therapeutic Development Workflow. The process from preclinical research to approval involves critical transitions where modalities face distinct challenges.
The Microbiome Consensus: A Paradigm for Standardization
Consensus Methodology as a Model for Field Advancement
The recent International Consensus Statement on Microbiome Testing in Clinical Practice provides a powerful paradigm for addressing standardization challenges that parallel those faced by developers of emerging therapeutic modalities [7]. Developed through a structured Delphi process involving 69 multidisciplinary experts from 18 countries, this consensus achieved an 80% agreement threshold for all recommendations, establishing a robust framework for translating complex biological data into clinically actionable standards [7] [12].
The consensus-building methodology offers a template that could benefit standardization efforts across emerging therapeutic modalities. The expert panel addressed five critical domains: (1) general principles and minimum requirements, (2) pre-testing procedures, (3) microbiome analysis methodologies, (4) reporting standards, and (5) clinical relevance assessment [7]. This systematic approach to establishing field-wide standards directly addresses the "methodological variability, incomplete understanding of which microbiome players are involved in health and disease, and the enormous inter-individual variability" that hinders clinical translation [14].
Analytical Standardization Protocols
The microbiome consensus establishes precise technical standards that could inform analogous efforts for characterizing emerging therapeutics:
- Sequencing Protocols: Recommending appropriate modalities for gut microbiome community profiling including amplicon sequencing (16S rRNA) and whole genome sequencing, while specifying that multiplex PCR and bacterial cultures cannot be considered comprehensive microbiome testing [7].
- Metadata Collection: Mandating comprehensive clinical metadata including patient age, gender, body mass index, gut transit time, current and past medications, and medical conditions to control for confounding variables [7] [23].
- Sample Handling Procedures: Standardizing stool collection kits with genome preservative, testing within recommended time frames, and storage of fecal samples at -80°C in the laboratory [7].
These standardized protocols enhance reproducibility and comparability across studies—a challenge equally relevant to the development of cell and gene therapies, where manufacturing and analytical variations significantly impact clinical outcomes [89].
Modality-Specific Bottlenecks and Consensus-Driven Solutions
Cell and Gene Therapy Challenges
Cell and gene therapies represent perhaps the most technologically advanced therapeutic modalities, yet they face significant developmental headwinds. The CAR-T pipeline "continues to grow rapidly" while "other emerging cell therapies have encountered challenges including clinical delays and failures, high manufacturing costs, and limited adoption" [90]. The gene therapy space has experienced "stagnating growth amid safety issues" with recent incidents leading to halted trials and regulatory scrutiny [90].
The consensus approach offers a framework for addressing these challenges through standardized characterization protocols similar to those established for microbiome testing. For example, the microbiome consensus recommendation that "providers of microbiome testing should communicate a reasonable, reliable, transparent, and scientific representation of the test" [7] has direct parallels for gene therapy developers needing to clearly communicate both potential benefits and limitations to regulators and patients.
RNA Therapeutics and Manufacturing Standardization
RNA therapeutics have demonstrated remarkable growth, with projected revenues up 65% year-over-year driven primarily by recently approved antisense oligonucleotides [90]. However, delivery barriers—especially to non-liver tissues—remain significant, and manufacturing complexities present substantial hurdles [88].
The microbiome consensus principle that "reports must include detailed clinical metadata" [12] to enable proper interpretation of results suggests a similar need for comprehensive characterization of RNA delivery systems and manufacturing processes. The establishment of standardized metrics for lipid nanoparticle characterization, potency assays, and purity assessments would address critical bottlenecks in RNA therapeutic development.
Table 2: Research Reagent Solutions for Therapeutic Development
| Research Reagent | Function in Development | Application Examples |
|---|---|---|
| Adeno-Associated Virus (AAV) Vectors | Gene delivery vehicle [88] | Gene therapy for inherited disorders [88] |
| Lipid Nanoparticles (LNPs) | Nucleic acid encapsulation and delivery [88] | mRNA vaccines, RNA therapeutics [88] |
| Bispecific Antibodies | Simultaneous targeting of two antigens [90] | Oncology, immune engagement [90] |
| PROTAC Molecules | Targeted protein degradation [88] | "Undruggable" target elimination [88] |
| 16S rRNA Gene Primers | Microbiome taxonomic profiling [7] | Microbial community analysis [7] |
| Shotgun Metagenomics Kits | Comprehensive genomic analysis [7] | Functional potential assessment [7] |
Analytical Workflows for Modality Characterization
The complexity of emerging therapeutic modalities demands sophisticated analytical approaches. The microbiome field has developed rigorous workflows that offer models for therapeutic characterization.
Figure 2: Standardized Microbiome Analysis Workflow. This consensus-based approach emphasizes controlled procedures and metadata integration, offering a model for characterizing complex therapeutics.
Standardized Experimental Protocols
For microbiome analysis, international consensus recommends specific procedural standards that could inform therapeutic characterization:
- Sample Collection: Use of stool collection kits with genome preservative and adherence to strict timeframes between collection and processing [7].
- DNA Extraction: Protocols including bead-beating steps to ensure accurate representation of diverse microbial communities [15].
- Sequencing Approaches: Selection of appropriate methodologies (16S rRNA amplicon sequencing or whole genome sequencing) based on research questions [7].
- Quality Controls: Inclusion of negative controls and mock communities throughout the extraction and sequencing process to detect contamination and technical biases [15].
These standardized protocols enhance reproducibility—a critical challenge for emerging modalities where manufacturing consistency directly impacts therapeutic efficacy and safety [89].
Data Analysis and Interpretation Standards
The microbiome consensus establishes rigorous standards for data analysis and interpretation that could benefit therapeutic development:
- Taxonomic Reporting: Recommendation to report with the "deepest possible taxonomic resolution" while excluding particular dysbiosis indices (e.g., Firmicutes/Bacteroidetes ratio) that do not capture meaningful variation [7].
- Diversity Metrics: Incorporation of ecological measures (alpha and beta diversity) with comparison to matched control groups [7].
- Functional Interpretation: Emphasis on mechanistic insights rather than correlative associations, acknowledging that "the direct application of microbiome tests to diagnose or manage health conditions is hindered by the unknowns in the microbiome" [14].
This cautious, evidence-based approach to data interpretation offers a model for evaluating emerging therapeutics, where early enthusiasm must be balanced with rigorous assessment of mechanistic evidence and clinical validity.
The analysis of therapeutic development bottlenecks reveals a complex landscape characterized by significant variation in success probabilities across drug modalities. While established modalities like monoclonal antibodies continue to demonstrate robust growth, emerging therapies including cell and gene treatments face substantial challenges in manufacturing, characterization, and clinical validation [90].
The international consensus approach to microbiome testing standardization provides a valuable model for addressing similar bottlenecks in therapeutic development. By establishing rigorous methodological standards, quality control procedures, and transparent reporting frameworks, the microbiome field has created a foundation for accelerated translation of basic research into clinical applications [7] [15].
For researchers and drug development professionals, embracing this consensus-driven mindset offers a pathway to overcoming critical bottlenecks in emerging therapeutic modalities. The integration of standardized analytical protocols, comprehensive metadata collection, and evidence-based interpretation frameworks can enhance reproducibility, facilitate regulatory evaluation, and ultimately improve the probability of technical and clinical success across all therapeutic modalities.
As the pharmaceutical landscape continues to evolve toward increasingly complex and personalized therapies, the principles embodied in the microbiome consensus—scientific rigor, methodological transparency, and multidisciplinary collaboration—will be essential for realizing the full potential of these groundbreaking treatments to address unmet medical needs and improve patient outcomes worldwide.
Benchmarking and Clinical Validation: Establishing Causality and Reproducibility
The expansion of bioinformatics software, particularly for microbiome analysis, presents a critical challenge for researchers and drug development professionals: selecting the optimal tool for a given scientific question. The discipline relies on computer technology and mathematical modeling to process biological data and solve biological science problems, generating vast amounts of information designed to quantify collections of biomolecules [91]. With the existence of numerous analysis platforms, each with detailed functional descriptions, the selection of software capable of presenting results relevant to one's research area and revealing the direction of subsequent investigations is a common concern [91]. Establishing a consensus approach for validating tool performance through standardized benchmarking is therefore paramount, especially as the field grapples with establishing causality between microbiome dynamics and host physiology [25]. This guide provides an objective comparison of bioinformatics tools based on experimental benchmark data, detailing methodologies and providing structured recommendations for pipeline evaluation.
The Critical Need for Standardized Benchmarking in Bioinformatics
Bioinformatics tool selection carries significant consequences for research outcomes, yet current selection processes often prioritize popularity over performance. A comprehensive analysis of Gene Set Analysis (GSA) tools revealed a striking discrepancy: the most popular methods were not necessarily the best performers when objectively evaluated [92]. This misalignment risks the functional interpretation of biological datasets in countless biomedical studies.
The root of this problem often lies in inadequate validation practices. An examination of 153 GSA tool publications found that only 61 included any validation procedure, with the most common strategy being "consistency with biological knowledge" – a subjective measure that simply confirms existing understanding rather than rigorously testing performance [92]. More reliable strategies, such as experimental confirmation of predictions and benchmark studies with simulated data, were among the least employed approaches [92]. This highlights a critical gap between software development and rigorous validation.
Beyond academic concerns, improper benchmarking has tangible consequences for research reproducibility and therapeutic development. In microbiome studies, biases can be introduced at every step: sample collection, DNA extraction, library construction, sequencing, bioinformatics, and data visualization [15]. The recent controversy surrounding the purported placental microbiome, initially reported but later attributed to contamination and misinterpretation, exemplifies how methodological flaws can misdirect scientific discourse [15]. Such issues underscore why benchmarking must extend beyond software algorithms to encompass entire experimental workflows.
Table 1: Common Benchmarking Pitfalls and Solutions
| Pitfall | Consequence | Solution |
|---|---|---|
| Using default parameters without justification | Suboptimal performance for specific data types | Document and justify all parameters [93] |
| Testing in inconsistent computational environments | Performance variations due to hidden variables | Fix software versions and use identical hardware [93] |
| Relying on subjective validation methods | Unreliable performance assessments | Use reference truth sets and quantitative metrics [92] [93] |
| Neglecting experimental controls | Inability to distinguish technical artifacts from biological signals | Include negative controls and mock communities [15] |
| Focusing solely on popularity metrics | Selection of suboptimal tools for specific applications | Consult independent benchmark studies [92] |
Experimental Design for Benchmarking Bioinformatics Pipelines
Reference Standards and Ground Truth Datasets
Robust benchmarking requires well-characterized reference materials with known answers against which tool performance can be measured. The Genome in a Bottle (GIAB) consortium provides human reference materials specifically designed for calibration and development of genome assembly methods [94]. For example, the HG002 sample (NA24385) is frequently used as a reference in benchmark studies due to its comprehensive characterization [94].
In microbiome research, mock communities – known mixtures of microorganisms or their DNA – serve as essential controls for assessing potential biases in taxonomic analyses [15]. These should reflect the diversity and taxonomic composition of the microbial communities under investigation. Both biological mock communities (containing naturally occurring sequences) and non-biological mocks (with lab-made variable regions not found in nature) help evaluate cross-sample contamination and parameterize bioinformatics pipelines [15]. Data from these controls should be released alongside sample data, with results compared to theoretical composition to quantify methodological accuracy.
Performance Metrics and Evaluation Criteria
Comprehensive benchmarking requires multiple, complementary performance metrics that collectively capture different dimensions of tool effectiveness. These metrics can be categorized as follows:
Accuracy Metrics: Sensitivity (true positive rate), precision (positive predictive value), F1-score (harmonic mean of precision and sensitivity), and overall concordance with known truth sets [94] [93]. For genome assembly, continuity and completeness metrics from tools like QUAST and BUSCO provide standardized assessments [94].
Computational Efficiency: Runtime, peak RAM usage, and scalability across sample sizes [93]. These practical considerations determine feasibility for different laboratory settings.
Reproducibility: Version stability, deterministic output, and consistency across repeated runs [93]. This ensures that results remain constant when analyses are repeated.
Usability: Configuration complexity, installation success rate, and documentation quality [93]. These factors influence adoption in diverse research environments.
Standardized Experimental Protocol
The following protocol provides a framework for benchmarking bioinformatics tools:
1. Experimental Setup
- Define clear research questions and performance metrics before initiating comparisons [93]
- Select appropriate reference datasets (e.g., GIAB for human genomics, mock communities for microbiome studies) [94] [15]
- Establish a fixed computational environment with containerized tools (Docker/Singularity) to ensure consistency [93] [95]
2. Data Processing
- Process raw data through each pipeline using both default and optimized parameters
- For microbiome studies, include negative controls and mock communities throughout wet-lab procedures [15]
- Convert all outputs to standardized formats (BAM, VCF, feature tables) for fair comparison [93]
3. Performance Assessment
- Compare results against ground truth using predefined metrics
- Evaluate statistical significance of performance differences
- Assess robustness through cross-validation or bootstrap resampling
4. Documentation and Reporting
- Share all code, parameters, and environment specifications
- Publish full results regardless of outcome to avoid publication bias [93]
- Visualize results honestly without manipulating axes to exaggerate differences [93]
Figure 1: Benchmarking Workflow. This diagram illustrates the standardized experimental protocol for benchmarking bioinformatics tools, from initial setup through documentation.
Comparative Analysis of Bioinformatics Tools
Genome Assembly Tools
A comprehensive benchmark of 11 genome assembly pipelines, including four long-read only assemblers and three hybrid assemblers combined with four polishing schemes, revealed significant performance differences [94]. Researchers used HG002 human reference material sequenced with Oxford Nanopore Technologies (47X coverage) and Illumina (35X coverage), assessing results with QUAST, BUSCO, and Merqury metrics alongside computational cost analyses [94].
Table 2: Performance Comparison of Genome Assembly Tools
| Assembly Tool | Type | Polishing Scheme | Accuracy (QV) | Contiguity (N50) | BUSCO Completeness | Computational Cost |
|---|---|---|---|---|---|---|
| Flye | Long-read only | Racon (1x) + Pilon (1x) | 42.5 | 28.7 Mb | 95.8% | Medium |
| Flye | Long-read only | Racon (2x) + Pilon (1x) | 49.3 | 29.1 Mb | 96.2% | High |
| Flye with Ratatosk | Error-corrected long reads | Racon (2x) + Pilon (1x) | 52.7 | 31.4 Mb | 97.5% | High |
| Canu | Long-read only | Racon (2x) + Pilon (1x) | 45.2 | 25.3 Mb | 94.1% | Very High |
| Raven | Long-read only | Racon (2x) + Pilon (1x) | 44.8 | 26.9 Mb | 94.7% | Medium |
| Shasta | Long-read only | Racon (2x) + Pilon (1x) | 41.3 | 22.4 Mb | 92.8% | Low |
The benchmark demonstrated that Flye outperformed all assemblers, particularly when combined with Ratatosk for error correction of long reads [94]. Polishing consistently improved assembly accuracy and continuity, with two rounds of Racon followed by Pilon yielding optimal results [94]. This comprehensive evaluation provided validated guidance for researchers requiring high-quality genome assemblies.
Taxonomic Profiling Tools
In microbiome research, different computational approaches exist for analyzing sequencing data, each with distinct strengths and limitations:
Marker Gene Analysis (16S rRNA)
- QIIME [96]: Provides interface for taxonomic assignment and diversity analysis
- MOTHUR [96]: Implements various algorithms for processing sequencing data
- DADA2 [96]: Uses quality profiles to correct sequencing errors
Shotgun Metagenomics
- Kraken [96]: Utilizes unique k-mer distributions to assign taxonomy
- MetaPhlAn2 [96]: Uses clade-specific marker genes to differentiate microbial taxa
- MEGAHIT [96]: Efficient de novo assembler for metagenomic data
Each approach carries different implications for resolution and functional inference. While 16S rRNA gene sequencing assesses diversity and taxonomic composition, it cannot be described as "metagenomics," which properly refers to random sequencing of all DNA within a sample to access functional potential [15]. The choice between these methods should align with research objectives and available resources.
Specialized Tool Performance
Performance benchmarking extends to specialized bioinformatics domains, including viral genomics. A comparison of three tools for identifying SARS-CoV-2 subgenomic RNAs (sgRNAs) – Periscope, LeTRS, and sgDI-tector – revealed high concordance in detecting canonical sgRNAs but greater variability in identifying noncanonical species [97].
This evaluation used amplicon-based Illumina sequencing of infected Caco-2 cells across multiple time points, with samples down-sampled to equal fragment counts for fair comparison [97]. The percentage of fragments supporting canonical sgRNAs remained small (0.25%-2.59% of initial fragments), consistent with previous reports [97]. Such specialized benchmarks help researchers select appropriate tools for specific applications beyond general microbiome profiling.
Implementation Frameworks for Reproducible Bioinformatics
Modern bioinformatics increasingly relies on workflow management systems that ensure reproducibility and scalability. These frameworks provide structured environments for implementing and comparing bioinformatics tools:
Table 3: Comparison of Bioinformatics Pipeline Frameworks
| Framework | Language | Execution Model | Strengths | Typical Use Case |
|---|---|---|---|---|
| Nextflow | DSL (Groovy-based) | Dataflow execution with channels | Reproducibility, portable across HPC/cloud | Genomics pipelines & reproducible science [95] |
| Flyte | Python (Typed) | Typed DAGs + container tasks | Type safety, versioning, lineage tracking | ML + Bioinformatics pipelines [95] |
| Prefect | Python | Dynamic runtime DAG | Developer-friendly, excellent observability | Research groups transitioning to automation [95] |
| Apache Airflow | Python | Static DAG scheduler | Enterprise readiness, extensive ecosystem | Large-scale production workflows [95] |
| Snakemake | Python | Rule-based execution | Readable syntax, integration with Python | Academic research, single-machine to cluster [93] |
Nextflow has emerged as particularly prominent in genomics due to its native support for reproducibility and hybrid execution across HPC and cloud environments [95]. The best-performing assembly pipeline identified in the benchmark study was implemented in Nextflow, enabling efficient parallelization and built-in dependency management [94]. This exemplifies how appropriate framework selection enhances the practical implementation of optimized bioinformatics workflows.
Figure 2: Essential Research Resources. This diagram categorizes key reagents and computational tools required for rigorous bioinformatics benchmarking.
Table 4: Essential Research Reagent Solutions
| Resource | Function | Application Examples |
|---|---|---|
| Genome in a Bottle (GIAB) Reference Materials | Provides benchmark genomes with characterized variants for method validation [94] | Calibrating variant calling pipelines; assessing assembly accuracy |
| Mock Microbial Communities | Known mixtures of microorganisms for quantifying technical biases in microbiome analysis [15] | Evaluating taxonomic classification accuracy; quantifying detection limits |
| Negative Controls (Blanks) | Reagent-only samples to identify contamination sources [15] | Controlling for environmental contamination in low-biomass studies |
| Unique Dual Indices | Barcoding system that reduces index misassignment during sequencing [15] | Multiplexing samples while maintaining sample integrity |
| Container Platforms (Docker/Singularity) | Encapsulates software environments for computational reproducibility [93] [95] | Ensuring consistent tool versions across computing environments |
| Workflow Management Systems | Orchestrates multi-step analyses with automatic dependency handling [95] | Implementing reproducible pipelines for large-scale data analysis |
Based on the consolidated benchmark findings, the following recommendations emerge for selecting and implementing bioinformatics tools:
First, prioritize independent performance assessments over popularity metrics. The most cited tools are not necessarily the best performers for specific applications [92]. Consult recent benchmark studies that use standardized metrics and reference datasets relevant to your research domain.
Second, implement comprehensive polishing strategies for genome assembly. For long-read assemblies, combine Flye with Ratatosk error correction followed by multiple rounds of Racon and Pilon polishing to achieve optimal accuracy and continuity [94].
Third, adopt workflow management frameworks like Nextflow to ensure reproducibility and scalability [95]. These systems provide built-in support for version control, checkpointing, and execution across diverse computing environments.
Fourth, incorporate appropriate controls throughout experimental workflows. Include mock communities, negative controls, and standardized reference materials to distinguish technical artifacts from biological signals [15]. Transparently report all control results alongside experimental findings.
Finally, embrace comprehensive benchmarking practices even when results contradict personal preferences or established conventions. As the field advances, maintaining rigorous, unbiased evaluation standards remains fundamental to generating reliable biological insights and advancing therapeutic development.
The human microbiome, particularly the gut microbiota, is a key mediator of essential human functions, including metabolism, immune regulation, and colonization resistance against pathogens [7]. Over the past decade, advances in sequencing technologies and analytical tools have revolutionized our understanding of its composition and function, revealing profound influences on human health and disease [25]. The therapeutic potential of microbiome manipulation is now being explored across multiple medical specialties, with significant implications for drug development and personalized medicine approaches.
The validation of microbiome-based approaches varies substantially across therapeutic areas, reflecting differences in disease mechanisms, available biomarkers, and clinical evidence. This guide objectively compares the application of microbiome analysis across three major therapeutic areas—gastrointestinal disorders, infectious diseases, and oncology—within the framework of international consensus standards for microbiome testing [7] [14]. A foundational understanding of these variations is crucial for researchers and drug development professionals seeking to implement microbiome science in their work.
Table: Overview of Microbiome Analysis Across Therapeutic Areas
| Therapeutic Area | Primary Microbial Mechanisms | Key Clinical Applications | Consensus Validation Level |
|---|---|---|---|
| Gastrointestinal | Dysbiosis, barrier function, metabolic output | IBD, IBS, recurrent C. difficile diagnosis & management | Established for C. difficile; emerging for IBD |
| Infectious Disease | Colonization resistance, pathogen exclusion | Recurrent C. difficile management, pathogen prediction | Established for C. difficile (FMT) |
| Oncology | Immunomodulation, drug metabolism | Immunotherapy response prediction, toxicity management | Emerging/Investigational |
Analytical Methodologies and Consensus Standards
International Consensus on Microbiome Testing
An international multidisciplinary expert panel has established standardized frameworks for microbiome testing in clinical practice through a Delphi consensus process [7] [14]. These guidelines address critical methodological considerations essential for generating reliable, reproducible data across therapeutic applications. The consensus emphasizes that appropriate modalities for gut microbiome community profiling include amplicon sequencing (e.g., 16S rRNA) and whole genome sequencing, while conventional microbial cultures or polymerase chain reactions, though useful for specific pathogen identification, cannot be considered comprehensive microbiome testing [7] [14].
The analytical workflow for microbiome analysis requires strict standardization at every stage, from sample collection to data interpretation. According to consensus statements, stool collection should utilize kits with genome preservative, and testing should occur within a recommended time frame with samples stored at -80°C in the laboratory [14]. The final report should include the patient's medical history and detailed test protocol methodology, including stool collection, DNA extraction, and post-sequencing analyses [7]. Critically, the consensus discourages reporting oversimplified metrics such as the Firmicutes/Bacteroidetes ratio, as they do not capture the complex variation in gut microbiome composition and lack sufficient evidence for establishing causal relationships with host health [14].
Experimental Workflow for Microbiome Analysis
The following diagram illustrates the standardized experimental workflow for microbiome analysis as recommended by international consensus guidelines:
Diagram Title: Standardized Microbiome Analysis Workflow
Essential Research Reagents and Materials
Table: Key Research Reagent Solutions for Microbiome Analysis
| Reagent/Material | Function | Application Considerations |
|---|---|---|
| Stool Collection Kit with DNA Stabilizer | Preserves microbial DNA integrity during transport and storage | Must maintain sample stability at variable temperatures; critical for reproducibility |
| DNA Extraction Kit | Isolates high-quality microbial DNA from complex samples | Should be optimized for bacterial cell wall lysis; key determinant of data quality |
| 16S rRNA Primer Sets | Amplifies variable regions for bacterial identification | Selection of variable region (V3-V4) affects taxonomic resolution |
| Shotgun Metagenomic Library Prep Kit | Prepares sequencing libraries for whole-genome analysis | Enables strain-level resolution and functional gene assessment |
| Positive Control Standards | Monitors technical variability and batch effects | Mock microbial communities essential for quality control |
| Bioinformatic Pipelines | Processes raw sequencing data into interpretable formats | QIIME 2, mothur, or HUMAnN2 for different analytical needs |
Gastrointestinal Applications
Validation Status and Clinical Utility
Gastrointestinal disorders represent the most validated application of microbiome analysis, with the strongest evidence base for clinical implementation. The international consensus recognizes fecal microbiota transplantation (FMT) as a recommended management strategy for recurrent Clostridioides difficile infection, representing the first routinely accepted microbiome-based therapy [7]. For other GI conditions like inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS), microbiome testing remains primarily investigational, though with promising associations documented in research settings.
The clinical utility of microbiome analysis in gastroenterology stems from the direct involvement of gut microbes in intestinal homeostasis, barrier function, and immune regulation. Dysbiosis—an imbalance in the gut microbial community—has been causally linked to the development and progression of various gastrointestinal diseases [25]. However, the consensus currently states there is insufficient evidence to widely recommend routine microbiome testing in clinical practice for most GI conditions, highlighting the need for dedicated validation studies [7].
Key Analytical Considerations
Microbiome analysis in gastrointestinal applications requires special attention to confounding factors that significantly influence microbial composition. The international consensus recommends collecting comprehensive clinical metadata to provide context for microbiome test results, including personal patient features (age, gender, body mass index), medication history (particularly antibiotics and proton pump inhibitors), and detailed medical history [14]. Standardized assessment of gut transit time is also recommended, as it significantly affects microbial community structure [7].
For gastrointestinal applications, the consensus emphasizes that microbiome reports should include alpha and beta diversity measures with the deepest possible taxonomic resolution, while excluding overly simplistic metrics like phylum-level composition or Firmicutes/Bacteroidetes ratios that lack clinical utility [14]. The reporting of taxa and clusters relevant to human health should be consistent and referenced against matched control groups to facilitate appropriate interpretation.
Infectious Disease Applications
Validation Status and Clinical Utility
In infectious diseases, microbiome applications have achieved validated clinical utility specifically for recurrent Clostridioides difficile infection (rCDI), for which fecal microbiota transplantation (FMT) is now recommended in clinical guidelines [7]. This represents the most established therapeutic application of microbiome science, with robust evidence supporting its efficacy in restoring microbial diversity and breaking the cycle of recurrence. The mechanism primarily involves the restoration of colonization resistance against pathogens through the reintroduction of diverse commensal communities.
Beyond C. difficile, microbiome testing in infectious diseases remains predominantly investigational, though with promising potential for predicting susceptibility to specific infections and understanding pathogen exclusion mechanisms. The gut microbiota serves as a key mediator of colonization resistance, limiting the expansion of opportunistic pathogens through resource competition, production of inhibitory compounds, and maintenance of gut barrier integrity [7]. However, the consensus does not currently endorse routine microbiome testing for predicting general infectious risk or for managing acute infections beyond the specific indication of rCDI.
Key Analytical Considerations
For infectious disease applications, microbiome analysis must distinguish between colonization, infection, and clinical disease states, requiring specialized analytical approaches. While comprehensive microbiome profiling utilizes sequencing technologies, targeted pathogen detection may employ conventional PCR or culture methods—though these targeted approaches are not considered microbiome testing per consensus definitions [7]. The functional capacity of the microbial community to resist pathogen colonization may be more informative than purely compositional metrics for infectious disease applications.
The consensus strongly recommends that microbiome testing for infectious disease indications be supervised by a referring healthcare provider, with clear communication about the limited evidence for most applications beyond rCDI [14]. Post-testing therapeutic advice by the testing provider is strongly discouraged, with management decisions remaining the responsibility of the treating clinician based on integrated clinical judgment.
Oncology Applications
Validation Status and Clinical Utility
In oncology, microbiome applications represent an emerging field with promising but not yet validated clinical utility. The most advanced evidence involves predicting response to immune checkpoint inhibitors (ICIs) in cancer immunotherapy [7]. Research has demonstrated that specific gut microbiome signatures can modulate antitumor immunity and influence treatment outcomes, with studies showing associations between microbial composition and response to immunotherapy in melanoma, renal cell carcinoma, and other malignancies [7] [98].
The potential mechanisms linking the microbiome to cancer therapy response include immunomodulation through molecular mimicry, antigen presentation, and cytokine production, as well as direct microbial metabolism of chemotherapeutic agents [25]. However, the international consensus currently categorizes these applications as investigational, with insufficient evidence for routine clinical implementation of microbiome testing in oncology practice. The field is rapidly evolving, with numerous clinical trials underway to validate specific microbial biomarkers for predicting and improving cancer treatment outcomes.
Key Analytical Considerations
Oncology applications present unique challenges for microbiome analysis due to the profound effects of cancer itself and its treatments (chemotherapy, radiation, immunotherapy) on microbial communities. The consensus emphasizes the critical importance of controlling for these confounders when interpreting microbiome data in oncology patients [7]. Comprehensive metadata collection is essential, including cancer type and stage, treatment history and timing, concomitant medications (especially antibiotics), and nutritional status.
For oncology applications, microbiome analysis should ideally incorporate functional assessments through metagenomic or metabolomic approaches, as mechanistic links to therapy response likely involve specific microbial functions rather than mere taxonomic composition. The consensus notes that therapeutic manipulation of the microbiome in oncology—through probiotics, prebiotics, or FMT—should be conducted under rigorous investigative conditions until validated approaches emerge [7].
Comparative Analysis Across Therapeutic Areas
Validation Metrics and Clinical Implementation
Table: Comparative Validation Metrics Across Therapeutic Areas
| Validation Parameter | Gastrointestinal | Infectious Disease | Oncology |
|---|---|---|---|
| Evidence Level | Established for rCDI; emerging for IBD/IBS | Established for rCDI | Emerging/Investigational |
| Consensus Recommendation | Conditional for rCDI; research for others | Recommended for rCDI | Research only |
| Regulatory Framework | Developing | Developing for FMT | Early stage |
| Standardized Protocols | Available for sequencing | Available for FMT | In development |
| Clinical Implementation | Selective | Established for rCDI | Clinical trials |
| Therapeutic Applications | FMT, dietary intervention | FMT | Immunotherapy modulation |
Methodological Considerations and Challenges
The application of microbiome analysis across therapeutic areas faces several shared methodological challenges that must be addressed for successful clinical translation. The international consensus identifies significant variability in microbiome composition driven by factors including diet, medications, age, and geographic location, complicating the definition of universal "healthy" or "disease-associated" profiles [7] [14]. This biological variability necessitates careful study design with appropriate controls and sufficient sample sizes to distinguish true disease signals from background variation.
Additional challenges include the gap between correlation and causation in microbiome-disease relationships, the limited knowledge most clinicians currently have about microbiome science, and the absence of validated tests for therapeutic monitoring [7]. The consensus strongly discourages direct-to-consumer testing without clinical guidance, noting the risk of inappropriate subsequent medical actions based on poorly interpreted results [14]. Furthermore, the analytical complexity of microbiome datasets requires specialized computational expertise that may not be readily available in all clinical settings.
Advancing Microbiome-Based Therapeutics
The future validation of microbiome analysis across therapeutic areas will require a shift from descriptive associations to mechanistic understanding of host-microbiome interactions [25]. Priority areas include advancing biomarker discovery through robust validation pipelines, developing standardized preclinical models that better recapitulate human physiology, and implementing multi-omics approaches to unravel the functional complexity of microbial communities [25]. For drug development professionals, these advances will enable more targeted therapeutic strategies that manipulate specific microbial functions or community structures to achieve clinical benefits.
The international consensus highlights the need for interdisciplinary collaboration to address persistent challenges in microbiome science, including ethical considerations, regulatory frameworks, and economic barriers to implementation [7] [25]. Future validation efforts should prioritize well-designed clinical studies that demonstrate not only statistical associations but also measurable improvements in patient outcomes and healthcare value. As the field matures, microbiome-based diagnostics and therapeutics are poised to become increasingly integrated into personalized treatment approaches across gastrointestinal, infectious disease, and oncology applications.
Concluding Comparative Assessment
Based on current evidence and consensus guidelines, gastrointestinal applications hold the most advanced validation status for microbiome analysis, with proven utility for recurrent C. difficile infection and emerging potential for IBD and IBS. Infectious disease applications are firmly established for this specific indication but lack validation for broader infectious risk assessment or management. Oncology applications represent the most emergent area, with promising evidence for predicting immunotherapy response but not yet reaching the threshold for routine clinical implementation.
Across all therapeutic areas, the international consensus emphasizes that microbiome testing should currently be guided by healthcare professionals with awareness of its limitations, and should prioritize patient care integration through rigorous evidence generation [7] [14]. As research advances, the validation landscape will continue to evolve, potentially expanding the clinical utility of microbiome analysis across these and other therapeutic domains.
The field of microbiome research is undergoing a critical paradigm shift, moving from documenting correlative relationships to establishing firm causal mechanisms. While early research successfully identified numerous associations between microbial communities and host health, the inherent complexity of the microbiome has made demonstrating causality extraordinarily difficult. This transition is essential for the development of reliable biomarkers and effective microbiome-based therapeutics [99]. The enthusiasm for microbiome-based interventions in both academic and industrial settings has been tempered by high-profile failures, highlighting the urgent need for more rigorous mechanistic understanding [99].
Establishing causality in microbiome research requires demonstrating that alterations in the microbiome precede and directly contribute to disease pathogenesis, rather than merely occurring as a consequence of the disease process or treatment [25]. This distinction is crucial for identifying molecular mechanisms that can serve as legitimate therapeutic targets. The challenge is particularly pronounced at the strain level, where individual bacterial strains within the same species can exhibit dramatically different biological properties due to extensive genetic and functional diversity [100]. This review examines the current methodologies, experimental models, and analytical frameworks enabling researchers to progress from correlation to causation in strain-level microbiome analysis.
The Scientific Framework: Chains of Evidence from Correlation to Causation
The Experimental "Funnel" for Establishing Causality
Research to uncover microbiome-driven phenotypes typically follows a systematic "chain of evidence" that progresses through five distinct levels of experimental validation [101]. This methodological funnel begins with broad observational studies and narrows progressively to specific molecular mechanisms:
- Level 1: Association Studies - Researchers identify microorganisms that are statistically associated with diseased versus healthy individuals through sequencing-based studies. These correlative observations generate hypotheses for further testing but cannot establish causation [101].
- Level 2: Germ-Free and Antibiotic-Treated Models - Microbiome-depleted organisms (germ-free animals or antibiotic-treated hosts) demonstrate whether microbes play necessary roles in disease phenotypes. If the phenotype is absent or altered in microbiome-depleted models, it suggests microbial involvement [101].
- Level 3: Fecal Microbiota Transplants (FMTs) - Transfer of microbial communities from diseased donors to recipient animals tests whether the phenotype can be transmitted via microbiota. Successful transfer provides stronger evidence for causality while narrowing the focus to transmissible components [101].
- Level 4: Microbial Strain Identification - Individual bacterial strains are isolated and tested in gnotobiotic models to identify specific microorganisms responsible for the phenotype [101].
- Level 5: Molecular Mechanism Elucidation - The specific bacterial molecules (metabolites, proteins, etc.) responsible for the host phenotype are identified and their mechanisms of action characterized [101].
This multi-level framework ensures rigorous validation at each step, progressively moving from community-level associations to strain-specific molecular mechanisms.
Strain-Level Resolution: Why Bacterial Strains Matter
The imperative for strain-level analysis stems from fundamental microbiological principles. A bacterial "species" represents a taxonomic construct that can contain individual strains with up to 30% difference in their genomic content—a greater genetic disparity than exists between humans and mice [100]. This extensive genetic microdiversity translates to functionally distinct strains within the same species, with differential impacts on host health and disease.
Notable examples illustrate this critical principle:
- Escherichia coli: While some strains are commensal gut residents, others like O104:H4 can acquire Shiga toxin-encoding prophages and become pathogenic [102].
- Akkermansia muciniphila: Specific strains exhibit anti-inflammatory properties with beneficial effects on obesity and diabetes, while other strains lack these characteristics [102].
- Ruminococcus gnavus: Certain strains bloom in inflammatory bowel disease (IBD) patients and harbor genes providing adaptive advantage in inflammatory conditions [103].
The functional consequences of strain-level differences can be dramatic even with minimal genetic variation. For instance, E. coli CFT073 (pathogenic) and E. coli Nissle 1917 (probiotic) share 99.98% genome sequence similarity yet have opposing effects on host health [102]. This resolution is essential for accurate biomarker discovery and targeted therapeutic development.
Table 1: Examples of Strain-Specific Functions with Clinical Relevance
| Bacterial Species | Strain-Specific Difference | Clinical Impact |
|---|---|---|
| Escherichia coli | Presence of Shiga toxin genes in O104:H4 | Associated with severe foodborne outbreaks |
| Akkermansia muciniphila | Anti-inflammatory properties in specific strains | Potential therapeutic for metabolic disorders |
| Ruminococcus gnavus | Specific strain blooms in IBD | Potential IBD biomarker and therapeutic target |
| Clostridium acnes | Heterogeneous strains across body sites | Differential association with skin health |
Methodological Approaches for Strain-Level Analysis
Computational Tools for Strain-Level Resolution
Advancements in computational methods have been instrumental in enabling strain-level analysis of microbiome data. Several sophisticated algorithms have been developed to address the unique challenges of distinguishing highly similar strains within complex microbial communities:
StrainScan is a recently developed tool that employs a novel hierarchical k-mer indexing structure to achieve high-resolution strain identification. Its innovative Cluster Search Tree (CST) architecture first clusters highly similar strains, then uses strain-specific k-mers to distinguish individual strains within these clusters. This approach achieves a 20% higher F1 score in identifying multiple strains compared to previous state-of-the-art tools [102].
StrainGE takes a different approach, using a database of marker genes to untangle strain mixtures. However, it is limited to reporting representative strains from predefined clusters, potentially missing important strain-level variations within these clusters [102].
EVORhA represents an assembly-based method that identifies strains through local haplotype assembly. It defines candidate strains as genetically distinct combinations of polymorphisms, then extends and merges these candidates based on read frequency and overlap. This method requires extremely high coverage (50-100× per strain) but can potentially resolve complete strain genomes [104].
Table 2: Comparison of Strain-Level Analysis Tools
| Tool | Methodology | Key Advantage | Limitation |
|---|---|---|---|
| StrainScan | Hierarchical k-mer indexing with Cluster Search Tree | 20% higher F1 score for multi-strain identification; higher resolution | Requires reference genomes for targeted bacteria |
| StrainGE | Marker-gene based with clustering | Identifies representative strains in mixtures | Limited to cluster-level resolution (0.9 k-mer Jaccard similarity) |
| StrainEst | Co-abundance based binning | Identifies strains without reference genomes | 99.4% ANI cutoff can group functionally distinct strains |
| EVORhA | Local haplotype assembly | Can reconstruct complete strain genomes | Requires extremely high coverage (50-100× per strain) |
| DESMAN | Variant frequency analysis | Estimates strain frequencies without assembly | Requires metagenome-assembled genomes (MAGs) as input |
Experimental Models for Establishing Causality
Preclinical models remain essential for moving from computational predictions to demonstrated causality in host-microbiome interactions. The recent Consensus Statement on establishing causality in microbiome research provides expert guidance on model selection and application [25]:
Germ-Free Animal Models provide the most controlled system for testing causal relationships between specific microorganisms and host phenotypes. These models allow researchers to introduce precisely defined microbial communities into previously sterile animals, enabling direct assessment of each strain's contribution to host physiology and disease [25].
Human Microbiota-Associated (HMA) Mice involve transplanting human fecal microbiota into germ-free animals, creating a model that more closely approximates the human microbial ecosystem while maintaining experimental control. These models have been particularly valuable for studying human-specific host-microbiome interactions [25].
Organoid and Gut-on-a-Chip Systems offer reduced complexity models for mechanistic studies at the cellular level. These systems recapitulate key aspects of intestinal architecture and function, enabling detailed investigation of host-microbiome interactions at the epithelial barrier. However, they lack the full physiological context of animal models [25].
Each model system presents distinct advantages and limitations, and the Consensus Statement emphasizes that human trials remain essential for ultimately establishing the efficacy of microbiome-based interventions [25].
Advanced Analytical Frameworks
Multi-Technology Meta-Analysis (MTMA)
The Multi-Technology Meta-Analysis (MTMA) framework represents a powerful approach for identifying robust, reproducible strain-disease associations across multiple studies and technologies. By integrating datasets generated using different DNA-profiling technologies (16S rRNA sequencing, whole-genome shotgun sequencing, phylogenetic microarrays), MTMA overcomes the limitations inherent to any single technology [103].
This approach was recently applied to inflammatory bowel disease (IBD), integrating 3,407 samples from 21 datasets spanning 15 cohorts. The analysis revealed that significant strain associations do not always correspond to species-level significance, and conversely, significant species associations are not always recaptured at the strain level [103]. This demonstrates the critical importance of strain-level resolution for identifying true biological signals.
The MTMA approach identified several previously unreported associations, including two uncharacterized Lachnospiraceae strains consistently decreased in both luminal and mucosal contents of IBD patients. These strains were correlated with inflammation-related pathways representing known mechanisms targeted for IBD treatment [103].
Machine Learning for Predicting Strain-Drug Interactions
Machine learning approaches now enable systematic prediction of how pharmaceuticals impact specific microbial strains. A recently developed random forest model integrates chemical properties of drugs with genomic features of microbes to predict strain-drug interactions with remarkable accuracy (ROC AUC of 0.972) [105].
This model uses 148 microbial features (describing the number of genes in each KEGG pathway) and 92 drug features (derived from the drug's SMILES representation) to predict whether a given drug will inhibit the growth of a specific microbial strain [105]. The framework successfully predicts outcomes of in vitro drug-microbe experiments as well as drug-induced microbiome dysbiosis in animal models and clinical trials.
This computational approach enables large-scale mapping of interactions between pharmaceuticals and human gut bacteria, demonstrating that medications' antimicrobial properties are tightly linked to their adverse effects. Such predictive frameworks have potential to guide personalized pharmaceutical treatment by identifying individuals at risk for microbiome-mediated side effects [105].
Experimental Protocols for Strain-Level Validation
Comprehensive Workflow for Strain-Level Causal Validation
The following experimental workflow integrates multiple technologies and approaches to establish causal mechanisms at the strain level:
Diagram: Comprehensive workflow for establishing causal mechanisms at the strain level, progressing from sample collection to molecular mechanism elucidation.
Detailed Methodological Protocols
Multi-Technology DNA Profiling Protocol:
- DNA Isolation: Use mechanical lysis with glass beads in a MagNA Lyser followed by column-based purification (e.g., MoBio Ultraclean Tissue and Cells DNA isolation kit) [103].
- 16S rRNA Gene Sequencing: Amplify the V4 region using fusion primers tailed with Illumina adaptors and indexing barcodes. Sequence on Illumina MiSeq platform (2×250 bp) [103].
- Whole-Genome Shotgun Sequencing: Fragment DNA, prepare libraries with appropriate size selection, and sequence on Illumina HiSeq or NovaSeq platforms (2×150 bp) [103].
- PhyloChip Analysis: Amplify V1-V9 regions of 16S rRNA gene and hybridize to G3 PhyloChip arrays following established protocols [103].
Strain-Level Bioinformatic Analysis:
- Quality Control: Remove low-quality reads and adapters using Trimmomatic or comparable tools.
- Strain Identification: Map reads against reference databases (StrainSelect) using StrainScan with default parameters [102] [103].
- Abundance Quantification: Calculate strain-level abundances based on uniquely mapping k-mers or reads.
- Statistical Analysis: Identify differentially abundant strains using appropriate methods (e.g., DESeq2, LEfSe) with multiple testing correction.
In Vivo Causal Validation:
- Gnotobiotic Model Development: Colonize germ-free mice with defined microbial communities including target strains [25] [101].
- Phenotypic Assessment: Monitor disease-relevant phenotypes (inflammatory markers, metabolic parameters, behavioral changes).
- Fecal Microbiota Transplantation: Transfer microbiota from human donors or characterized communities to recipient animals [101].
- Molecular Analysis: Profile host transcriptome, immune parameters, and metabolic outcomes.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Strain-Level Causality Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| DNA Isolation Kits | MoBio Ultraclean Tissue and Cells DNA isolation kit | High-quality DNA extraction from complex samples |
| Strain Reference Databases | StrainSelect, GTDB, NCBI RefSeq | Reference genomes for strain identification and quantification |
| Strain-Level Analysis Tools | StrainScan, StrainGE, StrainEst, EVORhA | Computational strain identification and abundance estimation |
| Sequencing Platforms | Illumina MiSeq, HiSeq, NovaSeq | High-throughput DNA sequencing for metagenomic analysis |
| Gnotobiotic Animal Facilities | Germ-free mouse colonies, isolators | Controlled systems for testing causal strain-phenotype relationships |
| Cell Culture Systems | Organoids, Gut-on-a-Chip devices | Reduced complexity models for mechanistic studies |
| Metabolomics Platforms | LC-MS, NMR spectroscopy | Identification and quantification of microbial metabolites |
The progression from correlative observations to causal mechanisms represents the essential maturation pathway for microbiome research. Strain-level validation stands as the critical frontier in this evolution, enabling researchers to move beyond statistical associations to definitive biological understanding. The integrated frameworks, methodologies, and tools reviewed here provide a roadmap for establishing causality through multi-level evidence chains, sophisticated computational approaches, and rigorous experimental validation.
As these approaches become increasingly standardized and accessible, we anticipate accelerated discovery of strain-specific contributions to human health and disease. This progress will ultimately unlock the potential of microbiome-based diagnostics, therapeutics, and personalized medicine approaches grounded in mechanistic understanding rather than correlative observation. The future of microbiome research lies not merely in identifying which microbes are present, but in definitively establishing how specific strains and their molecular products mechanistically influence host biology.
The development of microbiome-based therapies represents a paradigm shift in medicinal product development, requiring a fundamental re-evaluation of traditional clinical trial frameworks. Unlike conventional small-molecule drugs, microbiome-based therapeutics consist of living organisms designed to modulate the host's existing microbial communities, creating unique challenges in safety assessment and efficacy determination [106]. These products, which include fecal microbiota transplantation (FMT), live biotherapeutic products (LBPs), and rationally designed bacterial consortia, function through ecological mechanisms such as engraftment and community modulation rather than traditional pharmacological pathways [107]. This distinction necessitates specialized trial designs, novel safety monitoring approaches, and product-specific efficacy endpoints that reflect their biological complexity.
The regulatory landscape for these innovative therapies is still evolving. While the first microbiome-based medicinal products have recently received marketing approval for recurrent Clostridioides difficile infection (rCDI), the absence of well-defined regulatory guidelines for most indications requires developers to adopt a fresh approach to clinical trial design [106] [108]. This guide systematically compares the key considerations for microbiome-based therapy trials against traditional drug development approaches, providing researchers with evidence-based frameworks for designing robust clinical studies that can adequately capture the safety and efficacy profiles of these complex biological entities.
Comparative Analysis: Fundamental Differences in Trial Design
Safety and Tolerability Assessment
Table 1: Safety Assessment Comparison Between Small Molecule and Microbiome-Based Therapies
| Safety Consideration | Small Molecule Drugs | Microbiome-Based Therapies |
|---|---|---|
| Initial Study Population | Typically healthy volunteers [107] | Often patient populations from the start [106] [107] |
| Primary Safety Focus | Systemic toxicity, organ-specific damage, adverse events (AEs) [107] | Local tolerability, engraftment safety, ecological disruption [106] |
| Differentiation Challenge | Distinguishing drug effects from spontaneous health events | Separating therapy effects from underlying disease symptoms [106] [107] |
| Long-Term Monitoring | Defined by drug half-life and metabolites | Extended periods to monitor persistent ecological changes [106] |
| Unique Risks | Off-target binding, metabolite accumulation | Horizontal gene transfer, pathogen overgrowth, immune modulation [108] |
Safety assessment for microbiome-based therapies extends beyond conventional adverse event monitoring to include ecological safety parameters. Unlike small molecules that are metabolized and eliminated, living therapeutic organisms may persist, replicate, and integrate with the host's native microbiome through engraftment [106]. This necessitates monitoring for potential disruptions to the microbial ecosystem's balance, which could have unintended consequences. For site-specific applications (vaginal, topical, etc.), local tolerability becomes a primary endpoint rather than a secondary consideration [106]. Additionally, the common practice of initiating trials in patient populations rather than healthy volunteers, while providing early efficacy signals, complicates the distinction between adverse events and symptoms of the underlying condition being treated [107].
Efficacy Endpoints and Pharmacokinetics
Table 2: Efficacy Endpoints and Kinetic Assessment Comparison
| Efficacy Parameter | Small Molecule Drugs | Microbiome-Based Therapies |
|---|---|---|
| Primary Efficacy Measure | Symptom improvement, biomarker normalization [107] | Engraftment success, symptom improvement, metabolic output [106] [107] |
| Kinetic Assessment (PK) | Absorption, distribution, metabolism, excretion (ADME) [107] | Microbial quantification at site of action, metabolite production [107] |
| Dose-Response Relationship | Typically linear, predictable [107] | Often non-linear, plateau effect [106] [107] |
| Relevant Biological Samples | Blood, plasma, urine [107] | Stool, vaginal swabs, skin samples, bronchoalveolar lavage [107] |
| Key Analytical Methods | HPLC, mass spectrometry [107] | Genomic sequencing, metabolomics, cultivation assays [7] [109] |
The efficacy assessment of microbiome-based therapies requires endpoints that reflect their mechanism of action. Engraftment success—the measurable integration and persistence of therapeutic strains within the host microbiome—serves as a critical efficacy endpoint unique to this product category [106]. Unlike traditional pharmacokinetics that track drug concentration over time, microbiome-based product kinetics focus on quantifying microbial strains and their metabolic outputs at the site of action [107]. This often involves stool analysis for gut-based therapies, swabs for topical applications, or tissue biopsies for localized treatments. Efficacy measures must be product-specific and aligned with the intended function, ranging from improvement in stool consistency (using standardized tools like the Bristol Stool Chart) to reduction in dermatitis lesions or changes in tumor size in oncological applications [106] [107].
Trial Design and Control Strategies
Microbiome-based therapy trials often employ streamlined dose-finding approaches, as increasing the dose of living organisms does not necessarily enhance efficacy and may even introduce safety concerns [106]. Many early-phase trials focus on single-dose regimens, with higher doses tested primarily for safety assessment rather than efficacy optimization [106] [107]. Placebo-controlled designs remain essential for robust efficacy assessment in later-phase trials, though early-phase studies may bypass placebos to focus on rapid proof-of-concept generation [106]. The financial constraints common in this emerging field have led to innovative approaches such as single-cohort trials that combine safety, tolerability, and efficacy assessments, providing crucial proof-of-concept data for additional funding while maintaining scientific rigor [106].
Analytical Methodologies and Standardization Frameworks
Microbiome Analysis Techniques
The accurate assessment of microbiome-based therapy outcomes depends on robust analytical methodologies standardized across study sites. The international consensus statement on microbiome testing in clinical practice recommends appropriate modalities for gut microbiome community profiling, including amplicon sequencing (e.g., 16S rRNA gene sequencing) and whole genome sequencing (shotgun metagenomics) [7]. The consensus panel specifically notes that multiplex PCR and bacterial cultures, while potentially useful for specific applications, cannot be considered comprehensive microbiome testing methods nor serve as proxies for complete microbiome profiling [7].
Standardized protocols must address pre-analytical variables that significantly impact results. The international consensus recommends detailed documentation of stool collection and storage methods, DNA extraction techniques, amplification protocols, sequencing parameters, and post-sequencing analytical approaches [7]. These standards are essential for generating comparable data across different clinical sites and studies. The consensus discourages the use of oversimplified metrics like the Firmicutes-to-Bacteroidetes ratio as standalone assessments, emphasizing instead a multidimensional approach that captures the complexity of microbial ecosystems [109].
Figure 1: Standardized Workflow for Microbiome Analysis in Clinical Trials. This diagram outlines the critical phases from sample collection to data interpretation, highlighting key standardization requirements at each step.
Causality Assessment and Preclinical Models
Establishing causality between microbiome modifications and clinical outcomes remains a significant challenge in the field. The 2025 consensus statement on establishing causality in microbiome research emphasizes the importance of appropriate preclinical models for elucidating the functional role of host-microbiome interactions [25]. The Delphi survey identified germ-free animals, organoids, and ex vivo systems as essential tools, while highlighting the need for improved standardization and translational relevance [25].
These models enable researchers to investigate mechanisms underlying observed clinical effects and establish cause-effect relationships between therapeutic interventions and outcomes. The consensus recommends implementing bacterial isolates of relevance to humans in these models to improve their predictive value [25]. Additionally, the integration of multi-omics approaches (genomics, transcriptomics, proteomics, metabolomics) provides a powerful framework for unraveling microbiome complexity and bridging the gap between basic science and clinical translation [25].
Regulatory and Implementation Considerations
Evolving Regulatory Frameworks
The regulatory landscape for microbiome-based therapies is rapidly evolving, with significant developments in both European and American frameworks. The recent European Regulation on substances of human origin (SoHO) has established new guidelines for the development of microbiome-based therapies, creating a more structured pathway for these innovative products [108]. The regulatory status of a microbiome-based product depends primarily on its intended use, with classifications ranging from medicinal products to medical devices, food supplements, or cosmetics, each governed by different legislative texts and requirements [108].
The intended use, as defined by claims made in labeling, advertising, or oral statements, ultimately determines whether a product is regulated as a drug or under another framework [108]. This places significant importance on precise claim formulation throughout the development process. The first marketing approvals for microbiome-based therapies have been granted for recurrent Clostridioides difficile infection, with Rebyota (2022) and VOWST (2023) establishing precedent for future products [108]. As of 2025, multiple microbiome-based therapies are in clinical development for conditions including inflammatory bowel disease, graft-versus-host disease, and cancer immunotherapy combinations [110].
Practical Implementation and Resource Management
Financial constraints present significant challenges for many organizations developing microbiome-based therapies, particularly startups and academic spin-offs. To address funding limitations, companies can focus on cost-effective, single-cohort trials that combine safety, tolerability, and efficacy assessments [106]. While this approach may extend overall development timelines, it provides crucial proof-of-concept data to secure additional funding for subsequent trial phases without compromising data quality [106].
Engagement with regulatory authorities early in the development process is particularly crucial for microbiome-based products given the evolving regulatory landscape [106]. Scientific advice from the FDA, EMA, or other relevant national authorities provides valuable insights into specific trial expectations and regulatory requirements, potentially preventing costly design modifications later in development [106]. Additionally, the complexity of microbiome science necessitates close collaboration between clinical researchers and microbiome specialists throughout the trial design and implementation process to ensure appropriate endpoint selection, analytical methods, and data interpretation [111].
Essential Research Reagents and Methodologies
Table 3: Essential Research Reagent Solutions for Microbiome Clinical Trials
| Reagent Category | Specific Examples | Primary Function | Implementation Considerations |
|---|---|---|---|
| Sample Collection & Stabilization | DNA/RNA shield solutions, anaerobic transport systems, standardized swabs | Preserve microbial composition at collection, prevent overgrowth during transport | Stability validation under expected transport conditions; compatibility with downstream analyses [7] [109] |
| DNA Extraction Kits | MOBIO PowerSoil Pro, QIAamp DNA Stool Mini Kit | Lyse diverse cell wall types, inhibit removal, high-quality DNA extraction | Standardization across sites; validation for difficult-to-lyse species [7] [109] |
| Sequencing Reagents | 16S rRNA primers (V3-V4), shotgun library prep kits, sequencing standards | Comprehensive community profiling, functional gene assessment | Inclusion of positive controls; batch effect minimization [7] |
| Bioinformatic Tools | QIIME 2, Mothur, MetaPhlAn, HUMAnN | Data processing, taxonomy assignment, functional inference | Pipeline standardization; version control; reproducible workflows [7] |
| Culture Media | Pre-reduced anaerobically sterilized (PRAS) media, selective media | Strain isolation, viability assessment, functional validation | Anaerobic chamber maintenance; media quality validation [7] |
| Metabolomic Analysis | Mass spectrometry standards, metabolite extraction kits | Functional output measurement, mechanism elucidation | Standard curve validation; sample matrix effects assessment [25] |
The selection of appropriate research reagents and methodologies is critical for generating reliable, reproducible data in microbiome clinical trials. The international consensus statement emphasizes that microbiome testing should be performed in dedicated laboratories with specific space and facilities tailored for such testing to prevent contamination and ensure result accuracy [109]. Hospitals and accredited labs provide the specialized equipment, controlled environments, and trained personnel necessary for handling sensitive microbiome samples [109].
Figure 2: Preclinical Models for Microbiome Therapeutic Development. This diagram illustrates the primary applications and key limitations of major preclinical model systems used to establish causality and mechanism of action for microbiome-based therapies.
Standardization across multiple sites in multicenter trials is particularly challenging but essential. The international consensus recommends that microbiome testing reports briefly detail the test protocol, including methods of stool collection and storage, DNA extraction, amplification, sequencing, and post-sequencing analyses to enhance interpretability and cross-study comparisons [7]. The use of In Vitro Diagnostic (IVD)-certified tests, which follow strict quality control measures, represents an important step toward improving reproducibility and trust in microbiome-based diagnostics [109].
The clinical development of microbiome-based therapies requires a fundamental shift from traditional drug development paradigms. Safety assessment must expand to include ecological considerations such as engraftment stability and long-term microbiome impact, while efficacy endpoints need to be product-specific and reflective of the therapeutic mechanism of action. The field is rapidly advancing toward standardized methodologies, with international consensus emerging on appropriate analytical approaches, preclinical models, and regulatory frameworks.
As the pipeline of microbiome-based therapies continues to expand—with over 180 therapies in development across more than 140 companies—the lessons learned from early successes and failures will further refine these clinical trial considerations [110]. By adopting these specialized approaches to safety profiling and efficacy endpoint selection, researchers can generate the robust clinical evidence needed to advance innovative microbiome-based therapies through regulatory approval and into clinical practice, ultimately realizing the potential of microbiome modulation for a wide range of diseases.
The field of clinical microbiome testing is at a pivotal juncture, balancing promising scientific potential against the pressing need for robust regulatory and reporting standards. As commercial testing services proliferate, an international consensus has emerged regarding the essential frameworks required to ensure analytical validity, clinical utility, and ethical implementation. This guide examines the current landscape of microbiome test interpretation, comparing emerging standards against conventional practices and synthesizing evidence from recent international initiatives. The establishment of standardized methodologies represents a critical step toward translating microbiome research into validated clinical applications, particularly for researchers and drug development professionals navigating this complex domain.
The Regulatory Landscape: International Consensus Findings
Key Principles and Minimum Requirements
An international multidisciplinary expert panel convened to establish standardized practices for microbiome testing in clinical settings, creating a foundational framework for implementation. This consensus emphasizes that laboratories providing microbiome testing must adhere to rigorously high-quality standards and involve multidisciplinary expertise throughout the testing process [10] [14]. Importantly, both providers and consumers must acknowledge the currently limited evidence supporting microbiome testing's clinical applications, maintaining transparency about its experimental nature [14]. When testing results prompt changes to patient management, these modifications should be supervised by qualified healthcare professionals rather than through direct-to-consumer interpretation [14].
Appropriate Test Prescription and Pre-Testing Protocols
The international consensus explicitly outlines that microbiome test prescriptions should originate from licensed healthcare providers—including physicians, pharmacists, and dietitians—while specifically excluding non-licensed practitioners such as personal trainers, nutritionists, or osteopaths [14]. The consensus strongly discourages self-prescription by patients and advises against suspending treatments or altering usual diets before testing [14]. Comprehensive clinical metadata collection is mandatory, encompassing patient characteristics (age, gender, BMI, gut transit time), current and past medications, and medical history to properly contextualize microbiome results [14]. Standardized stool collection protocols requiring genome preservatives, specific timeframes for testing, and laboratory storage at -80°C complete the essential pre-analytical requirements [14].
Table: International Consensus on Microbiome Testing Key Elements
| Component | Consensus Standard | Traditional/Variable Practice |
|---|---|---|
| Test Prescription | Licensed healthcare providers only | Direct-to-consumer or non-licensed practitioners |
| Sample Collection | Standardized kits with genome preservative; strict timeframe | Variable collection methods; inconsistent preservation |
| Sample Storage | -80°C in dedicated laboratory | Variable temperatures; non-standardized facilities |
| Metadata Collection | Comprehensive clinical data mandatory | Limited or inconsistent data collection |
| Result Interpretation | Healthcare professional with microbiome expertise | Automated algorithms; non-specialist interpretation |
Analytical Method Standards and Reporting Requirements
Analytical Approaches and Methodological Considerations
The consensus guidelines definitively specify that gut microbiome profiling should utilize either amplicon sequencing (e.g., 16S rRNA) or whole-genome sequencing approaches [14]. Conventional microbial cultures or polymerase chain reaction methods, while potentially useful for specific pathogen identification, are not recommended for comprehensive microbiome analysis and cannot serve as proxies for microbiome testing [14]. When profiling microbial communities, testing must incorporate ecological measures including alpha and beta diversity metrics alongside complete taxonomic profiling, with comparisons made against appropriately matched control groups [14].
The technical execution of these methods requires sophisticated laboratory infrastructure. Marker gene analysis typically employs Illumina MiSeq platforms with region-specific primers (V1-V3 or V4) to sequence hypervariable regions, while shotgun metagenomics utilizes untargeted sequencing to capture all microbial genomes present [96]. Importantly, the field continues to evolve with emerging methodologies including metatranscriptomics, metabolomics, and metaproteomics, though these remain primarily research tools rather than clinical standards [96].
Standardized Reporting and Interpretation Frameworks
The consensus establishes rigorous reporting requirements that must include the patient's medical history and comprehensive test protocol details covering stool collection, DNA extraction, and post-sequencing analyses [14]. Taxa and clusters relevant to human health must be consistently reported alongside alpha and beta diversity measures at the deepest possible taxonomic resolution [14]. Conversely, the guidelines specifically exclude particular dysbiosis indices (e.g., Firmicutes/Bacteroidetes ratio) and composition at the phylum level, as these fail to capture gut microbiome variation within and between hosts and lack sufficient evidence for establishing causal relationships with health outcomes [14].
A critical distinction is made between interpretive responsibilities: post-testing therapeutic advice by the testing provider is strongly discouraged, with this task reserved for the referring healthcare provider who requested the testing [14]. This reflects the panel's position that direct consumer or patient requests for microbiome testing should be discouraged to prevent testing without clear clinical indications or awareness of limitations [14].
Table: Analytical Methods in Microbiome Testing
| Method | Primary Application | Technical Considerations | Clinical Utility |
|---|---|---|---|
| 16S rRNA Sequencing | Taxonomic profiling (bacteria) | Hypervariable region selection critical; 97% OTU threshold arbitrary | Established for community composition; limited functional insights |
| ITS Sequencing | Taxonomic profiling (fungi) | Similar limitations to 16S for fungi | Emerging standard for mycobiome analysis |
| Shotgun Metagenomics | Comprehensive microbial community analysis | Reference database dependent; computational demands high | Functional potential assessment; broader taxonomic resolution |
| Metatranscriptomics | Gene expression profiling | RNA stability challenges; host RNA contamination risk | Insights into active microbial functions; research phase |
Experimental Validation and Benchmarking Approaches
Experimental Designs for Test Validation
Robust experimental validation of microbiome testing methodologies requires carefully controlled benchmarking studies. One comprehensive approach involved sending a single fecal sample from a healthy adult donor to six different testing companies (five European-based, one USA-based) to evaluate consistency across platforms [112]. This design enabled direct comparison of results, interpretations, and recommendations provided by different companies, revealing significant variability in methodological transparency and result reliability [112]. Such benchmarking exercises are essential for identifying standardization gaps and establishing performance metrics for clinical implementation.
Experimental protocols must account for numerous pre-analytical variables including collection timing, storage conditions, and sample preservation methods [113]. Sterile collection tools, standardized timing in relation to food intake or medication, proper storage conditions to preserve microbial DNA/RNA integrity, and appropriate sample numbers (both temporal and spatial) represent critical factors requiring standardization [113]. Dedicated laboratory facilities with specialized equipment, controlled environments to prevent contamination, and trained personnel are essential for ensuring result accuracy and traceability [113].
Causality Establishment and Model Systems
Establishing causality between microbiome configurations and health outcomes remains a fundamental challenge. The Human Microbiome Action Consortium initiated a Delphi survey to assess the utility of preclinical models, including animal and cell-based systems, for elucidating causal relationships [25]. Preclinical models ranging from germ-free animals to organoids and gut-on-a-chip systems provide essential platforms for investigating host-microbiome interactions and establishing cause-effect relationships [25]. However, experts emphasize that these models require improved standardization and translational relevance, with implementation of bacterial isolates specifically relevant to humans [25].
The following experimental workflow diagram illustrates the consensus development process for establishing causality and validation standards:
Implementation Challenges and Future Directions
Addressing Microbiome Variability and Standardization
The inherent variability of microbiome composition presents significant challenges for clinical implementation. Factors including dietary habits, medication use, circadian rhythms, and environmental exposures substantially alter microbial composition within individuals, complicating diagnostic interpretations [113]. This biological variability necessitates standardized collection protocols, multiple longitudinal sampling in some cases, and careful control for confounding variables in analysis [113]. The use of In Vitro Diagnostic (IVD)-certified tests following strict quality control measures represents an important step toward improving reproducibility and trust in microbiome-based diagnostics [113].
Commercial testing services currently face criticism for over-promising messaging, methodological transparency deficiencies, and limited result reliability [112]. Experts recommend distinguishing regulatory requirements based on intended use: kits satisfying consumer curiosity should explicitly state this objective without disease mentions, while CE-marked IVD test kits with deeper analysis and interpretation should target trained healthcare professionals [112]. This distinction would create appropriate regulatory pathways for different use cases while protecting consumers from unvalidated health claims.
Research Reagent Solutions and Essential Materials
The following table details key research reagents and materials essential for implementing standardized microbiome testing protocols:
Table: Essential Research Reagent Solutions for Microbiome Testing
| Reagent/Material | Function | Technical Considerations |
|---|---|---|
| DNA Stabilization Buffers | Preserve microbial genomic material during sample transport | Must maintain DNA integrity without freezing; compatible with downstream applications |
| Extraction Kits with Mechanical Lysis | Break microbial cell walls for DNA recovery | Must efficiently lyse diverse microbial taxa; minimize biases against difficult-to-lyse organisms |
| PCR Primers for 16S rRNA Regions | Amplify target genes for sequencing | Selection of hypervariable regions (V1-V3, V3-V4, V4) affects taxonomic resolution |
| Sequencing Standards and Controls | Monitor technical performance and batch effects | Include positive controls (mock communities) and negative controls (extraction blanks) |
| Bioinformatic Pipelines (QIIME2, Mothur) | Process raw sequencing data into biological insights | Standardized workflows essential for reproducibility and cross-study comparisons |
| Reference Databases (Greengenes, SILVA) | Assign taxonomic classifications to sequences | Database choice and version significantly impact taxonomic assignment accuracy |
The establishment of international consensus standards for clinical microbiome test interpretation represents a transformative development for researchers and drug development professionals. These guidelines provide essential frameworks for analytical validation, methodological standardization, and appropriate clinical implementation. While significant challenges remain—particularly regarding biological variability, causality establishment, and regulatory harmonization—the foundational principles now exist to guide responsible development in this rapidly evolving field. The continuing evolution of these standards will depend on robust benchmarking studies, multidisciplinary collaboration, and thoughtful validation of microbiome-based biomarkers to fulfill the promise of microbiome science in clinical practice.
Conclusion
The validation of microbiome analysis approaches requires coordinated efforts across standardization, methodology, and clinical translation. Current international consensus emphasizes the need for rigorous benchmarking using reference reagents, strain-level resolution, and standardized reporting frameworks to advance from correlative observations to causal mechanistic insights. The promising success rates of microbiome-based therapies in gastrointestinal and infectious diseases demonstrate the field's potential, while highlighting the necessity of multidisciplinary collaboration between clinicians, microbiologists, and computational biologists. Future progress depends on addressing key challenges: developing site-specific complex reference materials, establishing universally accepted validation metrics, and conducting large-scale studies that control for host and environmental confounders. As the field evolves from descriptive to mechanistic understanding, validated microbiome analysis will increasingly enable targeted interventions, personalized microbiome-directed therapies, and reliable translation of microbiome science into clinical practice.
References
- 1. Microbiota vs Microbiome: Key Differences [https://www.allucent.com/resources/blog/what-difference-between-microbiome-and-microbiota]
- 2. Microbiota in health and diseases [https://www.nature.com/articles/s41392-022-00974-4]
- 3. Microbiome [https://en.wikipedia.org/wiki/Microbiome]
- 4. Microbiome definition re-visited: old concepts and new ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-020-00875-0]
- 5. Microbiomes: An Origin Story [https://asm.org/articles/2019/march/microbiomes-an-origin-story]
- 6. Microbiome Vs Microbiota - Know the Difference! [https://www.fiosgenomics.com/microbiome-vs-microbiota/]
- 7. International consensus statement on microbiome testing ... [https://www.sciencedirect.com/science/article/abs/pii/S246812532400311X]
- 8. Nutrition & microbiome research highlights NeuroGASTRO ... [https://www.gutmicrobiotaforhealth.com/nutrition-and-microbiome-research-highlights-from-neurogastro-2025/]
- 9. 2025 results: The International Microbiota Observatory [https://www.biocodexmicrobiotainstitute.com/en/international-microbiota-observatory/2025]
- 10. International consensus statement on microbiome testing in ... [https://pubmed.ncbi.nlm.nih.gov/39647502/]
- 11. International Researchers Draft Consensus Document That ... [https://www.darkdaily.com/?p=51012]
- 12. Clinical context over quick fix: the fresh consensus on ... [https://www.biocodexmicrobiotainstitute.com/en/pro/clinical-context-over-quick-fix-fresh-consensus-microbiome-testing]
- 13. International consensus statement on microbiome testing ... [https://pasteur.hal.science/pasteur-05265380]
- 14. International consensus on microbiome testing in clinical ... [https://www.gutmicrobiotaforhealth.com/new-international-consensus-on-microbiome-testing-in-clinical-practice/]
- 15. A blueprint for contemporary studies of microbiomes [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-025-02091-0]
- 16. Microbiome 101: Studying, Analyzing, and Interpreting Gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6391518/]
- 17. Current Capabilities of Gut Microbiome–Based Diagnostics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8206793/]
- 18. Microbiome [https://accelsiors.com/therapeutic-expertise/microbiome/]
- 19. A systematic framework for understanding the microbiome ... [https://www.nature.com/articles/s41392-024-01946-6]
- 20. A reconceptualized framework for human microbiome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12354763/]
- 21. Applying ecological principles to microbiome engineering [https://www.nature.com/articles/s41564-025-02076-7]
- 22. Microbiome Research - CD BioSciences [https://www.cd-clintrial.com/microbiome-research/]
- 23. Gut microbiome metagenomics in clinical practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562794/]
- 24. Frontiers | The human microbiome in clinical translation: from bench to bedside [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1632435/full]
- 25. A Consensus Statement on establishing causality ... [https://www.nature.com/articles/s41575-025-01041-3]
- 26. Frontiers | The human gut microbiota is associated with host lifestyle: a comprehensive narrative review [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1549160/full]
- 27. From Dysbiosis to Prediction: AI-Powered Microbiome Insights into IBD and CRC [https://www.mdpi.com/2036-7422/16/3/34]
- 28. Clinical translation of microbiome research: takeaways from the 2025 GMFH Summit [https://www.gutmicrobiotaforhealth.com/clinical-translation-of-microbiome-research-takeaways-from-the-2025-gmfh-summit/]
- 29. Next Generation Microbiome Research [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.719072/full]
- 30. Role of Keystone Species in an Ecosystem [https://education.nationalgeographic.org/resource/role-keystone-species-ecosystem/]
- 31. Identification of Keystone Species in the Metabolic Regulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8440917/]
- 32. Unlocking the healthy human microbiome: Redefining core ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11959916/]
- 33. Determining Gut Microbial Dysbiosis: a Review of Applied ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8208139/]
- 34. Development and Validation of a Novel Microbiome-Based ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.781275/full]
- 35. Toward a health-associated core keystone index for the ... [https://www.sciencedirect.com/science/article/pii/S2211124725001494]
- 36. Meta-analysis of gut microbiome reveals patterns ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12309989/]
- 37. Comparative evaluation of sequencing platforms [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365774/]
- 38. Evaluation of 16S rRNA gene sequencing for species and ... [https://www.nature.com/articles/s41467-019-13036-1]
- 39. Full-length 16S rRNA Sequencing Reveals Gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11912586/]
- 40. Next Generation Sequencing Improves Diagnostic 16S ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418051/]
- 41. Creating unity: linking 16S rRNA gene sequence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570451/]
- 42. A species-level identification pipeline for human gut ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1553124/full]
- 43. The unresolved struggle of 16S rRNA amplicon sequencing [https://environmentalmicrobiome.biomedcentral.com/articles/10.1186/s40793-025-00705-6]
- 44. Comparison of RNA- and DNA-based 16S amplicon ... [https://www.nature.com/articles/s41598-025-00969-5]
- 45. an extensive and high-resolution human-related full-length ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11792508/]
- 46. Comparison between 16S rRNA and shotgun sequencing in ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10621-7]
- 47. Computational Metagenomics: State of the Art [https://www.mdpi.com/1422-0067/26/18/9206]
- 48. Comparison between 16S rRNA and shotgun sequencing ... [https://www.nature.com/articles/s41598-021-82726-y]
- 49. Benchmarking metagenomic binning tools on real datasets ... [https://www.nature.com/articles/s41467-025-57957-6]
- 50. Prospective Comparison Between Shotgun Metagenomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9020828/]
- 51. Benchmarking short-read metagenomics tools for removing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11878760/]
- 52. Accurate profiling of microbial communities for shotgun ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-025-02249-w]
- 53. Enhanced metagenomic strategies for elucidating the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417494/]
- 54. A Focus on Metagenomics, Metatranscriptomics, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388303/]
- 55. Systematic metaproteomics mapping reveals functional ... [https://www.nature.com/articles/s41467-025-64433-8]
- 56. Effective data visualization strategies in untargeted ... [https://pubs.rsc.org/en/content/articlehtml/2025/np/d4np00039k]
- 57. metaTP: a meta-transcriptome data analysis pipeline with ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-025-06137-w]
- 58. Presentations [https://galaxyp.org/presentations/]
- 59. Visualizing metagenomic and metatranscriptomic data [https://www.sciencedirect.com/science/article/pii/S2001037024001430]
- 60. Metatranscriptomics-based metabolic modeling of patient ... [https://www.nature.com/articles/s41522-025-00823-6]
- 61. Microbiome-guided precision medicine: Mechanistic ... [https://www.sciencedirect.com/science/article/pii/S3050632825000186]
- 62. Microbiome Analysis via OTU and ASV-Based Pipelines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9029325/]
- 63. Microbiome Informatics: OTU vs. ASV [https://www.zymoresearch.com/blogs/blog/microbiome-informatics-otu-vs-asv?srsltid=AfmBOopU3q2L1F-AWpClGsmwEnttfl5FF2H20MYgtur_WGNtTmWBMmED]
- 64. OTU vs. ASV in Metagenomic Analysis [https://www.seqme.eu/en/blog/article/otu-vs-asv-in-metagenomic-analysis]
- 65. ASV vs OTUs clustering: Effects on alpha, beta, and gamma ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0309065]
- 66. ASVs vs OTUs: Decoding the Microbiome Alphabet Soup [https://elferachid.medium.com/asvs-vs-otus-decoding-the-microbiome-alphabet-soup-246c6e8d45c9]
- 67. Amplicon Sequencing Analysis:OTU or ASV? [https://www.cd-genomics.com/resource-amplicon-sequencing-analysis-out-asv.html]
- 68. The challenges and opportunities in the expanding horizons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584655/]
- 69. Live Biotherapeutic Products: Development, Investment, and ... [https://www.alacrita.com/whitepapers/live-biotherapeutic-products-development-challenges]
- 70. What's New and What's Next in Fecal Microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377394/]
- 71. Microbiome highlights from Digestive Disease Week 2025 [https://www.gutmicrobiotaforhealth.com/microbiome-highlights-from-digestive-disease-week-2025/]
- 72. Ferring Presents New Data Analyses for REBYOTA® (fecal ... [https://ferringusa.com/?press=ferring-presents-new-data-analyses-for-rebyota-fecal-microbiota-live-jslm-at-acg-2025]
- 73. Editorial: Live Biotherapeutic Products: where are we? [https://www.frontiersin.org/journals/microbiomes/articles/10.3389/frmbi.2025.1664282/full]
- 74. Shaping the future of probiotics, live biotherapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527994/]
- 75. Developing standards for the microbiome field - BioMed Central [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-020-00856-3]
- 76. Reporting guidelines for human microbiome research [https://www.nature.com/articles/s41591-021-01552-x]
- 77. Guide to LIMS: Core Functions & 2025 System Comparison [https://intuitionlabs.ai/articles/lims-system-guide-2025]
- 78. Comparison and Optimization of DNA Extraction Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11932244/]
- 79. Comparative pilot study of three commercial kits ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372513/]
- 80. Comparison of DNA extraction methods for detecting ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1675115/full]
- 81. Assessing different methods to preserve biochemical ... [https://www.sciencedirect.com/science/article/pii/S2211926425004412]
- 82. Reducing batch effects in single cell chromatin accessibility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11870453/]
- 83. Developing whole cell standards for the microbiome field [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-022-01313-z]
- 84. Developing whole cell standards for the microbiome field [https://pubmed.ncbi.nlm.nih.gov/35945640/]
- 85. Standardization of 16S rRNA gene sequencing using ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1517208/full]
- 86. Mock community taxonomic classification performance of ... [https://www.nature.com/articles/s41597-023-02877-7]
- 87. Dynamic clinical trial success rates for drugs in the 21st ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572394/]
- 88. Emerging modalities in therapeutics: A comprehensive guide [https://www.drugdiscoverynews.com/emerging-modalities-in-therapeutics-a-comprehensive-guide-16744]
- 89. Navigating the Complexities of Emerging Therapy ... [https://www.pharmtech.com/view/navigating-the-complexities-of-emerging-therapy-development]
- 90. Emerging New Drug Modalities in 2025 [https://www.bcg.com/publications/2025/emerging-new-drug-modalities]
- 91. Comparative analysis of commonly used bioinformatics ... [https://www.sciencedirect.com/science/article/abs/pii/S2452014423000626]
- 92. Popularity and performance of bioinformatics software [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-021-04124-5]
- 93. Benchmarking Bioinformatics Tools: A Practical Guide [https://adbioinformatics.com/benchmarking-bioinformatics-tools/]
- 94. Benchmarking of bioinformatics tools for the hybrid de novo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284544/]
- 95. A Comparative Review of Bioinformatics Pipeline Frameworks ... [https://www.tracer.cloud/resources/bioinformatics-pipeline-frameworks-2025]
- 96. Tools for Analysis of the Microbiome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7598837/]
- 97. Comparative analysis of bioinformatics tools to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10520259/]
- 98. Top Oncology Innovations That Shaped the First Half of 2025 [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]
- 99. Microbiome: Focus on causation and mechanism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6094951/]
- 100. Strain-level dissection of the contribution of the gut ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-016-0304-1]
- 101. Chains of evidence from correlations to causal molecules ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8480537/]
- 102. High-resolution strain-level microbiome composition analysis ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-023-01615-w]
- 103. Strain level and comprehensive microbiome analysis in ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.961020/full]
- 104. Computational Methods for Strain-Level Microbial ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.01925/full]
- 105. A data-driven approach for predicting the impact of drugs ... [https://www.nature.com/articles/s41467-023-39264-0]
- 106. Designing Effective Clinical Trials for Microbiome-Based ... [https://www.sgs.com/en-us/news/2025/01/designing-effective-clinical-trials-for-microbiome-based-products]
- 107. Small Molecule vs Microbiome-Based Clinical Trials [https://www.sgs.com/en-us/news/2025/01/decoding-the-differences-small-molecule-vs-microbiome-based-clinical-trials]
- 108. The regulatory framework for microbiome-based therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC11953238/]
- 109. Navigating microbiome variability: implications for research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12018463/]
- 110. Microbiome Disease Clinical Trial Analysis: Key Insights [https://www.globenewswire.com/news-release/2025/03/04/3036864/0/en/Microbiome-Disease-Clinical-Trial-Analysis-Key-Insights-into-Rich-Pipeline-Featuring-140-Companies-and-180-Therapies-DelveInsight.html]
- 111. The microbiome for clinicians [https://www.sciencedirect.com/science/article/pii/S0092867425004489]
- 112. Microbiome testing in Europe: navigating analytical, ethical ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-024-01991-x]
- 113. Frontiers | Navigating microbiome variability: implications for research, diagnostics, and direct-to-consumer testing [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1580531/full]