Validating Microbiome Biomarkers for Clinical Diagnostics: From Cohort Studies to Clinical Implementation
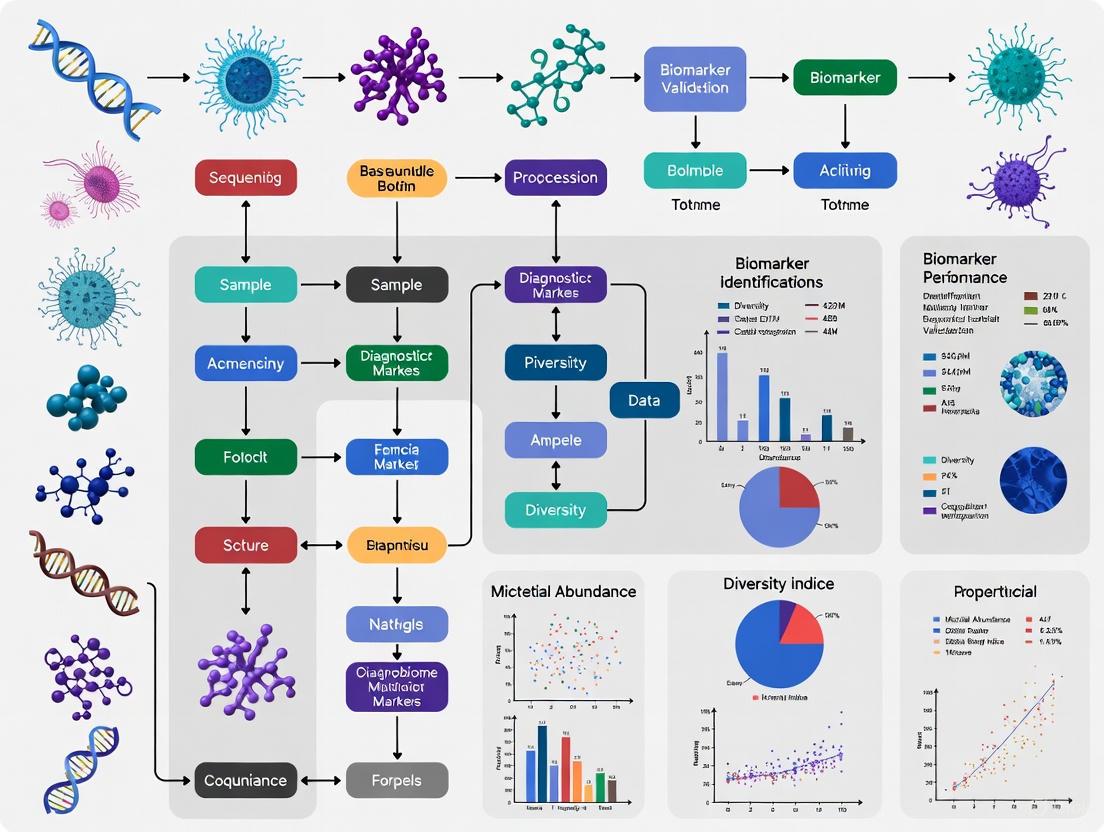
This comprehensive review examines the critical pathway for validating microbiome-based diagnostic biomarkers across diverse disease contexts.
Validating Microbiome Biomarkers for Clinical Diagnostics: From Cohort Studies to Clinical Implementation
Abstract
This comprehensive review examines the critical pathway for validating microbiome-based diagnostic biomarkers across diverse disease contexts. We explore the foundational evidence linking microbial signatures to diseases like colorectal cancer, IBD, and lung cancer, while addressing key methodological challenges in multi-omics integration, batch effect correction, and cohort study design. The article provides strategic frameworks for troubleshooting validation studies and compares emerging computational approaches for robust biomarker identification. By synthesizing evidence from large-scale validation cohorts and cross-study integrations, we outline a roadmap for translating microbial signatures into clinically viable diagnostic tools that could revolutionize precision medicine and early disease detection.
The Microbiome as a Diagnostic Frontier: Establishing Biological Plausibility and Clinical Associations
The traditional pathogen-centric model of disease is increasingly inadequate for understanding complex chronic illnesses. This guide compares the established pathogen model against the emerging holobiont theory, which considers the host and its entire microbial community as a single ecological unit. We objectively evaluate their performance through the lens of contemporary microbiome biomarker diagnostic validation cohort studies, providing experimental data and methodologies that are critical for researchers and drug development professionals. The analysis reveals that incorporating pathobiont dynamics and holobiont-system-level insights significantly improves diagnostic accuracy and predictive power for a range of diseases, from inflammatory conditions to neurodevelopmental disorders.
The concept of the holobiont—a host organism plus all its symbiotic microorganisms, including bacteria, fungi, and viruses—is reshaping fundamental concepts in human biology and disease [1]. This framework challenges the binary classification of microbes as purely "good" or "bad," introducing the critical concept of the pathobiont.
Unlike traditional pathogens, pathobionts are potentially beneficial microbes that can, under specific environmental conditions, contribute to disease [2]. The holobiont model posits that disease often results from ecosystem dysbiosis, where a shift in the microbial community structure and function leads to a loss of beneficial microbes, an expansion of pathobionts, and a breakdown in host-microbe homeostasis. This paradigm shift has profound implications for diagnostic strategies and therapeutic development.
Model Comparison: Pathogen-Centric vs. Holobiont-Based Diagnostics
The following analysis compares the diagnostic and predictive performance of the traditional pathogen model against the holobiont framework, based on cross-cohort validation studies.
Table 1: Diagnostic Model Performance Across Disease Categories
| Disease Category | Diagnostic Approach | Intra-Cohort Validation AUC (Mean) | Cross-Cohort Validation AUC (Mean) | Key Strengths & Limitations |
|---|---|---|---|---|
| Intestinal Diseases (e.g., CD, UC, CRC) | Pathogen-Centric | ~0.77 | Low (Except specific pathogens) | Limited to known etiological agents. |
| Holobiont (Microbiome Biomarkers) | ~0.77 | ~0.73 | Superior cross-cohort generalizability for prescreening. | |
| Autoimmune Diseases (e.g., MS, RA) | Pathogen-Centric | Variable | Very Low | Fails to capture complex, multi-factorial etiology. |
| Holobiont (Microbiome Biomarkers) | ~0.77 | Low to Moderate | Promising for stratification; performance improved by combined-cohort modeling. | |
| Mental/Nervous System Diseases (e.g., ASD, AD, PD) | Pathogen-Centric | Not Applicable | Not Applicable | Lacks a defined pathogenic basis for most disorders. |
| Holobiont (Microbiome Biomarkers) | ~0.77 | Low to Moderate | Provides novel, actionable biological insights where previous models failed. | |
| Graft-versus-Host Disease | Pathogen-Centric | Limited | Limited | Focuses on subsequent infections, not GVHD pathogenesis. |
| Holobiont (Microbiome Biomarkers) | N/A | N/A | Predictive of severity via loss of diversity and pathobiont expansion (e.g., Enterococcus) [3]. |
Key Insights from Comparative Data:
- Holobiont models match or exceed traditional models in intra-cohort validation, with AUCs around 0.77 [4].
- Cross-cohort validation, the gold standard for robustness, reveals the holobiont model's superior generalizability for intestinal diseases (AUC ~0.73) [4].
- For non-intestinal diseases, single-cohort microbiome classifiers perform poorly in cross-cohort validation. However, combined-cohort classifiers, which aggregate data from multiple studies, significantly improve performance, indicating that larger, more diverse datasets are key to robust holobiont-based diagnostics [4].
- The holobiont model provides value beyond diagnosis, offering mechanistic insights and predictive power for disease course and treatment response, as seen in GVHD and Multiple Sclerosis [2] [3].
Experimental Validation: Key Protocols and Workflows
Translating the holobiont theory into actionable diagnostics requires robust experimental protocols. Below are detailed methodologies from seminal studies.
Protocol 1: GWAS of the Plant Holobiont for Disease Resistance
This protocol from a pea root rot study [5] identifies how host genetics shape the microbiome to influence disease resistance.
Table 2: Key Reagents for Plant Holobiont GWAS
| Research Reagent / Solution | Function in Experimental Protocol |
|---|---|
| 252 Diverse Pea Lines | Provides genetic diversity for genome-wide association studies (GWAS). |
| Naturally Infested Soil | Serves as a consistent, complex source of soil-borne pathogens for phenotyping. |
| Genotyping-by-Sequencing (GBS) | A high-throughput method for discovering and genotyping thousands of SNP markers across the pea genome. |
| PacBio (Sequel II) & Illumina MiSeq | Platforms for sequencing the fungal ITS region and bacterial 16S rRNA gene, respectively. |
| UNOISE & DADA2 Pipelines | Bioinformatics tools for error-correcting and clustering sequences into operational taxonomic units (OTUs). |
| Zhongwang 6 Reference Genome | Used for aligning sequence reads and calling genetic variants. |
Experimental Workflow:
- Plant Cultivation and Phenotyping: Grow 252 diverse pea lines in naturally infested soil and sterile control soil under controlled conditions for 21 days. Assess disease symptoms using a Root Rot Index (RRI) and measure shoot dry weight [5].
- Host Genotyping: Extract DNA from one plant per line. Perform Genotyping-by-Sequencing (GBS). Align sequences to a reference genome ("Zhongwang 6") and call Single Nucleotide Polymorphisms (SNPs). Filter for quality, resulting in 18,267 markers [5].
- Microbiome Profiling:
- Fungal Communities: Amplify the entire ITS region from root DNA using ITS1f/ITS4 primers. Sequence on a PacBio Sequel II system. Cluster sequences into OTUs and assign taxonomy using the UNITE database.
- Bacterial Communities: Amplify the V3-V4 regions of the 16S rRNA gene. Sequence on an Illumina MiSeq platform. Call amplicon sequence variants and assign taxonomy using the SILVA database [5].
- Holobiont Genetic Analysis:
- Perform a Genome-Wide Association Study (GWAS) using host SNP markers, with the abundance of microbial OTUs as phenotypic traits.
- Identify Quantitative Trait Loci (QTLs) in the plant genome that are significantly associated with the abundance of specific microbes.
- Use Genomic Prediction models to compare the power of host QTLs versus microbial OTU abundances for predicting root rot resistance [5].
Protocol 2: Validating Microbial Drivers of Neurodevelopment
This protocol [6] demonstrates a bedside-to-bench approach to validate a specific pathobiont's causal role in a neurodevelopmental disorder.
Experimental Workflow:
- Human Cohort Observation: Conduct a pilot clinical study using Fecal Microbiota Transplantation (FMT) in children with Autism Spectrum Disorder (ASD). Observe that a reduction in Clostridium innocuum correlates with clinical improvement [6].
- Bacterial Strain Isolation: Islect C. innocuum strains from both ASD donors and neurotypical (NT) controls.
- Gnotobiotic Animal Modeling:
- Use the BTBR T+ tf/J mouse, an idiopathic ASD model that exhibits social deficits under specific pathogen-free (SPF) conditions but not in the germ-free (GF) state.
- Monocolonize GF BTBR mice with either ASD-derived or NT-derived C. innocuum strains at different developmental windows (gestation, early life, post-weaning, adulthood) [6].
- Phenotypic and Mechanistic Analysis:
- Assess offspring for social behavior (e.g., three-chamber test) and repetitive behaviors.
- Analyze the neonatal brain metabolome (e.g., neurotransmitters, succinate levels).
- Examine microglial morphology and gene expression via immunohistochemistry and RNA sequencing [6].
The Pathobiont Switch: A Core Signaling Pathway
A key mechanistic insight from the holobiont model is the context-dependent functionality of microbes. The same microbe can act as a symbiont or a pathobiont based on the host's internal environment [2].
Table 3: Factors Influencing the Pathobiont Switch
| Factor | Pro-Symbiont Effect | Pro-Pathobiont Effect |
|---|---|---|
| Inflammation | Low, controlled inflammation (e.g., from tissue repair). | High, chronic inflammation creates a selective pressure for pathobionts [2]. |
| Diet | High-fiber, phytoestrogen-rich diets support SCFA-producing symbionts [2]. | Western-style diets can promote pro-inflammatory microbial metabolites. |
| Host Genetics | HLA and other immune alleles that support microbial diversity. | MS-associated HLA alleles linked to dysbiosis and neuroinflammation [2]. |
| Pharmacotherapy | Targeted therapies, pre/probiotics. | Broad-spectrum antibiotics deplete symbionts, allowing pathobiont blooms [3] [1]. |
| Environmental Exposures | Toxicants like glyphosate can induce dysbiosis [2]. |
The Scientist's Toolkit: Essential Research Reagents
Successfully implementing holobiont research requires specific tools and reagents. The following table details essential items derived from the featured experimental protocols.
Table 4: Essential Research Reagent Solutions for Holobiont Studies
| Reagent / Solution | Function & Application |
|---|---|
| Gnotobiotic Mouse Models | Essential for establishing causality. Allows colonization of germ-free animals with defined microbial communities to study their specific functional impact [6]. |
| Human HLA Class II Transgenic Mice | Models to study how human genetic variations (a major risk factor for autoimmune disease) shape the microbiome and immune responses [2]. |
| Defined Microbial Consortia | Mixtures of specific bacterial strains (e.g., 15-strain consortia) used to test synergistic functions and as potential next-generation live biotherapeutics [1]. |
| Fecal Microbiota Transplantation (FMT) | An undefined, complex live biotherapeutic product used to restore a dysbiotic ecosystem to a healthy state in model systems and humans [1] [6]. |
| PacBio Long-Read & Illumina Short-Read Sequencers | Complementary sequencing technologies. PacBio is ideal for full-length 16S/ITS sequencing, while Illumina is suited for shallow-depth, high-throughput studies [5]. |
| 16S rRNA (V3-V4) & ITS Primers | Standard primer sets for amplifying bacterial and fungal genomic regions, respectively, for taxonomic profiling of microbial communities [5]. |
| UNITE & SILVA Databases | Curated reference databases for taxonomic classification of fungal (UNITE) and bacterial (SILVA) amplicon sequences [5]. |
The evidence from cross-cohort validation studies, GWAS of plant and animal holobionts, and mechanistic pathobiont research compellingly argues for a paradigm shift. The holobiont model, which integrates host genetics, microbial ecology, and pathobiont dynamics, provides a more robust framework for understanding disease etiology than the traditional pathogen-centric view.
While challenges remain—particularly in standardizing methodologies and improving cross-cohort generalizability for non-intestinal diseases—the integration of holobiont principles into diagnostic and drug development pipelines is no longer speculative. It is a necessary evolution for addressing the complexity of human disease in the 21st century. The experimental data and protocols outlined in this guide provide a foundation for researchers and drug developers to build upon, paving the way for Microbiome First Medicine and personalized, ecology-based therapeutic interventions [1].
The human microbiome has emerged as a critical modulator of human health and disease, with particular significance in oncology. Among various microbial inhabitants, Fusobacterium nucleatum (F. nucleatum), an anaerobic, Gram-negative bacterium, has transitioned from being regarded solely as an oral commensal to a potential oncobacterium associated with multiple cancer types [7]. Its enrichment in colorectal cancer (CRC) tissues has established it as a key subject in cancer microbiome research, but emerging evidence suggests its influence extends to other malignancies across anatomical boundaries [7]. This review synthesizes current understanding of F. nucleatum's role as a consistent microbial signature in CRC and other cancers, focusing on its pathogenic mechanisms, clinical implications, and potential as a diagnostic and therapeutic target. We objectively compare experimental data across studies and provide detailed methodologies to facilitate research reproducibility and biomarker validation in cohort studies.
Molecular Mechanisms ofFusobacterium nucleatumin Carcinogenesis
Adhesion and Invasion Mechanisms
Fusobacterium nucleatum initiates host-cell interaction through specific adhesins that facilitate attachment and invasion. The FadA adhesin binds directly to E-cadherin on epithelial cells, activating β-catenin signaling and driving oncogenic responses [7]. This interaction promotes cell proliferation and survival, positioning F. nucleatum as an active facilitator of malignant transformation [7]. Additionally, the Fap2 adhesin recognizes Gal-GalNAc overexpressed in colorectal cancer cells, enabling bacterial accumulation in tumor tissues [8]. These molecular interactions provide tropism mechanisms explaining F. nucleatum's enrichment in tumor microenvironments.
Immune Modulation and Inflammation
F. nucleatum significantly shapes the tumor immune microenvironment to favor cancer progression. It activates TLR4 signaling, leading to NF-κB activation and subsequent upregulation of pro-inflammatory cytokines including IL-1β, IL-6, IL-8, IL-17A, and TNF-α [9]. This inflammatory cascade establishes a chronic inflammatory state conducive to tumor growth. Furthermore, F. nucleatum recruits myeloid-derived suppressor cells (MDSCs) and modulates tumor-associated immune populations by suppressing cytotoxic activity to foster an immunosuppressive tumor microenvironment [9]. The bacterium also binds to Siglec-7 receptors on natural killer (NK) cells, thereby suppressing NK cell-mediated cytotoxicity against cancer cells [7].
Metabolic Reprogramming and Treatment Resistance
Recent evidence indicates F. nucleatum induces metabolic changes that promote cancer progression and treatment resistance. The bacterium shifts central carbon metabolism in tumor cells and promotes CRC cell invasion [8]. It also reduces m6A modification in CRC cells, enhancing their invasiveness [8]. Through the establishment of a pro-inflammatory and immunosuppressive tumor microenvironment that promotes metastasis and facilitates DNA damage, F. nucleatum enhances the tumor's susceptibility to the development of chemoresistance [9]. Transcriptomic analyses of F. nucleatum-infected CRC cells reveal activation of multiple chemoresistance-associated pathways, including those driving inflammation, immune evasion, DNA damage, and metastasis [9].
Table 1: Key Virulence Factors of F. nucleatum in Cancer Pathogenesis
| Virulence Factor | Molecular Function | Downstream Effects | Experimental Evidence |
|---|---|---|---|
| FadA adhesin | Binds E-cadherin on host cells | Activates β-catenin signaling; promotes proliferation & invasion | CRC cell culture models [7] |
| Fap2 adhesin | Recognizes Gal-GalNAc on cancer cells | Enhances bacterial tropism to tumors; inhibits immune cell cytotoxicity | Binding assays; immune cell cytotoxicity tests [8] |
| Lipopolysaccharides (LPS) | Activates TLR4 signaling | Induces NF-κB activation; pro-inflammatory cytokine production | TLR4 knockout models; cytokine measurements [9] |
| Metabolic byproducts | Alters host cell metabolism | Shifts central carbon metabolism; promotes invasion | Metabolomic profiling; invasion assays [8] |
3Fusobacterium nucleatumin Colorectal Cancer: Clinical Evidence and Diagnostic Applications
Epidemiological Associations and Distribution Patterns
Substantial clinical evidence establishes F. nucleatum's association with colorectal cancer pathogenesis. The abundance of F. nucleatum is generally elevated in feces and cancer tissues from CRC patients, with higher prevalence in right-sided colon cancers (proximal colon > distal colon > rectum) [10]. This distribution may reflect nutritional and environmental preferences of F. nucleatum in the gut [10]. Importantly, F. nucleatum enrichment is already observed in precursor lesions before malignant transformation, including adenomas and serrated polyps, suggesting potential involvement in early carcinogenesis [10].
Longitudinal studies demonstrate that F. nucleatum experience severely abrogates intra-personal stability of microbiome in IBD patients and induces highly variable gut microbiome between subjects [11]. Microbial classifier biomarkers associated with F. nucleatum detection successfully predict microbial alterations in both IBD and non-IBD conditions, providing a novel aspect of microbial homeostasis/dynamics [11].
Diagnostic and Prognostic Performance
F. nucleatum detection shows promising performance as a non-invasive biomarker for CRC screening and prognosis. Cohort studies demonstrate its diagnostic performance with area under the curve (AUC) values of 0.82–0.89 [8]. Importantly, F. nucleatum abundance correlates with advanced disease stage (stage III/IV OR = 2.87), lymph node metastasis (HR = 1.94), and reduced 5-year survival rates (35% vs. 62%) [8]. Metagenomic analysis reveals that high F. nucleatum abundance is closely related to TNM staging (C-index 0.81 vs. 0.69) and recurrence risk (AUC = 0.88) [8]. Notably, a nomogram model integrating F. nucleatum biomarkers improves the predictive accuracy of the traditional TNM staging system by 17.3% [8].
Table 2: Clinical Performance of F. nucleatum as a Biomarker in Colorectal Cancer
| Parameter | Performance Metrics | Study Details | Clinical Implications |
|---|---|---|---|
| Diagnostic Accuracy | AUC 0.82–0.89 | Cohort studies of fecal samples | Non-invasive screening potential |
| Disease Staging | Stage III/IV OR = 2.87 | Meta-analysis of tissue and fecal samples | Identifies advanced disease |
| Lymph Node Metastasis | HR = 1.94 | Tissue-based studies | Predicts aggressive behavior |
| Survival Impact | 5-year survival: 35% vs. 62% (high vs. low Fn) | Longitudinal cohort | Prognostic stratification |
| TNM Staging Enhancement | +17.3% accuracy with nomogram | Model integration studies | Improves current staging systems |
Consistency Across Age Groups
Recent evidence confirms that F. nucleatum associations with CRC remain consistent across different age groups, including young-onset colorectal cancer (yCRC). Deep metagenomic sequencing of stool samples from both old-onset CRC (oCRC) and yCRC patients reveals similar strain-level patterns of F. nucleatum, Bacteroides fragilis, and Escherichia coli [12]. Importantly, CRC-associated virulence factors (fadA, bft) are enriched in both oCRC and yCRC compared to their respective controls [12]. Microbiome-based classification models show similar prediction accuracy for CRC status in old- and young-onset patients, underscoring the consistency of microbial signatures across different age groups [12].
4Fusobacterium nucleatumin Extracolonic Cancers
Beyond colorectal cancer, F. nucleatum has been detected and implicated in the pathogenesis of various other malignancies. Its enrichment in oral squamous cell carcinoma (OSCC) tissues has been demonstrated through multiple studies, though detection rates vary [7]. In OSCC, F. nucleatum exhibits strong adherence to and invasion of human gingival epithelial cells, activating the NF-κB pathway, disrupting epithelial adhesion, and promoting epithelial-mesenchymal transition (EMT) [7]. The detection of F. nucleatum correlates with clinicopathological parameters, including tumor size and stage, suggesting potential influence on disease progression [7].
F. nucleatum's role also extends to interactions with human papillomavirus (HPV), particularly in head and neck cancers, suggesting potential synergistic effects in carcinogenesis [7]. Emerging evidence also associates Fusobacterium with pancreatic, esophageal, and gastric cancers, though mechanisms in these malignancies are less characterized [7] [9]. The bacterium's capacity to traverse anatomical boundaries and colonize distant sites underscores its potential systemic impact in cancer development.
Experimental Models and Research Methodologies
Standardized Co-culture Protocols for In Vitro Studies
Transcriptomic analyses of F. nucleatum interactions with CRC cells typically employ standardized co-culture systems. The general protocol involves infection of CRC cell lines (such as HCT116, HT29, or SW480) with F. nucleatum at multiplicities of infection (MOI) ranging from 100:1 to 500:1 (bacteria to eukaryotic cells) under anaerobic conditions [9]. Co-cultures are maintained for varying timepoints (typically 4-24 hours) before RNA extraction and transcriptomic analysis. These studies consistently reveal that F. nucleatum activates multiple chemoresistance-associated pathways, including those driving inflammation, immune evasion, DNA damage, and metastasis [9].
A meta-analysis of public transcriptomic datasets identified consistent patterns across multiple independent co-culture experiments, strengthening the biological relevance of findings [9]. This approach reduces noise and increases confidence in identifying genes consistently altered by F. nucleatum exposure across different experimental conditions.
Metagenomic Sequencing and Analysis Pipelines
For clinical correlation studies, shotgun metagenomic sequencing of stool or tissue samples represents the gold standard for F. nucleatum detection and quantification. The typical workflow includes:
- DNA Extraction: Using standardized kits with mechanical lysis to ensure Gram-positive and Gram-negative bacteria are equally represented [12]
- Library Preparation: Utilizing Illumina-compatible protocols with appropriate fragment sizes [12]
- Sequencing: Achieving sufficient depth (typically 70 million paired-end reads per sample) to detect low-abundance taxa [12]
- Bioinformatic Analysis:
This methodology allows for comprehensive assessment of F. nucleatum abundance while simultaneously evaluating the broader microbial context and functional potential.
Signaling Pathways and Host-Pathogen Interactions
The following diagram illustrates key molecular pathways through which F. nucleatum promotes colorectal carcinogenesis, based on transcriptomic analyses of infected host cells:
Figure 1: Molecular Pathways of F. nucleatum in Colorectal Cancer
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents and Methodologies for F. nucleatum Research
| Category | Specific Items/Protocols | Application/Purpose | Technical Notes |
|---|---|---|---|
| Bacterial Strains | F. nucleatum subspecies (animalis, nucleatum, vincentii, polymorphum) | Pathogenesis comparisons | Subspecies show different prevalence in CRC [10] |
| Cell Culture Models | CRC cell lines (HCT116, HT29, SW480); Oral epithelial cells | Host-pathogen interaction studies | Use anaerobic co-culture systems [9] |
| Molecular Reagents | Anti-FadA antibodies; E-cadherin expression constructs; TLR4 inhibitors | Mechanistic pathway validation | Blocking experiments establish causality [7] |
| Animal Models | ApcMin/+ mice; AOM/DSS colitis model; Germ-free mice | In vivo carcinogenesis studies | F. nucleatum alone insufficient for tumorigenesis [10] |
| Omics Technologies | Shotgun metagenomics; RNA-seq; Metabolomics platforms | Comprehensive profiling | Enables strain-level and functional analysis [12] |
| Bioinformatics Tools | MetaPhlAn2; DESeq2; Ingenuity Pathway Analysis | Data analysis and interpretation | Identifies enriched pathways and networks [9] |
The consistent demonstration of Fusobacterium nucleatum as a microbial signature across colorectal cancers and other malignancies underscores its potential significance as a diagnostic biomarker and therapeutic target. Evidence from multiple independent cohorts confirms its association with disease progression, treatment resistance, and poor clinical outcomes. The consistency of these findings across different age groups and geographical populations strengthens the case for its clinical relevance.
However, important challenges remain in translating these findings to clinical practice. Standardized detection protocols, validated threshold values, and defined targeted intervention strategies require further development and validation through multi-center prospective studies [8]. Future research should focus on elucidating the precise mechanisms underlying F. nucleatum's tropism for tumor tissues, its role in the oral-gut axis, and its interactions with other microbial community members in carcinogenesis. Therapeutic approaches targeting F. nucleatum, including antibiotic therapies, phage therapy, and immunomodulatory strategies, represent promising avenues for improving outcomes in F. nucleatum-associated malignancies.
As microbiome research continues to evolve, F. nucleatum serves as a paradigm for understanding how specific microbial constituents can influence cancer biology across traditional organ boundaries. The integration of microbial biomarkers into existing diagnostic and prognostic frameworks holds potential for enhancing precision oncology approaches and ultimately improving patient outcomes.
The human microbiome, a complex ecosystem of bacteria, fungi, and viruses, plays a critical role in maintaining health, and its disruption—termed dysbiosis—is a hallmark of numerous diseases. Advances in high-throughput sequencing and multi-omics technologies are rapidly uncovering specific microbial signatures associated with a spectrum of disorders, from gastrointestinal and respiratory conditions to metabolic diseases. These microbial biomarkers offer immense potential for revolutionizing diagnostic precision, prognostic stratification, and the development of novel therapeutics. This comparison guide objectively evaluates the experimental data and microbial landscapes linked to Crohn's disease, pancreatic cancer, peri-implantitis, and respiratory diseases, framing the findings within the context of biomarker validation for clinical translation. The supporting data, derived from rigorous cohort studies, are synthesized to provide researchers and drug development professionals with a clear overview of the current landscape and methodological standards.
Comparative Analysis of Disease-Associated Microbial Biomarkers
Table 1: Key Microbial Biomarkers and Their Diagnostic Performance Across Diseases
| Disease | Key Associated Microbial Taxa/Signatures | Proposed Functional Mechanisms | Reported Diagnostic Performance (AUC) | Sample Type |
|---|---|---|---|---|
| Crohn's Disease (CD) [13] | Panel of 20 species (e.g., Adherent-Invasive E. coli); Depletion of butyrate-producing species | AIEC virulence (adherence, invasion); Depletion of anti-inflammatory SCFAs like butyrate; Disrupted microbial fermentation pathways | 0.94 (External Validation) [13] | Fecal Samples |
| Pancreatic Cancer [14] | Porphyromonas gingivalis, Fusobacterium nucleatum, Aggregatibacter actinomycetemcomitans | Promotion of chronic inflammation; Immune modulation; Production of genotoxic metabolites; Bacterial translocation | DOR*: 4.85 (Single microbiome); 16.33 (Multiple microbiomes) [14] | Saliva / Oral Samples |
| Peri-implantitis [15] | Health: Streptococcus, Rothia; Disease: Prevotella, Porphyromonas, Treponema, Fusobacteria | Shift from aerotolerant Gram-positive to anaerobic Gram-negative bacteria; Increased amino acid metabolism producing pro-inflammatory metabolites | 0.85 (Integrated taxonomic & functional data) [15] | Peri-implant Biofilm |
| Respiratory Diseases (COPD, Asthma) [16] [17] | Gut/Lung Dysbiosis; Increased Proteobacteria (e.g., Haemophilus); Altered SCFA production | Immune dysregulation via gut-lung axis; Altered levels of circulating SCFAs (butyrate, acetate) affecting pulmonary immunity | Data primarily from pre-clinical and association studies [16] [17] | Fecal, BALF, and Lung Tissue |
DOR: Diagnostic Odds Ratio | *BALF: Bronchoalveolar Lavage Fluid*
Detailed Experimental Protocols for Biomarker Discovery
The identification of robust microbial biomarkers relies on standardized, multi-faceted experimental protocols. The methodologies below are representative of those used in high-quality validation cohort studies.
Sample Collection and Preparation
- Sample Acquisition: Procedures are body-site-specific. For gut microbiome studies, fecal samples are collected and immediately frozen at -80°C to preserve microbial integrity [13]. For oral/oro-pharyngeal microbiomes, saliva or mucosal swabs are used [14]. For respiratory studies, bronchoalveolar lavage (BALF) is collected with protective techniques to avoid upper airway contamination [18]. Peri-implantitis studies use customized protocols to co-isolate biofilm from implant surfaces [15].
- Nucleic Acid Extraction: DNA is extracted for metagenomic and 16S rRNA sequencing using kits designed for complex biological samples (e.g., Qiagen, Mo Bio Powersoil) [15] [13]. For metatranscriptomics, total RNA is extracted, followed by ribosomal RNA (rRNA) depletion to enrich for messenger RNA (mRNA) [13].
- Metabolite Extraction: For metabolomics, fecal samples are homogenized in phosphate buffer, and metabolites are extracted using mechanical disruption with zirconia/silica beads. The supernatant is filtered and prepared for analysis, such as by Nuclear Magnetic Resonance (NMR) spectroscopy [13].
Multi-Omics Data Generation and Analysis
- Shotgun Metagenomics: Extracted DNA is sequenced on platforms like Illumina HiSeq. Taxonomic profiling is performed using tools like MetaPhlAn v4, which leverages unique clade-specific marker genes. Functional potential is assessed by mapping reads to databases like UniRef90 using HUMAnN v3 [13].
- Metatranscriptomics: Sequencing libraries are prepared from rRNA-depleted RNA and sequenced. The resulting reads are mapped to custom genomic reference databases to quantify gene expression levels, revealing actively transcribed pathways and virulence factors [15] [13].
- Metabolomics: Processed samples are analyzed via NMR or Mass Spectrometry. Spectral data are referenced against compound libraries (e.g., Chenomx) for metabolite identification and quantification [13].
- Data Integration: Machine learning algorithms (e.g., Canonical Analysis of Principal Coordinates, random forests) are employed to integrate taxonomic, functional, and metabolite data to build predictive models and identify the most robust diagnostic biomarkers [15] [13].
Visualization of Research Workflows and Pathways
Multi-Omics Biomarker Discovery Pipeline
The following diagram illustrates the integrated workflow from sample collection to biomarker validation, a process common to the cited studies.
The Gut-Lung Axis Immune Pathway
This diagram outlines the key mechanistic pathway by which gut microbiota influence respiratory health, a core concept in understanding diseases like asthma and COPD [16] [17].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Reagents and Platforms for Microbial Biomarker Research
| Item/Category | Specific Examples | Function in Research Workflow |
|---|---|---|
| Nucleic Acid Extraction Kits | RNeasy Mini Kit (Qiagen); Powersoil Pro Kit (Qiagen) | High-quality DNA/RNA isolation from complex samples like stool and biofilm. |
| rRNA Depletion Kits | Ribo-zero Magnetic Kit | Removal of ribosomal RNA to enrich for messenger RNA in metatranscriptomic studies. |
| Sequencing Platforms | Illumina HiSeq/NovaSeq; PacBio Sequel | High-throughput sequencing for metagenomics and transcriptomics. |
| Bioinformatic Software | KneadData, MetaPhlAn v4, HUMAnN v3, Bowtie2 | Quality control, taxonomic profiling, functional pathway analysis, and read mapping. |
| Reference Databases | UniRef90, Virulence Factor Database (VFDB), NCBI Taxonomy | Functional gene annotation, virulence factor identification, and taxonomic classification. |
| Metabolomics Platforms | Bruker NMR Spectrometer; LC-MS Systems | Untargeted identification and quantification of microbial and host metabolites. |
| Machine Learning Frameworks | R, Python (scikit-learn) | Data integration and building predictive models from multi-omics data. |
The consistent emergence of specific microbial signatures across gastrointestinal, respiratory, and metabolic disorders underscores the microbiome's central role in human pathophysiology. The experimental data synthesized in this guide demonstrate that validated, multi-species biomarker panels can achieve high diagnostic accuracy, as seen in Crohn's disease and peri-implantitis. Furthermore, moving beyond taxonomy to include functional metatranscriptomic and metabolomic data significantly enhances predictive power and provides mechanistic insights.
Future research must focus on standardizing methodologies across larger, multi-center cohorts to facilitate clinical adoption. Longitudinal studies are needed to determine whether microbial shifts are causes or consequences of disease, which is critical for developing targeted microbial therapies like next-generation probiotics or dietary interventions. For drug development professionals, the microbiome presents a novel frontier for therapeutic innovation, offering strategies to modulate these complex ecological landscapes to treat and prevent a wide array of chronic diseases.
The human microbiome represents one of the most promising yet challenging frontiers in modern biomedical research. While numerous studies have identified associations between microbial communities and various disease states, a fundamental question persists: are observed microbiome alterations a cause or consequence of disease? This "chicken-or-egg" dilemma represents the central challenge in translating microbiome research into validated diagnostic tools and targeted therapies [19] [20]. Establishing causality is not merely an academic exercise—it is essential for identifying genuine therapeutic targets, developing reliable biomarkers, and creating effective microbiome-based interventions [21] [22].
The field is currently transitioning from observational studies to mechanistic research that can demonstrate causal relationships. This evolution requires sophisticated experimental frameworks that integrate multi-omics technologies, advanced preclinical models, and rigorous computational approaches [23] [21]. This guide examines the key methodologies, experimental models, and analytical tools enabling researchers to dissect causal relationships in microbiome-disease interactions, with particular emphasis on validation approaches suitable for diagnostic development.
Experimental Frameworks for Establishing Causality
The Sequential Evidence Funnel
Establishing microbiome-disease causality typically follows a systematic investigative progression, often described as an "evidence funnel" that moves from association to mechanism [22]. This framework provides a logical structure for building conclusive evidence and is particularly valuable for designing validation cohort studies.
Table 1: The Five-Level Evidence Funnel for Establishing Microbiome-Disease Causality
| Evidence Level | Experimental Approach | Key Insights Provided | Causal Inference Strength |
|---|---|---|---|
| Level 1: Association | Microbiome-wide association studies (MWAS) | Identifies microbial taxa/genes correlated with disease states | Weak - identifies correlations only |
| Level 2: Altered Phenotypes | Germ-free animals; antibiotic-treated models | Demonstrates phenotype changes with microbiome depletion | Moderate - shows microbiome involvement |
| Level 3: Phenotype Transfer | Fecal microbiota transplantation (FMT) | Transfers disease phenotype via microbiome transfer | Strong - demonstrates transferability |
| Level 4: Strain Isolation | Mono-association or defined consortia in gnotobiotic models | Identifies specific strains responsible for phenotypes | Very strong - pinpoints causative strains |
| Level 5: Molecular Mechanism | Metabolomics; genetic manipulation; receptor studies | Identifies specific molecules and mechanisms | Definitive - elucidates molecular pathways |
This funnel approach provides a systematic methodology for progressing from initial observations to mechanistic understanding. Research in obesity and metabolic disorders exemplifies this strategy, where initial observations of altered Firmicutes/Bacteroidetes ratios in obese individuals (Level 1) progressed through germ-free mouse experiments (Level 2), FMT studies (Level 3), and ultimately to the identification of specific bacterial strains and metabolites like short-chain fatty acids that directly influence host metabolism (Levels 4-5) [19] [22].
Methodological Framework for Causal Inference
The following diagram illustrates the integrated experimental workflow for establishing causality, from initial correlation to molecular mechanism:
Key Experimental Models & Methodologies
Animal Models for Causal Inference
Animal models remain indispensable for establishing causal relationships in microbiome research, with each model system offering distinct advantages and limitations for different research questions.
Table 2: Animal Models for Establishing Microbiome-Disease Causality
| Model System | Key Features | Best Applications | Limitations |
|---|---|---|---|
| Germ-free mice | No native microbiota; allows controlled colonization | Gold standard for FMT studies; mono-association experiments | Altered immune development; costly maintenance |
| Gnotobiotic models | Defined microbial communities | Studying specific microbial interactions; synthetic communities | Limited complexity; may not reflect native microbiota |
| Antibiotic-depleted mice | Microbiome reduction in conventional animals | Rapid assessment of microbiome involvement; adult-stage depletion | Incomplete depletion; off-target drug effects |
| Humanized mice | Human microbiome transplanted into germ-free mice | Studying human-specific microbiome functions | Limited host-microbe co-adaptation; genetic mismatch |
| Zebrafish | Optical transparency; high-throughput screening | Real-time visualization of host-microbe interactions | Physiological differences from mammals |
| Drosophila/C. elegans | Simple microbiota; genetic tractability | High-throughput screening; genetic studies | Limited translational relevance for complex diseases |
| Pigs | Physiological similarity to humans; similar organ size | Nutritional studies; translational research | Cost; limited genetic tools |
The selection of appropriate animal models depends heavily on the research question. For initial phenotype transfer studies, germ-free mice represent the benchmark model, while more complex questions may require humanized models or systems with greater physiological relevance to humans [23] [21]. Recent consensus statements emphasize that no single model is perfect, and combining multiple approaches often provides the most robust evidence for causality [21].
Fecal Microbiota Transplantation Protocols
FMT represents a crucial experimental approach for Level 3 evidence in the causality funnel, enabling researchers to determine whether a disease phenotype can be transferred through microbial communities alone [23] [22]. Standardized protocols are essential for generating reproducible, interpretable results.
Donor-Recipient Protocol Framework:
- Donor Selection & Characterization: Comprehensive screening of donor microbiome (16S rRNA sequencing, metagenomics), health status, and relevant phenotypic traits
- Inoculum Preparation: Fresh or cryopreserved fecal material (typically 80-100 mg/mL in sterile PBS with glycerol cryoprotectant) processed anaerobically
- Recipient Preparation: Germ-free animals preferred; antibiotic-depleted (ampicillin, vancomycin, neomycin, metronidazole for 2-3 weeks) or PEG-treated conventional animals as alternatives
- Transplantation Route & Schedule: Oral gavage (100-200μL) once daily for 3-5 consecutive days to ensure stable engraftment
- Phenotypic Assessment: Monitor disease-relevant parameters at predetermined endpoints (typically 2-8 weeks post-transplantation)
This approach has successfully transferred numerous phenotypes, including obesity, inflammatory bowel disease, and behavioral traits, providing compelling evidence for microbial involvement in these conditions [23] [22]. The consistency of phenotype transfer across multiple independent studies significantly strengthens causal inference.
Advanced Analytical Approaches
Multi-Omics Integration for Mechanistic Insights
The integration of multiple omics technologies is essential for progressing through the causality funnel, particularly for identifying molecular mechanisms (Level 5 evidence). Advanced computational methods now enable researchers to connect microbial features to host responses through systematic bioinformatic pipelines.
Table 3: Multi-Omics Technologies for Microbiome Causal Inference
| Technology | Data Type | Applications in Causality | Key Limitations |
|---|---|---|---|
| Shotgun Metagenomics | Microbial genetic potential | Identifying functional capabilities; strain tracking | Does not measure activity; database dependencies |
| Metatranscriptomics | Microbial gene expression | Assessing active microbial functions; regulation studies | Technical variability; host RNA contamination |
| Metabolomics | Microbial metabolite production | Direct measurement of functional output; host-microbe communication | Cannot always trace metabolites to producers |
| Proteomics | Microbial and host protein expression | Direct functional data; host response measurement | Technical complexity; limited dynamic range |
| Metagenome-wide Association Studies (MWAS) | Variant association with phenotype | Linking specific microbial genes to host traits | Population stratification; requires large cohorts |
| Artificial Intelligence/Machine Learning | Integrated multi-omics data | Pattern recognition; predictive modeling; biomarker discovery | "Black box" limitations; overfitting risks |
The power of multi-omics integration is exemplified in recent research on myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), where researchers combined gut metagenomics, plasma metabolomics, immune cell profiling, and clinical symptoms using a deep neural network (BioMapAI). This approach achieved 90% accuracy in distinguishing patients from controls and identified specific disruptions in butyrate production and tryptophan metabolism, providing compelling evidence for microbial involvement in this condition [24].
Computational & Statistical Methods for Causal Inference
Several specialized computational approaches have been developed specifically to address causal inference in microbiome research:
Mechanistic Modeling: Ecosystem-level models that incorporate microbial interactions, metabolic networks, and host responses to test causal hypotheses in silico [20].
Mendelian Randomization: Uses genetic variants as instrumental variables to strengthen causal inference in human observational studies, helping to overcome confounding factors [23].
Microbiome Engineering Approaches: CRISPR-based editing of microbial genomes allows direct testing of gene-specific effects on host phenotypes, providing powerful evidence for causal mechanisms [25].
The Scientist's Toolkit: Essential Research Reagents & Platforms
Table 4: Essential Research Reagents and Platforms for Causality Studies
| Reagent/Platform | Function | Key Applications |
|---|---|---|
| Gnotobiotic isolators | Maintain germ-free or defined microbiota animals | FMT studies; mono-association experiments |
| Cryopreservation media | Preserve microbial communities viability | Banking standardized microbiota inocula |
| Anaerobic chambers | Maintain oxygen-free conditions for strict anaerobes | Culturing fastidious microorganisms |
| 16S rRNA sequencing kits | Characterize microbial community composition | Initial community profiling; diversity assessment |
| Shotgun metagenomics kits | Assess functional genetic potential of communities | Strain-level analysis; gene content assessment |
| Metabolomics platforms | Measure microbial and host metabolites | Functional output assessment; metabolic pathways |
| Organ-on-a-chip systems | Model human organ systems with microbiome | Human-relevant host-microbe interaction studies |
| BioMapAI | Deep neural network for multi-omics integration | Identifying biomarkers across data types [24] |
| ProBiome | Biostatistical framework for microbiome analysis | Standardized analytical pipelines [20] |
| CRISPR-Cas systems | Precise microbial genome editing | Functional validation of microbial genes [25] |
Signaling Pathways in Microbiome-Host Communication
Understanding the molecular mechanisms through which the microbiome influences host physiology requires mapping the specific signaling pathways involved. The following diagram illustrates key established pathways in microbiome-host communication:
Validation Cohort Design & Biomarker Translation
For diagnostic development, rigorous validation cohort design is essential to move from correlative biomarkers to clinically useful tools. Key considerations include:
Prospective Cohort Design: Collecting samples prior to disease development enables true assessment of predictive value rather than mere association.
Multi-center Recruitment: Including diverse populations and geographic locations controls for cohort-specific biases and improves generalizability.
Longitudinal Sampling: Repeated measurements over time help distinguish cause from consequence by establishing temporal relationships.
Integrated Omics Platforms: Combining metagenomics, metabolomics, and host response markers increases predictive power and mechanistic insight, as demonstrated in the ME/CFS research that achieved 90% diagnostic accuracy [24].
Experimental Validation: Correlative findings from human studies should be tested in animal models or in vitro systems to establish causal relationships before diagnostic implementation.
The field is moving toward standardized biomarker validation pipelines that incorporate these elements, with recent consensus statements emphasizing the need for robust methodological standards and interdisciplinary collaboration [21].
Resolving the "chicken-or-egg" dilemma in microbiome-disease relationships requires methodical progression through sequential evidence levels, from initial correlation to molecular mechanism. The experimental frameworks and methodologies outlined in this guide provide a roadmap for researchers seeking to establish causality and develop validated microbiome-based diagnostics and therapies. As the field advances, the integration of multi-omics technologies, sophisticated animal models, and computational approaches will continue to enhance our ability to distinguish causal drivers from secondary consequences, ultimately enabling more targeted and effective microbiome-based interventions.
The human gastrointestinal tract hosts a complex ecosystem of trillions of microorganisms, collectively known as the gut microbiome, which engages in continuous bidirectional communication with distant organs through intricate networks termed "axes" [26]. These include the well-established gut-brain axis [27] [28] and other gut-organ pathways that collectively influence nearly every aspect of human physiology. The vast genetic and metabolic potential of the gut microbiome—encoding approximately 150 times more genes than the human genome—underpins its ubiquity in health maintenance, development, aging, and disease [27]. Emerging research underscores that local microbial dysbiosis (an imbalance in the gut microbial community) does not remain confined to the gastrointestinal tract but exerts systemic effects contributing to the pathophysiology of conditions ranging from neurodegenerative diseases to neurodevelopmental disorders, chronic fatigue, and metabolic conditions [29] [30] [24]. This review synthesizes current evidence on these gut-organ axes, with a specific focus on validating microbiome-derived biomarkers for diagnostic applications and exploring therapeutic implications within precision medicine frameworks.
Key Communication Pathways of the Gut-Organ Axes
The gut microbiome communicates with distant organs through multiple, interdependent signaling pathways. These mechanisms form the foundation for understanding how local dysbiosis can have systemic consequences.
Neural Pathways
The vagus nerve serves as a direct neural highway between the gut and the brain, providing rapid communication that influences mood, appetite, and parasympathetic output [29]. Vagal afferents detect mechanical stretch, nutrients, and microbial molecules in the gut, while efferent fibers carry brain commands back to influence gastrointestinal activity [29]. The significance of this pathway is highlighted by research showing that individuals who underwent vagotomy (surgical cutting of the vagus nerve) have a lower subsequent risk of developing Parkinson's disease, suggesting this pathway may facilitate the transmission of disease-provoking agents [29] [28]. Beyond the vagus nerve, the enteric nervous system (ENS)—sometimes called the "second brain"—contains over 100 million neurons that regulate gut motility, secretion, and blood flow [29] [28]. This extensive neural network can operate independently but maintains constant communication with the central nervous system.
Immune and Inflammatory Pathways
Gut microbes profoundly shape host immunity from development through adulthood [31] [29]. The gut-associated lymphoid tissue (GALT) represents the body's largest immune compartment, continuously sampling microbial antigens and coordinating appropriate responses [29]. Specific microbial groups drive the differentiation of distinct immune cell populations; for instance, segmented filamentous bacteria promote pro-inflammatory Th17 cells, while Clostridium species foster anti-inflammatory regulatory T cells (Tregs) [31]. Microbial-associated molecular patterns (MAMPs), such as lipopolysaccharide (LPS) from Gram-negative bacteria, can breach a compromised intestinal barrier, enter circulation, and trigger systemic inflammation, including neuroinflammation, by activating Toll-like receptors (TLRs) in peripheral tissues and the brain [29] [26]. This immune-mediated communication creates a vicious cycle wherein brain disorders are not confined to the CNS but involve a systemic network including the gut ecosystem [29].
Endocrine and Metabolic Pathways
Gut microbes produce and modulate a vast array of neuroactive and systemically active molecules. Short-chain fatty acids (SCFAs)—including acetate, propionate, and butyrate—are produced by microbial fermentation of dietary fiber and serve as crucial regulators of innate and adaptive immunity [31] [29]. SCFAs interact with G protein-coupled receptors (GPCRs) and act as histone deacetylase (HDAC) inhibitors to modulate inflammatory responses and influence T-cell differentiation [31]. Additionally, gut microbiota produce or influence the production of various neurotransmitters, including serotonin (5-HT), dopamine, and γ-aminobutyric acid (GABA) [32] [27]. Notably, approximately 90% of the body's serotonin is produced in the gut, where it influences motility and also communicates with the brain via the vagus nerve [32] [28]. Other crucial metabolites include bile acid derivatives and tryptophan metabolites, which can cross the blood-brain barrier (BBB) and influence CNS function [32] [29].
Figure 1: Key Communication Pathways of the Gut-Organ Axes. The gut microbiome communicates with distant organs through neural, immune, metabolic, and endocrine pathways, transmitting specific microbial signals that influence systemic physiology [31] [29] [27].
Disease-Specific Microbial Dysbiosis and Systemic Implications
Local alterations in gut microbial composition have been consistently associated with a spectrum of diseases across organ systems. The tables below summarize key dysbiosis signatures and their systemic implications across different disease categories.
Table 1: Microbial Dysbiosis Signatures in Neurological and Neuropsychiatric Conditions
| Disease/Condition | Consistent Microbial Alterations | Key Associated Metabolite Changes | Proposed Systemic Mechanisms |
|---|---|---|---|
| Parkinson's Disease (PD) | Increase: Lactobacillus, Akkermansia, Bifidobacterium; Decrease: Lachnospiraceae, Faecalibacterium [32] | Reduced SCFAs; Altered bile acid metabolism [29] | Vagus nerve transmission of α-synuclein pathology; neuroinflammation via microglial activation; intestinal barrier dysfunction [29] [28] |
| Alzheimer's Disease (AD) | Distinct profiles vs. healthy controls; Specific taxa implicated in preclinical AD [29] [27] | Altered SCFA patterns; Inflammatory microbial metabolites [29] | Compromised blood-brain barrier; microglial dysfunction (impaired Aβ clearance); systemic inflammation promoting neuroinflammation [27] |
| Autism Spectrum Disorder (ASD) | Lower microbial diversity; Depletion of beneficial taxa [30] | Altered SCFA profiles; disrupted tryptophan metabolism [30] | Immune activation; increased intestinal permeability ("leaky gut"); neuroimmune signaling; production of neuroactive metabolites [30] |
| Major Depressive Disorder | Gut-brain module analysis reveals distinct neuroactive potential [33] | Serotonin pathway disruption; inflammatory mediators [32] [24] | Vagal pathway modulation; HPA axis dysregulation; systemic inflammation affecting mood centers [26] |
| Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome (ME/CFS) | Microbial imbalance with elevated tryptophan, benzoate [24] | Lower butyrate; nutrient deficiencies; heightened inflammatory responses [24] | Disrupted microbiome-metabolite-immune interactions linked to fatigue, pain, sleep, and emotional symptoms [24] |
Table 2: Microbial Dysbiosis Signatures in Non-Neurological Conditions
| Disease/Condition | Consistent Microbial Alterations | Key Associated Metabolite Changes | Proposed Systemic Mechanisms |
|---|---|---|---|
| Inflammatory Bowel Disease (IBD) | Alterations in underreported species: Asaccharobacter celatus, Gemmiger formicilis, Erysipelatoclostridium ramosum [34] | Significant metabolite shifts: amino acids, TCA-cycle intermediates, acylcarnitines [34] | Perturbed microbial pathways and functions tied to inflammation; compromised mucosal immune homeostasis [31] [34] |
| Type 2 Diabetes (T2D) | Distinct enterotypes associated with disease progression [34] | 111 gut microbiota-derived metabolites significantly associated with T2D, particularly in BCAA, aromatic AA, and lipid pathways [34] | Microbial regulation of glucose homeostasis; insulin resistance through inflammatory mediators; energy harvest modulation [34] |
| Colorectal Cancer (CRC) | Elevated Bacteroides fragilis and other CRC-associated taxa [34] | Oncometabolites; decreased protective SCFAs [34] | Chronic inflammation; direct microbial genotoxicity; modulation of cellular proliferation/apoptosis [34] |
| Non-Alcoholic Fatty Liver Disease (NAFLD) | Specific dysbiosis signatures identified [32] | Altered bile acid metabolism; increased inflammatory mediators [32] | Bacterial translocation; endotoxin-induced inflammation; metabolic endotoxemia driving hepatic steatosis [32] |
Diagnostic Validation: From Microbiome Biomarkers to Clinical Applications
The translation of microbiome science into clinical practice relies on robust biomarker discovery and validation. Metagenomic sequencing has emerged as a cornerstone for precision diagnostics, enabling culture-independent pathogen detection and microbiome-based disease stratification [34].
Metagenomic Approaches and Analytical Frameworks
Shotgun metagenomic sequencing allows comprehensive profiling of microbial communities with unprecedented resolution [34]. The analytical workflow typically involves sample collection (often stool), DNA extraction, library preparation, high-throughput sequencing, bioinformatic processing (quality control, taxonomic profiling, functional annotation), and statistical integration with clinical metadata [34]. Key considerations for validation studies include:
- Standardization: Implementing standardized protocols (e.g., STORMS checklist) and reference materials (e.g., NIST stool reference) to reduce technical variability [34].
- Multi-omics Integration: Combining metagenomics with metabolomics, proteomics, and immunoprofilng to capture functional interactions [34] [24].
- Longitudinal Design: Tracking microbiome dynamics over time to establish temporal relationships and causal inference [30] [34].
- Machine Learning: Applying computational models to identify predictive microbial signatures and build diagnostic classifiers [34] [24].
Figure 2: Diagnostic Validation Workflow for Microbiome Biomarkers. The pathway from sample collection to validated biomarker panel involves multiple analytical stages, with integration of multi-omics data and clinical metadata to ensure robust biomarker performance [34] [24].
Clinically Validated Biomarker Performance
Several microbiome-based diagnostic models have demonstrated promising performance in clinical validation studies:
- Inflammatory Bowel Disease (IBD): Diagnostic models built on integrated microbiome-metabolome signatures achieved high accuracy (AUROC 0.92-0.98) in distinguishing IBD from controls across 13 cohorts [34].
- Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): The BioMapAI platform, integrating gut metagenomics, plasma metabolomics, immune cell profiles, and clinical symptoms, achieved 90% accuracy in distinguishing individuals with ME/CFS from healthy controls [24].
- Colorectal Cancer (CRC): A novel machine learning framework integrating metagenomic data with clinical parameters demonstrated superior accuracy in predicting CRC risk compared to existing methods [34].
- Type 2 Diabetes (T2D): Diagnostic panels generated from gut microbiota-derived metabolites achieved AUROC exceeding 0.80 for predicting disease progression [34].
These validation studies highlight the translational potential of microbiome-based diagnostics while underscoring the importance of multi-center cohorts, diverse population representation, and rigorous analytical standards [34].
Experimental Models and Methodologies for Gut-Organ Axis Research
Key Experimental Protocols
Research into gut-organ axes employs complementary experimental approaches spanning reductionist models to human studies:
Germ-Free (GF) Animal Models
- Protocol: Animals raised in sterile isolators with no exposure to microorganisms; can be colonized with specific microbial communities at defined timepoints [31] [30].
- Applications: Establishing causal roles of microbiota in neurodevelopment, immune function, and behavior; GF mice exhibit significant immune deficiencies, altered stress responses, and neurochemical abnormalities [31] [26] [30].
- Limitations: Artificial conditions; developmental compensation; limited translational relevance to complex human ecosystems [30].
Fecal Microbiota Transplantation (FMT)
- Protocol: Transfer of processed stool material from donor to recipient; in humans typically via colonoscopy, capsules, or enema; in animals via oral gavage [29] [34].
- Applications: Demonstrating transmissibility of phenotypes; therapeutic modification of recipient microbiome; studying microbial engraftment dynamics [29] [34].
- Validation: Metagenomic monitoring of donor strain engraftment; functional assessment through metabolomic profiling [34].
Gnotobiotic Models
- Protocol: Colonization of GF animals with defined microbial communities (human-derived microbiotas or simplified synthetic communities) [31].
- Applications: Determining functional contributions of specific microbial taxa or communities; studying community assembly and stability [31].
- Advantages: Combines experimental control of GF systems with physiological relevance of microbial colonization [31].
Multi-Omics Integration in Human Cohorts
- Protocol: Simultaneous collection of metagenomic, metabolomic, immunologic, and clinical data from well-phenotyped cohorts; integrated computational analysis [34] [24].
- Applications: Identifying biomarker signatures; mapping interactions across biological domains; generating hypotheses about mechanisms [24].
- Validation: Cross-validation in independent cohorts; testing in experimental models [34] [24].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Gut-Organ Axis Studies
| Reagent/Platform | Function/Application | Specific Examples/Considerations |
|---|---|---|
| Shotgun Metagenomic Sequencing | Comprehensive taxonomic and functional profiling of microbial communities | Illumina platforms; Oxford Nanopore for real-time sequencing [34] |
| 16S rRNA Gene Sequencing | High-throughput taxonomic profiling of bacterial communities | Cost-effective for large cohort studies; limited functional information [34] |
| Metabolomics Platforms | Characterization of small molecule metabolites derived from host and microbiome | LC-MS for SCFAs, bile acids, neurotransmitters; GC-MS for volatile compounds [34] [24] |
| Gnotobiotic Isolators | Maintenance of germ-free animals for colonization studies | Flexible film or rigid isolators; strict sterility monitoring protocols [31] |
| Organ-on-a-Chip Models | Microphysiological systems mimicking human gut-brain axis | Gut-brain axis chips with fluidic channels connecting intestinal and neural compartments [32] |
| Bioinformatic Pipelines | Processing and analysis of microbiome sequencing data | QIIME 2, mothur, HUMAnN for functional profiling; custom scripts for integration [34] |
| Artificial Intelligence Platforms | Integrated multi-omics analysis and biomarker discovery | BioMapAI for deep neural network modeling of microbiome-immune-metabolite interactions [24] |
Therapeutic Implications and Microbiome-Targeted Interventions
The gut-organ axis presents promising targets for therapeutic intervention across multiple disease states. Current approaches focus on modifying the gut microbiome or its metabolic output to restore homeostasis.
Microbiota-Targeted Therapeutic Strategies
Probiotics and Prebiotics
- Probiotics: Live microorganisms that confer health benefits when administered in adequate amounts [33]. Specific strains like Bifidobacterium longum APC1472 have shown anti-obesity effects in human trials [33].
- Prebiotics: Substrates selectively utilized by host microorganisms conferring health benefits [33]. Beyond traditional prebiotics (inulin, FOS), the concept is expanding to include human milk oligosaccharides, resistant starch, and polyphenols [33].
- Clinical Evidence: Multi-strain probiotics and specific strains (Bifidobacterium lactis, Bacillus coagulans Unique IS2) show effectiveness for chronic constipation; probiotics demonstrate benefits in some neurological, metabolic, and liver diseases [32] [33].
Fecal Microbiota Transplantation (FMT)
- Mechanism: Entire community approach to restore healthy microbial ecosystem [29] [34].
- Applications: Effective for recurrent Clostridioides difficile infection; under investigation for IBD, ASD with GI symptoms, and IBS [34].
- Optimization: Success depends on stable donor strain engraftment and restoration of key metabolites (SCFAs, bile acid derivatives, tryptophan metabolites); donor-recipient age compatibility may influence outcomes [34].
Dietary Interventions
- High-Fiber Diets: Increase SCFA production; high-fiber diet boosted SCFA production, expanded Tregs, strengthened gut barrier, and reduced CNS inflammation in EAE model of MS [29] [28].
- Fermented Foods: Increase microbial diversity and reduce inflammatory markers [28].
- Personalized Nutrition: Accounting for individual microbial variability in response to dietary components [33].
Small Molecule Therapies
- Postbiotics: Preparations of inanimate microorganisms and/or their components that confer health benefits [33].
- Receptor Agonists/Antagonists: Targeting specific microbial metabolite receptors (e.g., GPCR agonists for SCFAs) [31] [32].
- Microbial Metabolite Supplementation: Direct administration of beneficial microbial metabolites [29].
Clinical Translation Challenges
Despite promising preclinical results, clinical translation of microbiota-targeted therapies faces several challenges:
- Inter-individual Variability: Individual microbiome composition influenced by genetics, diet, lifestyle, and environment complicates universal interventions [32] [30].
- Causality Establishment: Determining whether microbiota alterations are cause, consequence, or modifier of disease processes [29] [30].
- Standardization: Lack of standardized protocols for microbiome-based therapies and outcome measures [34].
- Long-term Safety: Particularly important for pediatric interventions and FMT [30] [34].
The gut-organ axes represent fundamental communication networks that integrate local microbial communities with systemic physiology and disease processes. Mounting evidence demonstrates that microbial dysbiosis contributes to pathogenesis across multiple organ systems through immune, neural, endocrine, and metabolic pathways. While significant progress has been made in characterizing these interactions, several challenges remain for translating this knowledge into clinical practice.
Future research directions should prioritize:
- Longitudinal Multi-omics Studies: Tracking microbiome development and dynamics alongside host physiology over time in diverse populations [30] [34].
- Mechanistic Validation: Moving beyond correlations to establish causal relationships using gnotobiotic models, bacterial cultivation, and targeted interventions [31] [34].
- Standardization and Reproducibility: Implementing harmonized protocols, reference materials, and analytical frameworks across research centers [34].
- Personalized Approaches: Developing microbiome-informed precision medicine strategies accounting for individual microbial, genetic, and environmental contexts [32] [34].
- Ethical and Regulatory Frameworks: Addressing emerging ethical considerations in microbiome-based therapies and diagnostics [30] [34].
As these scientific and translational challenges are addressed, targeting the gut-organ axes holds immense promise for developing novel diagnostic, preventive, and therapeutic strategies across a spectrum of human diseases. The integration of microbiome science into clinical practice represents a paradigm shift toward more holistic, systems-level approaches to human health and disease.
Advanced Methodologies for Microbial Biomarker Discovery and Validation
The study of complex microbial ecosystems has evolved dramatically with the advent of high-throughput sequencing technologies. While metagenomics reveals the genetic potential of a microbial community and metatranscriptomics captures its actively expressed functions, metabolomics identifies the resulting biochemical byproducts [35]. Individually, each approach provides valuable but limited insights: metagenomics answers "what microorganisms are present and what could they potentially do?", metatranscriptomics addresses "what functions are they actively performing?", and metabolomics completes the picture by revealing "what metabolites are being produced?" [35]. However, integrative multi-omics approaches provide a powerful framework for understanding the molecular mechanisms underlying host-microbiome interactions in both health and disease states, offering unprecedented insights for diagnostic biomarker discovery and therapeutic target identification [36] [13] [34].
The clinical relevance of multi-omics integration is particularly evident in microbiome research, where microbial dysbiosis has been implicated in numerous conditions including inflammatory bowel disease, metabolic disorders, and various cancer types [13] [34]. By combining these complementary datasets, researchers can move beyond correlative associations toward mechanistic understandings of how microbial communities influence host physiology and disease pathogenesis [13]. This guide provides a comprehensive comparison of these three omics technologies, their experimental protocols, and their integrated application in microbiome biomarker research.
Technology Comparison: Complementary Methodological Approaches
The table below summarizes the core characteristics, outputs, and applications of the three omics technologies in microbiome research.
Table 1: Comparative analysis of metagenomics, metatranscriptomics, and metabolomics technologies
| Aspect | Metagenomics | Metatranscriptomics | Metabolomics |
|---|---|---|---|
| Analytical Target | Microbial DNA [36] [37] | Total RNA/mRNA [36] [37] | Small molecule metabolites [35] |
| Primary Output | Taxonomic profile & functional potential [36] [35] | Gene expression patterns & active pathways [36] [37] | Metabolic fluxes & end products [35] |
| Key Strengths | Identifies community composition; detects unculturable organisms [36] [37] | Reveals actively expressed genes; dynamic response view [36] [37] | Direct reflection of functional state; high sensitivity [35] [13] |
| Main Limitations | Functional inference only; host DNA contamination [36] [34] | RNA instability; host RNA contamination; computational complexity [36] [37] | Difficult metabolite identification; complex data interpretation [35] |
| Common Platforms | 16S rRNA sequencing; Whole Metagenome Shotgun [36] [35] | RNA-Seq [36] [13] | NMR; LC-MS; FTIR [13] [38] |
| Diagnostic Utility | Microbial signature identification [13] [34] | Active pathway analysis [13] [15] | Metabolic biomarker detection [13] [34] |
Key Differentiating Factors
The temporal resolution represents a fundamental distinction between these approaches. Metagenomics provides a static snapshot of microbial composition and genetic potential, while metatranscriptomics and metabolomics offer dynamic insights into microbial activities and outputs at the time of sampling [37]. This temporal dimension enables researchers to capture microbial community responses to environmental changes, therapeutic interventions, or disease progression.
From a clinical translation perspective, these technologies also differ in their biomarker potential. Metagenomic signatures can stratify patients based on their microbial composition, as demonstrated by enterotyping approaches [34]. Metatranscriptomics identifies actively expressed virulence factors and metabolic pathways with direct pathological significance [13] [15]. Metabolomics detects microbial metabolites with systemic effects on host physiology, such as short-chain fatty acids, bile acids, and amino acid derivatives [13] [34].
Experimental Protocols: From Sample to Data
Metagenomics Workflow
Metagenomic analysis begins with sample collection (stool, tissue, or other specimens) followed by DNA extraction using kits designed for microbial lysis [13]. For 16S rRNA sequencing, PCR amplification targets hypervariable regions of the bacterial 16S ribosomal RNA gene, followed by sequencing on platforms such as Illumina [36] [35]. Whole Metagenome Shotgun (WMS) sequencing fragments all DNA in the sample without targeted amplification, providing greater genomic coverage but requiring deeper sequencing [36]. Bioinformatic processing involves quality control (e.g., using KneadData), taxonomic profiling with tools like MetaPhlAn, and functional annotation using databases such as UniRef90 [13].
Metatranscriptomics Workflow
Metatranscriptomic analysis requires careful RNA preservation at collection due to RNA instability [36] [37]. After total RNA extraction, mRNA enrichment is performed through ribosomal RNA depletion [13]. The extracted mRNA is then reverse transcribed to complementary DNA (cDNA) and prepared for high-throughput sequencing [36]. Bioinformatic analysis includes read mapping to reference genomes, transcript quantification, and differential expression analysis [13] [15]. A significant challenge is distinguishing microbial RNA from abundant host RNA, particularly in low-biomass samples [36].
Metabolomics Workflow
Metabolomic analysis typically begins with metabolite extraction using appropriate solvents based on the chemical properties of target metabolites [13]. For NMR-based approaches, samples are mixed with a deuterated solvent and a reference compound (e.g., TSP) [13]. Liquid chromatography-mass spectrometry (LC-MS) provides higher sensitivity for detecting low-abundance metabolites, while Fourier-transform infrared (FTIR) spectroscopy offers a rapid, cost-effective alternative suitable for large-scale studies [38]. Data processing involves spectral alignment, peak detection, metabolite identification using reference libraries, and multivariate statistical analysis [13].
Integrated Multi-Omics Workflow
The integrated workflow combines these methodologies to provide a comprehensive view of microbial community structure and function. The following diagram illustrates the sequential relationship between these analytical approaches:
Figure 1: Integrated multi-omics workflow for microbiome analysis
Applications in Diagnostic Biomarker Research
Inflammatory Bowel Disease (IBD) Mechanisms
A landmark multi-omics study investigating Crohn's disease (CD) employed shotgun metagenomics on 212 samples, metatranscriptomics on 103 samples, and metabolomics on 105 samples [13]. The metagenomic analysis identified a panel of 20 microbial species that achieved exceptional diagnostic performance with an area under the ROC curve (AUC) of 0.94 in distinguishing CD from healthy controls [13]. Metatranscriptomics revealed significant alterations in microbial fermentation pathways, explaining the depletion of anti-inflammatory butyrate observed in metabolomic profiles [13]. Integration of all three datasets uncovered novel mechanisms where adherent-invasive Escherichia coli (AIEC) utilized propionate to drive expression of the ompA virulence gene, critical for bacterial adherence and invasion of host macrophages [13].
Peri-Implantitis Diagnostics
Research on peri-implantitis integrated full-length 16S rRNA gene sequencing with metatranscriptomics in 48 biofilm samples from 32 patients [15]. This approach revealed a shift from health-associated Streptococcus and Rothia species in healthy implants to anaerobic Gram-negative bacteria in diseased states [15]. Metatranscriptomic analysis identified enzymatic activities and metabolic pathways associated with disease, particularly highlighting the importance of amino acid metabolism in pathogen survival and virulence [15]. The integration of taxonomic and functional data enhanced predictive accuracy to an AUC of 0.85, outperforming single-omics approaches [15].
Urinary Tract Infection Pathogenesis
A study of urinary tract infections (UTIs) applied metatranscriptomic sequencing with genome-scale metabolic modeling to characterize active metabolic functions in patient-specific urinary microbiomes [39]. This approach revealed marked inter-patient variability in microbial composition, transcriptional activity, and metabolic behavior [39]. Analysis of virulence factor expression identified distinct strategies for nutrient acquisition and host invasion among uropathogenic E. coli strains [39]. The integration of gene expression data with metabolic models narrowed flux variability and enhanced biological relevance, highlighting the potential for personalized treatment approaches for managing multidrug-resistant infections [39].
Table 2: Key findings from multi-omics studies in human diseases
| Disease Context | Metagenomic Findings | Metatranscriptomic Findings | Metabolomic Findings | Diagnostic Performance |
|---|---|---|---|---|
| Crohn's Disease [13] | 20-species signature; Altered microbial composition | Disrupted fermentation pathways; AIEC virulence gene expression | Depleted butyrate; Altered SCFA profiles | AUC = 0.94 for species signature |
| Peri-Implantitis [15] | Shift from Gram-positive to anaerobic Gram-negative bacteria | Enhanced amino acid metabolism; Differential enzyme expression | - | AUC = 0.85 with integrated data |
| Type 2 Diabetes [34] | - | - | 111 gut microbiota-derived metabolites; Altered amino acid metabolism | AUC > 0.80 for metabolite panel |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key research reagents and platforms for multi-omics microbiome studies
| Category | Specific Tools/Reagents | Application Purpose |
|---|---|---|
| Sequencing Platforms | Illumina HiSeq; Oxford Nanopore | High-throughput DNA/RNA sequencing [13] [34] |
| Bioinformatics Tools | KneadData; MetaPhlAn; HUMAnN | Quality control; Taxonomic profiling; Functional analysis [13] |
| Reference Databases | UniRef90; VFDB; AGORA2 | Functional annotation; Virulence factor identification; Metabolic modeling [13] [39] |
| Metabolomics Platforms | NMR Spectrometry; UHPLC-HRMS; FTIR | Metabolite identification and quantification [13] [38] |
| RNA Handling Reagents | Ribo-zero Magnetic Kit; RNeasy Mini Kit | rRNA depletion; RNA purification [13] |
| Metabolic Modeling | Genome-scale metabolic models (GEMs) | Predicting microbial community metabolism [39] |
Integrated Data Analysis: From Raw Data to Biological Insight
The true power of multi-omics approaches emerges during integrated data analysis, which enables the construction of comprehensive networks linking microbial taxa to their functional activities and metabolic outputs. The following diagram illustrates the conceptual framework for integrating these diverse datasets:
Figure 2: Multi-omics data integration and analysis framework
Network-Based Integration Approaches
Network-based approaches have emerged as particularly powerful methods for integrating multi-omics datasets [35]. These methods identify correlation patterns between microbial abundance, gene expression, and metabolite levels to reconstruct functional relationships within microbial communities [35]. For example, in IBD research, microbiome-metabolome correlation networks illuminated perturbed microbial pathways and functions tied to inflammation [34]. Similarly, in peri-implantitis, network analysis revealed potential microbial interdependencies related to amino acid metabolism that contribute to disease pathogenesis [15].
Machine Learning Applications
Machine learning techniques are increasingly applied to integrated multi-omics data for biomarker discovery and disease prediction [13] [15] [34]. These approaches can identify complex, non-linear patterns across omics datasets that might be missed by traditional statistical methods. In Crohn's disease research, machine learning applied to multi-omics data enabled high-accuracy classification of disease states [13]. For colorectal cancer, integrative machine learning frameworks that combine metagenomic data with clinical parameters have demonstrated superior predictive accuracy compared to single-data-type approaches [34].
The integration of metagenomics, metatranscriptomics, and metabolomics represents a paradigm shift in microbiome research, moving beyond descriptive community profiling toward mechanistic understanding of host-microbiome interactions. The complementary nature of these approaches provides a more comprehensive view of microbial communities, capturing not only their composition but also their functional activities and metabolic outputs.
For diagnostic applications, multi-omics integration has demonstrated superior performance compared to single-omics approaches, as evidenced by the higher predictive accuracy achieved in conditions like Crohn's disease and peri-implantitis [13] [15]. The continued refinement of standardized protocols, computational tools, and reference databases will further enhance the clinical utility of these approaches. As the field progresses, multi-omics integration is poised to transform microbiome research, enabling the development of novel diagnostics, targeted therapies, and personalized interventions for a wide range of microbiome-associated diseases.
Cross-Cohort Integrative Analysis (CCIA) represents a methodological paradigm in biomedical research that addresses a critical challenge in biomarker discovery: the validation of findings across diverse, independent patient populations. This approach systematically integrates data from multiple cohorts and, when applicable, multiple omics technologies to identify biomarkers that remain robust despite population heterogeneity and technical variability. The fundamental premise of CCIA is that true biological signatures should demonstrate consistent performance across different study populations, geographical locations, and experimental batches. This framework is particularly crucial in microbiome and chronic disease research, where biological heterogeneity can otherwise lead to irreproducible findings and failed clinical translation.
The pressing need for CCIA approaches is underscored by the observation that despite advances in high-throughput technologies, most proposed biomarkers fail to progress to clinical application. As noted in cancer research, "most biomarkers and signatures are identified and validated within a single or very few independent cohorts, rendering them vulnerable to data inconsistency caused by population heterogeneity and technological variability" [40]. Similar challenges exist in microbiome research, where population-specific factors can significantly influence microbial community composition and function. By implementing rigorous cross-cohort validation, researchers can distinguish between cohort-specific artifacts and genuinely robust biological signals, thereby accelerating the development of reliable diagnostic, prognostic, and predictive biomarkers.
Core Methodological Framework of CCIA
Fundamental Principles and Workflow
The CCIA framework is built upon several core principles that distinguish it from traditional single-cohort analyses. First is the systematic integration of data from multiple independent cohorts, which may differ in demographic characteristics, geographical location, or technical processing. Second is the application of stringent batch effect correction to distinguish true biological signals from technical artifacts. Third is the implementation of consensus feature selection across cohorts to identify consistently informative biomarkers. Finally, cross-cohort validation ensures that models trained on one cohort maintain performance when applied to entirely independent populations.
A typical CCIA workflow progresses through sequential phases: (1) comprehensive data acquisition from multiple cohorts with standardized preprocessing; (2) rigorous quality control and batch effect correction; (3) cross-cohort feature selection using consensus approaches; (4) model building with integrated data; and (5) validation across independent cohorts to assess generalizability. This structured approach "helps mitigate biases associated with technological and population heterogeneity" [40] and establishes a foundation for clinically applicable biomarkers.
Comparative Analysis of CCIA Platforms and Tools
Table 1: Computational Platforms Supporting Cross-Cohort Integrative Analysis
| Platform/Tool | Primary Function | Data Types Supported | Key Features | Reference |
|---|---|---|---|---|
| SurvivalML | Prognostic biomarker discovery | Transcriptomics, survival data | Integrates 37,964 samples from 268 datasets across 21 cancer types; 10 machine learning algorithms | [40] |
| MultiBaC | Batch effect correction | Multi-omics data | ARSyN mode for batch correction; handles low-feature scenarios | [41] |
| MMUPHin | Microbiome batch correction | Metagenomic, metatranscriptomic | Corrects batch effects in microbial community data | [42] |
| Proposed CCIA Framework (ML-based) | Biomarker discovery | Transcriptomics | Combines LASSO, Boruta, and varSelRF with consensus feature selection | [41] |
CCIA in Microbiome Research: Applications and Outcomes
Microbial Biomarkers for Hypertension
A compelling implementation of CCIA in microbiome research comes from a hypertension study that analyzed fecal samples from 159 hypertensive patients and 101 healthy controls across two geographical regions (Beijing and Dalian) [42]. This cross-cohort analysis revealed significant alterations in gut bacterial diversity and composition in hypertensive patients compared to healthy controls. The study identified 61 bacterial species with significantly different abundance patterns that were consistent across both cohorts, providing a robust microbial signature of hypertension.
Notably, hypertension-enriched species included Lachnospiraceae (Clostridium symbiosum, Enterocloster bolteae) and Clostridium sp. AT4, while several Lachnospiraceae bacterium and Firmicutes bacterium species were significantly decreased in hypertensive patients [42]. The researchers developed classification models based on these bacterial signatures that achieved area under the curve (AUC) values greater than 0.70 in cross-cohort classification, demonstrating generalizability across populations. In contrast, fungal-based models performed poorly (AUC 0.55-0.57), suggesting that "the gut bacteriome may serve as a more reliable target for hypertension intervention compared to the gut mycobiome" [42].
Inflammatory Bowel Disease Diagnostics
In Crohn's disease (CD) research, a multi-omics CCIA approach applied to fecal samples identified a panel of 20 microbial species that achieved exceptional diagnostic performance with an AUC of 0.94 in an external validation cohort [13]. This study integrated shotgun metagenomics (212 samples), metatranscriptomics (103 samples), and metabolomics (105 samples) data, then validated findings in an additional 638 samples across multiple cohorts. The integrative analysis revealed not only taxonomic signatures but also functional disruptions, including altered microbial fermentation pathways that explain the depletion of anti-inflammatory butyrate observed in CD patients.
The CCIA approach enabled researchers to identify active virulence factor genes predominantly originating from adherent-invasive Escherichia coli (AIEC) in CD patients [13]. These findings unveiled novel mechanisms including "E. coli-mediated aspartate depletion and the utilization of propionate, which drives the expression of the ompA virulence gene, critical for bacterial adherence and invasion of the host's macrophages" [13]. Importantly, these microbiome alterations were absent in ulcerative colitis, underscoring the value of CCIA in distinguishing between related disease subtypes.
Peri-Implantitis Biomarker Discovery
In dental medicine, CCIA has been applied to identify diagnostic biomarkers for peri-implantitis, a biofilm-associated inflammatory condition affecting dental implants [15]. Researchers integrated full-length 16S rRNA gene sequencing and metatranscriptomics data from 48 biofilm samples, with validation in an additional 68 samples. This approach revealed a shift from health-associated Streptococcus and Rothia species in healthy sites to disease-associated anaerobic Gram-negative bacteria in peri-implantitis.
The integration of taxonomic and functional data enhanced predictive accuracy (AUC = 0.85) and identified both microbial and enzymatic biomarkers, including "urocanate hydratase, tripeptide aminopeptidase, NADH:ubiquinone reductase, phosphoenolpyruvate carboxykinase and polyribonucleotide nucleotidyltransferase" [15] as functional markers of disease. The cross-cohort validation confirmed that these signatures maintained diagnostic accuracy across different populations, though population-specific effects were observed, highlighting the importance of CCIA for accounting for geographical variability in microbiome studies.
Table 2: Performance of CCIA-Derived Biomarkers in Microbiome Studies
| Disease Context | Biomarker Type | Training Cohort Performance | Validation Cohort Performance | Key Biomarkers |
|---|---|---|---|---|
| Hypertension [42] | Bacterial species | AUC > 0.70 (internal) | AUC > 0.70 (cross-cohort) | 61 consistently differentiated species |
| Crohn's Disease [13] | Microbial panel | High diagnostic accuracy | AUC = 0.94 (external cohort) | 20-species signature |
| Peri-Implantitis [15] | Taxonomic & functional | - | AUC = 0.85 (integrated model) | Streptococcus, Rothia spp., and enzymatic activities |
| Kawasaki Disease [43] | Inflammation-related genes | AUC > 0.9 | AUC > 0.9 (independent cohorts) | ADM, ALPL, FCGR1A, HP, S100A12, SLC22A4 |
Comparative Experimental Protocols
Multi-Cohort Microbiome Analysis Protocol
The hypertension study [42] exemplifies a rigorous CCIA protocol for microbiome research. Researchers began with metagenome-wide analysis of fecal samples from two independent cohorts (Beijing and Dalian regions). Quality control of sequencing reads was performed using fastp v0.20.164, followed by multiple filtering steps including removal of reads shorter than 90bp, low-quality reads (Phred score <20), and low-complexity reads. Host-derived reads were removed by mapping to human genome references.
For taxonomic profiling, quality-filtered reads were aligned to the Unified Human Gastrointestinal Genome (UHGG) database using Bowtie2 with a stringent 95% nucleotide similarity threshold. To address batch effects between cohorts, researchers employed the MMUPHin pipeline [42], which effectively distinguishes biological signals from technical artifacts. Statistical analyses included alpha diversity assessment (species richness, Shannon and Simpson indices) and multivariate analyses (principal coordinate analysis). Differential abundance testing identified species consistently associated with hypertension across both cohorts, with significance defined as combined P < 0.05 and q = 0.25.
Machine Learning-Driven Biomarker Discovery
For pancreatic ductal adenocarcinoma (PDAC) metastasis, researchers developed a sophisticated CCIA pipeline [41] that integrated RNAseq data from five public repositories (TCGA, GEO, ICGC, CPTAC). The protocol included stringent data preprocessing: normalization using Trimmed Mean of M-values (TMM) to account for sequencing depth differences, filtering of low-expression genes (<5% quantile and <0.1 absolute fold change), and batch effect correction using ARSyN mode 1 from the MultiBaC package.
The machine learning workflow employed a 10-fold cross-validation process that combined three feature selection algorithms (LASSO logistic regression, Boruta, and varSelRF) across 100 models per fold. Genes consistently selected in at least 80% of models across five folds were considered robust biomarkers. This consensus approach specifically addressed the challenge that "variations in input parameters and sample variability from a target population can lead to vastly different predicted outcomes, leading to identification of inconsistent biomarker candidates" [41]. The final model was built using random forest classification and validated on independent cohorts.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Solutions for Implementing CCIA
| Tool/Reagent Category | Specific Examples | Function in CCIA | Key Features |
|---|---|---|---|
| Sequence Processing Tools | fastp v0.20.164, KneadData v0.7.4 | Quality control and decontamination | Removes low-quality reads, host contamination |
| Taxonomic Profiling | MetaPhlAn v4.0.3, Bowtie2 | Microbial community characterization | Species-level identification, alignment to reference databases |
| Batch Effect Correction | MMUPHin, ARSyN (MultiBaC) | Technical variability removal | Corrects for cohort-specific technical artifacts |
| Machine Learning Platforms | SurvivalML, glmnet, ranger | Predictive model building | Cross-cohort validation, multiple algorithm integration |
| Multi-omics Integration | HumanN v3.6, MOFA+ | Functional analysis across data types | Pathway analysis, latent factor modeling |
| Statistical Analysis | vegan package, limma, edgeR | Differential abundance/expression testing | Handles compositional data, multiple testing correction |
Discussion and Future Perspectives
The evidence from multiple studies consistently demonstrates that Cross-Cohort Integrative Analysis significantly enhances the robustness and generalizability of biomarker discoveries across diverse disease contexts. The CCIA framework addresses fundamental limitations in biomedical research by explicitly accounting for population heterogeneity and technical variability through rigorous cross-validation. In microbiome research specifically, CCIA has enabled the identification of microbial signatures that maintain diagnostic accuracy across geographical regions and patient populations, moving the field closer to clinically applicable biomarkers.
Future developments in CCIA will likely focus on several key areas. First, standardized protocols for cross-cohort data harmonization will be essential for maximizing the utility of publicly available datasets. Second, more sophisticated machine learning approaches that can effectively model the complex, multi-layered nature of microbiome-host interactions will enhance predictive power. Third, integration of longitudinal data will enable the identification of dynamic biomarkers that track with disease progression and treatment response. Finally, methodological advances in causal inference will help distinguish correlative from causative relationships in multi-cohort data.
As these methodological refinements progress, CCIA is poised to become the standard approach for biomarker discovery and validation, ultimately accelerating the translation of microbiome research into clinical applications that improve patient care across diverse populations. The continued development and adoption of CCIA frameworks represents a critical step toward realizing the promise of precision medicine in microbiome-related disorders.
The integration of machine learning (ML) into diagnostic modeling represents a paradigm shift in how researchers approach disease detection and biomarker discovery. Among the plethora of ML algorithms, Random Forest (RF) has emerged as a particularly powerful tool for classification tasks in complex biological data, often outperforming other classical algorithms [44]. RF is an ensemble learning method that operates by constructing a multitude of decision trees during training and outputting the class that is the mode of the classes for classification or mean prediction for regression of the individual trees [45]. Its inherent advantages include the ability to handle high-dimensional data, resistance to overfitting, and providing estimates of feature importance, making it exceptionally suitable for biomedical applications where the number of features often far exceeds the number of samples [46].
The performance of RF, and ML models in general, is critically dependent on the quality and relevance of input features. Feature selection—the process of selecting a subset of relevant features for use in model construction—serves as a crucial preprocessing step that enhances model interpretability, reduces computational complexity, and improves generalization performance by mitigating the curse of dimensionality [47]. This is particularly vital in microbiome biomarker studies, where datasets may contain thousands of microbial taxa or gene expression profiles, many of which are redundant or irrelevant to the classification task [48]. Effective feature selection helps identify the most biologically informative biomarkers, facilitating the development of robust diagnostic models with greater clinical applicability.
Within the specific context of microbiome biomarker diagnostic validation, RF coupled with sophisticated feature selection strategies has demonstrated remarkable potential. The gut microbiome, with its complex ecosystem of microorganisms, has been increasingly implicated in various diseases, including Parkinson's disease, colorectal cancer, and metabolic disorders [48] [49]. However, the high variability in microbiome composition across populations and studies presents significant challenges for developing universally applicable diagnostic models [48]. This comparison guide objectively evaluates the performance of RF and various feature selection methods in diagnostic modeling, with a particular focus on microbiome research, providing researchers and drug development professionals with evidence-based insights for their experimental designs.
Performance Comparison of Random Forest with Feature Selection Methods
Comprehensive Performance Metrics Across Biomedical Applications
Table 1: Performance of Random Forest with Different Feature Selection Methods in Diagnostic Modeling
| Application Domain | Feature Selection Method | Dataset Size | Key Performance Metrics | Number of Selected Features |
|---|---|---|---|---|
| Sports Effectiveness Evaluation [45] | Weighted Feature Importance + Optimized Artificial Raindrop Algorithm | Not Specified | Accuracy: Training: 0.849±0.021, Testing: 0.819±0.022F1-Score: 0.837±0.020 (Training), 0.864±0.021 (Testing) | Not Specified |
| Breast Cancer Diagnosis [46] | Seagull Optimization Algorithm (SGA) | Not Specified | Mean Accuracy: 99.01%Mean Accuracy Range: 85.35%-94.33% (with varying feature subsets) | 22 genes |
| Parkinson's Disease Microbiome Classification [48] | Ridge Regression (Baseline) | 4,489 samples (22 studies) | Average AUC (Within-Study): 71.9%Average AUC (Cross-Study): 61.0%Average AUC (With Multi-Study Training): 68.0% | Not Specified |
| Prediabetes Screening [44] | LASSO + PCA | 4,743 individuals | ROC-AUC: 0.9117Key Predictors Identified: BMI, age, HDL-C, LDL-C | 12 principal components (retaining 95% variance) |
| Alzheimer's Disease Prediction [50] | Backward Elimination with Ant Colony Optimization | 2,149 instances with 34 features | Accuracy: 95%±1.2%Precision: 95%±1.1%Recall: 94%±1.3%F1-Score: 95%±1.0%AUC: 98%±0.8% | 26 significant features |
| Usher Syndrome Biomarker Discovery [47] | Hybrid Sequential (Variance Thresholding + Recursive Feature Elimination + Lasso) | 42,334 mRNA features | Successfully reduced to 58 top mRNA biomarkers with robust classification performance | 58 mRNA biomarkers |
Comparative Analysis with Alternative Machine Learning Algorithms
Table 2: Random Forest vs. Other Classifiers in Biomedical Applications
| Comparative Study | Algorithms Compared | RF Performance | Best Performing Alternative | Key Findings |
|---|---|---|---|---|
| Breast Cancer Diagnosis [46] | RF, Linear Regression (LR), Support Vector Machine (SVM), K-Nearest Neighbors (KNN) | 99.01% accuracy with SGA feature selection | RF outperformed all alternatives | RF demonstrated consistent performance across varying feature subsets |
| Prediabetes Screening [44] | RF, XGBoost, SVM, KNN | ROC-AUC: 0.9117 | XGBoost followed closely | RF showed best robustness in generalizing across datasets; both tree-based models outperformed SVM and KNN |
| Alzheimer's Prediction [50] | RF with optimized feature selection vs. conventional ML algorithms including XGBoost | 95% accuracy | RF with BE-ACO outperformed all others | The framework showed statistically significant improvements (p < 0.001) over conventional algorithms |
| Parkinson's Microbiome [48] | RF, Ridge Regression, LASSO | Varied by dataset (Average AUC: 71.9% across studies) | Ridge Regression and LASSO sometimes outperformed RF on specific metagenomic data | RF generally performed better on 16S data, while Ridge/LASSO performed better on some shotgun metagenomics data |
Critical Considerations for Microbiome Biomarker Studies
The application of RF and feature selection in microbiome diagnostic validation presents unique challenges and considerations. A critical finding from large-scale meta-analyses is that study-specific models often fail to generalize across different populations. In Parkinson's disease microbiome studies, for instance, models trained on individual datasets showed promising within-study performance (average AUC of 71.9%) but significantly decreased accuracy when applied to external validation cohorts (average AUC of 61.0%) [48]. This highlights the critical importance of cross-study validation in microbiome biomarker research.
Training models on multiple datasets substantially improves generalizability, as demonstrated by the increase in average leave-one-study-out (LOSO) AUC to 68% in Parkinson's disease classification [48]. Additionally, the choice of sequencing technology impacts model performance, with shotgun metagenomics data generally yielding higher classification accuracy (average AUC 78.3% ± 6.5) compared to 16S rRNA data (average AUC 72.3% ± 11.7) [48].
Feature stability emerges as another crucial consideration alongside accuracy. Research on allergy biomarker discovery revealed that while RF can achieve high predictive accuracy (0.9999 with top five features), its feature importance rankings may be unstable, potentially leading to irreproducible biomarker selection [51]. This underscores the need for stability-aware feature selection approaches in diagnostic model development, particularly for microbiome studies where reproducibility across cohorts is essential for clinical translation.
Experimental Protocols for Diagnostic Modeling with Random Forest
Standardized Workflow for Microbiome-Based Diagnostic Models
The development of robust diagnostic models using RF and feature selection follows a systematic workflow encompassing data preprocessing, feature selection, model training, and validation. The following diagram illustrates a comprehensive experimental protocol integrating elements from multiple studies analyzed in this review:
Detailed Methodological Protocols
Data Preprocessing and Normalization
Microbiome data requires careful preprocessing to handle technical variability and compositionality. For 16S rRNA sequencing data, standard protocols include:
- Sequence Processing: Using QIIME2 or similar pipelines for demultiplexing, trimming, merging, and denoising reads to generate amplicon sequence variants (ASVs) [49].
- Taxonomic Classification: Assigning taxonomy using reference databases such as SILVA or Greengenes with pre-trained classifiers [49].
- Normalization: Applying total-sum scaling (TSS) or other normalization methods to account for varying sequencing depths [49].
- Filtering: Implementing prevalence filters (e.g., retaining taxa detected in at least 5% of samples) to reduce noise [48].
For gene expression data in biomarker discovery, similar preprocessing pipelines are employed, often using specialized tools like the Easy Microbiome Analysis Platform (EasyMAP) for standardized processing [49].
Feature Selection Methodologies
The studies reviewed implement diverse feature selection strategies:
Nature-Inspired Optimization Algorithms: The Seagull Optimization Algorithm (SGA) was successfully applied for gene selection in breast cancer diagnosis, systematically exploring the feature space to identify optimal gene subsets [46]. Similarly, Ant Colony Optimization and Whale Optimization Algorithm have been employed for feature selection in Alzheimer's disease prediction [50].
Statistical and Model-Based Methods: Least Absolute Shrinkage and Selection Operator (LASSO) regression effectively selects features by applying a penalty that drives less important coefficients to zero [44]. Recursive feature elimination systematically removes the least important features based on model performance [47].
Hybrid Sequential Approaches: Combining multiple feature selection techniques (e.g., variance thresholding, recursive feature elimination, and Lasso regression) within a nested cross-validation framework has proven effective for high-dimensional biomarker discovery, as demonstrated in Usher syndrome research [47].
Model Training and Hyperparameter Optimization
Optimal RF performance requires careful hyperparameter tuning:
- Hyperparameter Optimization: Nature-inspired algorithms such as Artificial Ant Colony Optimization and Bald Eagle Search have demonstrated substantial computational efficiency advantages over empirical approaches (81% reduction in computation time) [50].
- Cross-Validation Strategy: Nested cross-validation is preferred, with an inner loop for hyperparameter tuning and feature selection, and an outer loop for performance estimation to prevent optimistic bias [47].
- Class Imbalance Handling: Techniques such as Synthetic Minority Oversampling Technique (SMOTE) are applied to training data only, with careful separation to prevent data leakage [50].
Validation Protocols
Robust validation is essential for assessing diagnostic model generalizability:
- Cross-Study Validation: Evaluating model performance on completely independent datasets from different populations or research centers [48].
- Leave-One-Study-Out (LOSO) Validation: Training models on multiple studies and testing on each held-out study to assess generalizability [48].
- External Validation: Testing models on entirely independent cohorts, preferably from different geographical regions, to evaluate real-world applicability [49].
- Biological Validation: Experimentally validating computationally identified biomarkers using methods such as droplet digital PCR (ddPCR) to confirm biological relevance [47].
Signaling Pathways and Biological Mechanisms
Microbiome-Host Interactions in Disease Pathogenesis
Microbiome-based diagnostic models derive their predictive power from the fundamental role of microbial communities in human health and disease. The biological relevance of microbiome biomarkers is grounded in specific pathways through which gut microbes influence host physiology:
The pathway diagram illustrates key mechanisms identified in microbiome studies:
Short-Chain Fatty Acid (SCFA) Depletion: PD microbiome studies consistently show depletion of SCFA-producing bacteria. SCFAs (butyrate, propionate, acetate) maintain epithelial barrier integrity and colonic immune homeostasis. Their reduction compromises gut barrier function, potentially allowing translocation of pathogenic molecules [48].
Biotransformation of Environmental Toxins: Shotgun metagenomic analysis reveals enrichment of microbial pathways for solvent and pesticide biotransformation in PD. This aligns with epidemiological evidence that exposure to these molecules increases PD risk and raises the question of whether gut microbes modulate their toxicity [48].
Microbial Genotoxin Production: In colorectal cancer, bacteria such as Fusobacterium nucleatum and Porphyromonas gingivalis produce genotoxins that cause DNA damage in host cells, driving tumorigenesis [49].
Barrier Dysfunction and Inflammation: Microbiome alterations contribute to increased intestinal permeability, allowing bacterial translocation and systemic immune activation, which is implicated in various diseases including Parkinson's, colorectal cancer, and metabolic disorders [48] [49].
These biologically plausible mechanisms validate the relevance of microbiome biomarkers identified through RF and feature selection approaches, strengthening the case for their diagnostic utility.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents and Computational Tools for Microbiome Diagnostic Studies
| Category | Item/Reagent | Specific Function | Example Application |
|---|---|---|---|
| Sequencing Technologies | 16S rRNA Sequencing | Profiling microbial community composition using hypervariable regions | Initial microbiome profiling in Parkinson's disease studies [48] |
| Shotgun Metagenomics | Comprehensive analysis of microbial genes and functional pathways | Identifying microbial metabolic pathways in PD [48] | |
| Bioinformatics Tools | QIIME2 Pipeline | Processing and analyzing microbiome sequencing data | Microbiome data processing in colorectal cancer study [49] |
| Easy Microbiome Analysis Platform (EasyMAP) | Integrated platform for microbiome data analysis | Data preprocessing in CRC screening study [49] | |
| SIAMCAT (R Package) | Statistical inference and machine learning for microbiome data | Machine learning analysis in PD microbiome study [48] | |
| Feature Selection Algorithms | Seagull Optimization Algorithm (SGA) | Nature-inspired feature selection based on seagull behavior | Gene selection in breast cancer diagnosis [46] |
| Ant Colony Optimization | Swarm intelligence-based optimization for feature selection | Hyperparameter optimization in Alzheimer's prediction [50] | |
| LASSO Regression | Regularization technique that performs feature selection | Identifying key predictors in prediabetes screening [44] | |
| Validation Technologies | Droplet Digital PCR (ddPCR) | Absolute quantification of specific biomarkers with high precision | Experimental validation of mRNA biomarkers in Usher syndrome [47] |
| Synthetic Minority Oversampling Technique (SMOTE) | Addressing class imbalance in machine learning datasets | Handling data imbalance in Alzheimer's prediction [50] | |
| Reference Databases | SILVA Database | Curated database for taxonomic classification of microbiome data | Taxonomic classification in CRC study [49] |
This toolkit represents essential resources employed in the studies reviewed, providing researchers with a foundation for developing and validating microbiome-based diagnostic models using RF and feature selection methodologies.
The human microbiome has emerged as a rich source of biomarkers for disease diagnosis, prognosis, and therapeutic monitoring. Selecting the appropriate biospecimen for microbial biomarker detection is a critical decision that directly influences research outcomes, clinical applicability, and diagnostic accuracy. Stool, blood, and saliva each offer distinct advantages and limitations based on their biological composition, collection feasibility, and biomarker representation.
This guide provides an objective comparison of these three biospecimen sources within the context of microbiome biomarker diagnostic validation cohort studies. We present experimental data, methodological protocols, and analytical frameworks to assist researchers, scientists, and drug development professionals in making evidence-based decisions for their specific research objectives.
The diagnostic performance of microbial biomarkers varies significantly across different biospecimen sources, reflecting their distinct biological relationships to disease processes. The table below summarizes quantitative performance data from recent studies investigating biomarkers for colorectal cancer (CRC) and Parkinson's disease (PD).
Table 1: Diagnostic Performance of Microbial Biomarkers Across Biospecimens
| Disease | Biospecimen | Biomarker Type | Key Findings | Performance Metrics | Citation |
|---|---|---|---|---|---|
| Colorectal Polyps | Saliva | Microbial (16S rRNA) | Signature included P. gingivalis, F. nucleatum | AUC: 0.8167 | [52] |
| Colorectal Polyps | Feces | Microbial (16S rRNA) | Signature included R. gnavus, B. ovatus | AUC: 0.8051 | [52] |
| Colorectal Polyps | Saliva + Feces | Combined Microbial | Additive diagnostic value | AUC: 0.8217 | [52] |
| Parkinson's Disease | Saliva | Microbial (Shotgun Metagenomics) | Subspecies-level abundances best distinguished PD | AUC: 0.758 | [53] |
| Colorectal Cancer | Saliva | microRNAs (e.g., miR-92a, miR-29a) | High sensitivity and specificity for CRC detection | Sensitivity: 0.76, Specificity: 0.83 | [54] [55] |
Experimental Methodologies for Biospecimen Analysis
Sample Collection and Storage Protocols
Standardized collection and storage protocols are fundamental to maintaining sample integrity and ensuring reproducible results in cohort studies.
Saliva Collection: Participants should refrain from eating, drinking, chewing gum, smoking, or brushing teeth for 30 minutes before collection. Saliva can be collected using standardized kits like OMNIgene•ORAL (DNA Genotek), which homogenize samples at point of collection and maintain DNA stable at ambient temperature for 60 days [53]. The spitting method is considered easy and self-administerable with high participant compliance [54].
Stool Collection: Stool samples are typically collected using dedicated kits such as OMNIgene•GUT (DNA Genotek). These kits stabilize microbial DNA at room temperature, eliminating the need for immediate freezing and facilitating shipment from participants' homes to laboratory facilities [53].
Blood Collection: For microbiome analysis from blood, peripheral whole blood samples (e.g., 2.5 ml) should be collected in specialized systems like the PAXgene Blood RNA System according to manufacturer's instructions. Plasma can be separated by centrifugation (10 min at 1000×g) and stored at -80°C for preservation [56].
DNA Extraction and Sequencing Approaches
Different biospecimens require optimized processing protocols to extract high-quality microbial DNA for downstream analysis.
DNA Extraction: Microbial DNA extraction from both saliva and stool can be performed at room temperature using commercial kits such as the QIAGEN Powersoil Pro DNA isolation kit with a liquid-handling robot, following manufacturer protocols [53].
Sequencing Methods:
- Full-length 16S rRNA sequencing: Provides high taxonomic resolution at the species level and can be used for both salivary and fecal microbiota analysis [52].
- Shallow shotgun metagenomic sequencing: Enables comprehensive taxonomic and functional profiling across both stool and saliva samples, with a target depth of 2 million reads per sample recommended [53].
- RNA sequencing: For blood-based transcriptomic biomarkers, sequence libraries can be prepared using enzymatic tagmentation with low cycle polymerase chain reaction [56].
Bioinformatic and Statistical Analysis Pipelines
Robust bioinformatic processing is essential for deriving meaningful biological insights from microbiome sequencing data.
Taxonomic Annotation: Quality-controlled reads can be annotated taxonomically by alignment to databases containing all representative genomes in NCBI's RefSeq for bacteria with additional manually curated strains. Alignments are typically performed at 97% identity against all reference genomes [53].
Microbiome Analysis:
- Alpha-diversity: Assesses within-sample microbial diversity using metrics such as Shannon index or Chao1 [52].
- Beta-diversity: Evaluates between-sample microbial community differences using methods like Principal Coordinate Analysis (PCoA) with Bray-Curtis dissimilarity [52].
- Differential Abundance Analysis: Tools like Linear Discriminant Analysis Effect Size (LEfSe) can identify specific taxa with statistically significant differences in abundance between sample groups [52].
Diagnostic Model Construction: Machine learning approaches such as random forest models can be employed to identify optimal biomarker combinations. Model performance should be assessed using receiver operating characteristic (ROC) curves and area under curve (AUC) values [56] [52].
Practical Considerations for Research Implementation
Participant Compliance and Collection Feasibility
Participant compliance varies substantially across biospecimen types and directly impacts study feasibility and sample size attainment in validation cohorts.
Saliva: Presents the fewest barriers to collection, with easy self-administration potential that may increase screening participation, particularly in underserved or rural populations [54]. Saliva collection is completely non-invasive and painless, requiring no clinical supervision [54].
Stool: Collection is less invasive than blood draws but faces moderate compliance challenges due to patient reluctance in handling fecal matter [54]. The collection process can be self-administered but may be perceived as unpleasant by some participants [54].
Blood: Requires trained phlebotomists for collection, making it more difficult to scale for large population-based studies. Blood collection is considered highly invasive compared to other options [54].
Sample Stability and Storage Requirements
Different biospecimens present varying challenges for sample stability and storage logistics in multi-center cohort studies.
Saliva and Stool: Modern collection kits (e.g., OMNIgene series) rapidly homogenize samples at point of collection and maintain DNA stable at ambient temperature for extended periods (up to 60 days), with no cold chain required [53]. This facilitates mailing from participants' homes directly to processing facilities.
Blood: Requires more immediate processing and freezing for plasma separation. Long-term storage typically demands -80°C freezers, creating significant infrastructure requirements [56].
Biomarker Stability and Analytical Considerations
The stability of molecular targets varies across biospecimens, influencing pre-analytical processing requirements.
Microbial DNA: Generally stable across all three biospecimen types when properly preserved, with stool and saliva offering particularly robust DNA yields for microbiome analysis [53].
miRNAs: Demonstrate high stability in both blood and saliva, existing in different forms including freely circulating, protein-bound, or encapsulated within extracellular vesicles such as exosomes [55].
Research Reagent Solutions
Successful implementation of microbial biomarker studies requires specific reagents and platforms optimized for different biospecimen types.
Table 2: Essential Research Reagents for Microbial Biomarker Studies
| Reagent Category | Specific Product Examples | Application Notes |
|---|---|---|
| Sample Collection & Stabilization | OMNIgene•ORAL, OMNIgene•GUT (DNA Genotek), PAXgene Blood RNA System | Enables ambient temperature storage/stability; critical for multi-center cohort studies |
| DNA Extraction | QIAGEN Powersoil Pro DNA Isolation Kit | Effective for challenging samples like stool; room temperature processing possible |
| Library Preparation | Illumina DNA Prep Kit, Nextera XT Library Prep Kit | Compatibility with both 16S rRNA and shotgun metagenomic approaches |
| Sequencing | Illumina NovaSeq, MiSeq platforms (BoosterShot shallow shotgun) | Balance between depth and cost; 2 million reads/sample often sufficient |
| Computational Tools | CIBERSORTx, LEfSe, randomForest R package, QIIME 2, DESeq2 | Essential for immune deconvolution, differential abundance analysis, and machine learning |
Visualizing Experimental Workflows
The following diagram illustrates a generalized workflow for microbial biomarker discovery and validation across different biospecimen sources, highlighting parallel processing paths and key decision points.
The selection of biospecimen sources for microbial biomarker detection involves careful consideration of multiple factors, including diagnostic performance, practical implementation, and biological relevance to the disease under investigation. Stool remains the gold standard for gastrointestinal disorders, while saliva offers exceptional promise as a non-invasive alternative with high participant compliance. Blood provides unique insights into host-microbe interactions and systemic immune responses but presents greater logistical challenges.
Future directions in microbial biomarker research will likely focus on multi-specimen approaches that leverage the complementary strengths of different biosources. The integration of standardized protocols, advanced sequencing technologies, and sophisticated computational models will be essential for translating microbial biomarkers into clinically valuable diagnostic tools.
The translation of microbiome sequencing data into clinically viable diagnostic tests represents a frontier in precision medicine. Within this pipeline, quantitative polymerase chain reaction (qPCR) assays stand as a cornerstone technology, bridging the gap between discovery-based metagenomic surveys and affordable, rapid clinical diagnostics. The validation of microbial biomarkers for conditions such as hypertension [42] and peri-implantitis [15] requires technologies that are not only sensitive and specific but also cost-effective and scalable for routine use. While next-generation sequencing (NGS) identifies potential biomarkers, qPCR provides the quantitative, high-throughput validation necessary for clinical adoption. This guide objectively compares the performance of different qPCR approaches and alternative digital PCR (dPCR) platforms, providing researchers with the experimental data and protocols needed to develop robust, affordable diagnostic assays for microbiome-derived biomarkers.
Comparative Analysis of PCR Technologies for Diagnostic Assay Development
The selection of an appropriate amplification technology is fundamental to diagnostic assay performance. The table below provides a structured comparison of the primary PCR-based methods used in translating microbiome biomarkers into clinical diagnostics.
Table 1: Performance Comparison of PCR Technologies for Diagnostic Assay Development
| Technology | Quantification Method | Throughput | Best Use Case in Microbiome Diagnostics | Key Limitations |
|---|---|---|---|---|
| qPCR / Real-Time PCR [57] [58] | Relative quantification via Ct values and standard curves | High (96/384-well plates); Very High with Nano-fluidic Systems (5,184 reactions) [59] | Validating abundance of specific bacterial biomarkers (e.g., in hypertension [42]); High-throughput screening | Efficiency can be variable and affected by inhibitors; requires standard curves for absolute quantification |
| Digital PCR (dPCR) [60] [57] | Absolute quantification by Poisson statistics of end-point positive/negative partitions | Moderate | Absolute quantification of low-abundance microbial targets; detecting minor population shifts without standard curves | Higher cost per sample; more complex workflow; lower throughput than high-end qPCR systems |
| High-Throughput qPCR (Nano-scale) [61] [59] | Relative quantification via Ct values | Very High (5,184 reactions per run) | Large-scale validation studies; screening massive panels of microbial targets across many samples | High initial instrument investment; nanoliter volumes require precise fluid handling |
Experimental Protocols for qPCR Assay Validation
Robust assay validation is critical for generating clinically reliable data. The following section details key experimental protocols for establishing and validating qPCR assays targeting microbiome biomarkers.
Efficiency Estimation Using Dilution-Replicate Design
Accurate PCR efficiency (E) estimation is paramount, as small errors can lead to large miscalculations in target quantification due to the exponential nature of the reaction [62] [58]. The traditional method of using technical replicates for each sample can be inefficient. An alternative dilution-replicate design has been proposed to simultaneously estimate both PCR efficiency and initial DNA quantity from a single experiment with fewer overall reactions [62].
Detailed Protocol:
- Sample Dilution: For each test sample, prepare a series of dilutions (e.g., two-, ten-, and 50-fold). Using at least three dilution points is recommended.
- qPCR Run: Perform a single qPCR reaction for each dilution point per sample, without traditional identical replicates.
- Standard Curve Plotting: For each sample, plot the Cq values (y-axis) against the logarithm of the dilution factors (x-axis).
- Efficiency Calculation: Perform linear regression. The slope of the line is used to calculate efficiency:
E = 10^(-1/slope) - 1[62] [58]. - Global Efficiency Estimation: To improve accuracy, data from all samples can be fit simultaneously with a constraint of equal slope, yielding a globally estimated PCR efficiency that is more robust against outliers [62].
This design is particularly useful in microbiome studies where numerous samples and target genes are analyzed, as it reduces reagent costs and provides a direct efficiency estimate for each sample.
PCR-Stop Analysis for Assay Validation in the Boundary Limit Area
The PCR-Stop analysis is a validation tool that probes the performance of a qPCR assay during its initial cycles, providing essential data on quantitative resolution and the quantitative limit, particularly in the range above 10 initial target molecule numbers (ITMN) [63].
Detailed Protocol:
- Sample Preparation: Prepare six batches of eight identical reactions each, all containing the same target DNA quantity (>10 ITMN).
- Pre-runs: Subject the batches to ascending numbers of pre-amplification cycles (0 to 5). The "0 cycle" batch is placed directly in a cooler.
- Main qPCR Run: Transfer all batches to a real-time PCR thermocycler and run a full qPCR protocol.
- Data Analysis: Analyze the results based on four criteria [63]:
- Criterion I (Efficiency): Calculate the amplification efficiency during the initial cycles from the steady increase in average Cq values across batches.
- Criterion II (Consistency): Determine the Relative Standard Deviation (RSD) of the Cq values within the eight samples of each batch to assess assay consistency.
- Criterion III (Resolution): Assess the steady increase of values and regularity across batches to confirm quantitative resolution.
- Criterion IV (Qualitative Limit): Note any negative samples to demonstrate the qualitative detection limit.
This protocol is vital for verifying that an assay starts with its average efficiency from the first cycle, which is especially important for methods like the comparative Cq (2-ΔΔCq) used in relative gene expression analysis [63].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for qPCR Assay Development
| Item | Function / Application | Example Use Case |
|---|---|---|
| SYBR Green Master Mix [58] | Fluorescent dye that binds double-stranded DNA; used for monitoring amplification in real-time. | Gene expression quantification and microbial load assessment in microbiome samples. |
| TaqMan Probes [57] | Sequence-specific fluorescent probes providing higher specificity than intercalating dyes. | Multiplex detection of different microbial pathogens or functional genes in a single reaction. |
| Silica-based DNA Extraction Kits [57] | Purification of high-quality, inhibitor-free nucleic acids from complex biological samples (e.g., stool, biofilm). | Preparing template DNA from gut microbiome or oral biofilm samples for reliable qPCR results [42] [15]. |
| Exogenous Spike-in Controls [61] | Non-target DNA sequences added to the sample to control for variations in extraction and amplification efficiency. | Minimizing false negatives in pathogen detection panels; normalizing for PCR inhibition. |
| Primers for Reference Genes [58] | Amplifies constitutively expressed "housekeeping" genes used for data normalization. | Normalizing the abundance of a target microbial gene to a host gene or a conserved bacterial gene in a sample. |
Workflow and Decision Pathways for Diagnostic Development
The process of developing a diagnostic assay from sequencing data involves multiple steps, from biomarker discovery to the selection of the optimal detection platform. The diagram below outlines this integrated workflow.
Figure 1: From biomarker discovery to clinical validation workflow.
Following the establishment of a validation cohort, selecting the right detection technology is crucial. The decision pathway below outlines the logic for choosing between qPCR, dPCR, and high-throughput systems based on the specific requirements of the diagnostic project.
Figure 2: Decision pathway for PCR technology selection.
The development of affordable, clinic-ready diagnostic platforms from microbiome sequencing data relies heavily on the strategic implementation of qPCR and related technologies. As demonstrated in cross-cohort biomarker studies [42] [15], the transition from discovery to validation requires careful consideration of assay efficiency, throughput, and cost. By employing rigorous validation protocols like the dilution-replicate design [62] and PCR-Stop analysis [63], researchers can ensure the quantitative accuracy of their assays. The evolving landscape of PCR, including nano-scale high-throughput systems [59] and dPCR [60], offers a versatile toolkit for tailoring diagnostic development to specific clinical needs, ultimately paving the way for microbiome-based diagnostics to improve patient care.
Navigating Technical Challenges and Optimizing Study Designs for Clinical Translation
The pursuit of valid microbiome biomarkers for disease diagnostics hinges on the successful integration of data from multiple cohorts. A paramount obstacle in this endeavor is the presence of batch effects—technical variations introduced from different labs, sequencing times, or platforms that are unrelated to the biological signals of interest. If left uncorrected, these effects can produce misleading outcomes, obscure genuine discoveries, and severely undermine the reproducibility of findings, even leading to retracted studies [64]. This guide objectively compares the performance of leading computational solutions designed to overcome these challenges, providing researchers with the data needed to select the appropriate tool for robust multi-cohort integration in microbiome biomarker research.
Performance Benchmarking: A Comparative Analysis of Integration Tools
To aid in tool selection, we compare three advanced data integration methods, evaluating their performance, scalability, and suitability for different data types based on published evidence.
Table 1: Comparative Performance of Data Integration Tools
| Tool Name | Core Methodology | Best For | Data Retention | Runtime Efficiency | Key Advantage |
|---|---|---|---|---|---|
| BERT [65] | Batch-Effect Reduction Trees (Binary tree of ComBat/limma) | Large-scale, incomplete omic profiles (proteomics, transcriptomics, metabolomics) | Retains all numeric values (up to 5 orders of magnitude more than others) [65] | Up to 11× faster than competitors [65] | Handles severely imbalanced conditions with covariates & references |
| HarmonizR [65] | Matrix dissection & embarrassingly parallel ComBat/limma | Smaller datasets with arbitrary missingness | High data loss with increasing missing values (up to 88% loss with blocking) [65] | Slower, improved with batch blocking | The established imputation-free method for incomplete data |
| Federated Harmony [66] | Federated learning combined with Harmony algorithm | Distributed single-cell multi-omics data (scRNA-seq, scATAC-seq) | Comparable to centralized Harmony | Faster than centralized Harmony; avoids data transfer bottlenecks [66] | Privacy-preserving; enables integration without raw data sharing |
Experimental Protocols for Key Benchmarking Studies
The performance data presented in the comparison table are derived from controlled studies. Below are the detailed methodologies for the key experiments cited.
Protocol 1: Benchmarking BERT vs. HarmonizR on Simulated Omic Data
This protocol outlines the procedure used to generate the quantitative performance data for BERT and HarmonizR [65].
- Data Simulation: Generate a complete data matrix with 6000 features (simulating omic features) and 20 batches with 10 samples each. Simulate two distinct biological conditions.
- Introduce Missingness: Randomly select a subset of features to be completely missing in each batch, varying the ratio of missing values up to 50% under a Missing Completely at Random (MCAR) scheme.
- Algorithm Application: Apply both BERT (using default parameters) and HarmonizR (using its full dissection mode and blocking strategies of 2 or 4 batches) to the simulated datasets.
- Performance Metrics:
- Data Retention: Calculate the total number of numeric values retained in the integrated dataset for each method.
- Runtime: Measure the sequential execution time for 10 repetitions of each tool.
- Integration Quality: Compute the Average Silhouette Width (ASW) with respect to both the batch of origin (to measure batch effect removal) and the biological condition (to measure biological signal preservation).
Protocol 2: Validating Federated Harmony on Single-Cell Data
This protocol describes the experiment used to validate the performance of Federated Harmony against centralized Harmony [66].
- Data Curation: Collect a single-cell RNA sequencing (scRNA-seq) dataset from human peripheral blood mononuclear cells (PBMC) comprising 5 samples from different batches.
- Data Splitting: For Federated Harmony, split the dataset by its original batches and treat each as a separate, non-centralized institution to simulate a real-world, privacy-constrained scenario.
- Integration:
- Apply the standard, centralized Harmony algorithm to the entire dataset for a baseline result.
- Apply Federated Harmony to the split datasets, where only summary statistics are shared with a central server.
- Performance Evaluation:
- Visual Inspection: Generate UMAP plots from the integrated embeddings of both methods to visually assess cluster mixing (batch correction) and cell type separation (biological conservation).
- Quantitative Metrics: Calculate the Local Inverse Simpson's Index (LISI) to quantify batch mixing (iLISI) and cell type separation (cLISI). Higher iLISI scores indicate better batch integration.
- Clustering Accuracy: Use the Adjusted Rand Index (ARI) to compare the congruence of k-means clustering results from the integrated data with known cell type labels.
Visualizing Computational Workflows
The following diagrams illustrate the core logical workflows of the featured data integration tools, highlighting their distinct approaches to conquering batch effects.
BERT Hierarchical Integration Workflow
Federated Harmony Privacy-Preserving Workflow
The Scientist's Toolkit: Essential Research Reagents & Computational Solutions
Successful multi-cohort integration requires both robust algorithms and a suite of supporting tools and resources.
Table 2: Key Research Reagent Solutions for Data Integration
| Tool/Resource | Category | Primary Function | Relevance to Microbiome Studies |
|---|---|---|---|
| ComBat [65] | Algorithm | Empirical Bayes framework for adjusting batch effects. | Core correction engine used in BERT and HarmonizR for various omics data. |
| limma [65] [4] | Algorithm | Linear models for differential analysis and batch correction. | Used in BERT; also for covariate adjustment in microbiome ML pipelines [4]. |
| MMUPHin [4] | R Package | Meta-analysis and batch effect adjustment for microbiome data. | Specifically designed to control for cross-cohort batch effects in microbial community profiles. |
| xMarkerFinder [67] | Computational Framework | Standardized identification/validation of microbial biomarkers from cross-cohort data. | Addresses biomarker heterogeneity across studies; includes feature selection and validation. |
| MaAsLin2 [68] | Algorithm | Identifies differentially abundant microbial taxa and metabolic pathways. | Used to discover microbiome signatures associated with conditions like IBD in multi-cohort data. |
| TCGA/ICGC/CPTAC [69] | Data Archive | Large-scale, multi-omics reference datasets with clinical annotations. | Provide benchmark data for developing and testing integration methods in a cancer context. |
The choice of a data integration strategy is pivotal for the validation of microbiome biomarkers. BERT emerges as a powerful solution for large-scale studies with significant data incompleteness, offering superior speed and data retention. For projects where data privacy across institutions is a primary constraint, Federated Harmony provides a secure and effective alternative without sacrificing performance. The continued development and rigorous benchmarking of these computational tools are essential for overcoming the persistent challenge of batch effects, ultimately paving the way for reliable and reproducible microbiome-based diagnostics.
The pursuit of reliable microbiome-based diagnostics is critically hampered by a replicability crisis, largely driven by methodological heterogeneity in sample processing and sequencing. Inconsistent practices at every stage, from sample collection to computational analysis, introduce substantial variability that obscures true biological signals and impedes the validation of biomarkers across independent cohorts. This guide objectively compares the impact of standard versus standardized protocols, providing experimental data that underscore the urgency of adopting unified methodologies to advance robust diagnostic development.
Comparative Impact of Methodological Heterogeneity
The tables below summarize key experimental findings demonstrating how methodological choices introduce significant variability, affecting the replicability of microbiome studies.
Table 1: Impact of Sample Collection Timing on Microbial Composition Replicability
| Experimental Factor | Standard Practice | Controlled/Standardized Practice | Observed Effect on Microbiome | Quantitative Impact |
|---|---|---|---|---|
| Time of Collection | Ad hoc, unreported timing | Fixed morning collection | Dramatic population shifts throughout the day [70] | ~80% of microbiome composition differed in mouse models over 4 hours [70] |
| Data Replicability | Low; conflicting conclusions between researchers | High; consistent findings across experiments | Sample timing alone can explain failure to replicate results [70] | Conclusions dependent on collection time (morning vs. evening) [70] |
Table 2: Impact of Sample Processing and Computational Analysis on Data Output
| Experimental Factor | Standard Practice | Controlled/Standardized Practice | Observed Effect on Data | Quantitative Impact |
|---|---|---|---|---|
| Cell Clustering in scRNA-seq | A priori clustering applied to all cells | Annotation-free, cell-subset-specific analysis (e.g., MrVI) [71] | Reveals clinically relevant stratifications missed by oversimplification [71] | Detects disease-associated subpopulations (e.g., in COVID-19, IBD) invisible to standard methods [71] |
| Data Visualization & Aggregation | Aggregated taxa (e.g., "others" category), stacked bar charts [72] | Visualization of all OTUs/ASVs without aggregation (e.g., Snowflake) [72] | Preserves less abundant taxa and unique sample-specific microbes [72] | Enables identification of the core microbiome vs. sample-specific taxa [72] |
Detailed Experimental Protocols
Protocol for Investigating Diurnal Microbiome Variation
This protocol is designed to quantify the effect of sample collection timing on microbiome composition and subsequent analysis.
- Objective: To determine the intra-day variability of the gut microbiome and its impact on study replicability.
- Sample Collection:
- Cohort: Animal models (e.g., mice) or human participants.
- Schedule: Collect fecal samples at multiple, strictly timed intervals over a 24-hour period (e.g., every 4 hours). For human studies, control for diet and sleep cycles.
- Metadata Recording: Record exact collection time for all samples. This parameter is often overlooked in standard practice [70].
- DNA Extraction & Sequencing:
- Process all samples using the same DNA extraction kit and protocol to eliminate kit-to-kit variability.
- Perform 16S rRNA gene sequencing (e.g., V4 region) on all samples in a single, randomized sequencing run to avoid batch effects.
- Bioinformatic Analysis:
- Data Interpretation: The expectation is that samples collected closer in time will cluster together in a PCoA plot, while those collected 12 hours apart will show significant compositional dissimilarity, demonstrating the profound effect of collection timing.
Protocol for Annotation-Free Single-Cell Analysis
This protocol leverages the MrVI tool to identify sample stratifications based on cellular and molecular differences without pre-defined cell states.
- Objective: To perform exploratory and comparative analysis of multi-sample single-cell genomics data without relying on predefined cell clusters.
- Software Environment Setup:
- Install the
scvi-toolsPython package, which includes the MrVI module [71]. - Prepare input data: a counts matrix of gene expression from multiple samples with associated sample-level metadata (e.g., donor ID, disease status, perturbation).
- Install the
- Model Training and Execution:
- Model Initialization: Configure the MrVI model with the gene expression matrix and sample identifiers as the target covariate. Nuisance covariates (e.g., batch effect) can be specified for correction [71].
- Training: Train the deep generative model to learn latent representations
u_n(cell state) andz_n(cell state plus sample-level effects) [71].
- Exploratory Analysis:
- Compute a sample-by-sample distance matrix for each cell. MrVI performs a counterfactual analysis, estimating each cell's state had it come from a different sample [71].
- Use hierarchical clustering on these distance matrices to reveal de novo sample groupings driven by specific cellular subpopulations.
- Comparative Analysis:
- For differential expression (DE), MrVI uses the decoder network to compare gene expression profiles of cells from different sample groups (e.g., case vs. control) in the latent space, reporting effect sizes (fold change) without pre-clustering [71].
- For differential abundance (DA), the model compares the aggregate posteriors of cell states between sample groups [71].
Visualizing the Standardization Crisis and Solution Pathway
The following diagram illustrates the divergent outcomes of heterogeneous versus standardized research workflows, highlighting key points of failure and correction.
Pathway to Microbiome Diagnostic Validation
The Scientist's Toolkit: Key Research Reagent Solutions
For researchers designing microbiome biomarker validation studies, the selection of consistent reagents and computational tools is paramount. The following table details essential solutions for minimizing technical variability.
Table 3: Essential Research Reagents and Tools for Standardized Microbiome Research
| Item Name/ Category | Function & Application | Standardization Benefit |
|---|---|---|
| Standardized DNA Extraction Kit | Lyses microbial cells and purifies genomic DNA from complex samples (e.g., stool, skin swabs). | Minimizes batch-to-batch and kit-to-kit variability in extraction efficiency and inhibitor removal, crucial for cross-study comparisons [73]. |
| 16S rRNA Gene Sequencing Primers | Amplifies hypervariable regions for taxonomic profiling of bacterial communities. | Using the same primer set (e.g., V4) across a study and consortium ensures amplification of the same phylogenetic breadth, reducing bias [73]. |
| MrVI Software Tool | A deep generative model for exploratory and comparative analysis of multi-sample single-cell genomics data. | Identifies sample stratifications and differential expression/abundance without pre-clustering, revealing biological signals masked by oversimplified analysis [71]. |
| Snowflake R Package | Visualizes microbiome abundance tables as multivariate bipartite graphs without taxonomic aggregation. | Displays every observed OTU/ASV, preventing loss of low-abundance taxa and enabling clear identification of core vs. sample-specific microbes [72]. |
| Stable Reference Materials | Commercially available or community-developed mock microbial communities with known composition. | Serves as an internal control across experiments to track and correct for technical noise introduced during sample processing and sequencing [73]. |
The close association between gut microbiota dysbiosis and human diseases is increasingly recognized, holding significant promise for the development of non-invasive diagnostic tools. However, the field faces substantial challenges in identifying reliable microbial biomarkers, as contradictory results frequently emerge across different studies due to confounding batch effects and biological variability. These inconsistencies stem from multiple factors: different studies employ various experimental and computational methods during sample collection, processing, and data generation, causing extensive biases in microbial profiles. Additionally, microbial abundance varies substantially across studies due to divergence in community composition and structure, which may lead to false interactions and network structures. The lack of unbiased data integration methods has consequently impeded the discovery of disease-associated microbial biomarkers from different cohorts, limiting their clinical application [74].
Traditional approaches for identifying disease-related biomarkers have primarily relied on detecting differentially abundant microbial taxa between healthy and diseased groups. However, these abundance-based methods often fail to account for the complex ecological interactions within microbial communities, where species do not exist in isolation but rather form intricate networks of cooperation and competition. Furthermore, statistical tools developed to remove batch effects in other omics data, such as combat and limma, exhibit poor performance when applied to microbial datasets due to the unique sparsity characteristics of microbiome data. This analytical gap has driven the development of novel computational approaches that can more effectively integrate multi-cohort microbiome data while accounting for microbial interaction patterns [74].
Network-based approaches represent a paradigm shift in microbiome analysis, as they focus on the shifts in microbial interaction networks rather than simply comparing individual taxon abundances. By constructing co-occurrence networks that model the ecological relationships between microbial taxa, these methods can identify key structural changes in microbial communities associated with disease states. The application of co-occurrence networks simplifies the identification of disease-related biomarkers and can improve clinical prediction models. Nevertheless, significant challenges remain in network-based microbiome analysis, especially when integrating networks from multiple cohorts with different sample sizes and experimental conditions [74].
NetMoss Algorithm: Core Principles and Methodological Framework
NetMoss (Network Module Structure Shift) is an algorithm specifically designed to identify robust biomarkers by assessing shifts in microbial network modules between different biological states. The fundamental premise of NetMoss is that the importance of bacteria in disease states can be evaluated by their role in transforming network structure, focusing on preserved and altered microbial interactions rather than merely abundance changes. This approach addresses a critical limitation of traditional differential abundance analysis, which often fails to account for the complex ecological relationships within microbial communities [74] [75].
The algorithm operates on the principle that microbial species in the human gut form an interconnected network through cooperative and competitive relationships, and perturbations associated with disease states can alter this overall network structure. NetMoss quantifies these structural alterations through a NetMoss score, which serves as an indicator to measure interindividual variation of the human microbiome within a network structure framework under different states. This network-based perspective enables researchers to move beyond analyzing microbial taxa in isolation and instead understand how disease-associated dysbiosis affects the entire microbial ecosystem [75].
A key innovation of NetMoss is its specialized approach to handling batch effects during data integration. Unlike general batch correction methods that may inadvertently remove biological signal, NetMoss employs a network-based integration strategy that preserves relevant biological variation while minimizing technical artifacts. This capability is particularly valuable in microbiome research, where combining datasets from different studies is essential for achieving sufficient statistical power but introduces substantial technical variability [74].
Workflow and Computational Implementation
The NetMoss algorithm follows a structured workflow that can be divided into several key stages, each addressing specific challenges in microbiome data integration and network analysis.
Data Integration with Univariate Weighting: NetMoss first addresses batch effects during cohort integration through a univariate weighting method. This approach assigns greater weight to larger datasets to increase their contribution to the final integrated network, effectively preventing large studies from being overshadowed by smaller ones in the combined analysis. Validation through pairwise permutation tests has demonstrated that this weighting method efficiently highlights the strength of large studies in the final network and reduces bias in the integration process. The method shows significantly higher correlation between network distance and sample dissimilarity compared to traditional approaches, indicating better performance in describing variation among studies [74].
Network Construction and Module Detection: Following data integration, NetMoss constructs co-occurrence networks for both healthy and disease states. The algorithm identifies network modules—groups of highly interconnected taxa that may represent functional units within the microbial community. These modules are detected using topological properties rather than abundance patterns, focusing on the preserved and altered microbial interactions between states [74].
Calculation of NetMoss Scores: The core analytical step involves calculating NetMoss scores, which quantify the importance of each taxon based on its role in transforming network structure from healthy to disease state. The algorithm measures the extent to which each species' network connections and module affiliations shift between conditions. Taxa with high NetMoss scores are those that undergo significant changes in their network positioning, suggesting their potential importance in disease-associated dysbiosis [74] [75].
Biomarker Identification and Validation: Finally, NetMoss identifies robust biomarkers by selecting taxa with NetMoss scores exceeding a statistically determined threshold. These candidates can then be validated through classification models that assess their diagnostic performance in distinguishing disease from healthy states across multiple cohorts [76].
Table 1: Key Stages in the NetMoss Algorithm Workflow
| Stage | Key Operations | Output |
|---|---|---|
| Data Integration | Univariate weighting of datasets based on sample size | Batch-effect reduced combined dataset |
| Network Construction | Co-occurrence network modeling for healthy and disease states | Microbial interaction networks for each condition |
| Module Detection | Identification of highly interconnected taxa groups | Network modules representing functional units |
| Score Calculation | Quantification of structural shifts for each taxon | NetMoss scores indicating topological importance |
| Biomarker Validation | Performance assessment in classification models | Validated microbial biomarkers with diagnostic potential |
Diagram 1: NetMoss Algorithm Workflow - This flowchart illustrates the key stages in the NetMoss algorithm, from data integration to biomarker validation.
Performance Comparison with Alternative Network-Based Methods
Comparative Framework and Evaluation Metrics
When evaluating network-based biomarker discovery algorithms, several performance dimensions must be considered: classification accuracy, robustness across studies, biomarker compactness (number of identified features), and computational efficiency. NetMoss has been systematically compared against several other network-based approaches, including Neighbor Shift (NESH), Jaccard Edge Index (JEI), NetShift, and the more recently developed NetEnsa and Stiffness Network Analysis (SNA) [74] [77] [75].
These comparisons typically employ standardized evaluation frameworks using both simulated and real microbiome datasets. For simulated data, benchmark studies often generate known network structures with introduced perturbations to simulate disease states, allowing precise assessment of each algorithm's ability to recover the true driver taxa. For real-world validation, researchers use multiple disease-associated microbiome datasets (such as inflammatory bowel disease, colorectal cancer, Parkinson's disease, and autism spectrum disorder) with known clinical outcomes to evaluate diagnostic performance through metrics including area under the curve (AUC), accuracy, and biomarker consistency across studies [74] [76] [75].
The classification performance is typically measured using cross-validation approaches that assess how well biomarkers identified in one dataset generalize to independent cohorts. This validation strategy is particularly important for establishing clinical utility, as it tests the real-world scenario where diagnostic models must perform consistently across diverse patient populations and study designs [78] [76].
Comparative Performance Results
Table 2: Performance Comparison of Network-Based Biomarker Discovery Methods
| Method | Key Approach | Reported AUC Range | Biomarker Compactness | Key Limitations |
|---|---|---|---|---|
| NetMoss | Network module structure shift assessment | 0.79-0.82 [76] [79] | Moderate to High [74] | May identify excessive potential biomarkers [77] |
| NetEnsa | Multi-stage ensemble of co-occurrence networks | ~0.92 [77] | High (Avg. 18.22 nodes) [77] | Complex implementation; extensive computational requirements [77] |
| SNA | Stiffness network analysis measuring network resilience | Not fully reported [75] | Not fully reported | Limited validation across diverse disease contexts [75] |
| NetShift | Analysis of changes in community structure | Not fully reported | Low to Moderate [77] | Threshold delineation may include non-essential nodes [77] |
| NESH/JEI | Node-level network change metrics | Lower than NetMoss on simulated data [74] | Not reported | Inferior performance in identifying transited submodules [74] |
In head-to-head comparisons on simulated datasets, NetMoss has demonstrated superior performance in identifying driver bacteria associated with state transition. One benchmark study found that NetMoss correctly identified 86.7% of transited submodules in a perturbed network, outperforming both NESH and JEI methods, particularly as noise levels increased [74]. This robust performance under noisy conditions is particularly valuable for real-world microbiome data, which often contains substantial technical and biological variability.
When evaluating biomarker compactness, NetMoss tends to identify a moderate to high number of candidate biomarkers. While this comprehensive approach helps ensure important taxa aren't overlooked, it may present practical challenges for experimental validation and clinical implementation. In contrast, the newer NetEnsa algorithm demonstrates higher compactness, identifying fewer key nodes (average of 18.22 across 9 datasets) while maintaining high classification accuracy (AUC ~0.92) [77]. However, this improved compactness comes with increased computational complexity and implementation challenges.
For real-world disease applications, NetMoss has consistently demonstrated strong performance across multiple conditions. In Parkinson's disease research, a NetMoss-based classification model incorporating 11 optimized genera demonstrated high performance in distinguishing patients from healthy controls [76]. Similarly, in inflammatory bowel disease (IBD) research, NetMoss successfully identified stage-specific microbial biomarkers that effectively stratified patients according to disease severity, achieving an AUC of 0.79 in predictive models [79].
Diagram 2: Method Comparison Framework - This diagram illustrates the performance ranking of network-based biomarker discovery methods based on comparative studies.
Experimental Applications and Validation Protocols
Disease-Specific Implementation Case Studies
NetMoss has been successfully applied to identify microbial biomarkers across a spectrum of human diseases, demonstrating its versatility and robustness in different pathological contexts. In Parkinson's disease (PD) research, researchers performed a meta-analysis integrating six 16S rRNA gene amplicon sequencing datasets from five independent studies encompassing 550 PD and 456 healthy control samples. After identifying significant alterations in microbial composition and diversity, they utilized NetMoss to pinpoint potential biomarkers of PD. The resulting classification model incorporated 11 optimized genera and demonstrated high performance in distinguishing PD patients from controls, though the specific AUC values were not reported in the available excerpt. The study further linked these microbial alterations to functional pathways relevant to neurodegeneration, offering insights into potential therapeutic interventions [76].
In inflammatory bowel disease (IBD), researchers applied NetMoss to decode disease progression and establish a dynamic biomarker atlas for personalized disease stratification. The study recruited 97 participants (74 IBD patients and 23 healthy controls) and collected fecal samples for 16S rRNA sequencing. Using NetMoss, the researchers identified discriminative taxa specific to different IBD stages: Bifidobacterium.catenulatum and Bacteroides.fragilis in remission; Streptococcus.gallolyticus, Veillonella.atypica and Clostridium.butyricum in mild disease; Blautia.obeum in moderate disease; and Bacteroides.uniformis in severe IBD. The microbial biomarkers alone achieved an AUC of 0.79 in predictive models for disease staging, demonstrating the clinical utility of NetMoss-derived biomarkers [79].
For colorectal cancer (CRC), researchers collected 2,742 gut microbiota samples from seven independent studies representing three different countries. The initial analysis revealed significant heterogeneity among studies, with very few differentially abundant bacteria shared across multiple studies. After applying NetMoss, they identified more consistent biomarker patterns that transcended batch effects and cohort-specific biases. While specific AUC values for CRC classification were not provided in the excerpt, the authors reported that NetMoss demonstrated great advantages in identifying disease-related biomarkers compared to previous approaches in comprehensive evaluations on both simulated and real datasets [74].
Experimental Protocols and Methodological Details
The standard protocol for applying NetMoss to microbiome biomarker discovery follows a systematic process with specific quality control and analytical steps:
Sample Preparation and Sequencing: Experimental studies typically collect fecal samples from both case and control participants, followed by DNA extraction using commercial kits such as the QIAamp DNA Stool Mini Kit. The 16S rRNA gene amplification targets variable regions (typically V3-V4 or V4) using platform-specific primers, followed by sequencing on Illumina platforms (MiSeq or similar). The sequencing depth varies by study but typically achieves at least 40,000-50,000 reads per sample after quality control [76] [79].
Data Preprocessing and Quality Control: Raw sequencing data undergoes preliminary quality control including removal of barcodes, primers, and chimeras, followed by splicing and filtering of low-quality sequences. Bioinformatic processing includes clustering into operational taxonomic units (OTUs) or amplicon sequence variants (ASVs), taxonomic assignment using reference databases, and generation of abundance tables. Studies typically achieve high annotation efficiency (>90% OTU annotation) [79].
Network Construction and Analysis: For NetMoss analysis, co-occurrence networks are constructed separately for case and control groups using correlation measures. The algorithm employs a univariate weighting method during data integration to address batch effects, assigning greater weight to larger datasets to increase their contribution to the final integrated network. This approach has been validated to show significantly higher correlation between network distance and sample dissimilarity compared to traditional methods [74].
Validation and Statistical Analysis: Identified biomarkers are typically validated using machine learning classifiers to assess their diagnostic performance. Common approaches include cross-validation within the discovery cohort and external validation in independent datasets when available. Model performance is evaluated using standard metrics including AUC, accuracy, sensitivity, and specificity [76] [79].
Table 3: Essential Research Resources for NetMoss Implementation
| Resource Category | Specific Tools/Solutions | Application Context |
|---|---|---|
| Sequencing Platforms | Illumina MiSeq platform [76] | 16S rRNA gene amplicon sequencing |
| DNA Extraction Kits | QIAamp DNA Stool Mini Kit [79] | Microbial gDNA extraction from fecal samples |
| Primer Systems | 515F/806R (V4 region); 341F/806R (V3-V4 region) [76] | 16S rRNA gene amplification targeting specific variable regions |
| Computational Frameworks | R or Python ecological network analysis pipelines | Network construction and module detection |
| Bioinformatics Tools | QIIME 2, Mothur, DADA2 | Microbiome data preprocessing and OTU/ASV clustering |
| Validation Approaches | Machine learning classifiers (SVM, Random Forest) | Biomarker performance assessment and clinical utility estimation |
The successful implementation of NetMoss requires integration of both experimental and computational resources. For experimental validation, the selection of appropriate primer systems targeting specific 16S rRNA variable regions is critical, as different regions provide varying taxonomic resolution and amplification efficiency. The Illumina MiSeq platform has emerged as the dominant sequencing technology for these applications, providing the required read depth and quality for robust microbiome profiling [76].
On the computational side, implementation requires specialized pipelines for network construction and analysis. While the search results don't specify the exact software implementation of NetMoss, successful applications typically build upon standard microbiome analysis workflows using QIIME 2 or similar platforms for initial data processing, followed by custom R or Python scripts for the network analysis components. For validation studies, machine learning frameworks such as support vector machines (SVM) or random forests are commonly employed to assess the diagnostic performance of identified biomarkers [79].
For researchers seeking to implement NetMoss in their biomarker discovery workflows, it is essential to ensure adequate sample sizes across multiple cohorts to achieve sufficient statistical power. The algorithm's strength in batch effect correction makes it particularly valuable for meta-analyses combining data from different studies, but this advantage is only realized when sufficient datasets are available for integration. Additionally, careful attention must be paid to parameter selection for network construction, as different correlation measures and thresholding approaches can influence the resulting network topology and subsequent biomarker identification [74].
NetMoss represents a significant advancement in network-based approaches for microbial biomarker discovery, effectively addressing the critical challenge of batch effects in multi-cohort integration while capturing biologically relevant shifts in microbial community structure. Through its specialized network module structure shift assessment and univariate weighting method for data integration, NetMoss demonstrates consistent performance across diverse disease contexts including Parkinson's disease, inflammatory bowel disease, and colorectal cancer.
When compared to alternative network-based methods, NetMoss shows strengths in robustness and interpretability, though newer ensemble approaches like NetEnsa may offer advantages in biomarker compactness and classification accuracy for specific applications. The method's ability to identify biomarkers that consistently perform across validation cohorts highlights its value for developing clinically applicable diagnostic tools.
Future developments in network-based biomarker discovery will likely focus on enhancing computational efficiency, improving biomarker compactness without sacrificing sensitivity, and integrating multi-omics data layers to provide more comprehensive insights into host-microbiome interactions in health and disease.
The human gut microbiome shows great promise as a source of biomarkers for non-invasive disease diagnosis and stratification. However, the clinical application of gut microbial signatures faces a significant challenge: individual variability in host factors such as genetics, diet, medication use, and geography can dominate gut microbiome alterations and confound disease-specific signals [4]. This variability often leads to inconsistent findings across studies and impedes the development of robust, generalizable microbiome-based diagnostics. The interpretation of microbial signatures must therefore account for these host factors to achieve reliable performance across diverse populations. This guide compares approaches for microbial signature interpretation, with a focus on their capacity to control for host variability and ensure valid diagnostic conclusions.
Comparative Analysis of Interpretation Approaches
The table below objectively compares the core methodologies for interpreting microbial signatures in microbiome biomarker studies, highlighting their strengths and limitations in accounting for host factors.
Table 1: Comparison of Microbial Signature Interpretation Approaches
| Interpretation Approach | Core Methodology | Handling of Host Confounders | Cross-Cohort Validation (AUC Range) | Key Advantages | Principal Limitations |
|---|---|---|---|---|---|
| Associative (Standard) ML | Uses supervised learning (e.g., Random Forest, Lasso) to rank diseases based on posterior probability ( P(Disease|Evidence) ) [4] [80]. | Limited adjustment; confounders like drugs or diet can create spurious correlations [4] [80]. | Intestinal diseases: ~0.73 AUC [4]. Non-intestinal: Lower performance. | Simple implementation; strong performance in single-cohort validation [4]. | Prone to confounding; may identify statistically strong but causally irrelevant biomarkers [80]. |
| Counterfactual Causal Inference | Reformulates diagnosis as counterfactual inference, estimating the likelihood a disease caused the symptoms via hypothetical interventions [80]. | Explicitly models causal pathways; disregards diseases that could not have caused symptoms, even if correlated [80]. | Achieved ~77% diagnostic accuracy, outperforming standard associative algorithm and placing in top 25% of doctors [80]. | Mimics clinical reasoning; reduces spurious diagnoses from confounders; improves rare disease diagnosis [80]. | Requires explicit causal knowledge/dag; computationally intensive; more complex implementation [80]. |
| Cross-Cohort Meta-Analysis | Uses tools like MMUPHin to harmonize data from multiple cohorts, identifying shared microbial signatures across diverse populations [81] [82]. |
Identifies signatures robust to population-specific confounders (geography, technical variations) via batch effect correction [81]. | CRC MRSα: 0.619 - 0.824 AUC across 8 cohorts [81]. | Directly tests generalizability; generates signatures stable across populations and study designs [81]. | Requires multiple, large-scale cohorts; cannot resolve causal relationships. |
| Microbial Risk Score (MRS) | Constructs risk scores based on α-diversity of a core set of disease-associated species identified via cross-cohort analysis [81]. | The core species (e.g., P. micra, F. nucleatum) are selected specifically for their consistent association across different host populations [81]. | Varies between 0.619 and 0.824 across eight cohorts for Colorectal Cancer [81]. | More interpretable and better validated than complex ML models; simple, translatable metric [81]. | May overlook important functional or strain-level variations. |
Experimental Protocols for Validated Microbial Signatures
Protocol for Cross-Cohort Meta-Analysis and MRS Construction
This protocol, derived from a 2025 meta-analysis on colorectal cancer (CRC), details the steps for identifying host-factor-resistant microbial signatures [81].
- Cohort Assembly and Harmonization: Perform a meta-analysis of multiple metagenomic datasets, encompassing a total of 570 CRC cases and 557 controls from diverse geographical regions and populations. Use the
MMUPHintool to correct for cross-cohort batch effects arising from technical variations and population-specific confounders [81]. - Identification of Core Microbial Signatures: Apply statistical meta-analysis to identify differentially abundant microbial species that are consistently associated with the disease (e.g., CRC) across the majority of independent cohorts. The 2025 study identified a core set of six species: Parvimonas micra, Clostridium symbiosum, Peptostreptococcus stomatis, Bacteroides fragilis, Gemella morbillorum, and Fusobacterium nucleatum [81].
- Microbial Risk Score (MRS) Calculation: Construct a risk score based on the α-diversity of the validated sub-community. The MRSα is calculated as the Shannon diversity of the core set of disease-associated species. This method was found to be more interpretable and better validated across cohorts than scores built using weighted summation or complex machine learning algorithms [81].
- Validation: Conduct cohort-to-cohort validation, where a model trained on one cohort is tested on all other hold-out cohorts. The performance is measured using the Area Under the Receiver Operating Characteristic Curve (AUC) to demonstrate transferability [81].
Protocol for Systematic Cross-Cohort Validation of Classifiers
This protocol provides a framework for evaluating the generalizability of microbiome-based classifiers across 20 different diseases, as established in a large-scale 2023 study [4].
- Cohort Selection and Quality Control: Screen available cohorts (e.g., from the GMrepo v2 database) with strict inclusion criteria: case-control design, at least 15 valid samples per group, and no recent antibiotic or probiotic use. The final analysis included 83 cohorts with 5,984 cases and 3,724 controls [4].
- Data Preprocessing and Confounder Adjustment: Standardize microbial composition data (species or genus-level relative abundances). For each cohort, test for distributions of host confounders (age, gender, BMI) between cases and controls. For confounders with a significant difference (p-value < 0.05), adjust the microbial data using the
removeBatchEffectfunction from the 'limma' R package [4]. - Model Training and Validation:
- Intra-cohort Validation: Train machine learning classifiers (e.g., Lasso, Random Forest) on a single cohort and evaluate performance using 5-fold cross-validation repeated 3 times.
- Cross-cohort Validation: Train a classifier on one cohort and directly apply it to predict disease status in all other independent cohorts of the same disease. Record the AUC for each pairwise validation [4].
- Performance Analysis and Sample Size Estimation: Analyze the cross-cohort performance patterns across different disease categories (intestinal, metabolic, autoimmune, etc.). For diseases with poor performance, build a "combined-cohort" classifier trained on data merged from multiple cohorts and estimate the sample size required to achieve a cross-cohort AUC of >0.7 [4].
Visualizing Workflows and Causal Relationships
Workflow for Robust Microbial Signature Discovery
The diagram below illustrates the integrated workflow for discovering and validating microbial signatures that are robust to individual host variability.
Causal vs. Associative Diagnostic Reasoning
This diagram contrasts the standard associative model of diagnosis with the counterfactual causal model, highlighting how the latter accounts for confounding host factors.
The table below lists key reagents, databases, and computational tools essential for conducting research on microbial signatures and accounting for host variability.
Table 2: Key Research Reagents and Resources for Microbial Signature Studies
| Resource Name | Type | Primary Function in Research | Relevance to Host Factor Analysis |
|---|---|---|---|
| MMUPHin R Package [81] [4] | Computational Tool | Performs meta-analysis and batch effect correction of microbiome data from multiple cohorts. | Directly adjusts for batch effects arising from host geography, population, and study design. |
| BugSigDB [83] | Curated Database | A community-editable database of manually curated microbial signatures from published differential abundance studies. | Enables comparison of signatures across studies to identify those robust to different host populations. |
| CAMI Benchmarking [84] | Benchmarking Initiative | Provides critical assessment of metagenome interpretation tools using realistic datasets to ensure reproducibility. | Helps validate tools and methods against standardized data, controlling for technical variation. |
| SHAP (SHapley Additive exPlanations) [84] | Explainable AI (XAI) Tool | A model-agnostic method for interpreting the output of complex machine learning models. | Identifies which microbial features (and potentially correlated host factors) most drive a model's prediction. |
| EXPERT [84] | ML Model (Transfer Learning) | A deep learning model pre-trained on large databases and fine-tuned for specific tasks like CRC staging. | Transfer learning helps models generalize better to new populations with different host factor distributions. |
| Fluorescently-Tagged Bacteroides [85] | Biological Model System | Engineered gut bacterial strains that express fluorescent proteins for spatial tracking in the gut of model organisms. | Allows direct investigation of how host factors (e.g., gut anatomy, colonization history) affect microbial localization. |
Longitudinal study designs are essential for decoding the complex role of the microbiome in disease progression. Unlike cross-sectional approaches that provide a single snapshot, longitudinal sampling tracks microbial communities within the same hosts over multiple timepoints, capturing their dynamic responses to disease development, treatment interventions, and environmental exposures [86]. This temporal dimension is crucial for understanding whether microbial shifts precede disease onset (suggesting potential causative roles) or simply coincide with disease states [87]. However, these studies present significant analytical challenges due to the high-dimensionality of microbiome data (typically hundreds to thousands of microbial taxa), frequent missing values from irregular sampling, and substantial inter-individual variability that can obscure consistent temporal patterns [88] [87].
The compositional nature of microbiome data further complicates analysis, as abundances are relative rather than absolute [89]. This means that an observed increase in one taxon's abundance necessarily corresponds to decreases in others, creating mathematical constraints that standard statistical methods violate. Additionally, microbiome data are characterized by zero-inflation (many taxa have no recorded abundance in most samples) and overdispersion (variance exceeds mean abundance) [90] [91]. These characteristics demand specialized analytical frameworks that can distinguish true biological signals from technical artifacts while respecting the intrinsic structure of microbial community data.
Comparative Analysis of Methodological Frameworks
Multiple advanced computational frameworks have been developed specifically to address the analytical challenges of longitudinal microbiome studies. The table below compares three prominent approaches that represent distinct methodological paradigms.
Table 1: Comparison of Longitudinal Microbiome Analysis Frameworks
| Framework | Core Methodology | Primary Applications | Temporal Handling | Key Advantages |
|---|---|---|---|---|
| SysLM [88] | Deep learning (Temporal Convolutional Network + BiLSTM) with causal inference | Missing value imputation, classification, multi-type biomarker discovery | Captures temporal causality and long-term dependencies | Integrates deep learning with causal modeling for enhanced interpretability |
| LP-Micro [87] | Polynomial group lasso with machine learning (XGBoost, DNN) and permutation testing | Feature screening, disease outcome prediction, critical time point identification | Groups taxonomic effects across timepoints as unified trajectories | Identifies incident disease-related taxa and critical predictive windows |
| coda4microbiome [89] | Compositional data analysis with penalized regression on pairwise log-ratios | Microbial signature identification, prediction modeling | Summarizes log-ratio trajectories via area under the curve | Respects compositional nature of data; provides interpretable log-ratio signatures |
Performance Benchmarking
Each framework demonstrates distinct strengths in validation studies. SysLM shows superior performance in imputation tasks, achieving mean absolute error (MAE) values below 0.15 and R² values exceeding 0.85 across multiple datasets including DIABIMMUNE, IBD, and T2D cohorts [88]. Its integration of temporal convolutional networks with bidirectional long short-term memory (BiLSTM) architecture enables robust capture of both forward and backward temporal dependencies in sparse microbial data.
LP-Micro demonstrates exceptional prediction accuracy in clinical applications, achieving area under the curve (AUC) values of 0.89-0.94 for predicting early childhood caries using oral microbiome trajectories and 0.79-0.86 for forecasting weight loss following bariatric surgery using gut microbiome dynamics [87]. The framework's polynomial group lasso implementation successfully identified Streptococcus mutans as most predictive of dental caries at approximately 39 months, aligning with clinical understanding of disease progression.
coda4microbiome maintains compositional robustness while achieving competitive prediction performance, with cross-validated accuracy of 0.82-0.91 for distinguishing Crohn's disease patients from controls using microbial balances [89]. By construction, its log-ratio approach ensures invariance to sample sequencing depth and prevents artifacts introduced by analyzing relative abundances as independent variables.
Table 2: Experimental Performance Metrics Across Methodologies
| Framework | Datasets Validated | Primary Metrics | Reported Performance | Clinical/Biological Insights |
|---|---|---|---|---|
| SysLM [88] | DIABIMMUNE, IBD, T2D, cystic fibrosis | MAE, MSE, AUC for classification | MAE: 0.10-0.15; AUC: 0.88-0.93 | Revealed novel microbial mechanisms in ulcerative colitis |
| LP-Micro [87] | Early childhood caries, bariatric surgery | AUC, precision-recall, feature importance scores | AUC: 0.79-0.94 depending on application | Identified 39 months as critical window for caries prediction |
| coda4microbiome [89] | Crohn's disease, infant microbiome development | Prediction accuracy, balance interpretation | Accuracy: 0.82-0.91; robust to compositionality | Discovered microbial balances distinguishing disease states |
Experimental Protocols and Workflows
Systematic Longitudinal Microbiome Analysis (SysLM) Protocol
The SysLM framework employs a two-module architecture for comprehensive longitudinal analysis. The SysLM-I module handles missing data imputation through an advanced deep learning approach:
Step 1: Data Preprocessing
- Normalize raw sequence counts using cumulative sum scaling (CSS) to address varying sequencing depths
- Integrate metadata including patient demographics, clinical variables, and sampling timepoints
- Apply three feature enhancement strategies to amplify biological signals: alpha-diversity preservation, beta-diversity maintenance, and temporal smoothing
Step 2: Temporal Pattern Capture
- Process time-series data through Temporal Convolutional Network (TCN) to capture long-range dependencies
- Simultaneously process sequences through Bidirectional LSTM (BiLSTM) to model forward and backward temporal relationships
- Generate imputed values while preserving ecological characteristics through specialized loss functions:
Loss_SysLM-I = loss_r + w_α * loss_α + w_β * loss_β [88]
where loss_r measures reconstruction error, loss_α preserves Shannon diversity, and loss_β maintains Bray-Curtis distance structure
Step 3: Causal Inference (SysLM-C Module)
- Construct three causal spaces to identify differential, network, core, dynamic, disease-specific, and shared biomarkers
- Apply counterfactual reasoning to estimate microbial effects on disease progression
- Validate causal relationships through stability selection and cross-cohort replication
The following workflow diagram illustrates the integrated SysLM framework:
Longitudinal Prediction Microbiome (LP-Micro) Protocol
The LP-Micro framework implements a streamlined workflow for predictive modeling from longitudinal microbiome data:
Step 1: Polynomial Group Lasso Feature Screening
- Represent each taxon's temporal trajectory using natural cubic splines with 3-5 degrees of freedom
- Apply group lasso regularization to select taxa whose complete temporal trajectories predict disease outcomes
- Optimize regularization parameter λ through k-fold cross-validation to maximize predictive accuracy
Step 2: Machine Learning Model Implementation
- Train multiple classifier types on selected features: Lasso, Random Forest, XGBoost, SVM, and deep learning architectures (NN, LSTM, GRU, CNN-GRU)
- Implement ensemble learning to stabilize predictions across models
- Evaluate performance via stratified cross-validation with held-out temporal windows
Step 3: Interpretable Feature Importance Testing
- Compute permutation importance scores for each selected taxon
- Generate p-values through group-wise permutation testing to assess statistical significance
- Aggregate importance scores across timepoints to identify critical predictive windows
The LP-Micro analytical workflow is visualized below:
Compositional Data Analysis (coda4microbiome) Protocol
The coda4microbiome framework addresses the compositional nature of microbiome data through log-ratio analysis:
Step 1: All-Pairs Log-Ratio Transformation
- Compute all pairwise log-ratios log(Xj/Xk) for K taxa, creating K(K-1)/2 features
- For longitudinal data, calculate area under the curve for each log-ratio trajectory to summarize temporal patterns
Step 2: Penalized Logistic Regression
- Fit elastic-net regularized models (α=0.9, λ optimized via cross-validation) to predict outcomes from log-ratios:
ĝ(E(Y)) = β_0 + Σ_{1≤j<k≤K} β_jk · log(X_j/X_k) [89]
- Apply zero-sum constraint on coefficients to ensure compositional invariance
Step 3: Microbial Signature Interpretation
- Identify the balance between groups of taxa that optimally predicts disease status
- Visualize log-ratio trajectories distinguishing cases from controls
- Validate signature stability through bootstrap resampling
Successful implementation of longitudinal microbiome studies requires carefully selected analytical tools and resources. The following table catalogues essential solutions referenced in the methodologies discussed.
Table 3: Essential Research Reagent Solutions for Longitudinal Microbiome Analysis
| Category | Specific Solution | Function/Purpose | Implementation Examples |
|---|---|---|---|
| Statistical Modeling | Zero-inflated models (ZINB, ZIG) | Account for excess zeros in count data | Modeling low-abundance taxa in sparse time-series data [91] |
| Normalization Methods | Cumulative Sum Scaling (CSS) | Correct for variable sequencing depth | metagenomeSeq normalization prior to temporal analysis [90] |
| Differential Abundance | ANCOM, ALDEx2, LinDA | Identify differentially abundant taxa | Controlling false discovery in longitudinal feature selection [90] [89] |
| Causal Inference | Counterfactual frameworks | Estimate causal microbial effects | SysLM-C module for identifying disease-contributing taxa [88] |
| Batch Correction | ComBat, Remove Unwanted Variation (RUV) | Adjust for technical variability | Harmonizing multi-center longitudinal microbiome data [90] |
| Data Integration | Multi-omic integration frameworks | Combine microbiome with metabolome/proteome | Enhancing predictive power in disease progression models [34] |
Longitudinal microbiome study designs represent a paradigm shift in understanding microbial dynamics throughout disease progression. The comparative analysis presented here demonstrates that methodological selection should be guided by specific research objectives: SysLM for comprehensive causal biomarker discovery, LP-Micro for clinical prediction modeling, and coda4microbiome for compositionally robust signature identification. Each framework provides distinct advantages for tackling the analytical challenges inherent in temporal microbiome data.
Future methodological development must address several critical frontiers. Multi-omic integration will be essential for connecting microbial dynamics with host responses through metabolomic, proteomic, and immunologic profiling [34]. Real-time adaptive sampling frameworks could optimize timing of sample collection based on emerging microbial patterns. Furthermore, standardized validation protocols across diverse populations will be necessary for clinical translation of microbiome-based diagnostics and monitoring tools. As these methodologies mature, longitudinal microbiome analyses will increasingly enable proactive healthcare interventions targeting microbial communities before irreversible disease progression occurs.
Validation Frameworks and Performance Metrics Across Disease Contexts
Multi-cohort validation has emerged as a fundamental requirement for establishing robust, generalizable diagnostic biomarkers in microbiome research. The inherent variability of the gut microbiome across populations, geographical regions, and technical platforms creates significant challenges for biomarker development that single-cohort studies cannot adequately address [4] [92]. By integrating data from multiple independent cohorts, researchers can distinguish genuine biological signals from cohort-specific noise, thereby developing diagnostic tools with enhanced clinical applicability across diverse populations.
This comparative guide examines multi-cohort validation strategies through the lens of global colorectal cancer (CRC) and inflammatory bowel disease (IBD) studies, two fields where microbiome-based diagnostics have shown particular promise. We objectively analyze the performance of various technological approaches, present structured experimental data, and detail the methodologies that have proven most effective for cross-cohort validation. The insights derived from these studies provide a strategic framework for researchers developing and validating microbiome-based diagnostics across disease states.
Performance Comparison of Multi-Cohort Validated Diagnostic Approaches
The table below summarizes the performance metrics of various diagnostic approaches that have undergone multi-cohort validation in CRC and IBD research, highlighting the relative strengths of different technological platforms.
Table 1: Performance Comparison of Multi-Cohort Validated Diagnostic Approaches
| Technology Platform | Target Condition | Cohorts Validated | Key Performance Metrics | Reference |
|---|---|---|---|---|
| cfDNA Fragmentomics | CRC | 4 hospitals (China) | AUC: 0.926, Sensitivity: 91.3%, Specificity: 82.3% | [93] |
| Universal Bacterial Markers (7 species) | CRC | 4 cohorts (USA, Austria, China, Germany/France) | AUC: 0.80, Increased to 0.88 with clinical data | [94] |
| Tumor Location-Specific Microbial Panels | CRC | 6 cohorts (global) | rCRC: AUC 91.59%, lCRC: AUC 91.69%, RC: AUC 90.53% | [95] |
| Gut Microbiome Classifiers | Intestinal Diseases | 83 cohorts (20 diseases) | Cross-cohort AUC: ~0.73 for intestinal diseases | [4] |
| FML-Corrected Metagenomic Models | CRC | 7 cohorts (global) | Superior cross-cohort robustness vs. uncorrected models | [92] |
The performance data reveals several critical trends. First, cfDNA fragmentomics demonstrates exceptionally high sensitivity (91.3%) and specificity (82.3%) for CRC detection, with consistent performance across stages I-IV [93]. Second, microbial marker panels show robust diagnostic capability across diverse populations, with performance improving when tumor location is considered or when combined with clinical variables [95] [94]. Third, gut microbiome classifiers generally maintain better cross-cohort performance for intestinal diseases compared to non-intestinal conditions, highlighting the site-specific advantage for gastrointestinal disorders [4].
Experimental Protocols for Multi-Cohort Validation
Sample Collection and Cohort Design Standards
Successful multi-cohort validation requires standardized sample collection protocols across participating centers. For CRC studies, this typically involves:
Patient Enrollment: Prospective recruitment with clearly defined inclusion/exclusion criteria across multiple medical centers. The DECIPHER-D-Colon study, for instance, enrolled participants from four different hospitals with consistent criteria: aged ≥18 years, diagnosed with CRC or benign colorectal disease, provided written informed consent, and able to provide peripheral blood samples for cfDNA extraction [93].
Control Selection: Careful matching of controls to account for potential confounders. Studies should include both healthy controls and patients with non-cancerous colorectal conditions to enhance clinical relevance [93] [94].
Sample Size Determination: Power calculations based on expected effect sizes. Simulation analyses have demonstrated that multi-cohort approaches significantly increase statistical power compared to single-cohort studies, with an estimated power of 0.88 for detecting 20% abundance changes in microbial species versus approximately 0.5 power in single-cohort studies [94].
Ethical Considerations: Centralized IRB approval with provisions for retrospective sample inclusion when appropriate. The DECIPHER-D-Colon study utilized an approved protocol that permitted retrospective inclusion of samples collected prior to the approval date to support recruitment for rare disease subgroups [93].
Metagenomic Sequencing and Analysis Workflow
For microbiome-based studies, the following standardized metagenomic workflow has been successfully applied across multiple cohorts:
Sample Preprocessing: Using KneadData for quality control and host contamination removal, with Trimmomatic for sequence quality filtering and adapter trimming (parameters: ILLUMINACLIP:TruSeq3-PE.fa:2:40:15 SLIDINGWINDOW:4:20 MINLEN:50) [92].
Taxonomic Profiling: Strain-level analysis using Sylph against a custom non-redundant strain database or MetaPhlAn for species-level classification [92].
Fecal Microbial Load (FML) Correction: Application of Microbial Load Predictor to estimate FML from species-level taxonomic profiles, significantly reducing technical confounding and improving cross-cohort model performance [92].
Data Integration: Batch effect correction using tools like the 'MMUPHin' R package with project-ID as the controlling factor to minimize technical variation between cohorts [4].
The following diagram illustrates the complete multi-cohort validation workflow for microbiome-based diagnostic studies:
Machine Learning and Statistical Validation Methods
The development of classifiers robust across cohorts requires specialized machine learning approaches:
Algorithm Selection: Random Forest and Lasso logistic regression are preferred for their performance with high-dimensional compositional data and resistance to overfitting [4]. For cfDNA fragmentomics, stacked ensemble models integrating multiple fragmentomics features have demonstrated superior performance [93].
Feature Selection: Multi-algorithm approaches combining unsupervised and supervised methods. The frailty assessment study employed five complementary algorithms: LASSO regression, VSURF, Boruta algorithm, varSelRF, and Recursive Feature Elimination, followed by intersection analysis to identify core features consistently selected across all algorithms [96].
Validation Framework: Nested cross-validation with strict separation of training and validation sets. Studies should employ leave-one-cohort-out validation where models are trained on all but one cohort and tested on the held-out cohort [94]. Sample partitioning should maintain an 8:2 training-test ratio with 100 repeated random groupings to ensure robustness [92].
Performance Assessment: Evaluation using AUC, sensitivity, specificity, and time-dependent AUC for prognostic models. For CRC detection, sensitivities should be reported across all stages (I-IV) to demonstrate consistent performance [93].
Visualization of Key Methodological Approaches
cfDNA Fragmentomics Analysis Pipeline
The following diagram details the cfDNA fragmentomics workflow that has demonstrated high accuracy in multi-center CRC detection studies:
Multi-Cohort Microbial Marker Validation Strategy
This diagram illustrates the comprehensive strategy for identifying and validating universal microbial markers across diverse populations:
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for Multi-Cohort Microbiome Studies
| Category | Specific Tool/Platform | Function in Research | Representative Use Cases |
|---|---|---|---|
| Sequencing Platforms | Illumina WGS | Whole genome metagenomic sequencing | CRC microbiome profiling across 7 global cohorts [92] |
| Taxonomic Profiling | MetaPhlAn4 | Species-level taxonomic classification | Gut microbiome analysis in 83 cohorts across 20 diseases [4] |
| Strain-Level Analysis | Sylph | High-resolution strain-level profiling | Identification of functionally heterogeneous conspecific strains in CRC [92] |
| Proteomic Profiling | SomaScan Platform | High-throughput proteomic analysis | Identification of pre-diagnostic protein markers for lymphoid malignancies [97] |
| Data Integration | MMUPHin | Batch effect correction and meta-analysis | Cross-cohort microbial association analysis [4] |
| Microbial Load Estimation | Microbial Load Predictor (MLP) | Fecal microbial load prediction from taxonomic profiles | Technical confounding reduction in multi-cohort CRC models [92] |
| Statistical Analysis | MaAsLin2 | Multivariate association modeling | Differential abundance analysis in multi-cohort studies [92] |
The evidence from global CRC and IBD studies consistently demonstrates that multi-cohort validation is not merely a final verification step but should be integrated throughout the diagnostic development pipeline. Successful strategies share several common elements: standardized protocols across participating centers, intentional cohort diversity to represent target populations, appropriate batch effect correction methods, and validation frameworks that test generalizability rather than just optimal performance.
The most robust diagnostic approaches—whether based on microbial markers, cfDNA fragmentomics, or proteomic profiles—maintain their performance across geographical, technical, and population variations when these multi-cohort principles are applied. Researchers should prioritize cross-cohort validity from the earliest stages of study design, as this approach ultimately determines the clinical utility and translational potential of microbiome-based diagnostics.
As the field advances, emerging technologies like strain-resolved metagenomics and multi-omic integration hold promise for further improving diagnostic accuracy, but their ultimate value will depend on rigorous validation across diverse populations using the principles outlined in this guide.
The Area Under the Receiver Operating Characteristic curve (AUC or AUROC) has emerged as a fundamental metric for evaluating the performance of diagnostic tests, including those based on microbiome biomarkers [98] [99]. ROC analysis provides a comprehensive framework for assessing a test's ability to discriminate between diseased and non-diseased individuals across all possible thresholds, overcoming the limitations of single sensitivity and specificity values [98] [99]. This guide objectively compares AUROC performance benchmarks across microbiome-based diagnostic studies, detailing methodological protocols and validation challenges to inform researchers and drug development professionals in the field of microbiome biomarker diagnostic validation cohort studies.
AUROC Performance Benchmarks by Disease Area
Table 1: Microbiome-Based Diagnostic Performance Across Diseases
| Disease/Condition | Reported AUROC Range | Sample Type | Key Findings | Citation |
|---|---|---|---|---|
| Colorectal Cancer (CRC) | 0.54 - 0.89 (Early CRC) | Fecal samples | Performance improved when combined with FIT; high heterogeneity between studies. | [100] |
| Crohn's Disease (CD) | 0.94 (External Validation) | Fecal samples | 20-species signature achieved high diagnostic performance in external validation. | [13] |
| Parkinson's Disease (PD) | Average 71.9% (Within-Study), 61% (Cross-Study) | Fecal samples | Models were study-specific with poor generalizability; combined datasets improved performance (AUC 68%). | [48] |
| Gastric Cancer (GC) | 0.81 (Microbiome only), 0.86 (Combined Model) | Fecal samples | Integration of 10 tumor biomarkers with microbiome data improved diagnostic accuracy. | [101] |
| Intestinal Diseases | ~0.73 (Cross-Cohort) | Fecal samples | Showed more consistent cross-cohort performance compared to non-intestinal diseases. | [4] |
| COVID-19 | 0.93 (sROC Curve) | Multiple matrices | Mass spectrometry-based diagnostics showed high aggregate accuracy across studies. | [102] |
Table 2: General Interpretive Guidelines for AUROC Values
| AUROC Value | Interpretation Suggestion | Clinical Utility Implication |
|---|---|---|
| 0.9 ≤ AUC | Excellent | High clinical utility |
| 0.8 ≤ AUC < 0.9 | Considerable | Good clinical utility |
| 0.7 ≤ AUC < 0.8 | Fair | Moderate clinical utility |
| 0.6 ≤ AUC < 0.7 | Poor | Limited clinical utility |
| 0.5 ≤ AUC < 0.6 | Fail | No discriminative power |
Methodological Protocols and Experimental Workflows
Sample Processing and Multi-Omics Sequencing
Microbiome diagnostic studies typically follow a standardized workflow from sample collection to model building, with variations depending on the omics technology employed.
Figure 1: Generalized workflow for microbiome-based diagnostic test development.
Key methodological considerations include:
Sample Collection and Storage: Fecal samples are typically collected using standardized kits and immediately frozen at -80°C to preserve microbial integrity [13] [101]. For multi-omics approaches, parallel processing of samples for DNA, RNA, and metabolomic analysis is required.
Nucleic Acid Extraction: DNA extraction utilizes kit-based methods (e.g., Guhe Stool Mag DNA Kit) with quality assessment via spectrophotometry and gel electrophoresis [101]. For metatranscriptomics, total RNA extraction includes steps for ribosomal RNA depletion to enrich for messenger RNA [13].
Sequencing Approaches:
- 16S rRNA amplicon sequencing: Targets hypervariable regions (e.g., V4) for cost-effective taxonomic profiling [101].
- Shotgun metagenomics: Provides comprehensive genomic content allowing for species-level identification and functional potential assessment [4] [13].
- Metatranscriptomics: Reveals actively expressed genes and pathways through RNA sequencing [13].
Metabolomic Profiling: Complementary metabolomic analysis using NMR spectrometry or mass spectrometry identifies microbial metabolites (e.g., short-chain fatty acids) that may serve as functional biomarkers [13].
Bioinformatics and Machine Learning Protocols
Table 3: Common Analytical Tools and Algorithms in Microbiome Diagnostics
| Analysis Type | Common Tools/Approaches | Primary Function | Considerations |
|---|---|---|---|
| Taxonomic Profiling | MetaPhlAn, QIIME 2, Vsearch | Identifies microbial taxa from sequence data | Metagenomics offers higher resolution than 16S data [4] |
| Functional Profiling | HUMAnN, Virulence Factor DB | Predicts metabolic pathways and virulence factors | Metatranscriptomics reveals actively expressed functions [13] |
| Machine Learning | Random Forest, LASSO, Ridge Regression | Builds classification models from microbiome features | Random Forest handles complex data; regression methods aid feature selection [4] [48] |
| Cross-Study Validation | SIAMCAT, MMUPHin | Evaluates model generalizability across cohorts | Critical for assessing real-world applicability [4] [48] |
Cross-Study Validation and Performance Challenges
A critical challenge in microbiome-based diagnostics is the performance degradation when models are applied to external cohorts. This phenomenon has been systematically documented across multiple diseases:
Figure 2: Cross-study validation workflow and performance challenges.
Key findings on validation challenges include:
Study-Specific Biases: Research has demonstrated that machine learning models trained on single cohorts achieve high intra-cohort validation (average AUC ~0.77) but show significantly reduced accuracy in cross-cohort validation, except for intestinal diseases which maintain ~0.73 AUC [4].
Disease-Specific Patterns: For Parkinson's disease, within-study cross-validation achieved 71.9% AUC, but cross-study validation dropped to an average of 61%, highlighting the limited generalizability of single-cohort models [48].
Technical and Biological Confounders: Variation in sequencing methodologies (16S vs. shotgun metagenomics), bioinformatic processing, and population characteristics (diet, medications, geography) significantly impact cross-study reproducibility [4] [48].
Improvement Strategies: Training models on combined datasets from multiple cohorts significantly improves generalizability, with leave-one-study-out (LOSO) validation for Parkinson's disease reaching 68% AUC [48].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Research Reagents and Platforms for Microbiome Diagnostic Studies
| Reagent/Platform | Specific Examples | Research Application | Performance Considerations |
|---|---|---|---|
| DNA Extraction Kits | Guhe Stool Mag DNA Kit | Microbial genomic DNA isolation from fecal samples | Critical for yield and quality; affects downstream sequencing [101] |
| RNA Extraction Kits | RNeasy Mini Kit (Qiagen) | Total RNA isolation for metatranscriptomics | Includes rRNA removal steps for mRNA enrichment [13] |
| Sequencing Platforms | Illumina HiSeq, NovaSeq | High-throughput DNA/RNA sequencing | Shotgun metagenomics generally outperforms 16S in classification [4] [13] |
| Metabolomics Platforms | NMR Spectrometry, LC-MS | Identification and quantification of metabolites | Reveals functional biomarkers like SCFA depletion in Crohn's [13] |
| Immunoassay Analyzers | Roche Cobas 8000 | Measurement of clinical tumor biomarkers | Enables integration of microbiome with conventional biomarkers [101] |
| Bioinformatics Tools | QIIME 2, MetaPhlAn, HUMAnN | Taxonomic and functional profiling | Standardized pipelines essential for cross-study comparisons [13] [101] |
Microbiome-based diagnostic tests show promising AUROC values across various diseases, with particularly strong performance in intestinal disorders. However, significant challenges remain in achieving consistent cross-study validation, necessitating standardized methodologies and combined-cohort modeling approaches. The integration of multi-omics data and conventional biomarkers represents a promising path toward improved diagnostic accuracy and clinical applicability. Future research should prioritize large-scale validation studies and address technical and biological confounders to advance the field of microbiome-based diagnostics toward routine clinical implementation.
The early detection of cancer is a critical objective in oncology, as it significantly increases treatment efficacy, survival rates, and overall patient outcomes [103] [104]. Within this field, biomarkers—biological molecules indicative of normal or pathological processes—serve as essential tools for screening, diagnosis, and prognosis [105] [104]. Traditionally, cancer diagnostics have relied on biomarkers such as circulating proteins and genetic mutations. However, the emerging field of oncobiomics explores the intricate relationship between the human microbiome and cancer, proposing microbial species and communities as novel diagnostic indicators [106] [107]. This guide provides a comparative analysis of microbial and traditional biomarkers for early cancer detection, framed within the context of diagnostic validation cohort research. It is designed to equip researchers and drug development professionals with objective data on the performance characteristics, methodologies, and clinical applicability of these two biomarker classes to inform research and development strategies.
Performance Comparison: Key Metrics and Clinical Data
The following tables summarize the performance characteristics of traditional and microbial biomarkers for early cancer detection, based on recent validation studies.
Table 1: Performance Metrics of Traditional Biomarkers in Early Cancer Detection
| Biomarker | Cancer Type | Key Application | Sensitivity/Specificity/Other Metrics | References |
|---|---|---|---|---|
| Carcinoembryonic Antigen (CEA) | Colorectal (CRC) | Monitoring, Prognosis | Low sensitivity for early-stage CRC (18.8%-52.2%); sensitivity ↑ to 85.3% when in panel with CA19-9, CA242, etc. | [105] |
| SEPT9 (methylated) | Colorectal (CRC) | Non-invasive Screening | Sensitivity: 76.6%; Specificity: 95.9% | [105] |
| Circulating Tumor DNA (ctDNA) - Mutation-based | Pan-Cancer (e.g., Lung) | Early Detection | Limited by tumor heterogeneity (e.g., misses ~50% of lung adenocarcinoma with EGFR test) | [108] |
| Circulating Tumor DNA (ctDNA) - Methylation-based | Pan-Cancer | Early Detection | Can detect changes occurring before gene mutation; challenges with DNA damage during analysis | [108] |
| Alpha-fetoprotein (AFP) | Liver (HCC) | Diagnostic Biomarker | Misses ~30% of hepatocellular carcinoma cases when used alone | [108] |
| Multi-factor Algorithm (GALAD) | Liver (HCC) | Early Detection | Demonstrates better performance than single biomarkers like AFP | [108] |
Table 2: Performance Metrics of Microbial Biomarkers in Early Cancer Detection
| Biomarker / Classifier | Cancer Type | Key Application | Sensitivity/Specificity/Other Metrics | References |
|---|---|---|---|---|
| Random Forest Classifier (11 microbial markers) | Colorectal Adenoma | Discriminate Adenoma from Control | AUC = 0.80 (Discovery); Avg. AUC = 0.76 (Validation across cohorts) | [109] |
| Random Forest Classifier (26 microbial markers) | Colorectal Adenoma & CRC | Discriminate Adenoma from CRC | AUC = 0.89 (Discovery); Avg. AUC = 0.89 (Validation across cohorts) | [109] |
| Fusobacterium nucleatum | Colorectal (CRC) | Carcinogenesis & Prognosis | Associated with proliferation and chemotherapy resistance; mechanistic role via FadA/Fap2 adhesins. | [106] [107] |
| Porphyromonas gingivalis | Pancreatic | Non-invasive Biomarker | Increased levels in salivary and gut microbiota of patients. | [106] [107] |
| Circulating Microbiome DNA | Pan-Cancer | Early Detection | Alterations in circulating microorganisms show promise; requires large-scale validation. | [108] |
Experimental Protocols for Biomarker Validation
Robust experimental protocols are fundamental for the discovery and validation of both traditional and microbial biomarkers. The following sections detail standard methodologies employed in validation cohort studies.
Protocol for Microbial Biomarker Analysis (16S rRNA Sequencing)
This protocol is adapted from multi-cohort validation studies for colorectal adenoma [109].
1. Sample Collection and DNA Extraction:
- Material: Collect stool samples from participants (e.g., healthy controls, adenoma patients, CRC patients) in a validation cohort. Preserve samples immediately at -80°C.
- Method: Extract microbial genomic DNA using a commercial kit (e.g., QIAamp PowerFecal Pro DNA Kit). Quantify DNA concentration and quality using spectrophotometry.
2. 16S rRNA Gene Amplification and Sequencing:
- Material: Prepare primers targeting hypervariable regions (e.g., V3-V4) of the 16S rRNA gene, and use a high-fidelity DNA polymerase for PCR.
- Method: Amplify the target region via PCR. Clean the amplicons and attach dual-index barcodes. Pool the barcoded libraries in equimolar ratios and perform sequencing on an Illumina MiSeq or HiSeq platform to generate paired-end reads.
3. Bioinformatic Processing and Data Analysis:
- Tool: Use the QIIME 2 (Quantitative Insights Into Microbial Ecology 2) platform for data analysis.
- Method: Import raw sequencing data and denoise it to generate amplicon sequence variants (ASVs). Assign taxonomy to ASVs using a reference database (e.g., SILVA or Greengenes). Perform downstream analyses including:
- Alpha-diversity: Calculate Shannon and Simpson indices to assess within-sample diversity.
- Beta-diversity: Calculate metrics like UniFrac to compare microbial communities between sample groups.
- Differential Abundance Analysis: Use a blocked Wilcoxon rank-sum test (adjusting for "study" as a confounder) to identify ASVs significantly altered between disease states.
4. Machine Learning and Model Validation:
- Tool: Employ Random Forest or other machine learning algorithms.
- Method: Construct a classifier using differentially abundant ASVs as features. Validate the model's performance using study-to-study transfer validation or leave-one-dataset-out (LODO) validation, reporting the Area Under the Curve (AUC) to assess diagnostic accuracy.
Protocol for Traditional Biomarker Analysis (Liquid Biopsy and ctDNA)
This protocol outlines the analysis of ctDNA, a key traditional biomarker, focusing on different analytical approaches [105] [108].
1. Sample Collection and Plasma Preparation:
- Material: Collect peripheral blood into cell-stabilizing tubes (e.g., Streck Cell-Free DNA BCT).
- Method: Process blood samples within a defined window (e.g., 6-24 hours). Centrifuge to separate plasma, then perform a second high-speed centrifugation to remove residual cells. Store plasma at -80°C.
2. Cell-free DNA (cfDNA) Extraction:
- Material: Use a commercial cfDNA extraction kit (e.g., QIAamp Circulating Nucleic Acid Kit).
- Method: Extract cfDNA from plasma according to the manufacturer's instructions. Elute and quantify cfDNA using a fluorescence-based assay (e.g., Qubit dsDNA HS Assay).
3. Target Analysis:
- A. Mutation-based Analysis:
- Method: Use next-generation sequencing (NGS) panels or digital PCR (dPCR) to identify and quantify specific somatic mutations (e.g., in KRAS, BRAF, EGFR) in the ctDNA.
- B. Methylation-based Analysis:
- Method: Treat extracted cfDNA with bisulfite to convert unmethylated cytosines to uracils. Perform subsequent sequencing (e.g., whole-genome bisulfite sequencing or targeted bisulfite sequencing) to identify cancer-specific methylation patterns (e.g., in SEPT9).
- C. Fragmentomics-based Analysis:
- Method: Sequence the cfDNA library and analyze the fragmentation patterns—such as fragment size distribution and genomic positioning—using computational tools and AI.
- A. Mutation-based Analysis:
4. Data Analysis and Interpretation:
- Tool: Use specialized bioinformatic pipelines for variant calling, methylation analysis, or fragmentomics analysis.
- Method: Compare results against reference databases and healthy control cohorts to classify samples as positive or negative for cancer signals.
Signaling Pathways and Experimental Workflows
Microbial Mechanisms in Carcinogenesis
The following diagram illustrates key signaling pathways through which specific microbes, such as Fusobacterium nucleatum, contribute to colorectal carcinogenesis, a central concept in microbiome biomarker research [106] [107].
Workflow for Microbial Biomarker Validation
This diagram outlines the end-to-end experimental workflow for discovering and validating microbial biomarkers in a multi-cohort study, from sample collection to model validation [109].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for Biomarker Validation Studies
| Item | Function/Application | Examples / Notes |
|---|---|---|
| Cell-Free DNA Collection Tubes | Stabilizes blood cells and prevents genomic DNA contamination for liquid biopsy. | Streck Cell-Free DNA BCT tubes. |
| Nucleic Acid Extraction Kits | Isolate high-quality microbial DNA from stool or cfDNA from plasma. | QIAamp PowerFecal Pro DNA Kit (stool), QIAamp Circulating Nucleic Acid Kit (plasma). |
| 16S rRNA Primers & Kits | Amplify hypervariable regions for microbial community profiling. | Illumina 16S Metagenomic Sequencing Library preparation protocols. |
| Next-Generation Sequencing (NGS) Platforms | For high-throughput sequencing of 16S rRNA amplicons, ctDNA, and whole metagenomes. | Illumina MiSeq/HiSeq for 16S; NovaSeq for WGS and ctDNA. |
| Digital PCR (dPCR) Systems | For absolute quantification of rare mutations or specific microbial taxa with high sensitivity. | Bio-Rad QX200 Droplet Digital PCR system, Thermo Fisher QuantStudio. |
| Bioinformatics Software Platforms | Process and analyze sequencing data, from quality control to taxonomic assignment. | QIIME 2, mothur, R/Bioconductor packages (phyloseq, DESeq2). |
| Machine Learning Algorithms | Build and validate diagnostic models using high-dimensional biomarker data. | Random Forest, Support Vector Machines (SVMs); implemented in R (caret) or Python (scikit-learn). |
A critical challenge in modern microbiome research is translating findings from homogenous study populations into clinically useful tools that function reliably across diverse human populations. The examination of ethnically diverse cohorts is not merely a box-ticking exercise in inclusivity; it is a fundamental requirement for assessing the generalizability of microbiome-based biomarkers and diagnostics. This guide compares the performance of microbial signatures when validated across multiple ethnicities, providing a data-driven framework for evaluating the robustness of microbiome research outcomes.
The Imperative for Diverse Cohorts in Microbiome Research
Human gut microbiome composition demonstrates significant variation across racial and ethnic groups, a difference that emerges in early infancy and persists through adulthood [110]. One large-scale analysis found that ethnicity explained far more of the differences in gut microbiota than other demographic factors, lifestyle variables, or medical information [111]. This variation stems from a complex interplay of dietary patterns, environmental exposures, socioeconomic factors, and host genetics that are often correlated with ethnic identity.
For microbiome-based diagnostics to achieve clinical utility, they must demonstrate reliability across this natural variation. Research has revealed both promising universal biomarkers and concerning population-specific limitations, highlighting why ethnically diverse validation cohorts are essential for distinguishing broadly applicable signatures from those with restricted utility.
Comparative Performance of Microbiome Biomarkers Across Ethnicities
Table 1: Generalizability of Microbiome Biomarkers Across Diseases and Populations
| Condition | Biomarker Performance | Ethnic Groups Studied | Key Microbial Features | Generalizability Assessment |
|---|---|---|---|---|
| Inflammatory Bowel Disease | 87.5% accuracy in CD, 79.1% in UC diagnosis [112] | Chinese, Westerners [112] | Increased Actinobacteria/Proteobacteria; Decreased Clostridiales [112] | High - Robust diagnostic model across ethnicities [112] |
| Colorectal Cancer | AUC = 0.85 [113] | Multi-cohort (18 studies) [113] | Fusobacterium nucleatum, pks+ E. coli, oral taxa enrichment [113] | High - Universal signatures across populations [114] [113] |
| Depressive Symptoms | α-diversity predicts symptoms (p<0.023) [111] | Dutch, S-Asian Surinamese, African Surinamese, Ghanaian, Turkish, Moroccan [111] | Christensenellaceae, Lachnospiraceae, Ruminococcaceae [111] | High - Association generalizes across ethnicities [111] |
| Lifestyle Intervention Response | AUC up to 0.86 for predicting responders [115] | Multiple ethnicities [115] | Bacteroides stercoris, Prevotella copri, B. vulgatus as resistance biomarkers [115] | High - Predictive model validated across ethnicities [115] |
| Rectal Cancer Microbiome | Significant β-diversity clustering by ethnicity (p<0.001) [116] | White Hispanic vs. non-Hispanic [116] | Prevotellaceae enriched in White Hispanic patients [116] | Low - Distinct signatures by ethnicity [116] |
Experimental Protocols for Cross-Population Validation
Meta-Analysis Framework with Batch Effect Correction
Large-scale meta-analysis of multiple cohorts represents the gold standard for assessing biomarker generalizability. The following workflow outlines the key methodological considerations:
Protocol Implementation:
Cohort Integration: Combine data from studies representing diverse populations. A recent colorectal cancer analysis integrated 3,741 stool metagenomes from 18 cohorts across different geographic regions [113].
Batch Effect Correction: Apply specialized methods like Conditional Quantile Regression (ConQuR) to remove technical variation while preserving biological signals. ConQuR uses a two-part quantile regression model to effectively address batch effects in microbiome data [114].
Cross-Validation: Implement strict cross-cohort validation where models trained on one population are tested on completely separate ethnic groups. The lifestyle intervention study by et al. demonstrated this approach, achieving AUC=0.86 when predicting intervention responders across different ethnicities [115].
Diversity Scaling Analysis
Diversity scaling analysis using the Diversity-Area Relationship (DAR) framework quantifies how microbial diversity partitions across populations and can reveal ethnic-specific patterns:
Methodology:
- Apply DAR power law models to compare diversity scaling parameters across ethnic groups
- Use Hill numbers to measure diversity at different orders (q=0,1,2)
- Fit both power law (PL) and power law with exponential cutoff (PLEC) models
- Compare maximal accrual diversity and scaling parameters (z) across groups
One study applying this approach to seven Chinese ethnic groups found that diversity scaling parameters showed minimal differences (<0.5%) across ethnicities, suggesting common structural principles in gut microbiome organization despite compositional differences [117].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Essential Methodologies and Platforms for Cross-Population Microbiome Research
| Category | Tool/Platform | Specific Application | Role in Generalizability Assessment |
|---|---|---|---|
| Bioinformatics Pipelines | QIIME2 [114] | 16S rRNA data processing | Standardized processing across studies |
| DADA2 [116] | Amplicon Sequence Variant calling | High-resolution taxonomic profiling | |
| MetaPhlAn 4 [113] | Metagenomic taxonomic profiling | Uniform species-level characterization | |
| HUMAnN 3 [113] | Metagenomic functional profiling | Pathway analysis across populations | |
| Statistical Methods | PERMANOVA [114] | β-diversity significance testing | Detects ethnicity-associated differences |
| ANCOM-BC [110] | Differential abundance testing | Identifies ethnicity-associated taxa | |
| LinDA/MaAsLin2 [116] | Differential abundance with confounders | Robust detection of associations | |
| ConQuR [114] | Batch effect correction | Enables cross-study integration | |
| Machine Learning Frameworks | Random Forest [115] | Response prediction | Tests biomarker generalizability |
| MMUPHIN [114] | Meta-analysis framework | Batch correction while finding associations |
Interpretation Framework for Cross-Population Biomarker Performance
The following decision tree provides a systematic approach for evaluating biomarker generalizability across ethnic groups:
Application Guidance:
Universal Biomarkers: Microbial signatures for IBD diagnosis [112] and colorectal cancer detection [113] demonstrate high generalizability, maintaining performance across ethnic boundaries.
Context-Dependent Associations: The link between gut microbiota and depressive symptoms shows consistent directionality across ethnic groups, though effect sizes may vary [111].
Population-Specific Signatures: Rectal cancer microbiomes show distinct clustering by ethnicity, suggesting population-specific microbial interactions that may require tailored approaches [116].
The evidence consistently demonstrates that neglecting ethnic diversity in microbiome study cohorts risks developing diagnostics with restricted utility and perpetuating health disparities. Researchers should prioritize:
Prospective Diverse Recruitment: Intentionally including underrepresented populations in initial discovery cohorts rather than only in validation phases.
Standardized Reporting: Explicitly documenting ethnic composition and socioeconomic context of study populations to enable proper generalizability assessment.
Hierarchical Validation: Implementing cross-validation frameworks that explicitly test performance degradation when moving between ethnic groups.
Contextual Interpretation: Recognizing that even universal biomarkers may operate within population-specific environmental and genetic contexts.
Microbiome research stands at the frontier of personalized medicine, but this promise can only be realized through deliberate attention to the rich tapestry of human diversity. The methodological framework presented here provides a pathway toward more equitable and broadly applicable microbiome science.
The translation of microbiome research into clinically viable diagnostic tools represents a frontier in precision medicine. While initial discovery studies frequently identify promising microbial biomarkers, their real-world utility depends on rigorous validation across independent cohorts. Independent validation is the process of verifying a biomarker's performance in populations distinct from those used in its discovery, confirming that the findings are not artifacts of a specific study cohort but generalizable truths. This process is particularly crucial for microbiome-based diagnostics because the gut microbiome is highly sensitive to confounders including diet, geography, medication use, and sequencing methodologies [4]. Without robust cross-cohort validation, diagnostic models may fail when applied in new clinical settings, delaying patient care and wasting resources.
The field is progressing from single-cohort studies toward multi-cohort frameworks that systematically assess diagnostic generalizability. For instance, a 2023 meta-analysis evaluated cross-cohort performance of gut microbiome-based classifiers for 20 different diseases, revealing both opportunities and significant challenges in achieving reproducible results [4]. Similarly, a 2024 study developed a microbiome-based diagnostic test for inflammatory bowel disease (IBD) and validated it across diverse populations, demonstrating the potential for clinical application [68]. This guide examines the essential steps and methodologies for moving from promising discovery to clinically implemented microbiome-based diagnostics, with objective comparisons of validation approaches and their performance characteristics.
Cross-Cohort Validation Performance Across Diseases
The performance of microbiome-based classifiers varies substantially across disease types and validation frameworks. Systematic analysis reveals that diagnostic accuracy generally remains high for intestinal diseases during cross-validation but drops significantly for many non-intestinal conditions.
Table 1: Cross-Cohort Validation Performance of Microbiome-Based Diagnostic Classifiers
| Disease Category | Specific Diseases | Intra-Cohort AUC | Cross-Cohort AUC | Key Performance Factors |
|---|---|---|---|---|
| Intestinal Diseases | Colorectal Cancer (CRC), Inflammatory Bowel Disease (IBD), Crohn's Disease (CD), Ulcerative Colitis (UC) | ~0.95 [68] | ~0.73-0.94 [4] [68] | Metagenomic sequencing outperforms 16S; combined-cohort training improves generalizability |
| Metabolic Diseases | Type 2 Diabetes (T2D), Obesity | ~0.77 | Significantly lower than intestinal diseases [4] | Strongly confounded by medications (e.g., metformin); requires larger sample sizes |
| Autoimmune Diseases | Rheumatoid Arthritis (RA), Multiple Sclerosis (MS) | ~0.77 | Variable performance [4] | Geographic and ethnic variations affect biomarker consistency |
| Mental/Nervous System Diseases | Autism Spectrum Disorder (ASD), Parkinson's Disease (PD), Alzheimer's Disease (AD) | ~0.77 | Generally low except for specific conditions [4] | Often dominated by confounding factors like dietary preferences |
| Liver Diseases | Non-alcoholic Fatty Liver Disease (NAFLD), Liver Cirrhosis (LC) | ~0.77 | Moderate performance [4] | Medication effects (e.g., proton pump inhibitors) can dominate microbiome signals |
Key insights from comparative analyses indicate that intestinal diseases consistently show superior cross-cohort validation performance, with inflammatory bowel disease (IBD) diagnostics achieving areas under the curve (AUC) >0.90 in both discovery and validation cohorts [68]. This robustness likely stems from the direct interaction between gut microbes and intestinal pathology. In contrast, classifiers for metabolic, autoimmune, and mental diseases experience significant performance degradation in cross-cohort validation, highlighting the challenges of distant signaling and substantial confounding effects [4].
Experimental Protocols for Validation Studies
Cohort Selection and Sample Processing
Robust validation requires careful cohort design and standardized laboratory protocols. The meta-analysis by [4] established rigorous inclusion criteria: case-control studies with clearly defined disease information, minimum of 15 valid samples per group, and exclusion of participants with recent antibiotic or probiotic use. For IBD diagnostics, [68] analyzed 5,979 fecal samples from 13 cohorts across eight countries, ensuring geographic and ethnic diversity in validation cohorts.
Sample processing follows standardized pipelines:
- Fecal Sample Collection: Participants provide fresh fecal samples using standardized collection kits with stabilizers to preserve microbial DNA
- DNA Extraction: Use of validated kits (e.g., QIAamp PowerFecal Pro DNA Kit) with rigorous quality control measures
- Sequencing Approach Selection: Choice between:
- 16S rRNA Gene Sequencing: Lower cost but limited to genus-level taxonomy
- Whole Metagenomic Shotgun (mNGS) Sequencing: Higher resolution to species level and functional potential [4]
- Bioinformatic Processing: Quality filtering, removal of human reads, taxonomic profiling using reference databases, and functional annotation
Statistical Analysis and Machine Learning Protocols
Validation studies employ sophisticated statistical frameworks to build and test diagnostic models:
Differential Abundance Analysis:
- Use generalized linear models (MaAsLin2) to identify differentially abundant taxa
- Adjust for clinical covariates (age, gender, BMI)
- Apply false discovery rate (FDR) correction for multiple testing [68]
Machine Learning Classifier Development:
- Algorithm selection: Random Forest, Lasso, Elastic Net, or Ridge Regression
- Five-fold cross-validation with three repetitions on discovery cohorts
- Feature selection based on importance scores and biological relevance [4]
Cross-Cohort Validation Framework:
- Intra-cohort validation: Performance assessment on holdout samples from the same cohort
- Cross-cohort validation: Application of trained classifiers to completely independent cohorts
- Combined-cohort modeling: Training on samples pooled from multiple cohorts to improve generalizability [4]
Performance Metrics:
- Area Under the Receiver Operating Characteristic Curve (AUC)
- Sensitivity and specificity calculations
- Marker Similarity Index to quantify cross-cohort biomarker consistency [4]
Visualization of Validation Workflows and Pathways
Experimental Workflow for Microbiome Diagnostic Validation
Microbiome Signaling Pathways in Disease
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Essential Research Reagents for Microbiome Diagnostic Validation
| Reagent/Category | Specific Examples | Function in Validation Pipeline |
|---|---|---|
| DNA Extraction Kits | QIAamp PowerFecal Pro DNA Kit, DNeasy PowerSoil Kit | Standardized microbial DNA isolation with removal of PCR inhibitors |
| Sequencing Technologies | Illumina NovaSeq (mNGS), PacBio Sequel (16S full-length), Ion Torrent | High-throughput sequencing with different resolutions and cost structures |
| PCR Reagents | ddPCR Supermix, qPCR master mixes, target-specific primers/probes | Validation of specific bacterial markers identified through sequencing |
| Bioinformatic Tools | QIIME2, MOTHUR, MaAsLin2, HUMAnN2, PICRUSt2 | Taxonomic profiling, differential abundance analysis, functional prediction |
| Reference Databases | Greengenes, SILVA, GTDB, UNIREF | Taxonomic classification of sequence reads and functional annotation |
| Statistical Packages | R packages: phyloseq, vegan, randomForest, glmnet | Statistical analysis, machine learning, and data visualization |
The selection of appropriate reagents and platforms significantly impacts validation outcomes. For instance, [4] demonstrated that classifiers using metagenomic data consistently outperformed those based on 16S amplicon data for intestinal diseases, highlighting the importance of sequencing depth and resolution. The transition from discovery to clinical application often involves moving from sequencing-based approaches to targeted detection methods. The IBD diagnostic developed by [68] utilized a multiplex droplet digital PCR (m-ddPCR) test targeting selected bacterial species, demonstrating that focused assays can maintain diagnostic performance while improving clinical practicality.
Independent validation remains the critical gateway between promising microbiome discoveries and clinically useful diagnostic tools. The comparative data presented in this guide demonstrates that while robust validation is achievable—particularly for intestinal diseases—it requires meticulous attention to cohort design, standardization of methodologies, and comprehensive performance assessment across diverse populations. The emerging framework for microbiome-based diagnostic validation emphasizes multi-cohort designs, combined-cohort modeling to improve generalizability, and systematic assessment of confounding factors [4].
Future directions in the field include integration of microbiome biomarkers with other diagnostic modalities, development of standardized analytical frameworks, and adherence to emerging guidelines for AI-based biomarkers [118]. As validation methodologies mature and datasets expand, microbiome-based diagnostics hold exceptional promise for transforming disease detection and personalized medicine approaches across numerous clinical domains.
Conclusion
The validation of microbiome biomarkers represents a paradigm shift in diagnostic medicine, offering non-invasive approaches for early disease detection across multiple conditions. Successful translation requires robust multi-cohort validation frameworks, advanced computational methods for batch effect correction, and standardized methodologies to ensure reproducibility. Future research must focus on elucidating causal mechanisms, developing large-scale prospective studies, and integrating microbiome biomarkers with existing clinical diagnostics. The convergence of multi-omics technologies, artificial intelligence, and carefully designed validation cohorts will ultimately enable the clinical implementation of microbiome-based diagnostics, paving the way for personalized medicine approaches that leverage our microbial counterparts for improved human health.
References
- 1. Enhancing Human Superorganism Ecosystem Resilience ... [https://www.mdpi.com/2673-8007/1/3/31]
- 2. Research | Mangalam Laboratory - Department of Pathology [https://mangalam.lab.uiowa.edu/research]
- 3. The microbiome in graft-versus-host disease: a tale of two ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06797-5]
- 4. Performance of Gut Microbiome as an Independent Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10161951/]
- 5. Holobiont-based genetic analysis reveals new plant and ... [https://bmcplantbiol.biomedcentral.com/articles/10.1186/s12870-025-06995-9]
- 6. IMPACTT Symposium 2025 Abstracts [https://www.impactt-microbiome.ca/impactt-symposium-2025-abstracts/]
- 7. Fusobacterium in the microbiome: from health to disease ... [https://www.nature.com/articles/s41522-025-00838-z]
- 8. Potential and application of Fusobacterium nucleatum in ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1652702/full]
- 9. Fusobacterium nucleatum and Its Impact on Colorectal Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523259/]
- 10. Fusobacterium nucleatum and colorectal cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC9745098/]
- 11. Opportunistic detection of Fusobacterium nucleatum as a ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-020-01887-4]
- 12. Consistent signatures in the human gut microbiome of old [https://www.nature.com/articles/s41467-024-47523-x]
- 13. Microbiome multi-omics analysis reveals novel biomarkers ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00802-1]
- 14. Oral microbiome as a diagnostic biomarker for pancreatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541924/]
- 15. Integrative microbiome- and metatranscriptome-based ... [https://www.nature.com/articles/s41522-025-00807-6]
- 16. Respiratory diseases and gut microbiota [https://pmc.ncbi.nlm.nih.gov/articles/PMC11286581/]
- 17. Respiratory diseases and the gut microbiota: an updated ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1629005/full]
- 18. Lung microbiome: new insights into the pathogenesis of ... [https://www.nature.com/articles/s41392-023-01722-y]
- 19. The gut microbiota and obesity: from correlation to causality [https://pubmed.ncbi.nlm.nih.gov/23912213/]
- 20. Microbiome analysis: Correlation is not causation [https://lizard.bio/knowledge-hub/microbiome-correlation-not-causation]
- 21. A Consensus Statement on establishing causality ... [https://www.nature.com/articles/s41575-025-01041-3]
- 22. Chains of evidence from correlations to causal molecules ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8480537/]
- 23. Approaches to discern if microbiome associations reflect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9361767/]
- 24. Gut microbiome may predict invisible chronic fatigue ... [https://www.jax.org/news-and-insights/2025/july/gut-microbiome-may-predict-invisible-chronic-fatigue-syndrome-and-long-covid]
- 25. Microbiome engineering to enhance disease resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479497/]
- 26. Microbiome Gut-Brain-Axis: Impact on Brain Development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289773/]
- 27. Microbiota–gut–brain axis and its therapeutic applications ... [https://www.nature.com/articles/s41392-024-01743-1]
- 28. The gut-brain connection: What the science says [https://med.stanford.edu/news/insights/2025/03/gut-brain-connection-long-covid-anxiety-parkinsons.html]
- 29. Microbiota–gut–brain axis in neurodegenerative diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436269/]
- 30. Harnessing the microbiota-gut–brain axis to prevent and ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07279-4]
- 31. decoding the gut–immune–brain axis in health and disease [https://www.nature.com/articles/s41423-025-01333-3]
- 32. Recent drug delivery systems targeting the gut-brain ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325006131]
- 33. Nutrition & microbiome research highlights NeuroGASTRO ... [https://www.gutmicrobiotaforhealth.com/nutrition-and-microbiome-research-highlights-from-neurogastro-2025/]
- 34. Gut microbiome metagenomics in clinical practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562794/]
- 35. Metagenomics, Metatranscriptomics, and Metabolomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4869604/]
- 36. A Focus on Metagenomics, Metatranscriptomics, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388303/]
- 37. Metatranscriptomics vs Metagenomics: Exploring the ... [https://www.cosmosid.com/blog/metatranscriptomics-vs-metagenomics-exploring-the-difference/]
- 38. Comparison of two metabolomics-platforms to discover ... [https://www.sciencedirect.com/science/article/pii/S0010482524014781]
- 39. Metatranscriptomics-based metabolic modeling of patient ... [https://www.nature.com/articles/s41522-025-00823-6]
- 40. Efficient discovery of robust prognostic biomarkers and ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525000667]
- 41. Robust and consistent biomarker candidates identification by ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-024-02578-0]
- 42. Cross-cohort microbiome-wide study reveals consistent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455987/]
- 43. Integrative machine learning identifies robust inflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12128390/]
- 44. Optimizing Feature Selection and Machine Learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12314567/]
- 45. Research and performance analysis of random forest ... [https://www.nature.com/articles/s41598-024-76706-1]
- 46. SGA-Driven feature selection and random forest ... [https://www.nature.com/articles/s41598-025-95786-1]
- 47. A Hybrid Sequential Feature Selection Approach for ... [https://www.mdpi.com/2218-273X/15/7/963]
- 48. Machine learning-based meta-analysis reveals gut ... [https://www.nature.com/articles/s41467-025-56829-3]
- 49. Gut microbiome-based machine learning model for early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12509340/]
- 50. Enhancing Alzheimer's disease prediction using random ... [https://www.sciencedirect.com/science/article/pii/S2452318625000352]
- 51. Accuracy Is Not Enough: Stability-Aware Feature Selection ... [https://pubmed.ncbi.nlm.nih.gov/40985317/]
- 52. Salivary and fecal microbiota: potential new biomarkers for ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1182346/full]
- 53. Oral and gut microbiome profiles in people with early ... [https://www.nature.com/articles/s43856-024-00630-8]
- 54. Can Salivary Biomarkers Serve as Diagnostic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384429/]
- 55. Circulating miRNAs as liquid biopsy biomarkers for ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1574586/full]
- 56. Biomarker discovery for non-invasive diagnosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226589/]
- 57. Towards practical point-of-care quick, ubiquitous ... [https://www.nature.com/articles/s41378-025-01057-4]
- 58. Assessment of Mathematical Approaches for the Estimation ... [https://www.mdpi.com/2673-8856/4/3/12]
- 59. High-Throughput Pathogen Detection Unlocks Affordable ... [https://www.labmanager.com/high-throughput-pathogen-detection-unlocks-affordable-assay-development-33082]
- 60. Comparison of quantitative PCR and digital PCR assays ... [https://www.sciencedirect.com/science/article/pii/S0166093423001842]
- 61. High-throughput pathogen detection for affordable assay ... [https://www.takarabio.com/AMPexpo?srsltid=AfmBOoqVilDvyMO_sGCjv6rkQPkg7capSifpKF9gT-6pOKYcZm4XSa0T]
- 62. Efficient experimental design and analysis of real-time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3710343/]
- 63. PCR-Stop analysis as a new tool for qPCR assay validation [https://www.nature.com/articles/s41598-018-26116-x]
- 64. Assessing and mitigating batch effects in large-scale omics ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03401-9]
- 65. High performance data integration for large-scale analyses ... [https://www.nature.com/articles/s41467-025-62237-4]
- 66. Harmony-based data integration for distributed single-cell ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013526]
- 67. Identification and validation of microbial biomarkers from ... [https://pubmed.ncbi.nlm.nih.gov/38745111/]
- 68. Noninvasive, microbiome-based diagnosis of inflammatory ... [https://www.nature.com/articles/s41591-024-03280-4]
- 69. A review on multi-omics integration for aiding study design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372284/]
- 70. New findings may fix the replicability crisis in microbiome ... [https://www.eurekalert.org/news-releases/1049490]
- 71. Deep generative modeling of sample-level heterogeneity ... [https://www.nature.com/articles/s41592-025-02808-x]
- 72. Snowflake: visualizing microbiome abundance tables as ... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2024.1331043/full]
- 73. Towards standardized and reproducible research in skin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9790573/]
- 74. Large-scale microbiome data integration enables robust ... [https://www.nature.com/articles/s43588-022-00247-8]
- 75. Resilience of human gut microbiomes in autism spectrum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11878074/]
- 76. Microbial biomarker discovery in Parkinson's disease through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11513973/]
- 77. Gut microbiome network ensemble analysis for identifying ... [https://www.sciencedirect.com/science/article/abs/pii/S2212429225008727]
- 78. Disrobiom: A novel approach to discover robust biomarkers ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809424009935]
- 79. Decoding IBD progression: a dynamic biomarker atlas for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07024-x]
- 80. Improving the accuracy of medical diagnosis with causal ... [https://www.nature.com/articles/s41467-020-17419-7]
- 81. Cross-cohort analysis identifies shared gut microbial ... [https://pubmed.ncbi.nlm.nih.gov/40528214/]
- 82. Meta-analysis of the human gut microbiome uncovers shared ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11334437/]
- 83. BugSigDB captures patterns of differential abundance ... [https://www.nature.com/articles/s41587-023-01872-y]
- 84. Harnessing machine learning for metagenomic data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12625703/]
- 85. Stanford researchers use color-coding to pinpoint locations of ... [https://biox.stanford.edu/highlight/stanford-researchers-use-color-coding-pinpoint-locations-gut-bacterial-strains]
- 86. How longitudinal data can contribute to our understanding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9980606/]
- 87. Decoding longitudinal microbiome trajectories [https://pmc.ncbi.nlm.nih.gov/articles/PMC12342957/]
- 88. A systematic longitudinal study of microbiome: integrating ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-12282-6]
- 89. coda4microbiome: compositional data analysis for ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05205-3]
- 90. A Survey of Statistical Methods for Microbiome Data Analysis [https://www.frontiersin.org/journals/applied-mathematics-and-statistics/articles/10.3389/fams.2022.884810/full]
- 91. Hypothesis testing and statistical analysis of microbiome [https://pmc.ncbi.nlm.nih.gov/articles/PMC6128532/]
- 92. Multi-cohort metagenomics reveals strain functional ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1656016/full]
- 93. A multi-center study for colorectal cancer early detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574013/]
- 94. Multi-cohort analysis of colorectal cancer metagenome ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-018-0451-2]
- 95. Multi-cohort analysis reveals colorectal cancer tumor ... [https://www.sciencedirect.com/science/article/pii/S1931312825000952]
- 96. Development and multi-cohort validation of a machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357463/]
- 97. Multi-cohort high-dimensional proteomics reveals early risk ... [https://www.nature.com/articles/s41467-025-64534-4]
- 98. Receiver Operating Characteristic (ROC) Curve Analysis for Medical Diagnostic Test Evaluation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3755824/]
- 99. Receiver operating characteristic curve analysis in diagnostic accuracy studies: A guide to interpreting the area under the curve value - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 100. A systematic review of microbiome-derived biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9804137/]
- 101. Prediction model based on gut microbiota as a non- ... [https://link.springer.com/article/10.1007/s00253-025-13548-5]
- 102. Systematic review with meta-analysis of diagnostic test accuracy for COVID-19 by mass spectrometry - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8548837/]
- 103. Emerging biomarkers for early cancer detection and diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359849/]
- 104. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 105. Beyond Detection: Conventional and Emerging Biomarkers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427498/]
- 106. Microbiota as diagnostic biomarkers: advancing early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12095362/]
- 107. Microbiota as diagnostic biomarkers: advancing early ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1559480/full]
- 108. Progress in early cancer detection in the clinical laboratory [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/early-cancer-detection-progress.html]
- 109. Identification of microbial markers across populations in ... [https://www.nature.com/articles/s41467-021-23265-y]
- 110. Human microbiome variation associated with race and ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10434942/]
- 111. The gut microbiota and depressive symptoms across ethnic ... [https://www.nature.com/articles/s41467-022-34504-1]
- 112. Gut Microbiota Offers Universal Biomarkers across ... [https://pubmed.ncbi.nlm.nih.gov/29404425/]
- 113. Pooled analysis of 3741 stool metagenomes from 18 ... [https://www.nature.com/articles/s41591-025-03693-9]
- 114. Meta-analysis of gut microbiome reveals patterns ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12309989/]
- 115. Identification of robust and generalizable biomarkers for ... [https://pubmed.ncbi.nlm.nih.gov/37553697/]
- 116. Assessment of Distinct Gut Microbiome Signatures in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11361339/]
- 117. Diversity Scaling Analysis of Chinese Gut Microbiomes ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.736393/full]
- 118. The first ESMO guidance for AI-based biomarkers [https://dailyreporter.esmo.org/spotlight/the-first-esmo-guidance-for-ai-based-biomarkers]